Abstract
Purpose
The effectiveness of a neuromuscular electrical stimulation (NMES) program has been shown to be proportional to the maximal evocable torque (MET), which is potentially influenced by pulse characteristics such as duration and frequency. The aim of this study was to compare MET between conventional and wide-pulse NMES at two different frequencies.
Methods
MET—expressed as a percentage of maximal voluntary contraction (MVC) torque—and maximal tolerable current intensity were quantified on 71 healthy subjects. The right quadriceps was stimulated with three NMES protocols using different pulse duration/frequency combinations: conventional NMES (0.2 ms/50 Hz; CONV), wide-pulse NMES at 50 Hz (1 ms/50 Hz; WP50) and wide-pulse NMES at 100 Hz (1 ms/100 Hz; WP100). The proportion of subjects reaching the maximal stimulator output (100 mA) before attaining maximal tolerable current intensity was also quantified.
Results
The proportion of subjects attaining maximal stimulator output was higher for CONV than WP50 and WP100 (p < 0.001). In subjects who did not attain maximal stimulator output in any protocol, MET was higher for both WP50 and WP100 than for CONV (p < 0.001). Maximal tolerable current intensity was lower for both WP50 and WP100 than for CONV and was also lower for WP100 than for WP50 (p < 0.001).
Conclusion
When compared to conventional NMES, wide-pulse protocols resulted in greater MET and lower maximal tolerable current intensity. Overall, this may lead to better NMES training/rehabilitation effectiveness and less practical issues associated with maximal stimulator output limitations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuromuscular electrical stimulation (NMES) is a strength training/rehabilitation modality used for improving neuromuscular function in healthy subjects (Gondin et al. 2011) and for preserving/restoring muscle mass and function during and after a period of disuse in a variety of patient populations (Maffiuletti 2010; Maffiuletti et al. 2018). The most commonly stimulated muscle is the quadriceps femoris (Bax et al. 2005; Maffiuletti et al. 2018), for both functional and practical reasons. NMES usually consists in the application of pulsed currents with specific characteristics, the most important being pulse intensity, duration and frequency. General evidence-based recommendations (i.e. biphasic pulses lasting 100–500 µs with a frequency of 50–100 Hz) correspond to the conventional use of NMES (Vanderthommen and Duchateau 2007).
NMES treatment effectiveness is proportional to the maximal torque that could be evoked by a single NMES train (Lai et al. 1988; Natsume et al. 2018; Selkowitz 1985)–hereafter referred to as maximal evocable torque (MET)–that requires the use of high current intensities. As such, the main limitation of conventional NMES is the level of discomfort, given that subjects are invited to consistently attain the maximal tolerable current intensity (Delitto et al. 1992). Some subjects could approach or even reach the maximal stimulator output of standard devices (~ 100 mA), particularly following multiple NMES sessions, since tolerance to high-intensity NMES has been found to increase during a training program (Gondin et al. 2011). The use of large electrodes (owing to reduced current density) (Flodin et al. 2022), which has recently been recommended for an optimal application of NMES to the quadriceps femoris (Maffiuletti et al. 2018), could even lead to a greater proportion of subjects reaching the maximal stimulator output. In turn, this may lead to more subjects training at suboptimal workload (i.e. MET being less than maximal theoretical NMES-evoked torque).
Besides greater current intensity, wider pulses and higher frequencies have been demonstrated to increase NMES-evoked torque (Gorgey et al. 2009, 2006; Gorgey and Dudley 2008; Gregory et al. 2007). Wide-pulse NMES, which encompasses the use of 1-ms pulses, has recently been introduced with the goal to evoke more physiological submaximal contractions (i.e. recruitment of motor units following the Henneman’s size principle) (Bergquist et al. 2011b; Collins 2007), but not necessarily to maximize MET. However, knee extensor MET has been shown to be greater with intermediate-duration (0.2 ms) than with short-duration (0.05 ms) pulses (Scott et al. 2009). In contrast, Liebano et al. (2013) failed to demonstrate a significant variation of MET between 0.4-, 0.7- and 1-ms pulses but suggested that the increasing trend of MET with pulse duration they observed (i.e. MET being 5.5% greater for 1-ms than 0.4-ms pulses) could reach significance with more subjects. It is, therefore, reasonable to assume that wide-pulse NMES at the maximal tolerable current intensity may generate a higher MET than conventional NMES with shorter pulses. Wide-pulse NMES also has the advantage of requiring relatively low current intensities compared to conventional NMES to evoke a similar submaximal torque (Espeit et al. 2021; Neyroud et al. 2014), because of the greater current charge resulting from the utilization of wide pulses, and this could potentially circumvent the technical limit of the stimulator.
Therefore, the aim of this study was to compare MET (primary outcome), maximal tolerable current intensity and the proportion of subjects attaining the maximal stimulator output (secondary outcomes) of a commercially available stimulator (100 mA) between conventional NMES of the quadriceps femoris muscle and wide-pulse NMES at two different frequencies in a large cohort of healthy subjects. We hypothesized that MET would be higher, maximal tolerable current intensity would be lower, and the proportion of subjects attaining the maximal stimulator output would be smaller for wide-pulse than for conventional NMES.
Materials and methods
Subjects
Seventy-one healthy volunteers (28 women, age: 25 ± 4 yr, height: 173 ± 9 cm, body mass: 69 ± 11 kg) participated in this study. Subjects were recruited from the Jean Monnet University community (Saint-Etienne, France) and the majority of them (89%) were graduate students. None of the subjects had previously engaged in systematic NMES training. The local ethical committee (CPP SUD-EST I; 2021-A00507-34) approved the study, and written informed consent was obtained from all subjects. The study was conducted according to the Declaration of Helsinki.
Experimental design
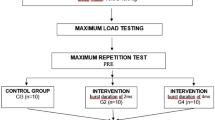
Subjects were seated in an isometric dynamometer (ARS dynamometry; S2P Ltd., Ljubljana, Slovenia) with the hips at 90° and the tested knee (right) at 60° of flexion (Fig. 1). The leg was attached to the dynamometer lever by a noncompliant strap just proximal to the intermalleolar axis. The trunk was securely strapped to the dynamometer chair. After a standardized warm-up of 10 submaximal contractions, subjects performed three maximal voluntary contractions (MVC) of the knee extensors separated by 1-min rest periods. During these contractions, subjects were instructed to contract their muscles as strongly as possible for ~ 4 s with a progressive torque build-up. MVC torque was the highest torque recorded during the three MVCs.
Subsequently, three NMES protocols with different pulse duration/frequency combinations were tested in a random order: conventional NMES (0.2 ms/50 Hz, CONV), wide-pulse NMES at 50 Hz (1 ms/50 Hz, WP50) and wide-pulse NMES at 100 Hz (1 ms/100 Hz, WP100). Current was delivered with a commercially available NMES unit (BioStim 2.1, Mazet Santé, Electronique du Mazet, Le Mazet Saint Voy, France), which can provide biphasic symmetric rectangular pulses with a maximal stimulator output of 100 mA at 50 Hz and of 90 mA at 100 Hz. Two large self-adhesive electrodes were placed over the quadriceps femoris muscle bellies, as recently recommended (Maffiuletti et al. 2018). One electrode, measuring 198 cm2 (180 × 110 mm, axion GmbH, Leonberg, Germany), was positioned on the distal third of the thigh. The other electrode, measuring 85 cm2 (125 × 86 mm, axion GmbH), was placed 5–7 cm below the inguinal ligament (Fig. 1). After a quick standardized familiarization (i.e. a progressive increase of the current intensity during a 20-s period up to 10% MVC) with the three NMES protocols, maximal tolerable current intensity and MET were determined in each condition. Briefly, current intensity was progressively increased during 20-s trains separated by 20-s rest periods (a maximum of four trains were necessary) until NMES-induced discomfort became intolerable (i.e. maximal tolerable current intensity) or until maximal stimulator output was reached. The intensity was first quickly increased by the investigator to reach ~ 10% of MVC torque and thereafter it was further increased by the subject up to maximal tolerable current intensity or maximal stimulator output using a remote control. Rest periods of 3 min were provided between each NMES protocol to minimize fatigue. Subjects were consistently asked to relax their muscles during NMES. MET, expressed in percentage of MVC, was the highest torque evoked at either maximal tolerable current intensity or maximal stimulator output. The proportion of subjects having reached the maximal stimulator output before attaining the maximal tolerable current intensity was also quantified for CONV, WP50 and WP100 (maximal stimulator output: 100, 100 and 90 mA, respectively).
Statistics
All data are presented as mean values ± SD. Statistical analyses were performed with JAMOVI software (version 1.1.9). The Shapiro–Wilk test was used to examine data normality. The Chi-squared test was performed to compare the proportion of subjects attaining the maximal stimulator output in each NMES protocol. These subjects were excluded from the remaining analyses. One-way repeated measures ANOVAs were used to compare MET and maximal tolerable current intensity between the different NMES protocols (CONV vs WP50 vs WP100). In case of a significant main effect of protocol, Tukey post hoc tests were used. Partial eta-squared (η2p) and Cohen’s d were calculated for effect size, with values representing small (η2p ≥ 0.1 and d ≥ 0.2), medium (η2p ≥ 0.25 and d ≥ 0.5), and large (η2p ≥ 0.4 and d ≥ 0.8) effects. Statistical significance was set at p < 0.05.
Results
The proportion of subjects attaining the maximal stimulator output was higher for CONV (30%; 3 women and 18 men) than WP50 (3%; 2 men; p < 0.001) and WP100 (4%; 3 men; p < 0.001), without any difference between WP50 and WP100 (p = 0.649). The subjects attaining maximal stimulator output with wide-pulse protocols (WP50 and WP100) also reached maximal stimulator output with CONV. The remaining results refer to the 50 subjects (25 women and 25 men) who did not attain maximal stimulator output in any condition.
There was an effect of NMES protocol on MET (p < 0.001; η2p = 0.162) and maximal tolerable current intensity (p < 0.001; η2p = 0.963). MET was higher for both WP50 (p < 0.001; d = 0.598) and WP100 (p = 0.024; d = 0.395) compared to CONV (45.4 ± 17.9 vs 43.0 ± 16.5 vs 39.1 ± 14.0% MVC, respectively), with no difference between WP50 and WP100 (p = 0.236; d = 0.226) (Fig. 2A). Maximal tolerable current intensity was lower for both WP50 (p < 0.001; d = 5.07) and WP100 (p < 0.001; d = 6.07) compared to CONV (45.2 ± 12.1 vs 41.7 ± 10.5 vs 76.7 ± 12.3 mA, respectively). Maximal tolerable current intensity was also lower for WP100 than for WP50 (p < 0.001; d = 0.882) (Fig. 2B).
Maximal evocable torque (MET; panel A) and maximal tolerable current intensity (panel B) for conventional NMES (0.2 ms/50 Hz, CONV), wide-pulse NMES at 50 Hz (1 ms/50 Hz, WP50) and wide-pulse NMES at 100 Hz (1 ms/100 Hz, WP100) for the subjects who did not attain MSO (n = 50). The box extends from the 25th to 75th percentiles, the horizontal line within the box represents the median, and the whiskers represent the minimum and the maximum values. Dots represent individual data. ### significant difference (p < 0.001). # significant difference (p < 0.05)
Discussion
The main findings of the present study were that, when compared to conventional NMES, wide-pulse protocols resulted in greater MET, lower maximal tolerable current intensity and consequently in a lower proportion of subjects attaining the maximal stimulator output.
Our main finding of a greater MET for the two wide-pulse protocols compared to conventional NMES is in agreement with previous results obtained for a range of shorter pulse durations (Scott et al. 2009). These authors reported a greater MET with intermediate-duration (0.2 ms) than with short-duration (0.05 ms) pulses. However, Liebano et al. (2013) reported a small increase of MET with increasing pulse duration from 0.4 to 1 ms, but failed to observe significant differences between the conditions. This was likely due to a lack of statistical power (i.e. small sample size; 19 women), an issue that was prevented in the present study thanks to a greater sample size (i.e. 71 subjects tested; statistical power = 0.999). There is increasing evidence that the effectiveness of any NMES training/rehabilitation program (i.e. the training-induced strength gain) is proportional to the MET, usually referred to as NMES training intensity (Lai et al. 1988; Natsume et al. 2018; Selkowitz 1985). Considering the pioneer study of Lai et al. (1988) who reported NMES training-induced strength gains of 24 and 48% for MET of 25 and 50% MVC, respectively (i.e. a linear dose–response relationship between treatment effectiveness and MET), the greater MET of our wide-pulse protocols compared to conventional NMES (i.e. approximately 45% vs 40% MVC) could be translated into a potential benefit of 5% in terms of expected effectiveness. Several authors reported MET ranging from 25 to 90% MVC for the healthy quadriceps (Gondin et al. 2011; Vanderthommen and Duchateau 2007), while the lower range of MET that is needed for strengthening effects has been suggested to be around 15–20% MVC (Flodin et al. 2022; Maffiuletti et al. 2018). Therapeutic window ranges of 25–50% and 15–25% MVC have also been advocated for healthy subjects/orthopaedic patients and cardiorespiratory patients, respectively (Maffiuletti et al. 2018). The mean METs reported in the present study for the three protocols (39–45% MVC) are in accordance with the aforementioned literature and are within the effective window range for healthy subjects.
To the best of our knowledge, a comparison between wide-pulse and conventional NMES training programs has never been conducted when considering NMES applied at maximal tolerable current intensity on the quadriceps femoris muscle. A first physiological explanation for the greater MET obtained with wide-pulse protocols could be the occurrence of the so-called “extra torque” with wide-pulse NMES (Collins 2007). At low current intensities, the use of wide pulses favors the recruitment of sensory axons having a longer strength-duration and lower rheobase than motor axons (Veale et al. 1973), which may lead to the development of central torque in addition to the peripheral depolarization of motor axons (Collins 2007). Our team recently reported similar extra torque for WP50 and WP100 at submaximal intensities (Espeit et al. 2021), whose magnitude (5–10% MVC) seems in accordance with the “extra” MET observed in the present study. However, the use of high current intensities such as those used in this study may reduce or even eliminate the central torque due to a greater antidromic collision in motor axons. In the present study, the progressive increase of current intensity during single NMES trains precluded the measurement of this phenomenon, but to the best of our knowledge, central torque has never been observed with current intensities evoking more than 20% MVC (Bergquist et al. 2011a). In addition to this indirect recruitment, a second explanation could be the direct recruitment of additional, presumably larger/faster motor units with wide-pulse NMES. Compared to narrower pulses, the use of wide pulses is associated with a greater current charge which may indeed lead to the additional recruitment of larger motor units (Gorgey et al. 2009; Gorgey and Dudley 2008). In this sense, Gorgey et al. (2006) reported a greater increase of evoked torque than activated area measured by MRI, using wider pulse durations. The greater resulting tension (i.e. torque/activated area) suggested the recruitment of presumably faster muscle fibers (Bodine et al. 1987). However, Feiereisen et al. (1997) conversely suggested that the recruitment of fast muscle fibers tended to increase with narrower (0.1-ms) compared to wider (1-ms) pulses. Therefore, it remains difficult to speculate on why and how wide-pulse NMES could induce greater MET than conventional NMES. A third explanation could be a possible attenuation of MET for conventional NMES due to muscle fatigue and/or excitability threshold increase of the axonal terminal branches (Papaiordanidou et al. 2014). Indeed, as a consequence of the higher maximal tolerable current intensity for conventional than wide-pulse NMES, MET was reached using longer stimulation periods for conventional NMES. We, therefore, cannot rule out the possibility that this might have partially reduced the “real” MET.
The lower maximal tolerable current intensity for wide-pulse (WP50 an WP100) than conventional NMES was not a surprising result since a lower current intensity is needed to provide a similar current charge (i.e. the product of pulse intensity and duration) with wider pulse durations. This is perfectly illustrated by the ⁓tenfold higher current intensity required to evoke 10% MVC on the plantar flexor muscles for conventional compared to wide-pulse NMES (Espeit et al. 2021; Neyroud et al. 2014). Thus, the lower maximal tolerable current intensity of wide-pulse NMES substantially reduces the likelihood of reaching the maximal stimulator output, particularly in trained subjects. As a practical observation, several subjects reach the maximal stimulator output after multiple sessions of conventional NMES–mainly due to improved current tolerance (Gondin et al. 2011)–which precludes the use of optimal NMES procedures. Using wide-pulse instead of shorter conventional-duration pulses may represent a potential solution to this problem and would allow better effectiveness for more participants, even if most of the commercially available NMES units have an upper limit of 500–600 µs for pulse duration. We recommend manufacturers to provide equipment allowing to increase pulse duration to 1 ms, while we also hope that clinicians will consider this practical tip when selecting NMES devices and protocols. The use of wide-pulse NMES should be accompanied by some caution. Despite lower current intensities, wide-pulse NMES often result in greater current charge and density (i.e. the amount of current divided by electrode area) compared to narrow pulses, which could lead to skin irritation/burn in proximity to the electrode. To prevent this issue, we recommend the use of biphasic symmetrical pulses to avoid electrochemical burn caused by an accumulation of ions below the electrode, and large and relatively new electrodes (to limit loss of adhesion and drying of the gel) to decrease current density and allow a better dispersion of the current (Nussbaum et al. 2017).
Study limitations
Although a maximal stimulator output of 100 mA is very common for commercially-available NMES unit, some stimulators (e.g. Compex Sport) can deliver current intensities up to 120 mA. It may decrease the proportion of subjects attaining the maximal stimulator output, especially for conventional NMES, and therefore, exclude less subjects from the NMES protocols comparison. However, these stimulators cannot generate wide pulses (i.e. they generally allow pulse duration ≤ 0.4 ms). Moreover, shorter trains (≤ 4 s) were usually used in previous studies investigating MET to minimize the duration of the discomfort and the effects of muscle fatigue (Liebano et al. 2013; Scott et al. 2009), while recommendations for the use of NMES in rehabilitation specify trains of approximately 10 s duration (Spector et al. 2016). We rather used 20-s trains, because it was more convenient to reach maximal tolerable current intensity through the NMES device we used. Finally, a supplementary 20-s train at constant maximal tolerable current intensity would allow the estimation of potential extra torque occurrence (Espeit et al. 2021; Wegrzyk et al. 2015), but it would also cause considerable discomfort and muscle fatigue.
Conclusion
In conclusion, the present study demonstrated a greater MET (i.e. better expected NMES training/rehabilitation effectiveness) and a lower maximal tolerable current intensity (i.e. less practical issues with maximal stimulator output limitations) with wide-pulse compared to conventional NMES of the quadriceps muscle. Further research is required to extend the present results to other muscles and clinical populations, and to confirm these findings during the course of NMES training/rehabilitation programs.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author [TL] on reasonable request.
Abbreviations
- ANOVA:
-
Analysis of variance
- CONV:
-
Conventional NMES
- MET:
-
Maximal evocable torque
- MVC:
-
Maximal voluntary contraction
- NMES:
-
Neuromuscular electrical stimulation
- WP50:
-
Wide-pulse NMES at 50 Hz
- WP100:
-
Wide-pulse NMES at 100 Hz
References
Bax L, Staes F, Verhagen A (2005) Does neuromuscular electrical stimulation strengthen the quadriceps femoris? A systematic review of randomised controlled trials. Sports Med 35(3):191–212. https://doi.org/10.2165/00007256-200535030-00002
Bergquist AJ, Clair JM, Collins DF (2011a) Motor unit recruitment when neuromuscular electrical stimulation is applied over a nerve trunk compared with a muscle belly: triceps surae. J Appl Physiol 110(3):627–637. https://doi.org/10.1152/japplphysiol.01103.2010
Bergquist AJ, Clair JM, Lagerquist O, Mang CS, Okuma Y, Collins DF (2011b) Neuromuscular electrical stimulation: implications of the electrically evoked sensory volley. Eur J Appl Physiol 111(10):2409–2426. https://doi.org/10.1007/s00421-011-2087-9
Bodine SC, Roy RR, Eldred E, Edgerton VR (1987) Maximal force as a function of anatomical features of motor units in the cat tibialis anterior. J Neurophysiol 57(6):1730–1745. https://doi.org/10.1152/jn.1987.57.6.1730
Collins DF (2007) Central contributions to contractions evoked by tetanic neuromuscular electrical stimulation. Exerc Sport Sci Rev 35(3):102–109. https://doi.org/10.1097/jes.0b013e3180a0321b
Delitto A, Strube MJ, Shulman AD, Minor SD (1992) A study of discomfort with electrical stimulation. Phys Ther 72(6):410–421. https://doi.org/10.1093/ptj/72.6.410. (discussion on 421–414)
Espeit L, Rozand V, Millet GY, Gondin J, Maffiuletti NA, Lapole T (2021) Influence of wide-pulse neuromuscular electrical stimulation frequency and superimposed tendon vibration on occurrence and magnitude of extra torque. J Appl Physiol 131(1):302–312. https://doi.org/10.1152/japplphysiol.00968.2020
Feiereisen P, Duchateau J, Hainaut K (1997) Motor unit recruitment order during voluntary and electrically induced contractions in the tibialis anterior. Exp Brain Res 114(1):117–123. https://doi.org/10.1007/pl00005610
Flodin J, Mikkelsen C, Ackermann PW (2022) Knee extensor force production and discomfort during neuromuscular electrical stimulation of quadriceps with and without gluteal muscle co-stimulation. Eur J Appl Physiol 122(6):1521–1530. https://doi.org/10.1007/s00421-022-04949-9
Gondin J, Cozzone PJ, Bendahan D (2011) Is high-frequency neuromuscular electrical stimulation a suitable tool for muscle performance improvement in both healthy humans and athletes? Eur J Appl Physiol 111(10):2473–2487. https://doi.org/10.1007/s00421-011-2101-2
Gorgey AS, Dudley GA (2008) The role of pulse duration and stimulation duration in maximizing the normalized torque during neuromuscular electrical stimulation. J Orthop Sports Phys Ther 38(8):508–516. https://doi.org/10.2519/jospt.2008.2734
Gorgey AS, Mahoney E, Kendall T, Dudley GA (2006) Effects of neuromuscular electrical stimulation parameters on specific tension. Eur J Appl Physiol 97(6):737–744. https://doi.org/10.1007/s00421-006-0232-7
Gorgey AS, Black CD, Elder CP, Dudley GA (2009) Effects of electrical stimulation parameters on fatigue in skeletal muscle. J Orthop Sports Phys Ther 39(9):684–692. https://doi.org/10.2519/jospt.2009.3045
Gregory CM, Dixon W, Bickel CS (2007) Impact of varying pulse frequency and duration on muscle torque production and fatigue. Muscle Nerve 35(4):504–509. https://doi.org/10.1002/mus.20710
Lai HS, Domenico GD, Strauss GR (1988) The effect of different electro-motor stimulation training intensities on strength improvement. Aust J Physiother 34(3):151–164. https://doi.org/10.1016/S0004-9514(14)60607-3
Liebano RE, Rodrigues TA, Murazawa MT, Ward AR (2013) The influence of stimulus phase duration on discomfort and electrically induced torque of quadriceps femoris. Braz J Phys Ther 17(5):479–486. https://doi.org/10.1590/S1413-35552012005000112
Maffiuletti NA (2010) Physiological and methodological considerations for the use of neuromuscular electrical stimulation. Eur J Appl Physiol 110(2):223–234. https://doi.org/10.1007/s00421-010-1502-y
Maffiuletti NA, Gondin J, Place N, Stevens-Lapsley J, Vivodtzev I, Minetto MA (2018) Clinical use of neuromuscular electrical stimulation for neuromuscular rehabilitation: what are we overlooking? Arch Phys Med Rehabil 99(4):806–812. https://doi.org/10.1016/j.apmr.2017.10.028
Natsume T, Ozaki H, Kakigi R, Kobayashi H, Naito H (2018) Effects of training intensity in electromyostimulation on human skeletal muscle. Eur J Appl Physiol 118(7):1339–1347. https://doi.org/10.1007/s00421-018-3866-3
Neyroud D, Dodd D, Gondin J, Maffiuletti NA, Kayser B, place N (2014) Wide-pulse-high-frequency neuromuscular stimulation of triceps surae induces greater muscle fatigue compared with conventional stimulation. J Appl Physiol 116(10):1281–1289. https://doi.org/10.1152/japplphysiol.01015.2013
Nussbaum EL, Houghton P, Anthony J, Rennie S, Shay BL, Hoens AM (2017) Neuromuscular electrical stimulation for treatment of muscle impairment: critical review and recommendations for clinical practice. Physiother Can 69(5):1–76. https://doi.org/10.3138/ptc.2015-88
Papaiordanidou M, Stevenot JD, Mustacchi V, Vanoncini M, Martin A (2014) Electrically induced torque decrease reflects more than muscle fatigue. Muscle Nerve 50(4):604–607. https://doi.org/10.1002/mus.24276
Scott WB, Causey JB, Marshall TL (2009) Comparison of maximum tolerated muscle torques produced by 2 pulse durations. Phys Ther 89(8):851–857. https://doi.org/10.2522/ptj.20080151
Selkowitz DM (1985) Improvement in isometric strength of the quadriceps femoris muscle after training with electrical stimulation. Phys Ther 65(2):186–196. https://doi.org/10.1093/ptj/65.2.186
Spector P, Laufer Y, Elboim Gabyzon M, Kittelson A, Stevens Lapsley J, Maffiuletti NA (2016) Neuromuscular electrical stimulation therapy to restore quadriceps muscle function in patients after orthopaedic surgery: a novel structured approach. J Bone Joint Surg Am 98(23):2017–2024. https://doi.org/10.2106/JBJS.16.00192
Vanderthommen M, Duchateau J (2007) Electrical stimulation as a modality to improve performance of the neuromuscular system. Exerc Sport Sci Rev 35(4):180–185. https://doi.org/10.1097/jes.0b013e318156e785
Veale JL, Mark RF, Rees S (1973) Differential sensitivity of motor and sensory fibres in human ulnar nerve. J Neurol Neurosurg Psychiatry 36(1):75–86. https://doi.org/10.1136/jnnp.36.1.75
Wegrzyk J, Foure A, Vilmen C, Ghattas B, Maffiuletti NA, Mattei JP, Place N, Bendahan D, Gondin J (2015) Extra Forces induced by wide-pulse, high-frequency electrical stimulation: occurrence, magnitude, variability and underlying mechanisms. Clin Neurophysiol 126(7):1400–1412. https://doi.org/10.1016/j.clinph.2014.10.001
Acknowledgements
The authors thank all the subjects for their participation and the company Mazet Santé for the loan of the stimulator. The authors sincerely thank Callum Brownstein for English editing.
Funding
The authors declare that the results of the study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation. No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by LE. The first draft of the manuscript was written by LE and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Communicated by Toshio Moritani.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Espeit, L., Lapole, T., Millet, G.Y. et al. Wide-pulse electrical stimulation of the quadriceps allows greater maximal evocable torque than conventional stimulation. Eur J Appl Physiol 123, 1209–1214 (2023). https://doi.org/10.1007/s00421-023-05145-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-023-05145-z