Abstract
Background
As non-ampullary duodenal cancer is relatively rare, the optimal treatment strategy, including the appropriate surgical procedure and efficacy of adjuvant chemotherapy, remains unclear. This nationwide survey aimed to clarify the actual lymph node spread pattern and determine the optimal treatment strategy for this disease, using a large-scale database.
Methods
We used a questionnaire and a retrospective registry of 1083 patients with non-ampullary duodenal cancer who had undergone surgery during 2008–2017 in 114 high-volume Japanese Society of Hepatobiliary and Pancreatic Surgery-certified training institutions. Propensity score-matched analyses were conducted to minimise background bias. Cox regression was performed to identify covariates associated with recurrence-free survival. There were distinct disparities in the nodal dissection rate according to the predominant tumor location and tumor invasion depth. Metastases were frequently observed in the peripancreatic nodes and those along the superior mesenteric artery, irrespective of tumor location. Their dissection seemed to be beneficial for improved survival. In the overall cohort, no survival benefit was observed in patients who received adjuvant chemotherapy when compared with that in patients who underwent surgery alone. Nevertheless, in the matched cohort, adjuvant chemotherapy for > 6 months was associated with a significant improvement in recurrence-free survival (median: 43.5 vs. 22.5 months, p = 0.016), particularly in patients with tumor invasion of the subserosa or deeper tumor invasion, lymph node metastasis, or elevated serum carbohydrate antigen 19-9 levels.
Conclusion
Pancreatoduodenectomy should be the standard procedure for advanced non-ampullary duodenal cancer. Adjuvant chemotherapy for > 6 months, especially for advanced tumors, significantly improves survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-ampullary duodenal cancer is a relatively rare disease with no established treatment guidelines [1, 2]. It is generally acknowledged that surgical resection is the only potentially curative treatment. Due to anatomical reasons, surgical procedures vary drastically depending on tumor location and depth of invasion, and include local resection (LR), pancreatoduodenectomy (PD), distal gastrectomy (DG), and pancreas-preserving duodenectomy. Such diversity leads to significant differences in the type of reconstruction, mortality, morbidity, and postoperative quality of life [3,4,5,6,7,8]. In addition, unlike other gastrointestinal malignancies, the survival benefit of adjuvant chemotherapy for patients with non-ampullary duodenal cancer remains controversial [9,10,11].
Some meta-analyses and systematic reviews have focused on the treatment of duodenal cancer [1, 12,13,14,15,16,17]. However, the majority were retrospective, single-institutional, and small case series. We conducted a nationwide survey to investigate the optimal treatment strategy for non-ampullary duodenal cancer, aiming mainly to elucidate the precise lymph node spread pattern, determine the appropriate surgical procedure and extent of lymph node dissection according to both predominant tumor location and depth of invasion, and define the role of adjuvant chemotherapy using a large comprehensive database.
Methods
Study design and population
This national questionnaire survey included patients with non-ampullary duodenal cancer who had undergone surgical treatment between January 2008 and December 2017. We selected Japanese Society of Hepatobiliary and Pancreatic Surgery-certified training institutions with high volumes of hepato-biliary-pancreatic surgeries because PD, the most frequently selected type of surgical resection for this disease, is often associated with a relatively high rate of complications. The study protocol was approved by the institutional ethical review boards of all participating hospitals. Informed consent for analysis was obtained from all participants by the opt-out approach.
Definitions
The duodenum is divided anatomically into four segments: first (superior segment), second (descending segment), third (horizontal segment), and fourth (ascending segment). Patients with third or fourth segment tumors were classified into a single group (third/fourth) due to small sample size. Pathological tumor depth was classified as follows: is/M, tumor in situ or tumor confined to the lamina propria; SM, tumor confined to the submucosa; MP, tumor invasion of the muscularis propria; SS, tumor invasion of the subserosa; SE, tumor invasion that is contiguous to or penetrates the serosa and is exposed to the peritoneal cavity; and SI, tumor invasion of adjacent structures. The number of lymph node stations (nos.) was determined according to the uniform definition of pancreatic carcinoma established by the Japan Pancreas Society [18]. Procedures performed included PD, DG, and LR of the duodenum. Lymph node dissection included systematic regional lymphadenectomy and limited lymph node dissection. Perioperative complications were assessed according to the Clavien–Dindo classification [19, 20]. The indication for adjuvant chemotherapy and selection of the chemotherapeutic regimens were left to the discretion of physicians.
Statistical analysis
All statistical analyses were performed using JMP software ver. 14.3 (SAS Institute Inc.). The final follow-up date was June 30, 2019. Overall survival (OS) was defined as the period from the time of surgery to the date of death from any cause or censoring until the date of the last follow-up. Recurrence-free survival (RFS) was calculated from surgery to the first detection of recurrence or earlier death of any cause. Data from patients who were alive without recurrence at the last follow-up were censored for the RFS analysis. Kaplan–Meier survival analysis and the corresponding log-rank tests were carried out to determine differences in survival rates. Categorical variables were compared using the χ-squared test. Continuous variables were compared using the Mann–Whitney U test or Kruskal–Wallis test. The univariate and multivariate hazard ratios (HRs) were calculated using a Cox proportional hazard model. p < 0.05 was considered statistically significant.
A matched cohort study using propensity score methodology was used to minimize the treatment bias associated with the administration of adjuvant chemotherapy. A propensity score for each patient was calculated by logistic regression using the co-variables known to affect postoperative outcomes. One-to-one propensity score-matched study groups were created using nearest-neighbor matching without replacement. A caliper of 0.20 multiplied by the standard deviation of the logit of the propensity score was used. Outcomes were compared between the two groups before and after propensity score matching.
We used a previously described method to evaluate the therapeutic benefits of lymph node dissection [21, 22]. The frequency of metastasis at each station was determined by dividing the number of patients with metastasis at that station by the number of patients in whom that station was dissected. The cumulative 5-year OS rate of patients with metastasis at each nodal station was calculated while discounting the presence/absence of metastasis at other stations. An index of the benefit gained by dissection at each station was calculated by multiplying the frequency of metastasis by the 5-year OS rate of patients with metastasis for each station. The index was not determined for stations that had not been dissected in all patients or in which no metastasis was reported in any patients in whom the station had been dissected. Similarly, we did not determine the index when all surviving patients with metastasis at the station had been censored within a 5-year period.
Results
Clinicopathological characteristics and survival outcomes
Among 230 Japanese Society of Hepatobiliary and Pancreatic Surgery-certified training institutions, 114 (49.5%) participated in this study, and 1083 patients were included in the analysis (Supplemental Fig. 1). Clinicopathological characteristics according to tumor invasion depth are presented in Table 1. The median follow-up duration was 38.3 months (0.2–137.8). The most frequent procedure in patients with SM or deeper invasion was PD, whereas LR was mostly performed in is/M patients. In addition, DG was performed for 79 patients (29%) of tumors predominantly located in the first segment (Supplemental Table 1). The rates of 30-day mortality after LR/DG/PD were 0/0/0.7%, respectively.
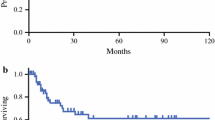
The 5-year OS and RFS rates were 70.8% and 69.5%, respectively. The survival curves were well stratified according to the depth of tumor invasion (Fig. 1). Furthermore, the median post-recurrence survival was 14.2 months (0.2–107.7). The 1-, 2- and 3-year post-recurrence survival rates were 55.0, 30.0 and 17.2%, respectively.
Cumulative survival curves according to the depth of tumor invasion. a Overall and b recurrence-free survival analysis. is/M tumor in situ or confined to the lamina propria, SM tumor confined to the submucosa, MP tumor invades the muscularis propria, SS tumor invades the subserosa, SE tumor invasion is contiguous to the serosa or penetrates the serosa and is exposed to the peritoneal cavity, SI tumor invades adjacent structure
Rates of lymph node dissection and metastasis according to tumor location
As the anatomical distribution of regional lymph nodes and the pattern of lymph node metastasis influence the choice of surgical procedure, we further evaluated the incidence of metastasis in each nos. The analysis was conducted on patients with advanced (MP or deeper) tumors because the rates of lymph node dissection and metastasis among patients with is/M tumors were very low. Patients with SM were independently evaluated because their rate of positive lymph node metastasis was non-negligible but still relatively low (Table 1, Supplemental Fig. 2 and Supplemental Fig. 3).
Overall, 10,183 lymph nodes from 599 patients with advanced cancer were analyzed; the median number of harvested lymph nodes per patient was 17 (0–88). Metastasis to at least one lymph node station was found in 363 patients (61.4%). The frequency of lymph node metastasis according to tumor location and depth of invasion is summarized in Fig. 2 and Supplemental Fig. 3. For cancers predominantly in the first or second segments, lymph nodes along the common hepatic artery and hepatoduodenal, infra-pyloric, and posterior pancreatic head nodes (nos. 8, 12, 6, 13) were usually dissected. Pancreatic nodes and nodes along the superior mesenteric artery were preferentially dissected in cancers predominantly in the third/fourth segments, while the frequency of dissection for nos. 8 and 6 remained below 50%. The frequency of nodal dissection along the left gastric artery and around the celiac axis area (nos. 7, 9) was very low, regardless of tumor location or depth.
Distribution of lymph node metastasis in MP or deeper non-ampullary duodenal cancer according to tumor location. a the first segment (n = 136), b the second segment (n = 366), c the third/fourth segments of the duodenum (n = 97) No.5, supra-pyloric; No.6, infra-pyloric; No.7, left gastric artery; No.8, along the common hepatic artery; No.9, around the celiac axis; No.12, hepatoduodenal; No.13, posterior pancreatic head; No.14, along the superior mesenteric artery; No.17, anterior pancreatic head; No.16, para-aortic lymph nodes
Metastasis rates were relatively high at nos. 13, 14, and 17 in all cancers. The rate of metastasis at nos. 6 was low, but not negligible in the first and second segments. The rates of metastasis at nos. 5, 7, and 9 were extremely low and unrelated to tumor location or depth. However, this might be a reflection of their low dissection rates.
Estimated survival benefit of nodal dissection
Table 2 shows the frequency of lymph node metastases, 5-year OS rate for involvement at each nodal station, and survival benefit index of advanced cancer (MP/SS/SE/SI) according to tumor location. For tumors predominantly in the second segment, the index was highest for nos. 13 followed by 17 and 14. The index values for these stations were also high in cancers predominantly located in the first segment. The frequency of metastases in those stations was equivalent, even in III/IV segment-predominant cancer, while the index values were low despite the optimal cut-off value not being clear. For cancers predominantly in the first segment, the index values were also high in nos. 6, 12, and 8. In contrast, the index value of para-aortic lymph nodes was very low in all cancers.
Impact of adjuvant chemotherapy for non-ampullary duodenal cancer
Adjuvant chemotherapy was administered to 278 (25.7%) patients. The most frequent regimen was S-1 monotherapy (n = 220), followed by capecitabine plus oxaliplatin (n = 24), modified FOLFOX6 (fluorouracil, leucovorin, and oxaliplatin, n = 15), S-1 plus gemcitabine (n = 3), S-1 plus irinotecan (n = 3), tegafur/uracil (n = 3), capecitabine monotherapy (n = 2), gemcitabine monotherapy (n = 2), S-1 plus oxaliplatin (n = 2), paclitaxel monotherapy (n = 1), 5-FU monotherapy (n = 1), irinotecan plus bevacizumab (n = 1), and S-1 plus cisplatin (n = 1). Median duration of treatment was 7.4 months (0.1–64.4).
In the overall cohort, there were significant differences in age, ASA classifications, tumor location, CA19-9 level, surgical procedure, rate of lymph node dissection, tumor size, tumor depth, rate of positive lymph node metastasis, histological differentiation type, residual tumor between patients with and without adjuvant chemotherapy administration. To control for treatment bias, one-to-one propensity score matching was performed using these co-variables, creating 188 well-balanced pairs of patients (Table 3). In the overall cohort, the RFS of patients who started adjuvant chemotherapy and received it for over 6 months was shorter than those who underwent surgery alone or received adjuvant chemotherapy for less than 6 months (median RFS 28.8 months vs. not reached, p < 0.001; Supplemental Fig. 4a and 44.1 months vs. not reached, p < 0.001; Supplemental Fig. 4b). In the matched cohort, there was no difference in RFS between patients who started adjuvant chemotherapy and those that did not (median RFS 29.2 vs. 41.1 months, p = 0.819; Supplemental Fig. 4c), but the RFS of those who received adjuvant chemotherapy for over 6 months was significantly better than that of those who received less than 6 months’ treatment (median RFS 43.5 vs. 22.5 months, p = 0.016; Supplemental Fig. 4d). The median duration of adjuvant therapy of those who received over 6 months in matched cohort was 10.1 months (6.2–64.4). The OS of patients who received adjuvant chemotherapy for over 6 months was also significantly better than that of those who received less than 6 months’ treatment (median OS not reached vs. 48.2 months, p < 0.001).
Cox proportional hazards regression analysis of RFS was performed to evaluate the prognostic importance of adjuvant chemotherapy. Univariate analysis identified ASA (American Society of Anesthesiologists) classification, CEA (carcinoembryonic antigen), CA19-9 (carbohydrate antigen 19–9), tumor size, positive lymph node metastasis, pathological differentiation type, microscopically positive margin (R1), initiation of adjuvant chemotherapy, and over 6 months of adjuvant chemotherapy as significant predictors of RFS in the entire cohort (Table 4). Among these, CA19-9, positive lymph node metastasis, R1 status, and over 6 months of adjuvant chemotherapy were independently associated with RFS. Furthermore, adjuvant chemotherapy for over 6 months was independently associated with prolonged RFS in the matched cohort [HR, 0.610; 95% confidence interval (CI), 0.437–0.839; p = 0.002].
Finally, the efficacy of adjuvant chemotherapy in patient subgroups was analyzed. Adjuvant chemotherapy for over 6 months led to significant improvement in RFS in patients with SS or deeper tumors (HR, 0.626; 95% CI, 0.446–0.865; p = 0.004), lymph node metastases (HR, 0.553; 95% CI, 0.377–0.793; p = 0.001), and elevated CA19-9 levels (HR, 0.535; 95% CI, 0.331–0.838, p = 0.006) (Fig. 3).
Discussion
The rarity of non-ampullary duodenal cancers makes randomized clinical trials that could answer questions regarding diagnosis and optimal treatment challenging. Therefore, treatment strategy is often decided based on individual experience or institutional policy. To improve patient care, we conducted a nationwide survey and collected precise large-scale clinical data from accredited surgical centers in Japan. This study involving 1083 patients that underwent resection of non-ampullary duodenal cancer revealed several important findings.
The 5-year OS in the present study was 70.8%, more favorable than that reported previously [12, 13, 23,24,25,26,27]. This may be because our cohort included 484 patients with relatively early-stage tumors (is/M and SM), accounting for 44.7% of all patients. This is likely because esophagogastroduodenoscopy is a common practice in Japan due to the high incidence of gastric cancer. Furthermore, our study demonstrated that postoperative prognosis depends on tumor depth, suggesting that the optimal treatment may vary according to the depth of invasion, similar to other gastrointestinal cancers.
This study showed that the frequency of lymph node metastasis in each nodal station differed according to the tumor location. Therefore, the optimal surgical procedure for non-ampullary duodenal cancer would depend on the tumor location, depth of invasion, and extent of lymph node involvement.
Patients with is/M tumors are generally considered to have minimal risk of lymph node metastasis. In this study, 1.5% (6/398) of patients with is/M tumors had positive lymph nodes. Therefore, if precise pretreatment determination of tumor depth can be made, the optimal treatment for is/M tumors would be endoscopic resection. If endoscopic resection is not suitable or technically challenging, LR without lymph node dissection may be indicated. For SM tumors, curative-intent surgery with regional lymph node dissection, mostly PD, may be generally recommended because lymph node metastasis is identified in > 10% of patients. However, pre- and intraoperative assessments of tumor depth and lymph node metastasis are occasionally unreliable, and over- or underestimations may occur. Therefore, if the final pathological examination after endoscopic resection or LR reveals a tumor depth of SM or deeper, a second surgery with lymph node dissection should be considered.
Regarding MP or deeper tumors, we demonstrated the pattern of spread for each nos. according to tumor location. We also determined the benefits of nodal dissection by evaluating the incidence of metastasis at each station and the corresponding 5-year survival rate, irrespective of metastases to other stations. The distribution of lymph node metastasis and therapeutic benefit of nodal dissection for tumors predominantly in the first and second segments were mostly similar. Therefore, PD may be oncologically adequate in these cases. While occasionally performed, DG for tumors predominantly located in the first segment may be insufficient because the metastasis rates and therapeutic value of dissection of the pancreatic nodes and those along the superior mesenteric artery were equivalent to those of infra-pyloric nodes and those along the common hepatic artery. In contrast, PD may be generally recommended for the complete removal of possible lymph node metastasis in third/fourth segment tumors. Pancreatic lymph nodes and those along the superior mesenteric artery are reasonable targets for dissection given the incidence of metastasis, although the apparent therapeutic benefit of dissection of tumors predominantly located in the third/fourth segments seems to be low. In nos. 6, 8, and 12, the rate of metastasis might be underestimated, as the frequency of dissection was very low. The clinical importance of PD is related to local control of the disease as well as comprehensive lymph node staging.
Para-aortic lymph node metastasis is currently considered as distant metastasis in almost all gastrointestinal malignancies. The therapeutic benefit index of para-aortic lymph node dissection was extremely low (0–3.2 in advanced tumors; Table 2). Thus, prophylactic dissection or aggressive resection is not recommended for patients with suspected para-aortic node metastasis. Taken together, this study suggested that PD could be the standard procedure for all cases of advanced non-ampullary duodenal cancer. Further, LR and DG may be tentatively recommended as an alternative option, especially for patients unable to tolerate PD.
The importance and optimal indications of adjuvant chemotherapy for non-ampullary duodenal cancer have not been established. In this study, approximately 25% of patients received adjuvant chemotherapy, mostly for advanced tumors. Since prospective randomized trials to explore the survival impact of adjuvant chemotherapy are not feasible in non-ampullary duodenal cancer, propensity score matching was utilized to minimize imbalances in patient demographics, tumors, and treatment-related covariates. Recently, two analyses from the National Cancer Data Base evaluating the efficacy of adjuvant chemotherapy in non-ampullary duodenal cancer were reported [28, 29]. One compared surgery alone with adjuvant chemotherapy for duodenal adenocarcinoma as a part of small bowel adenocarcinoma. In the matched cohort, OS was significantly improved with adjuvant chemotherapy in stage III tumors of the duodenum and jejunoileum [28]. The other showed that the addition of radiation to adjuvant chemotherapy had no survival benefit, even in high-risk patients with duodenal adenocarcinoma including positive-margin surgical resection and T4 classification [29]. Although the National Cancer Data Base is the authoritative registry of cancer statistics in the United States, it has some unavoidable limitations including the lack of detailed information of the adjuvant chemotherapy and long-term surveillance. We focused on clinical data collected over a decade at accredited high-volume surgical centers to ensure the reliability of data. Although previous reports had investigated OS, we evaluated RFS to clarify the true effect of adjuvant chemotherapy, as post-recurrence treatment affects OS. Adjuvant chemotherapy showed no survival benefit in the overall cohort. This was considered to be a product of selection bias, as adjuvant chemotherapy was administered for the more advanced tumors. The propensity-matched analysis demonstrated improved RFS when adjuvant chemotherapy was administered for > 6 months. Multivariate analysis indicated the favorable impact of administration for > 6 months. The exploratory subgroup analysis identified specific populations, including patients with SS or deeper tumors, positive lymph node metastasis, and preoperative elevated CA19-9 level, expected to benefit from adjuvant chemotherapy. Based on the data, > 6 months of adjuvant chemotherapy may be recommended for high-risk groups; however, the optimal regimen has not yet been established. The results from BALLAD (NCT02502370) and J-BALLAD (JCOG1502C) [30], ongoing open-label randomized controlled trials aiming to evaluate the benefit of three adjuvant chemotherapy regimens (infusional 5-FU/LV, FOLFOX, and capecitabine plus oxaliplatin) for resected small bowel adenocarcinoma, might help answer this question.
Our recommendations provide a tentative standard for non-ampullary duodenal cancer treatment. Nevertheless, this study had certain limitations. First, the study’s retrospective nature meant that selection bias, including differing treatment strategies at each institution, is inevitable. In fact, the actual rate of regional lymph node metastasis remains unclear, as sufficient dissection might not have been performed in certain cases. Second, the small number of patients meant that we could not evaluate neoadjuvant therapy, which is an important topic in contemporary cancer treatment. Third, the therapeutic efficacy of radiation for non-ampullary duodenal cancer was not evaluated because its use is less common in Japan than in western countries [31]. However, the large-scale data presented in this study may provide useful information when managing this rare disease in daily clinical practice.
In conclusion, this study suggests that PD should be the standard procedure for advanced tumors. Furthermore, adjuvant chemotherapy for > 6 months appears to significantly improve survival. Further multi-institutional investigations are necessary to verify these recommendations.
Abbreviations
- LR:
-
Local resection
- PD:
-
Pancreatoduodenectomy
- DG:
-
Distal gastrectomy
- is/M:
-
Tumor in situ or tumor confined to the lamina propria
- SM:
-
Tumor confined to the submucosa
- MP:
-
Tumor invasion of the muscularis propria
- SS:
-
Tumor invasion of the subserosa
- SE:
-
Tumor invasion that is contiguous to or penetrates the serosa and is exposed to the peritoneal cavity
- SI:
-
Tumor invasion of adjacent structures
- nos.:
-
Number of lymph node stations
- OS:
-
Overall survival
- RFS:
-
Recurrence-free survival
- HR:
-
Hazard ratio
- ASA:
-
American Society of Anesthesiologists
- CEA:
-
Carcinoembryonic antigen
- CA19-9:
-
Carbohydrate antigen 19-9
- CI:
-
Confidence interval
References
Buchbjerg T, Fristrup C, Mortensen MB. The incidence and prognosis of true duodenal carcinomas. Surg Oncol. 2015;24(2):110–6.
Aparicio T, Zaanan A, Mary F, et al. Small bowel adenocarcinoma. Gastroenterol Clin N Am. 2016;45(3):447–57.
Kato Y, Takahashi S, Kinoshita T, et al. Surgical procedure depending on the depth of tumor invasion in the duodenal cancer. Jpn J Clin Oncol. 2014;44(3):224–31.
Cloyd JM, Norton JA, Visser BC, et al. Does the extent of resection impact survival for duodenal adenocarcinoma? Analysis of 1,611 cases. Ann Surg Oncol. 2015;22(2):573–80.
Kohga A, Yamamoto Y, Sano S, et al. Surgical strategy for T1 duodenal or ampullary carcinoma according to the depth of tumor invasion. Anticancer Res. 2017;37(9):5277–83.
Rangelova E, Blomberg J, Ansorge C, et al. Pancreas-preserving duodenectomy is a safe alternative to high-risk pancreatoduodenectomy for premalignant duodenal lesions. J Gastrointest Surg. 2015;19(3):492–7.
Sakamoto T, Saiura A, Ono Y, et al. Optimal lymphadenectomy for duodenal adenocarcinoma: does the number alone matter? Ann Surg Oncol. 2017;24(11):3368–75.
Kaklamanos IG, Bathe OF, Franceschi D, et al. Extent of resection in the management of duodenal adenocarcinoma. Am J Surg. 2000;179(1):37–41.
Singhal N, Singhal D. Adjuvant chemotherapy for small intestine adenocarcinoma. Cochrane Database Syst Rev. 2007. https://doi.org/10.1002/14651858.CD005202.pub2.
Overman MJ, Kopetz S, Lin E, et al. Is there a role for adjuvant therapy in resected adenocarcinoma of the small intestine. Acta Oncol (Madr). 2010;49(4):474–9.
Ye X, Zhang G, Chen H, et al. Meta-analysis of postoperative adjuvant therapy for small bowel adenocarcinoma. PLoS ONE. 2018;13(8):1–12.
Li D, Si X, Wan T, et al. Outcomes of surgical resection for primary duodenal adenocarcinoma: a systematic review. Asian J Surg. 2019;42(1):46–52.
Meijer LL, Alberga AJ, de Bakker JK, et al. Outcomes and treatment options for duodenal adenocarcinoma: a systematic review and meta-analysis. Ann Surg Oncol. 2018;25(9):2681–92.
Cecchini S, Correa-Gallego C, Desphande V, et al. Superior prognostic importance of perineural invasion vs. lymph node involvement after curative resection of duodenal adenocarcinoma. J Gastrointest Surg. 2012;16(1):113–20.
Solaini L, Jamieson NB, Metcalfe M, et al. Outcome after surgical resection for duodenal adenocarcinoma in the UK. Br J Surg. 2015;102(6):676–81.
Jiang QL, Huang XH, Chen YT, et al. Prognostic factors and clinical characteristics of patients with primary duodenal adenocarcinoma: a single-center experience from China. Biomed Res Int. 2016. https://doi.org/10.1155/2016/6491049.
Sarela AI, Brennan MF, Karpeh MS, et al. Adenocarcinoma of the duodenum: importance of accurate lymph node staging and similarity in outcome to gastric cancer. Ann Surg Oncol. 2004;11(4):380–6.
Classification of pancreatic carcinoma fourth English Edition; 2017.
Clavien PA, Sanabria JR, Mentha G, et al. Recent results of elective open cholecystectomy in a North American and a European center. Comparison of complications and risk factors. Ann Surg. 1992;216(6):618–26.
Dindo D, Demartines N, Clavien P-A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Sasako M, McCulloch P, Kinoshita T, et al. New method to evaluate the therapeutic value of lymph node dissection for gastric cancer. Br J Surg. 1995;82(3):346–51.
Yamashita H, Seto Y, Sano T, et al. Results of a nation-wide retrospective study of lymphadenectomy for esophagogastric junction carcinoma. Gastric Cancer. 2017;20(s1):69–83.
Poultsides GA, Huang LC, Cameron JL, et al. Duodenal adenocarcinoma: clinicopathologic analysis and implications for treatment. Ann Surg Oncol. 2012;19(6):1928–35.
He J, Ahuja N, Makary MA, et al. 2564 resected periampullary adenocarcinomas at a single institution: trends over three decades. HPB. 2014;16(1):83–90.
Onkendi EO, Boostrom SY, Sarr MG, et al. 15-year experience with surgical treatment of duodenal carcinoma: a comparison of periampullary and extra-ampullary duodenal carcinomas. J Gastrointest Surg. 2012;16(4):682–91.
Bakaeen FG, Murr MM, Sarr MG, et al. What prognostic factors are important in duodenal adenocarcinoma? Arch Surg. 2000;135(6):632–5.
Gibbs JF. Duodenal adenocarcinoma: Is total lymph node sampling predictive of outcome. Ann Surg Oncol. 2004;11(4):354–5.
Ecker BL, McMillan MT, Datta J, et al. Efficacy of adjuvant chemotherapy for small bowel adenocarcinoma: a propensity score-matched analysis. Cancer. 2016;122(5):693–701.
Ecker BL, McMillan MT, Datta J, et al. Adjuvant chemotherapy versus chemoradiotherapy in the management of patients with surgically resected duodenal adenocarcinoma: a propensity score-matched analysis of a nationwide clinical oncology database. Cancer. 2017;123(6):967–76.
Kitahara H, Honma Y, Ueno M, et al. Randomized phase III trial of post-operative chemotherapy for patients with stage I/II/III small bowel adenocarcinoma (JCOG1502C, J-BALLAD). Jpn J Clin Oncol. 2019;49(3):287–90.
Lim YJ, Kim K. Effect of postoperative radiotherapy on survival in duodenal adenocarcinoma: a propensity score-adjusted analysis of surveillance, epidemiology, and end results database. Int J Clin Oncol. 2018;23(3):473–81.
Acknowledgements
We are grateful to the 114 Japanese institutions that took part in the survey. The order of these institutions listed below was determined according to the number of patients enrolled. Department of Gastroenterological Surgery, Cancer Institute Hospital, Japanese Foundation for Cancer Research; Division of Hepatobiliary and Pancreatic Surgery, Shizuoka Cancer Center; Department of Surgery, Kansai Medical University; Department of Surgery, Kinki University Faculty of Medicine; Department of Surgery, Institute of Gastroenterology, Tokyo Women’s Medical University; Department of Gastroenterological Surgery (Surgery II), Nagoya University Graduate School of Medicine; Department of General and Gastroenterological Surgery, Osaka Medical College; Second Department of Surgery, School of Medicine, Wakayama Medical University; Department of Gastrointestinal Surgery, Tenri Hospital; Department of Surgery, The Jikei University School of Medicine; Department of Surgery, Nara Medical University; Department of Gastroenterological Surgery, Toranomon Hospital; Department of Surgery, Graduate School of Biomedical & Health Sciences, Hiroshima University; Department of Gastroenterological Surgery, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences; Department of Surgical Oncology, Gifu University; Department of Surgery, Saitama Medical Center, Jichi Medical University; Department of Gastroenterological Surgery, Sendai Kousei Hospital; Division of Digestive and General Surgery, Niigata University Graduate School of Medical and Dental Sciences; Department of Surgery, Ehime Prefectural Central Hospital; Department of Gastroenterological Surgery, Graduate School of Life Sciences, Kumamoto University; Department of Gastroenterological Surgery II, Hokkaido University Graduate School of Medicine; Department of Gastroenterological and Pediatric Surgery, Oita University Faculty of Medicine; Department of Gastroenterological Surgery, Hyogo Cancer Center; Department of Surgery, Hokkaido Shokakika Hospital; Department of Gastroenterological Surgery, Ibaraki Prefectural Central Hospital; Department of Hepato‐Biliary‐Pancreatic Surgery, Osaka City General Hospital; Division of Hepatobiliary and Pancreatic Surgery, National Cancer Center Hospital East; Hepato‐Biliary‐Pancreatic Surgery Division, Department of Surgery, Graduate School of Medicine, University of Tokyo; Department of Gastroenterological Surgery, Hiroshima City Hiroshima Citizens Hospital; Department of Gastroenterological Surgery and Oncology, Kitano Hospital; Department of Surgery, Jichi Medical University; Department of Gastroenterological and General Surgery, School of Medicine, Showa University; Department of Gastroenterological Surgery, Osaka University Graduate School of Medicine; Department of General Surgery, Toyohashi Municipal Hospital; Department of Gastroenterological Surgery, Aichi Cancer Center Hospital; Department of Hepato‐Biliary‐Pancreatic Surgery, National Hospital Organization, Fukuyama Medical Center; Department of Surgery, Katsushika Medical Center, the Jikei University School of Medicine; Second Department of Surgery, Hamamatsu University School of Medicine; Department of Surgery, Kumamoto Regional Medical Center; Department of Digestive Surgery, Osaka International Cancer Institute; Department of Surgery, Toyonaka Municipal Hospital; Department of Surgery, Division of General and Gastroenterological Surgery, Toho University School of Medicine; Department of Surgery, Fujita Health University; Department of Surgery, Osaka Red Cross Hospital; Department of Surgery, Otsu Red Cross Hospital; Department of Surgery, Kitasato University School of Medicine; Department of Surgery, Kimitsu Chuo Hospital; Department of Hepatobiliary and Pancreatic Surgery, Graduate School of Medicine, Gunma University; Department of Surgery/Gastroenterological Surgery, Nagano Municipal Hospital; Department of Surgery, Hyogo College of Medicine; Department of Surgery, Oita Prefectural Hospital; Department of Surgery, Osaka Saiseikai Nakatsu Hospital; Department of Surgery, Okayama Saiseikai General Hospital; Department of Surgery, Kurume University School of Medicine; Department of Surgery, Kochi Medical School; Department of Surgery, Iwakuni Clinical Center; Department of Surgery, Southern TOHOKU General Hospital; Department of Surgery, Musashino Red Cross Hospital; Department of Surgery, Ogaki Municipal Hospital; Department of Gastroenterological Surgery, Fukuyama City Hospital; Department of Hepato‐Biliary‐Pancreatic Surgery, National Hospital Organization Kyushu Medical Center; Department of Surgery, National Hospital Organization, Kure Medical Center and Chugoku Cancer Center; Department of Surgery, Kobe City Medical Center General Hospital; Division of gastroenterological surgery, Saitama Cancer Center; Department of Surgery, The Jikei University School Daisan Hospital; Department of Hepatobiliary-Pancreatic Surgery, Tohoku University Graduate School of Medicine; Division of Hepato‐Biliary‐Pancreatic Surgery, Department of Surgery, University of Miyazaki Faculty of Medicine; Department of Surgery, JA Hiroshima General Hospital; Department of Gastroenterological Surgery, Kagawa University School of Medicine; Department of Surgery, Japanese Red Cross Kyoto Daiichi Hospital; Department of Hepato‐Biliary‐Pancreatic Surgery, Tochigi Cancer Center; Department of Hepato-Biliary-Pancreatic and Transplant Surgery, Fukushima Medical University; Department of Surgery, National Defense Medical College; Department of Surgery, Yamagata Prefectural Central Hospital; Department of Surgery, Yao Municipal Hospital; Department of Gastroenterological Surgery, Akita University Graduate School of Medicine; Department of Surgery, Iwate Medical University School of Medicine; Department of Surgery, National Hospital Organization, Osaka National Hospital; Department of Surgery, Kawasaki Municipal Hospital; Department of Surgery, Kyoto Katsura Hospital; Department of Surgery, Kyorin University School of Medicine; Department of Surgery, Keio University School of Medicine; Department of Surgery, Sakai City Medical Center; Department of Digestive and General Surgery, Faculty of Medicine, Shimane University; Department of Biliary‐Pancreatic Surgery, Fujita Health University Bantane Hospital; Department of Surgery, Toyama Prefectural Central Hospital; Department of Surgery, Iwaki City Medical Center; Department of Surgery, Kasugai Municipal Hospital; Department of Surgery, Kin-ikyo Chuo Hospital; Department of Surgery, Gunma Saiseikai Maebashi Hospital; Department of Gastroenterological Surgery, Saiseikai Suita Hospital; Department of Gastroenterological Surgery, Hakodate Municipal Hospital; Department of Gastroenterology, Shinshu University Graduate School of Medicine; Department of Surgery and Science, Graduate School of Medicine and Pharmaceutical Sciences, University of Toyama; Department of Gastroenterological Surgery, Nagoya City University Graduate School of Medical Sciences; Department of Gastroenterological Surgery, Hirosaki University School of Medicine; First Department of Surgery, Faculty of Medicine, University of Fukui; Department of Surgery, Matsuyama Red Cross Hospital; Department of Gastroenterological, Breast and Endocrine Surgery, Yamaguchi University Graduate School of Medicine; Department of Surgery, JA Onomichi General Hospital; Department of Surgery, Osaka Police Hospital; Department of Surgery, National Hospital Organization Nagasaki Medical Center; Department of Surgery, Nara Prefecture General Medical Center; Department of Surgery, Japanese Red Cross Maebashi Hospital; Department of Hepato‐Biliary‐Pancreatic Surgery and Transplantation, Ehime University Graduate School of Medicine; Department of Surgery, Hokkaido P.W.F.A.C. Sapporo Kosei General Hospital; Department of Surgery, Niigata Prefectural Central Hospital; Department of Surgery, Niigata Prefectural Shibata Hospital; Department of Surgery, Kansai Rosai Hospital; Department of Surgery Nagoya Central Hospital; Hepatobiliary‐Pancreatic and Transplant Surgery, Mie University Graduate School of Medicine; Department of Gastroenterological Surgery, Yokohama City University Graduate School of Medicine; First Department of Surgery, Yamagata University Graduate School of Medical Science; Department of Gastroenterological Surgery, Tokyo Medical University Ibaraki Medical Center. We also would like to express our sincere appreciation to the Japan Duodenal Cancer Guideline Committee and many doctors related to this research opportunity.
Funding
This work was supported by the Health and Labor Sciences Research Grant (grant number H29-GANTAISAKU-IPPAN-013). The funders had no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Author information
Authors and Affiliations
Consortia
Contributions
All authors equally took part in the conception of the study. KN drafted the manuscript. MS supervised the writing of the manuscript. All authors approved the final version of the manuscript and unanimously agreed to be accountable for all aspects of the work and to ensure that any questions related to the accuracy or integrity of any part of the report are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nakagawa, K., Sho, M., Okada, Ki. et al. Surgical results of non-ampullary duodenal cancer: a nationwide survey in Japan. J Gastroenterol 57, 70–81 (2022). https://doi.org/10.1007/s00535-021-01841-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-021-01841-9