Abstract
Purpose
The use of synthetic materials in emergency surgery for abdominal wall hernia in a potentially infected operating field has long been debated. In the present study, we evaluated the outcome of mesh prostheses in the management of incarcerated and strangulated abdominal wall hernias with or without organ resection.
Methods
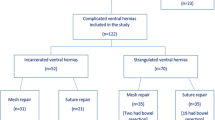
Between March 2012 and January 2020, medical records of 301 patients who underwent emergency surgery for incarcerated and strangulated abdominal wall hernias were retrospectively evaluated. The interventions were exclusively realized by two surgical teams, one of which used polypropylene mesh prostheses (group I), whereas the second team performed primary hernia repair (group II). The outcome of patients was observed for a mean follow-up period of 18.2 months. Categorical data were analyzed with the χ2 test or likelihood ratio. Logistic regression was used for adjustments in multivariate analysis. Statistical analyses were realized with SPSS, version 18. P values < 0.05 were considered statistically significant. For multiple comparisons between types of hernia, the significance level was set to P < 0.0083 according to Bonferroni adjustment.
Results
Of the 301 patients, 190 were men (63.1%), and 111 were women (36.9%). The mean age was 59,98 years (range 17–92). Overall, 226 (75.1%) patients were treated with synthetic mesh replacement. One hundred two organ resections (34%) were performed involving the omentum, small intestine, colon, and appendix. No significant difference was identified in terms of postoperative complications, between the two groups both in patients who underwent organ resection and in patients who did not.
Conclusion
Synthetic materials may safely be used in the emergency management of incarcerated and strangulated groin and abdominal wall hernias in patients with or without organ resection, although they cannot formally be recommended due to the limited number of cases of the present study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The beneficial outcomes of different types of abdominal wall hernias treated by prosthetic materials on an elective surgical basis have been well documented [1,2,3]. However, many patients remain undiagnosed or are reluctant to have surgical correction of their hernias. Neglected hernias may become incarcerated, which is defined as a hernia in which the content has become manually irreducible. A certain proportion of incarcerated cases may subsequently become complicated and strangulated. Strangulation occurs when the blood supply to the hernia content is compromised. Strangulation subsequently leads to ischemia, necrosis, perforation, or abscess formation, thus transforming a relatively simple surgical procedure into a highly challenging one.
The bacterial translocation in incarcerated or strangulated surgical site makes the use of prosthetic materials questionable. Their use in emergency surgery for abdominal incarcerated and strangulated hernias has been studied so far with conflicting results. Classic surgical teaching contraindicates the use of prosthetic repair in the setting of acute incarceration and/or strangulation for fear of prosthetic infection [4]. Some groups, however, have reported that incarcerated and strangulated hernias can be repaired safely with a prosthetic mesh [5,6,7,8].
Recently, the World Society of Emergency Surgery (WSES), aiming to provide evidence-based guidance, published recommendations for emergency repair of abdominal wall hernias in adults [9, 10]. These guidelines are mainly based on the classification of the Centers for Disease Control and Prevention (CDC) of the degree of wound contamination [11].
In the present study, the validity of mesh prostheses in the emergency surgical management of different types of incarcerated and strangulated abdominal wall hernias with or without organ resection was evaluated.
Material and methods
Between March 2012 and January 2020, medical records of 301 patients who underwent emergency surgery for incarcerated and strangulated abdominal wall hernias in Istanbul Training and Research Hospital were retrospectively evaluated. Incarcerated abdominal wall hernias like inguinal, umbilical, incisional, femoral, epigastric, and Spigelian hernias and strangulated hernias that required omentum, small intestine, colon, or appendix resection were included in the study.
The interventions were exclusively realized by two surgical teams, one of which used polypropylene (PP) mesh prostheses (group no. 1), whereas the second team performed uniquely primary hernia repair (group no. 2). Data for patient demographics, hernia type and content, length of the operation, type of repair, type of organ resection, mortality, hospital stay, postoperative complications, and late hernia recurrences were recorded.
All operations were performed under general anesthesia. One gram of cefazolin (first-generation cephalosporin) was administered intravenously in the OR.
Operative techniques
Primarily, the hernia sac was identified and explored. Protection of the operative field from contamination was realized by povidone-iodine and/or warm physiological saline-soaked towels. The contents of the hernia sac were assessed for viability and reduced into the abdomen if viable. In strangulated cases, when the contents were nonviable, warm saline-soaked towels were applied and the organ was re-accessed. If still not viable, the strangulated site of the organ was resected.
Small intestinal end-to-end anastomoses were performed using extramucosal 3/0 polyglycolic continuous suture and end-to-end large bowel anastomoses were performed using whole layer 3/0 polyglycolic interrupted sutures.
Inguinal hernias were either repaired by tension-free repair as described by Lichtenstein et al. [1, 2], using a polypropylene mesh (Prolene, Ethicon) and a 2/0 polypropylene interrupted suture to fix the mesh or herniorrhaphy was performed using Shouldice or Bassini methods. Femoral hernias were treated by a mesh plug repair of the femoral ring or herniorrhaphy was performed using the McVay method. Umbilical and incisional hernias were repaired using an onlay polypropylene mesh after closing the fascia underneath the mesh. In incisional hernias, the defect was vertically closed by simple interrupted non-absorbable sutures (Prolene no.1- Ethicon). 18 Fr suction drain was placed subcutaneously in patients with umbilical and incisional hernias whether an onlay mesh was used or not. Epigastric and Spigelian hernias were repaired either by simple fascial suture or by onlay mesh.
Postoperative course
Oral intake was allowed the evening of surgery. In patients who underwent resection, oral intake was deferred until the second or third postoperative day depending on the return of bowel peristalsis.
Patients with no evidence of ischemia received one gram of the first-generation cephalosporin intravenously in the OR for short-term prophylaxis. In patients with intestinal strangulation or in patients who underwent any organ resection (small bowel, colon, omentum, or appendix) , intravenous antibiotic therapy was continued up to the discharge day and then switched to oral antibiotics until the end of the first week.
The first follow-up visit occurred one week after discharge to check the wound and remove sutures. Drains were removed when the daily draining amount was less than 20 ml serous fluid. Subsequent follow-up examinations were realized after 1 month, 6 months, 1 year, and yearly thereafter. All patients had a physical examination and completed a questionnaire containing questions concerning recovery and pain after 1 month and 6 months. They were also instructed to visit the hospital if they experienced any symptoms of recurrent hernia. Twelve patients (eight of which were from the mesh group) were lost from follow-up before 1 month.
The endpoints of the present study were the rate of postoperative complications, operative time, mortality, hospital stay, and late hernia recurrence in patients managed by mesh repair or herniorrhaphy for incarcerated and strangulated abdominal wall hernias with or without organ resection.
Statistical analysis
Categorical data were analyzed with the χ2 test or Likelihood Ratio. Mantel-Haenszel stratified analysis was used for the adjustment of confounding variables. The correlation between categorical variables was analyzed with Kendall’s tau-b test. Logistic regression was performed by joining all the variables considered bivariates (as strata), and their effects on each other were adjusted.
P values <0.05 (2 sided) were considered statistically significant. The limit is set to P < 0.0083 with Bonferroni adjustment for multiple comparisons between hernia types.
Results
Of the 301 patients, 190 were men (63.1%), and 111 were women (36.9%). The mean age was 59.98 years. The mean age for men was 58.55 years, and for women was 62.43 years. Women were significantly older than men (p<0.05).
Overall 226 patients (75.1%) underwent hernia repair with a monofilament polypropylene mesh, whereas 75 (24.9%) patients underwent primary hernia repair. One hundred forty-one (46.8%) inguinal, 51 (16.9%) umbilical, 59 (19.6%) incisional, 40 (13.3%) femoral, 7 (2.3%) epigastric, and 3 (1%) Spigelian hernias were treated.
In terms of hernia type, there was a significant difference between both sexes. Inguinal hernias were significantly more frequent in men ((P < 0.05), whereas incisional and femoral hernias were significantly more frequent in women ((P< 0.05). Primary hernia repair was most frequently performed in umbilical hernias (P˂0.05). The distribution of hernia type and type of repair is given in Table 1.
Twenty-seven (9%) of the 301 hernias were recurrent and were most frequently inguinal (66.7%). Eighteen of inguinal (12.8%), four of umbilical (7.8%), four of incisional (6.8%), and one of the femoral hernias (2.5%) were recurrent hernias.
In terms of hernia content, no significant difference was found between inguinal, umbilical, femoral, and incisional hernias, although the small intestine was significantly more frequently encountered in epigastric hernias (P ˂0.05).
Strangulation was present in 102 (34%) patients. Organ resection was significantly more frequent in umbilical, femoral, and epigastric hernias (P˂0.001). The most frequently resected organs were the omentum and small intestine. Omentum and small intestine resections were performed in 65 (63.7%) and 32 (31.4%) patients, respectively (P˂0.05), without any significant distribution between different types of hernias (P=0.380). No significant difference was found according to type of hernia and type of repair in patients who underwent organ resection or not (P=0,124 and P=0.400 respectively).
Concerning the operative time, no significant difference was found according to a hernia type and repair type (P =0.187).
Surgical site infections (SSI) (n =26 or 8.6%), seromas (n =19 or 6.3%), and hematomas (n =13 or 4.3%) were the most frequently encountered postoperative complications (Table 2). The wound infections were superficial and were successfully managed with drainage and local wound care. There was no statistically significant difference between patients in the mesh group and primary repair group in terms of postoperative complications (p =0.134).
In univariate analysis, the presence of mesh appears to be effective, with a borderline meaningless (p=0.067), emphasizing that the use of mesh may reduce the possible complication outcome by half (OR = 0.57).
The complication rates were evaluated according to the hernia type (by removing the epigastric and Spiegelian hernias with few samples). There was no significant difference between hernia types in terms of complication rate (p = 0.119).
To adjust the effects of the confounding factors and to analyze the effect of mesh on complications within hernia types (inguinal, femoral, umbilical, and incisional), we used Mantel-Heanszel stratified analysis (Yes/No), and adjusted the “P” values according to Bonferroni approach. Assuming six different comparisons for four types of locations (inguinal, femoral, umbilical, and incisional), the significance level was adjusted to P<0.0083 ( 0.05/6). No significant results were obtained concerning the effect of mesh on complications between hernia types.
No significant relationship was found between types of hernia and types of complications (P=*0.898).
In terms of postoperative complications, there was no significant relationship between patients who underwent resection or not (p=0.480). With a mean follow-up of 15.3 months (5 patients died after small bowel resection), in patients who underwent small intestinal resection, only one from the mesh group developed a surgical site infection.
A subgroup analysis was performed by grouping groin hernias (the femoral and inguinal hernias) together against ventral hernias (the incisional and umbilical hernias). In terms of postoperative complications, no significant difference was found between the two groups in patients who underwent resection or not.
There were two anastomotic leakages. These patients underwent primary repair of umbilical and femoral hernias with small intestinal resection-anastomosis. One patient died in ICU whereas the second patient was treated with Miculicz stoma. Nine of the eleven (3.7%) patients who died in the early postoperative period were over 75 years who had one or more concomitant disease such as chronic obstructive pulmonary disease, diabetes, hypertension, obesity, or other. All patients had organ resections. Four patients were operated upon for inguinal hernias with strangulation of the small intestine and had intestinal resection with immediate restoration of the intestinal continuity by end-to-end anastomosis (3 mesh, 1 non-mesh repair). One patient with a strangulated umbilical hernia underwent concommitant small intestinal and colon resection with end-to-end anastomosis. Six patients (three incisional, two umbilical, and one inguinal hernia) had omentum resection. The major causes of death were pneumonia, myocardial infarction, peritonitis, and sepsis with multiorgan failure.
Early recurrence was encountered in one patient and in two patients in group I and group II, respectively. The patient in group I was treated for strangulated incisional hernia with small intestinal resection-anastomosis and onlay mesh repair. Both patients in group II underwent primary repair for incarcerated inguinal hernia.
Mean hospital stay was 3.50 days (min. 1max. 11). The hospital stay was significantly longer in women, whether or not organ resection was performed (P˂0.05). Also, patients with primary repair stayed longer (P ˂0.05). The hospital stay was significantly longer in umbilical and incisional hernias (P ˂0.05).
The mean follow-up period was 18.2 months. The longest follow-up term was 42 months and the shortest was 1 month. The follow-up rates were 06 months = 11%, 612 months = 43%,
1-2 y = 25%, and 2-3 y = 21%.
An eighty-year-old man who underwent omentum resection with mesh plug repair for femoral hernia, presented with groin abscess due to mesh reaction 2 years after the first operation. The mesh had to be removed in this patient.
We had six inguinal (four in the mesh group and two in the non-mesh group; 4.23% of total inguinal hernias), four umbilical (one in the mesh group and three in the non-mesh group; 7.8% of total umbilical hernias), and four incisional (two in the mesh group and two in the non-mesh group; 6.8% of total incisional hernias) late hernia recurrences.
One patient initially treated for strangulated umbilical hernia with small intestine resection underwent two additional operations for incarceration 1 year and 2 years after the initial operation. One patient initially operated upon for incarcerated inguinal hernia presented with small intestine strangulation 2 months after the initial operation. One patient who was initially operated upon for an incarcerated umbilical hernia presented with small intestine strangulation 1 year after the initial operation.
Discussion
Abdominal wall hernias have longtime been successfully treated by prosthetic materials in elective surgery [1,2,3]. However, their use in emergency surgery for prosthetic repair of incarcerated or strangulated hernias is debated. Classic surgical teaching used to contraindicate the use of synthetic materials in potentially infected surgical fields, arguing that these materials were more susceptible to surgical field infection [4]. On the other hand, there has been growing evidence that Lichtenstein hernioplasty can be safely performed for strangulated groin hernias, with good short-term and intermediate-term outcomes [6, 7]. Some studies found a low incidence of wound infections in acute hernia repaired with prosthetic mesh in contaminated areas [7, 8]. The surgeon has to choose between a higher risk of surgical site infection when a synthetic mesh is used and a higher incidence of recurrence rate when the mesh is abandoned [12].
Recently, in 2017, Birindelli et al. published the recommendations of the World Society of Emergency Surgery (WSES) for emergency repair of abdominal wall hernias in adults [9], which was updated in 2020 [10]. These guidelines are mainly based on the classification of Centers for Disease Control and Prevention (CDC) of the degree of wound contamination[11]. WSES recommends prosthetic repair in a “clean surgical field” for patients with intestinal incarceration and no signs of intestinal strangulation or concurrent small bowel resection (clean surgical field-CDC wound class I) (grade 1A recommendation). Emergent hernia repair with a synthetic mesh can also be performed in intestinal strangulation and/or concomitant small bowel resection without gross enteric spillage (clean-contaminated surgical field-CDC wound class II) with low risk of recurrence (grade 1A recommendation). For stable patients with strangulated hernia with small bowel necrosis and/or gross enteric spillage during intestinal resection (contaminated, CDC wound class III) or peritonitis from small bowel perforation (dirty surgical field, CDC wound class IV), the primary repair is recommended when the size of the defect is small (< 3 cm); when the direct suture is not feasible, a biological mesh may be used for repair (grade 2C recommendation).
In the present study, patients who underwent emergency surgery for incarcerated and strangulated groin and abdominal wall hernias treated with and without synthetic grafts were investigated. The comparison of the two groups revealed no statistically significant difference in terms of postoperative complications both in incarcerated and strangulated hernias. These findings were in accordance withrecent reviews stating similar findings [9, 13].
A subgroup analysis between the groin and ventral hernias, in terms of postoperative complications, found no significant difference between the two groups, both in patients who underwent resection and not.
Our patients with no evidence of ischemia received one gram of the first-generation cephalosporin intravenously in the OR for short-term prophylaxis. WSES guidelines recommend short-term antibiotic prophylaxis in patients with intestinal incarceration with no evidence of ischemia and no bowel resection (CDC wound class I-grade 2C recommendation) [10]. In patients with intestinal strangulation and/or concurrent resection of any organ, including omentum, small bowel, or large bowel (CDC wound classes II and III), 48-h antimicrobial prophylaxis is recommended (grade ‘C recommendation) [10]. In our study, patients with intestinal strangulation and patients who underwent any organ resection (small bowel, colon, omentum, or appendix) received intravenous antibiotic therapy which was continued up to the discharge day and then switched to oral antibiotics until the end of the first week. Without a control group, this treatment cannot be recommended in current practice due to cost, side effects, and the development of resistance.
Different pathophysiologic mechanisms have been proposed to explain the development of specific infectious complications. Surgical site infection (SSI) is significantly facilitated by the presence of adhesions and hematomas, the advanced age of 60-70 years old, a length of surgery of over 90 min, a hernia duration of over 24 months, obesity, and organ functional deterioration [14]. Intravascular catheters and urinary catheters are the two most common causes of nosocomially acquired bloodstream infections.
Chronic mesh infections are responsible for high morbidity, high cost, and long-term risk of chronic SSI of 2.1% [15]. The conventional view suggested that using synthetic mesh would increase the chance of SSI and mesh-related complications [16, 17]. In late or chronic infections the infected mesh can hardly be salvaged. Indeed, 4.5% of mesh removals are made necessary by infection [18]. Some suggest that complete mesh removal is required if we hope to achieve healing. [19, 20].
Three types of meshes are the most used: polypropylene, polyester, and polytetrafluoroéthylen (ePTFE)-based meshes. Pain, seroma, and persisting infection were established as mesh-related complications and seem to be associated with small pore-sized, heavy-weight meshes [21]. To improve the functional outcomes and decrease the mesh infection rates, large pore-sized, light meshes were developed. A study compared the outcomes between PP, PET, and ePTFE meshes demonstrated a significantly greater incidence of entero-cutaneous fistula formation, mesh infections, and recurrences with multifilament PET mesh when compared with other materials [22]. When PTFE meshes get infected, the prostheses have to be removed.
On the contrary, some authors claim that SSI does not result in prosthetic mesh infection. Throughout the 10-year duration of their study, Bessa et al. have found no evidence to support the concept that the presence of acute incarceration, strangulation, or wound infection results in polypropylene mesh infection [23, 24].
In our study, twenty-six surgical site infections were encountered and were managed by antibiotics and dressings. One patient who initially underwent omentum resection with mesh plug repair for femoral hernia, presented with a groin abscess 2 years after the initial operation. Mesh removal was required to facilitate the cessation of the groin infection in this patient.
Another important risk factor for SSI is the presence of small bowel or large bowel obstruction or necrosis. Many surgeons are still afraid of an increased rate of surgical site infection could be associated with mesh implantation in the setting of incarcerated and strangulated bowel loops [23, 25]. These operations are more likely to be performed emergently and are considered “clean-contaminated or “contaminated” rather than “clean” surgeries.
There is no consensus on the use of prostheses in the potentially infected operating field [8]. Some authors claim that the presence of a nonviable intestine cannot be considered a contraindication to the use of a prosthetic repair [4, 6, 8, 26]. Pans et al. reported no wound infection in 9 patients (25.7%) who had small bowel resection followed by the implantation of a pre-peritoneal mesh [4]. On the contrary, Nieuwenhuizen et al. reported high wound infection rates in patients requiring intestinal resection [23].
In our series, strangulation was present in 102 (34%) patients. The incidence of patients who underwent resection was significantly more frequent in umbilical, femoral, and epigastric hernias (P ˂0.001). The most frequently resected organs were the omentum and small intestine, without any significant distribution according to different types of hernias. No significant relationship was found between the type of hernia and type of repair in patients who underwent organ resection or not. In terms of postoperative complications, there was no significant relationship between patients who underwent resection and not (P =0.480).
Concerning the operative time, we found no significant difference according to the hernia type and repair type.
We had thirty-two patients who underwent resection with immediate anastomosis of the nonviable small intestine. Seventeen patients were treated by mesh repair and fifteen patients by a simple repair. We found no significant relationship in terms of postoperative complications, between patients who underwent resection and not. With a mean follow-up of 15.3 months (5 patients died after small bowel resection), in patients who underwent small intestinal resection, only one from the mesh group developed a surgical site infection. It is impossible to draw a definite conclusion from the presented data due to the limited number of cases. The retrospective nature and the small study size are important limitations of this work, concerning a rare condition. The use of mesh after resection of the strangulated colon is still controversial and cannot generally be recommended.
Eleven (3.7%) patients died in the early postoperative period. Nine of the eleven patients were over 75 years. They all had one or more concomitant disease. All had organ resections. Five patients underwent small intestinal (one patient underwent concomitant small intestine and colon resection) resection, and omentum resections were performed in six patients. The major causes of death were pneumonia, myocardial infarction, peritonitis, and sepsis with multiorgan failure. Azari et al. and Compagna et al. reported an increased mortality rate in elderly patients over 80 [27, 28].
The recurrence following an emergency hernioplasty for incarcerated inguinal hernia seems to be lower than that reported for emergency herniorrhaphy, which ranges from 6.2 to 14.3 % [29, 30]. Late hernia recurrence can be associated with increased intra-abdominal pressure, progressive weakness of the abdominal wall, mesh shrinkage, and abnormal collagen metabolism [31]. Our late recurrence rate for inguinal hernia, umbilical hernia, and incisional hernia was 4.23, 7.8, and 6.8%.
Conclusion
Our findings support the use of prosthetic materials in the emergency management of the incarcerated abdominal wall hernias. The use of prosthetic materials may be taken into consideration in the management of strangulated abdominal wall hernias as well, in patients either with or without organ resection. We cannot formally recommend it though, due to the limited number of cases that do not allow us to draw a definite conclusion. Equally, the use of mesh after resection of the strangulated colon is still controversial and cannot generally be recommended.
Finally, we think that the present study adds supportive evidence to WSES guidelines for emergency repair of abdominal wall hernias in adults.
References
Lichtenstein IL, Shulman AG, Amid PK, Montllor MM (1989) The tension-free hernioplasty. Am J Surg 157:188–193
Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J et al (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia. 13:343–403
Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J (2004) Longterm follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240:578–583
Pans A, Desive C, Jacquet N (1997) Use of a preperitoneal prosthesis for strangulated groin hernia. Br J Surg 84:310–312
D’Ambrosio R, Capasso L, Sgueglia S, Iarrobino G, Buonincontro S, Carfora E, Borsi E (2004) The meshes of polypropylene in emergency surgery for strangulated hernias and incisional hernias. Ann Ital Chir 75(5):569–573
Wysocki A, Kulawik J, Pozniczek M, Strzalka M (2006) Is the Lichtenstein operation of strangulated groin hernia a safe procedure? World J Surg 30:2065–2070
Bessa SS, Katri KM, Abdel-Salam WN, Abdel-Baki NA (2007) Early results from the use of the Lichtenstein repair in the management of strangulated groin hernia. Hernia. 11(3):239–242
Lohsiriwat V, Sridermma W, Akaraviputh T, Boonnuch W, Chinsawangwatthanakol V, Methasate A et al (2007) Surgical outcomes of Lichtenstein tension-free hernioplasty for acutely incarcerated inguinal hernia. Surg Today 37(3):212–214
Birindelli A, Sartelli M, Di Saverio S, Coccolini F, Ansaloni L, van Ramshorst GH, Campanelli G, Khokha V, Moore EE, Peitzman A, Velmahos G, Moore FA, Leppaniemi A, Burlew CC, Biffl WL, Koike K, Kluger Y, Fraga GP, Ordonez CA, Novello M, Agresta F, Sakakushev B, Gerych I, Wani I, Kelly MD, Gomes CA, Faro MP Jr, Tarasconi A, Demetrashvili Z, Lee JG, Vettoretto N, Guercioni G, Persiani R, Tranà C, Cui Y, Kok KYY, Ghnnam WM, Abbas AE, Sato N, Marwah S, Rangarajan M, Ben-Ishay O, Adesunkanmi ARK, Lohse HAS, Kenig J, Mandalà S, Coimbra R, Bhangu A, Suggett N, Biondi A, Portolani N, Baiocchi G, Kirkpatrick AW, Scibé R, Sugrue M, Chiara O, Catena F. 2017 update of the WSES guidelines for emergency repair of complicated abdominal wall hernias. World J Emerg Surg 2017;12-37.
De Simone B, Birindelli A, Ansaloni L, Sartelli M, Coccolini F, Di Saverio S (2020) Emergency repair of complicated abdominal wall hernias: WSES guidelines. Hernia. 24:359–368
Garner J (1986) CDC guideline for prevention of surgical wound infections. Infect Control 7(3):193–200
Emile SH, Elgendy H, Sakr A, Gado WA, Aly A et al (2017) Outcomes following repair of incarcerated and strangulated ventral hernias with or without synthetic mesh. World J Emerg Surg 12-31
Lockhart K, Dunn D, Teo S, Ng JY, Dhillon M, Teo E, van Driel ML (2018) Mesh versus non-mesh for inguinal and femoral hernia repair. Cochrane Database Syst Rev 9(9):CD011517
Praveen S, Rohaizak M (2009) Local antibiotics are equivalent to intravenous antibiotics in the prevention of superficial wound infection in inguinal hernioplasty. Asian J Surg 32:59–63
Kokotovic D, Bisgaard T, Helgstrand F (2016) Long-term recurrence and complications associated with elective incisional hernia repair. JAMA. 316(15):1575
Nilsson H, Nilsson E, Angeras U, Nordin P (2011) Mortality after groin hernia surgery: delay of treatment and cause of death. Hernia. 15:301–307
Burcharth J (2014) The epidemiology and risk factors for recurrence after inguinal hernia surgery. Dan Med J 61(5):B4846
Hawn MT, Snyder CW, Graham LA et al (2010) Long-term follow-up of technical outcomes for incisional hernia repair. J Am Coll Surg (5):648–657
Chung L, Tse GH, O’Dwyer PJ (2014) Outcome of patients with chronic mesh infection following abdominal wall hernia repair. Hernia. 18(5):701–704
Bueno-Lledó J, Torregrosa-Gallud A, Carreño-Saénz O et al (2016) Partial versus complete removal of the infected mesh after abdominal wall hernia repair. Am J Surg 214:47–52
Conze J, Krones CJ, Schumpelick V et al (2007) Incisional hernia: challenge of re-operations after mesh repair. Langenbeck's Arch Surg 392:453–457
Gilbert AI, Graham MF (1997) Infected grafts of incisional hernioplasties. Hernia. 1(2):77–81
Nieuwenhuizen J, Van Ramshorst GH, ten Brinke JG, de Wit T, van der Harst E, Hop WC, Jeekel J, Lange JF (2011) The use of mesh in acute hernia: frequency and outcome in 99 cases. Hernia. 15(3):297–300
Bessa SS, Abdel-fattah MR, Al-Sayes IA, Korayem IT (2015) Results of prosthetic mesh repair in the emergency management of the acutely incarcerated and/or strangulated groin hernias: a 10-year study. Hernia. 19:909–914
Kaoutzanis C, Leichtle SW, Mouawad NJ, Welch KB, Lampman RM, Cleary RK (2013) Postoperative surgical site infections after ventral/incisional hernia repair: a comparison of open and laparoscopic outcomes. Surg Endosc 27:2221–2230
Campanelli G, Nicolsi FM, Pettinari D, Avesani EC (2004) Prosthetic repair, intestinal resection, and potentially contaminated areas: safe and feasible? Hernia. 8:190–192
Azari Y, Perry Z, Kirshtein B (2015) Strangulated groin hernia in octogenarians. Hernia. 19:443–447
Compagna R, Rossi R, Fappiano F, Bianco T, Accurso A, Danzi M et al (2013) Emergency groin hernia repair: implications in elderly. BMC Surg 13:29–32
Elsebae MM, Nasr M, Said M (2008) Tension-free repair versus Bassini technique for strangulated inguinal hernia: a controlled randomized study. Int J Surg 6:302–305
Brasso K, Londal Nielsen K, Christiansen J (1989) Long-term results of surgery for incarcerated groin hernia. Acta Chir Scand 155:583–585
Jansen PL, Klinge U, Jansen M, Junge K (2009) Risk factors for early recurrence after inguinal hernia repair. BMC Surg 9:18
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Ethical approval was waived by the local Ethics Committee of Istanbul Training and Research Hospital, in view of the retrospective nature of the study and all the procedures being performed were part of the routine care.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tomaoglu, K., Okmen, H. Prosthetic mesh hernioplasty versus primary repair in incarcerated and strangulated groin and abdominal wall hernias with or without organ resection. Retrospective study. Langenbecks Arch Surg 406, 1651–1657 (2021). https://doi.org/10.1007/s00423-021-02145-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-021-02145-5