Abstract
Background
The purpose of this study was to compare the incidence of postoperative surgical site infections (SSIs), operative times (OTs), and length of hospital stay (LOS) after open and laparoscopic ventral/incisional hernia repair (VIHR) using multicenter, prospectively collected data.
Methods
The incidence of postoperative SSIs, OTs, and LOS was determined for cases of VIHR in the American College of Surgeons’ National Surgical Quality Improvement Program database in 2009 and 2010. Open and laparoscopic techniques were compared using a propensity score model to adjust for differences in patient demographics, characteristics, comorbidities, and laboratory values.
Results
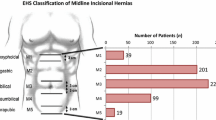
A total of 26,766 cases met the inclusion criteria; 21,463 cases were open procedures (reducible, n = 15,520 [72 %]; incarcerated/strangulated, n = 5,943 [28 %]), and 5,303 cases were laparoscopic procedures (reducible, n = 3,883 [73 %]; incarcerated/strangulated, n = 1,420 [27 %]). Propensity score adjusted odds ratios (ORs) were significantly different between open and laparoscopic VIHR for reducible and incarcerated/strangulated hernias with regard to superficial SSI (OR 5.5, p < 0.01 and OR 3.1, p < 0.01, respectively), deep SSI (OR 6.9, p < 0.01, and OR 8.0, p < 0.01, respectively) and wound disruption (OR 4.6, p < 0.01 and OR 9.3, p = 0.03, respectively). The risk for organ/space SSI was significantly greater for open operations among reducible hernias (OR 1.9, p = 0.02), but there was no significant difference between the open and laparoscopic repair groups for incarcerated/strangulated hernias (OR 0.8, p = 0.41). The OT was significantly longer for laparoscopic procedures, both for reducible (98.5 vs. 84.9 min, p < 0.01) and incarcerated/strangulated hernias (96.4 vs. 81.2 min, p < 0.01). LOS (mean, 95 % confidence interval) was significantly longer for open repairs for both reducible (open = 2.79, 2.59–3.00; laparoscopic = 2.39, 2.20–2.60; p < 0.01) and incarcerated/strangulated (open = 2.64, 2.55–2.73; laparoscopic = 2.17, 2.02–2.33; p < 0.01) hernias.
Conclusions
Laparoscopic VIHR for reducible and incarcerated/strangulated hernias is associated with shorter LOS and decreased risk for superficial SSI, deep SSI, and wound disruption, but longer OTs when compared to open repair.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In the United States, it is estimated that over 400,000 patients undergo treatment for ventral or incisional hernias each year, a number that continues to increase annually [1]. Incisional hernias are a common complication after abdominal surgery, with a reported incidence of 3–13 % [2–4]. The incidence increases up to 80 % for those who develop wound infections [5–7]. The clinical and economic burden of these hernias is substantial and ranges from discomfort or pain to bowel obstruction or incarceration, and even death. Surgical intervention is the only potentially curative approach. These data imply that many patients undergoing any type of abdominal operation will require additional surgical intervention to repair a resultant incisional hernia. Taking into consideration the morbidity and costs related to ventral/incisional hernia repairs (VIHRs), it becomes apparent that the efficacy of repair techniques is crucial and is among the most vexing of all hernia surgeries [8].
Several techniques and technologies have been developed for the repair of ventral/incisional hernias. Yet there is still controversy as to which is the optimal treatment approach for repair of such hernias, and recurrence rates remain unacceptably high. The insertion of a prosthetic material to strengthen the abdominal wall allows for a tension-free repair, but such repairs are still associated with a significant recurrence rate ranging between 2 and 36 % [9–11]. A randomized, multicenter study demonstrated that nearly half of all primary repairs and one-fourth of mesh repairs fail within 3 years [7]. Moreover, the use of prosthetic material carries the risk of severe wound complications, which itself is an independent risk factor for hernia recurrence and further morbidity [7].
In 1993, LeBlanc and Booth first described the laparoscopic approach for ventral hernia repair with insertion of an intraperitoneal expanded polytetrafluoroethylene (ePTFE) mesh without closing the fascial gap [12]. Since then, the laparoscopic repair has become an acceptable yet underutilized alternative to open repair. A recent meta-analysis of 10 published randomized, controlled trials comparing the open to laparoscopic approach demonstrated fewer wound infections with laparoscopy [13]. Many of these studies, however, have a rather small number of participants and might not have been adequately powered to determine the morbidity of open VIHR compared to laparoscopic repair.
To avoid the high costs associated with a randomized, controlled trial including thousands of patients, we queried the prospectively collected multicenter American College of Surgeons’ National Surgical Quality Improvement Program (ACS-NSQIP) database to compare the incidence of postoperative surgical site infections (SSIs) between open and laparoscopic VIHR. Our aim was to specifically determine outcomes for reducible and incarcerated/strangulated hernia subgroups separately. We also compared operative times (OTs) and the impact of the two techniques on length of hospital stay (LOS).
Materials and methods
The ACS-NSQIP database was queried for cases of VIHRs in 2009 and 2010, a time period when both surgical techniques were in common use. The ACS-NSQIP is a large, rigorously maintained database recording more than 135 variables, including preoperative risk factors, intraoperative occurrences, and 30-day postoperative outcomes for patients undergoing major surgical procedures in both the inpatient and outpatient setting. Data are recorded by trained and certified clinical nurse reviewers at each participating hospital, and the ACS-NSQIP has been validated and proven to be a reliable, comprehensive tool for quality improvement [14]. Cases were sampled by Current Procedural Technology (CPT) codes for open hernia repairs (49560, 49561, 49565, 49566) and laparoscopic hernia repairs (49654, 49655, 49656, 49657). Separate analyses were performed for reducible and incarcerated/strangulated hernias. The institutional review board at the Saint Joseph Mercy Health System approved this study.
Exclusion criteria included age under 18 years, current pregnancy, involvement in trauma, American Society of Anesthesiology classification of 5 and 6, presence of systemic inflammatory response syndrome, severe sepsis or septic shock within 48 h before the index operation, and the presence of preoperative open wounds, with or without infection.
Outcomes of interest were OTs, and all types of postoperative wound occurrences including superficial SSI, deep SSI, organ/space SSI, and wound disruption. The definitions for these categories were based on Centers for Disease Control and Prevention and ACS-NSQIP terminology. LOS, defined as the day of discharge minus the day of operation, was also examined.
Thirty-seven risk factors were included in our statistical model, comparing the 30-day outcomes for open versus laparoscopic VIHR including emergent surgery, initial or recurrent hernia, inpatient or outpatient procedure, demographic characteristics, general health factors, comorbidities, preoperative laboratory values, and intraoperative factors (Table 1). Patient demographics included age, gender (male/female), ethnicity (white, African American), and body mass index. General health factors included tobacco use (defined as smoking history within 1 year before the index operation), alcohol use (defined as more than 2 drinks per day within 2 weeks before admission to the hospital for the index operation), functional health status before surgery (independent, partially/totally dependent), American Society of Anesthesiology class (1–4), and surgery within 30 days of the index operation. Comorbidities included diabetes mellitus (non-insulin-dependent or insulin-dependent), pulmonary (chronic obstructive pulmonary disease, moderate dyspnea, or dyspnea at rest), hypertension requiring medications, cardiovascular (angina within the month before the index operation, myocardial infarction within 6 months before the index operation, congestive heart failure within 30 days before the index operation, history of percutaneous coronary intervention, history of cardiac surgery), peripheral vascular disease (claudication, rest pain, or gangrene, history of revascularization or amputation for peripheral vascular disease), renal failure (acute renal failure, renal failure requiring dialysis), ascites, disseminated cancer, chemotherapy or radiotherapy for malignancy within 30 days of the index operation, chronic steroid use, loss of more than 10 % of body weight in the 6 months before the index operation, bleeding disorders, and cerebrovascular events (history of transient ischemic attack, cerebrovascular accident with or without neurologic deficit, hemiplegia, paraplegia, quadriplegia, impaired sensorium). Level of residency supervision was an intraoperative risk factor. All the above listed risk factors, except age, were included as discrete categories. For preoperative laboratory variables, abnormal values were defined as white blood count <4.5 or >11.0 × 103/μL, hematocrit <38 or >45 %, platelet count <150 or >400 × 103/μL, blood urea nitrogen >40 mg/dL, creatinine >1.2 mg/dL, mean serum albumin <3.2 gm/dL, serum total bilirubin >1.0 mg/dL, alkaline phosphatase >125 IU/L, aspartate aminotransferase >40 IU/L, international normalized ratio >1.5, and partial thromboplastin time >35 s.
Initial comparisons of the risk factors for the open and laparoscopic VIHR groups were made by the Pearson χ2 test or Fisher’s exact test where appropriate for categorical variables, and independent-sample t tests for continuous variables (i.e., age).
Initial unadjusted odds ratios (ORs) comparing open versus laparoscopic repair were calculated for any postsurgical wound infection combined (any occurrence of superficial, deep, or organ/space SSI, or wound disruption) by logistic regression. Separate unadjusted comparisons of the incidence of each type of wound occurrence for open versus laparoscopic surgery were also executed by logistic regression. Because of the skewed nature of LOS (75 % of patients had a LOS of 3 days or less; maximum was 120 days), comparisons of LOS for the two surgery types were made by a negative binomial regression model [15].
A propensity score analysis was used to adjust for the differences between patients undergoing open or laparoscopic repair, and to allow for a more unbiased comparison between patients in these two surgical groups. To implement the propensity score model, the probability of undergoing hernia repair via open or laparoscopic technique was estimated for each patient by a multivariate logistic regression model based on the 37 risk factors described above (Table 1). To assess the effectiveness of the propensity score method in producing comparable groups for the two types of surgery, the balance between patient characteristics in the open and laparoscopic repair groups was estimated controlling for propensity score quintile.
Propensity score–adjusted comparisons between the two groups were calculated by fitting a logistic regression model, stratifying on propensity score quintile, and including any covariates that were still unbalanced between the two groups. The propensity score–adjusted ORs comparing the two groups were calculated for each of the wound infection outcomes and mean LOS.
Categorical risk factors were expressed in absolute numbers and percent in each category. Continuous variables, such as age, were expressed as arithmetic mean ± standard deviation. Because of its skewed nature, the LOS was expressed as geometric mean ± 95 % confidence interval (CI). Wound occurrences were expressed as number and percentage for each repair method in the subgroups of reducible and incarcerated/strangulated cases. Statistical significance for all analyses was indicated by a p value of 0.05 or less. Analyses were performed by SAS software for Windows, release 9.2.
Results
For the years 2009 and 2010, a total of 28,269 cases of open and laparoscopic VIHR were listed in the ACS-NSQIP database, with 26,766 cases (94.7 %) meeting our inclusion criteria. Patient demographics and other characteristics are listed in Table 2. Open surgery was performed in 21,463 cases, 15,520 (72.3 %) of which had been classified as reducible, and 5,943 (27.7 %) of which had been classified as incarcerated/strangulated. Laparoscopic surgery was performed in 5,303 cases, 3,883 (73.2 %) of which had been classified as reducible, and 1,420 (26.8 %) of which had been classified as incarcerated/strangulated. Patient characteristics initially differed significantly between the two groups in 16 of 37 covariates for the reducible hernias, and in 21 of 37 covariates for the incarcerated/strangulated hernias (Table 1). For incarcerated/strangulated cases, propensity score stratification was successful in eliminating all differences between the two groups, and for reducible hernias only a single significant difference remained (emergency status of operation) between the two surgery types (Table 1). Therefore, analyses for the reducible hernia subgroup included emergency surgery status as a predictor, along with surgery type, after stratifying on propensity score quintile.
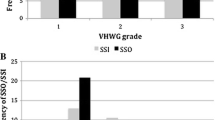
In propensity score analysis of reducible hernias, we found that the risk for all four types of wound occurrences was significantly greater for open than for laparoscopic repairs after adjusting for propensity score quintile (Table 3). Specifically, the odds of an adverse event were 5.5 times greater for superficial SSI (OR 5.5, 95 % CI 3.6–8.4, p < 0.01), 6.9 times greater for deep SSI (OR 6.9, 95 % CI 3.0–15.6, p < 0.01), 4.5 times greater for wound disruption (OR 4.5, 95 % CI 1.8–11.0, p < 0.01), and 1.9 times greater for organ/space SSI (OR 1.9, 95 % CI 1.1–3.3, p = 0.02). For incarcerated/strangulated hernias, the risk of superficial SSI, deep SSI, and wound disruption was also significantly higher for open compared to laparoscopic operations after adjusting for propensity score quintile. Specifically, the odds of an adverse event were 3.1 times greater for superficial SSI (OR 3.1, 95 % CI 1.9–5.2, p < 0.01), 7.9 times greater for deep SSI (OR 7.9, 95 % CI 2.5–25.4, p < 0.01) and 9.3 times greater for wound disruption (OR 9.3, 95 % CI 1.3–67.8, p = 0.03). There was no significant difference between the open and laparoscopic groups for incarcerated/strangulated cases with regard to organ/space SSI (OR 0.80, 95 % CI 0.4–1.5, p = 0.41).
After adjusting for propensity score quintile, the mean LOS was significantly longer for open than for laparoscopic repairs, which was true for both reducible hernias (open: OR 2.70, 95 % CI 2.59–3.00; laparoscopic: OR 2.39, 95 % CI 2.20–2.60; p < 0.01), and incarcerated/strangulated hernias (open: OR 2.64, 95 % CI 2.55–2.73; laparoscopic: OR 2.17, 95 % CI 2.02–2.33; p < 0.01).
When comparing the OT between open and laparoscopic operations, only cases with a duration of more than 20 min and less than 240 min were included in an attempt to exclude potentially erroneous data entries. For the reducible hernias, the mean OT for laparoscopic repair was significantly longer than for open repair, after adjusting for propensity score quintile and emergency status (98.5 vs. 84.9 min, p < 0.01). For cases of incarcerated/strangulated hernias, the OT for laparoscopic repair was also significantly longer than for open repair, after adjusting for propensity score quintile (96.4 vs. 81.2 min, p < 0.01).
Discussion
This analysis of more than 26,000 cases of open and laparoscopic VIHRs in ACS-NSQIP hospitals throughout the United States suggests the superiority of laparoscopy with regard to several important postoperative outcomes. Several studies advocated that laparoscopic VIHR can improve outcomes with regard to overall complications, recurrence rates, and LOS [16, 17]. However, these results were not demonstrated consistently [18–20], and only few randomized, controlled trials comparing open and laparoscopic VIHRs have been published [18, 21–25].
Limiting our analysis to the years 2009 and 2010 was necessary because of the small number of laparoscopic VIHRs recorded in the ACS-NSQIP database before 2009. This still provided adequate numbers to allow for an adequately powered comparison of the two techniques. Fewer than 20 % of VIHRs in both 2009 (18.5 %) and 2010 (19.9 %) were performed laparoscopically, suggesting that minimally invasive repair is still a developing technique that requires the acquisition of advanced laparoscopic skills and that may be perceived as technically challenging to many. Therefore, it is conceivable that the level of comfort with this approach is fairly low for those general surgeons who have not undergone extensive laparoscopic training. Additionally, small hernia defects may appear to be more easily repaired through a small incision via the open technique. It is yet to be determined with large randomized, controlled trials whether the higher costs and lower reimbursements associated with the laparoscopic approach are offset by the reported advantages of this technique, such as shorter LOS and return to baseline functional status. Although Misra et al. reported increased cost with the laparoscopic approach, a recent study that used the Nationwide Inpatient Sample demonstrated lower total hospital charges when the laparoscopic approach was used for ventral hernia repairs, which was believed to be partly related to the shorter LOS [21, 26].
The ACS-NSQIP data revealed that postoperative adverse wound occurrences in patients undergoing VIHR are relatively low. For reducible hernias, the incidence of any wound occurrence was 5.5 versus 1.2 % for open and laparoscopic techniques, respectively. For incarcerated/strangulated hernias, the incidence of wound occurrences was also low, at 6.6 versus 2.4 % for open and laparoscopic techniques, respectively. These results compare favorably with previously reported results, which ranged from 0 to 33 % for open repairs and from 0 to 6 % for laparoscopic repairs [13]. In fact, the ACS-NSQIP outcomes are better than the majority of the individual studies included in a recent Cochrane review of 10 available published randomized controlled trials [13]. However, the available trials were rather small and were of a single center, with only 11–104 study participants in each group. Taking into consideration that postoperative SSIs after VIHRs are relatively uncommon, we estimated that at least 2,000 patients would be required for an adequately powered randomized controlled trial to detect a difference between open versus laparoscopic repair for any wound complication. Even larger numbers would be necessary to detect differences for each individual type of SSI, an approach that is neither practical nor cost-effective.
To our knowledge, this is one of the few studies to compare postoperative SSI outcomes between open and laparoscopic repairs, analyzing separately reducible and incarcerated/strangulated hernias. Separating the two groups is important because repairs of incarcerated/strangulated hernias are performed in a potentially contaminated environment, a setting that may be associated with higher rates of wound infections, particularly with the use of mesh [27, 28]. The ACS-NSQIP data demonstrated that the incidence of postoperative wound infections for incarcerated/strangulated hernias is only 1.1 % higher than for reducible hernias with the open technique. Similarly, with laparoscopy, the incidence of postoperative wound infections for incarcerated/strangulated hernias was only 1.2 % higher compared to reducible hernias. These differences, though small, are significant, and they suggest that patients who undergo operative intervention for an incarcerated/strangulated hernia are more likely to develop a postoperative SSI, regardless of the surgical approach.
Although postoperative wound complications in patients undergoing VIHR in the ACS-NSQIP database were low, the reported morbidity was significantly greater with the open than the laparoscopic technique. For reducible hernias, patients undergoing open repair were at significantly greater risk of developing a superficial SSI, deep SSI, wound disruption, or organ/space SSI compared to patients undergoing laparoscopic repair. For incarcerated/strangulated hernias, patients undergoing open repair were found to be at significantly higher risk of superficial SSI, deep SSI, and wound disruption, but not organ/space SSI. These findings are in accordance with another recent ACS-NSQIP study and two recent meta-analyses [13, 29, 30]. It is not surprising that the open approach is associated with more skin and subcutaneous tissue infections, given the resultant trauma from the potentially extensive dissection of the subcutaneous tissue. The laparoscopic technique involves almost no dissection of subcutaneous tissue, and the incisions are much smaller, making migration of bacteria to the subcutaneous space less likely. However, it has been postulated that the laparoscopic approach is associated with more severe intra-abdominal complications, such as intraoperative hemorrhage or bowel injury, given the need for extensive lysis of adhesions in the area of the abdominal wall in which the mesh will be positioned [31, 32]. One would expect a significant increase in the incidence of organ/space SSIs using the laparoscopic technique. In our study, there was no such increase in these adverse outcomes in the laparoscopic group. In fact, the risk of organ/space infection for reducible hernias was found to be higher in the open group, and for the incarcerated/strangulated cases there was no difference between the two repair approaches. This may be attributed to the superior visualization that laparoscopy provides, which enables easier identification and dissection of tissue planes.
Today’s need to minimize health care expenditures makes the postoperative LOS a critical factor in the decision-making process for the selection of any surgical technique. Duration of hospitalization can also be a surrogate of other important outcomes that were not assessed in our study, such as postoperative pain and return of bowel function. It can also significantly affect the overall hospital cost. Our results demonstrated a significantly shorter LOS in the laparoscopic group for both reducible and incarcerated/strangulated hernias. Many studies have examined duration of hospitalization with inconsistent results. Although some randomized, controlled trials and retrospective cohort studies reported results similar to our study, others failed to demonstrate a significant difference in LOS [26, 29, 33–35]. Interestingly, Sauerland et al. [13] argued that LOS can only be reduced by laparoscopic surgery if the expected LOS after open hernia repair is relatively long.
The impact of postoperative SSIs on LOS and health care costs cannot be overestimated. It is not surprising that SSI occurrence for a variety of surgical procedures has been associated with increased LOS and treatment costs [36, 37]. Readmission to the hospital, frequent follow-up visits, or even need for home health care for regular wound dressing changes can add to the high costs related to these infections. The additional burden on patients should not be underestimated. For instance, patients with SSI are not only at risk for complications that result from prolonged hospitalization, such as hospital-acquired infections and pressure ulcers, but also complications related to antibiotic therapy, such as antimicrobial resistance and Clostridium difficile colitis. Therefore, it is apparent that any technique that reduces postoperative SSIs rates and its associated harmful outcomes can potentially improve the quality of care and considerably reduce treatment costs.
One of the important determinants in evaluating the effectiveness of a surgical procedure is the OT. In the current literature, some trials found that laparoscopic surgery took significantly longer than open surgery, whereas the opposite was true in other trials [13]. Our study examined differences in the OT between open and laparoscopic VIHRs, and we analyzed reducible and incarcerated/strangulated hernias separately. We found that the OT was significantly longer with the laparoscopic approach for both types of hernias. It is possible that limited surgical experience may have contributed to this difference, as the use of laparoscopy for repair of these hernias is still in its infancy in several institutions. Additionally, for nonreducible hernias, the laparoscopic approach may have taken longer, given the more extensive dissection required for mobilization. Unfortunately, specific information regarding classification of the hernia defect and some details of the repair (e.g., position of the mesh, use of tacks for fixation of the mesh in laparoscopic repairs) are not available in the ACS-NSQIP database.
There are several limitations associated with the use of the ACS-NSQIP database for this comparison that warrant discussion and should be taken into consideration when interpreting the results of this study. To adjust for differences in patient characteristics and comorbidities between the open and laparoscopic groups, we used the well-recognized technique of propensity score matching [38–41]. However, propensity score stratification does not represent true randomization; it can only adjust for known and measured confounders. Furthermore, the ACS-NSQIP database does not record all disease- and procedure-specific details, including presenting symptoms and surgical indication for the repair, as well as important hernia characteristics, such as defect size and number of previous recurrences. Intraoperative details such as overall complexity of the operation, conversion rates, occurrence of inadvertent bowel injury, and surgeon-specific factors including surgical technique details, type and positioning of mesh, and surgeon experience and technical expertise are not available in the database. All these factors may have an important impact on the outcomes examined.
In addition, the ACS-NSQIP database does not offer charge or cost data. Therefore, it is not possible to provide a direct estimate of the treatment cost associated with each technique. This makes it impossible to detect potential financial savings that would be incurred by adoption of the laparoscopic approach. Although we were able to analyze differences in LOS between the two techniques, the ACS-NSQIP database provides no information regarding patient-centered outcomes such as postoperative pain and recuperation times. A word of caution seems appropriate here regarding the generalizability of our results. Although the ACS-NSQIP database is limited to ACS-NSQIP participating hospitals, it includes more than 450 hospitals across the United States, making it a representative sample.
In conclusion, most VIHRs are not currently performed via a minimally invasive approach. It appears that the decision to perform open versus laparoscopic repair is guided more by individual and institutional experience than by evidence-based principles. This multi-institutional analysis examined a large sample of patients undergoing VIHR, resulting in statistically significant findings and adding relevant information to the quest for the optimal VIHR technique. We demonstrated that laparoscopic VIHR for reducible and incarcerated/strangulated hernias is associated with decreased risk of superficial SSIs, deep SSIs, and postoperative wound disruption compared to open repair. The incidence of all postoperative SSIs was significantly higher for incarcerated/strangulated hernias. Additionally, laparoscopic repair was associated with a shorter LOS. These data suggest that in eligible cases, laparoscopy should be used more frequently for the repair of ventral and incisional hernias. This study also confirms the need for more procedure-targeted programs in the ACS-NSQIP, to streamline and optimize data collection for ventral/incisional hernias, in an attempt to eliminate the current limitations of the ACS-NSQIP database.
References
DeFrances CJ, Cullen KA, Kozak LJ (2007) National Hospital Discharge Survey: 2005 annual summary with detailed diagnosis and procedure data. Vital Health Stat 13:1–209
Hoer JJ, Junge K, Schachtrupp A, Klinge U, Schumpelick V (2002) Influence of laparotomy closure technique on collagen synthesis in the incisional region. Hernia 6:93–98
Lomanto D, Iyer SG, Shabbir A, Cheah WK (2006) Laparoscopic versus open ventral hernia mesh repair: a prospective study. Surg Endosc 20:1030–1035
Mudge M, Hughes LE (1985) Incisional hernia: a 10 year prospective study of incidence and attitudes. Br J Surg 72:70–71
Cassar K, Munro A (2002) Surgical treatment of incisional hernia. Br J Surg 89:534–545
Iqbal CW, Pham TH, Joseph A, Mai J, Thompson GB, Sarr MG (2007) Long-term outcome of 254 complex incisional hernia repairs using the modified Rives-Stoppa technique. World J Surg 31:2398–2404
Luijendijk RW, Hop WC, van den Tol MP, de Lange DC, Braaksma MM, JN IJ, Boelhouwer RU, de Vries BC, Salu MK, Wereldsma JC, Bruijninckx CM, Jeekel J (2000) A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med 343:392–398
Read RC, Yoder G (1989) Recent trends in the management of incisional herniation. Arch Surg 124:485–488
van der Linden FT, van Vroonhoven TJ (1988) Long-term results after surgical correction of incisional hernia. Neth J Surg 40:127–129
Liakakos T, Karanikas I, Panagiotidis H, Dendrinos S (1994) Use of Marlex mesh in the repair of recurrent incisional hernia. Br J Surg 81:248–249
Toniato A, Pagetta C, Bernante P, Piotto A, Pelizzo MR (2002) Incisional hernia treatment with progressive pneumoperitoneum and retromuscular prosthetic hernioplasty. Langenbecks Arch Surg 387:246–248
LeBlanc KA, Booth WV (1993) Laparoscopic repair of incisional abdominal hernias using expanded polytetrafluoroethylene: preliminary findings. Surg Laparosc Endosc 3:39–41
Sauerland S, Walgenbach M, Habermalz B, Seiler CM, Miserez M (2011) Laparoscopic versus open surgical techniques for ventral or incisional hernia repair. Cochrane Database Syst Rev (3) CD007781. doi:10.1002/14651858.CD007781.pub2
Khuri SF, Daley J, Henderson W, Hur K, Demakis J, Aust JB, Chong V, Fabri PJ, Gibbs JO, Grover F, Hammermeister K, Irvin G III, McDonald G, Passaro E Jr, Phillips L, Scamman F, Spencer J, Stremple JF (1998) The Department of Veterans Affairs’ NSQIP: the first national, validated, outcome-based, risk-adjusted, and peer-controlled program for the measurement and enhancement of the quality of surgical care. National VA Surgical Quality Improvement Program. Ann Surg 228:491–507
Hilbe JM (2007) Negative binomial regression. Cambridge University Press, Cambridge
LeBlanc KA (2000) Current considerations in laparoscopic incisional and ventral herniorrhaphy. JSLS 4:131–139
Chowbey PK, Sharma A, Khullar R, Mann V, Baijal M, Vashistha A (2000) Laparoscopic ventral hernia repair. J Laparoendosc Adv Surg Tech A 10:79–84
Carbajo MA, Martin del Olmo JC, Blanco JI, de la Cuesta C, Toledano M, Martin F, Vaquero C, Inglada L (1999) Laparoscopic treatment vs open surgery in the solution of major incisional and abdominal wall hernias with mesh. Surg Endosc 13:250–252
Heniford BT, Park A, Ramshaw BJ, Voeller G (2000) Laparoscopic ventral and incisional hernia repair in 407 patients. J Am Coll Surg 190:645–650
Park A, Birch DW, Lovrics P (1998) Laparoscopic and open incisional hernia repair: a comparison study. Surgery 124:816–821
Misra MC, Bansal VK, Kulkarni MP, Pawar DK (2006) Comparison of laparoscopic and open repair of incisional and primary ventral hernia: results of a prospective randomized study. Surg Endosc 20:1839–1845
Barbaros U, Asoglu O, Seven R, Erbil Y, Dinccag A, Deveci U, Ozarmagan S, Mercan S (2007) The comparison of laparoscopic and open ventral hernia repairs: a prospective randomized study. Hernia 11:51–56
Navarra G, Musolino C, De Marco ML, Bartolotta M, Barbera A, Centorrino T (2007) Retromuscular sutured incisional hernia repair: a randomized controlled trial to compare open and laparoscopic approach. Surg Laparosc Endosc Percutan Tech 17:86–90
Olmi S, Scaini A, Cesana GC, Erba L, Croce E (2007) Laparoscopic versus open incisional hernia repair: an open randomized controlled study. Surg Endosc 21:555–559
Asencio F, Aguilo J, Peiro S, Carbo J, Ferri R, Caro F, Ahmad M (2009) Open randomized clinical trial of laparoscopic versus open incisional hernia repair. Surg Endosc 23:1441–1448
Colavita PD, Tsirline VB, Walters AL, Lincourt AE, Belyansky I, Heniford BT (2013) Laparoscopic versus open hernia repair: outcomes and sociodemographic utilization results from the nationwide inpatient sample. Surg Endosc 27(1):109–117
Alvarez Perez JA, Baldonedo RF, Bear IG, Solis JA, Alvarez P, Jorge JI (2003) Emergency hernia repairs in elderly patients. Int Surg 88:231–237
Nieuwenhuizen J, van Ramshorst GH, ten Brinke JG, de Wit T, van der Harst E, Hop WC, Jeekel J, Lange JF (2011) The use of mesh in acute hernia: frequency and outcome in 99 cases. Hernia 15:297–300
Mason RJ, Moazzez A, Sohn HJ, Berne TV, Katkhouda N (2011) Laparoscopic versus open anterior abdominal wall hernia repair: 30-day morbidity and mortality using the ACS-NSQIP database. Ann Surg 254:641–652
Sajid MS, Bokhari SA, Mallick AS, Cheek E, Baig MK (2009) Laparoscopic versus open repair of incisional/ventral hernia: a meta-analysis. Am J Surg 197:64–72
Berger D, Bientzle M, Muller A (2002) Postoperative complications after laparoscopic incisional hernia repair. Incidence and treatment. Surg Endosc 16:1720–1723
LeBlanc KA, Elieson MJ, Corder JM 3rd (2007) Enterotomy and mortality rates of laparoscopic incisional and ventral hernia repair: a review of the literature. JSLS 11:408–414
Forbes SS, Eskicioglu C, McLeod RS, Okrainec A (2009) Meta-analysis of randomized controlled trials comparing open and laparoscopic ventral and incisional hernia repair with mesh. Br J Surg 96:851–858
Hwang CS, Wichterman KA, Alfrey EJ (2009) Laparoscopic ventral hernia repair is safer than open repair: analysis of the NSQIP data. J Surg Res 156:213–216
Pring CM, Tran V, O’Rourke N, Martin IJ (2008) Laparoscopic versus open ventral hernia repair: a randomized controlled trial. ANZ J Surg 78:903–906
de Lissovoy G, Fraeman K, Hutchins V, Murphy D, Song D, Vaughn BB (2009) Surgical site infection: incidence and impact on hospital utilization and treatment costs. Am J Infect Control 37:387–397
Wick EC, Hirose K, Shore AD, Clark JM, Gearhart SL, Efron J, Makary MA (2011) Surgical site infections and cost in obese patients undergoing colorectal surgery. Arch Surg 146:1068–1072
Hutter MM, Randall S, Khuri SF, Henderson WG, Abbott WM, Warshaw AL (2006) Laparoscopic versus open gastric bypass for morbid obesity: a multicenter, prospective, risk-adjusted analysis from the National Surgical Quality Improvement Program. Ann Surg 243:657–662
Leichtle SW, Mouawad NJ, Welch K, Lampman R, Whitehouse WM Jr, Heidenreich M (2012) Outcomes of carotid endarterectomy under general and regional anesthesia from the American College of Surgeons’ National Surgical Quality Improvement Program. J Vasc Surg 56(81–88):e83
D’Agostino RB Jr (2007) Propensity scores in cardiovascular research. Circulation 115:2340–2343
Kennedy GD, Rajamanickam V, O’Connor ES, Loconte NK, Foley EF, Leverson G, Heise CP (2011) Optimizing surgical care of colon cancer in the older adult population. Ann Surg 253:508–514
Disclosures
Drs. Christodoulos Kaoutzanis, Stefan W. Leichtle, Nicolas J. Mouawad, Richard M. Lampman, and Robert K. Cleary, and Ms. Kathleen B. Welch have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kaoutzanis, C., Leichtle, S.W., Mouawad, N.J. et al. Postoperative surgical site infections after ventral/incisional hernia repair: a comparison of open and laparoscopic outcomes. Surg Endosc 27, 2221–2230 (2013). https://doi.org/10.1007/s00464-012-2743-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2743-0