Abstract
Completion of high-intensity interval training (HIIT) leads to significant increases in maximal oxygen uptake (VO2max) and oxidative capacity. However, individual responses to HIIT have been identified as approximately 20–40% of individuals show no change in VO2max, which may be due to the relatively homogeneous approach to implementing HIIT. Purpose: This study tested the effects of HIIT prescribed using ventilatory threshold (VT) on changes in VO2max and cycling performance. Methods: Fourteen active men and women (age and VO2max = 27 ± 8 year and 38 ± 4 mL/kg/min) underwent nine sessions of HIIT, and 14 additional men and women (age and VO2max = 22 ± 3 year and 40 ± 5 mL/kg/min) served as controls. Training was performed on a cycle ergometer at a work rate equal to 130%VT and consisted of eight to ten 1 min bouts interspersed with 75 s of recovery. At baseline and post-testing, they completed progressive cycling to exhaustion to determine VO2max, and on a separate day, a 5 mile cycling time trial. Results: Compared to the control group, HIIT led to significant increases in VO2max (6%, p = 0.007), cycling performance (2.5%, p = 0.003), and absolute VT (9 W, p = 0.005). However, only 57% of participants revealed meaningful increases in VO2max and cycling performance in response to training, and two showed no change in either outcome. Conclusions: A greater volume of HIIT may be needed to maximize the training response for all individuals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Current physical activity guidelines for all adults (Garber et al. 2011) recommend 150 min/week of moderate-intensity continuous training (MICT) to enhance cardiorespiratory fitness (VO2max), which benefits physical function and health status. However, regular participation in physical activity is low in most adults (< 25%, CDC 2014). Primary barriers to physical activity include lack of enjoyment and time (Trost et al. 2002). In the last decade, there has been extensive interest in the efficacy of high-intensity interval training (HIIT) to increase cardiometabolic health in various populations including healthy young adults as well as those with chronic disease (Weston et al. 2014a, b). HIIT and its more intense form, sprint interval training (SIT), are characterized by brief, intense efforts of near-maximal to supramaximal effort separated by active recovery, and require lower exercise duration than MICT (Gibala et al. 2014). Data show similar (Burgomaster et al. 2008) and in some cases superior adaptations with HIIT or SIT versus MICT (Milanovic et al. 2015), emphasizing its efficacy in various populations.
However, the optimal regime of HIIT remains to be identified. Typically, HIIT is prescribed based on a specific fraction of maximal heart rate or peak power output (e.g., 80–100% of maximal heart rate or power output) determined from ramp exercise on the cycle ergometer. In the case of SIT, exercise is typically performed at specific power outputs relative to body mass (5.0–8.5%). Nevertheless, basing training on an absolute intensity fails to account for individual metabolic responses to exercise (Katch et al. 1978), as participants train at different relative intensities based on their ventilatory threshold (VT) (Scharhag-Rosenberger et al. 2010),which results in inhomogeneous metabolic strain. A previous study demonstrated that blood lactate (BLa) concentration at different %VO2max significantly varies across individuals of similar fitness level (Scharhag-Rosenberger et al. 2010), which suggests a disparate level of metabolic strain and fatigue at identical relative intensities in homogeneous populations. And, it is the magnitude of this acute response which is thought to elicit various chronic adaptations to exercise training (Coffey and Hawley 2007). In one study (Wolpern et al. 2015), completion of 12 weeks of MICT prescribed according to VT led to greater increases in VO2max compared to when intensity was based on HR. In sedentary adults, similar results were shown in response to 13 weeks of standardized or individualized MICT (Dalleck et al. 2016). Nevertheless, the intensity of training based on VT was higher than that based on heart rate, so it is unclear if the greater magnitude of adaptation is due to this factor or the individualized regime. To our knowledge, only one study has prescribed HIIT using VT. In persons with cardiovascular disease, Tamburus et al. (2016) prescribed 16 weeks of HIIT according to VT, and results showed significant increases in VO2 and workload at VT. However, this study did not measure changes in VO2max, and some of the training was performed at relatively moderate intensities which may not represent HIIT, so the overall efficacy of this approach is poorly understood. Overall, these two studies have methodological flaws which somewhat hamper their examination of potential superiority of threshold-based exercise training.
Although HIIT-derived increases in outcomes including VO2max, oxidative capacity, and glycemic control are consistently reported (Gibala et al. 2014; Jelleyman et al. 2015; Milanovic et al. 2015), it is apparent that individual responses to HIIT do occur. Two studies (Astorino and Schubert 2014; Gurd et al. 2016) documented that approximately 20–50% of participants undergoing various HIIT and SIT protocols show non-response in at least one outcome measure including VO2max, fat oxidation, heart rate, or, lactate threshold. This is concerning especially when physical activity is used to combat the enhanced health risks consequent with sedentarism and chronic disease. The reasons for this non-response are poorly understood, although it may be related to participants’ baseline status, habitual physical activity, dietary practices, genetics, and the traits of the exercise regime (Mann et al. 2014). Common practice when implementing HIIT is to use a “one size fits all” approach, in which the clinician or scientist employs an identical HIIT regime in each participant. However, this approach does not follow recent recommendations (Buford et al. 2013) concerning personalizing exercise training to maximize the training response.
In this feasibility study, we tested the effects of short-term HIIT prescribed according to VT on changes in VO2max and time trial performance. Previous studies in our lab (Wood et al. 2016; Green et al. 2017) demonstrate near-maximal values of oxygen uptake and BLa in response to acute bouts of interval training based on fractions of peak power output, yet the magnitude of these responses varies across individuals. Prescribing HIIT based on VT puts participants at an equivalent level of metabolic strain versus training at an absolute intensity based on heart rate or peak power output. It was hypothesized that this regime will elicit significant changes in our outcomes versus non-exercising controls, and lower incidence of non-response than rates equal to 20–50% reported in previous HIIT studies (Astorino and Schubert 2014; Gurd et al. 2016) in which peak power output was used to set training intensity.
Materials and methods
Participants
Healthy, physically active men and women who performed more than 150 min per week of exercise in the last year including resistance training, CrossFit,™ aerobic exercise, and non-competitive sport were recruited to participate in this study. Participants were non-obese, did not smoke, were not taking any medications or supplements, and had no physical condition which may alter their responses. Participants who served as controls (CON) were not randomized to this group, but were individuals who desired to complete the testing yet lacked the time to undergo training. Their physical characteristics are shown in Table 1. Their aggregate VO2max is classified as “fair” to “average” according to norms for adults aged 20–49 years old (ACSM 2018). There was no difference (p > 0.05) in any variable at baseline between individuals who completed training and CON except for body mass index. They provided written informed consent before participating in the study, and the protocol was approved by the CSU—San Marcos Institutional Review Board.
Study design
Participants undergoing HIIT performed 3 days per week of training for 3 weeks, whereas CON completed pre- and post-testing which were separated by 3 weeks. For all sessions, participants arrived well-rested and hydrated, and followed a 3 h fast and 24 h abstention from intense physical activity, which were confirmed with a written log. In addition, participants completed a 24 h food log at baseline which was replicated for all subsequent assessments. All sessions were held at the same time of day ± 60 min within subjects. Participants were instructed to maintain their habitual physical activity and dietary patterns during the study, which were confirmed using written logs submitted at the end of the study. Temperature and relative humidity of the lab were maintained at 18–21 °C and 40–60%, respectively. Strong verbal encouragement was provided during all sessions.
Baseline testing
Initially, participant height and body mass were determined using a calibrated scale. After 5 min of seated rest, a fingertip blood sample was taken to assess blood lactate concentration (BLa) using a lancet (Owen Mumford, Inc., Marietta, GA) and portable monitor (Lactate Plus, Nova Biomedical, Waltham, MA). Then, they were prepared for incremental exercise to exhaustion on an electrically braked cycle ergometer (Velotron Dynafit Pro, RacerMate, Seattle, WA). After a 2 min warm-up at 40–70 W, work rate was increased in a ramp-like manner by 20–35 W/min until volitional exhaustion. Maximal BLa was also determined through acquisition of another fingertip sample 3 min post-exercise.
After 10 min of light pedaling at 10%PPO, participants pedaled “all-out” at a supramaximal work rate equal to 105%PPO to verify attainment of VO2max. This constant load test performed at a work rate above that eliciting VO2max has been identified as a robust approach to confirm VO2max attainment in many populations (Poole and Jones 2017). They underwent a 25 min passive recovery, then initiated 5 min of pedaling at 20%PPO, followed by a 5 mile cycling time trial on the same cycle ergometer using the flat course (Velotron 3D software). This was used to familiarize participants with a cycling time trial. This program displays the participant on the computer screen competing against an avatar. Participants were instructed to use the gears to go as fast as they could during the bout. No information was given to participants other than gearing, distance covered, and distance remaining, which were continuously shown on the computer screen. Settings for seat/bar height of the cycle ergometer were recorded and used for all subsequent sessions. On the following two sessions, participants followed the aforementioned pre-test guidelines, then warmed up for 3 min at each of 10 and 20%PPO prior to repeating the 5 mile time trial. The fastest time from any of these three sessions was selected as their measure of baseline cycling performance.
High-intensity interval training
Training was supervised and consisted of nine sessions of low-volume HIIT. Before each session, participants completed a 5 min warm-up at 10%PPO. During sessions 1–3, 4–6, and 7–9, participants completed 8, 9, and 10 60 s bouts of HIIT, with each bout separated by a 75 s recovery at 10%PPO. Intensity was set at 130% of the power output associated with each individual’s VT. On day 1 and 9 of HIIT, BLa was determined via fingertip blood samples taken pre-exercise and after bout 4 and 8. Also on these days, enjoyment of training was determined using the Physical Activity Enjoyment Scale (PACES, Kendzierski and DeCarlo 1991). This 18-item survey was completed 10 min post-exercise and consists of various questions on a 1–7 Likert scale.
Post-testing
Following procedures outlined above, measures of VO2max and TT performance were repeated at the same time of day a minimum of 48 h after the last training session. At least 48 h was allotted between these sessions in all participants. Participants in the control group completed these sessions 3 weeks after the last baseline session.
Measures
During ramp exercise, gas exchange data were acquired every 30 s using a metabolic cart (ParvoMedics True One, Sandy, UT) which was calibrated before exercise according to the manufacturer. VO2max was identified as the mean of two highest 30 s values taken from the last 60 s of progressive exercise. Peak power output was identified as that work rate (in Watt) coincident with volitional exhaustion. During all sessions, heart rate (HR) was assessed using telemetry (Polar Electro, Woodbury, NY). Oxygen pulse was calculated as the quotient of VO2 (mL/min) and HR. To assess the ventilatory threshold, two experimenters independently examined plots of change in the ventilatory equivalents of oxygen and carbon dioxide (VEVO2 and VEVCO2) versus time, using the criterion developed by Caiozzo et al. (1982) of “the time at which VEVO2 exhibited a systematic increase without a concomitant increase in VEVCO2.” If disagreement occurred between these individuals, a third researcher was consulted. This value was expressed in Watt as well as a percentage of PPO and HRmax. To estimate changes in time trial performance, cycling time (seconds) and mean power output (in Watt) were recorded. A 3-day food log including one weekend day was completed before and at the end of the study. Participants were requested to list specific names, volumes, and preparation of various foods. This information was analyzed using commercially available software (http://ndb.nal.usda.gov/ndb/foods/list) to determine total energy (in kilocalories) as well as macronutrient intake (in grams).
Determination of typical error
As used in a prior study (Raleigh et al. 2016), typical error (TE) was computed using data from our control participants using the following equation: TE = SDdiff/√2. In this equation, SDdiff is the standard deviation of the change scores between the two repeated tests. A nonresponder for each outcome was defined as an individual who failed to demonstrate a change greater than 2 × TE (0.12 L/min, 21.2 s, and 19.4 W for VO2max, time trial performance, and VT, respectively). This approach was used as it represents a threshold past which the odds of a real change are 12:1 (Hopkins 2000).
Data analyses
Data are expressed as mean ± SD and were analyzed using SPSS Version 24.0 (Chicago, IL). The Shapiro–Wilks test was used to assess normality. Independent t test was performed to identify differences in demographic and physiological variables between groups at baseline as well as the change in VO2max, time trial performance, and VT. Repeated two-way ANOVA (time = pre versus post, group = HIIT versus CON) with repeated measures was performed to identify differences in VO2max, gas exchange variables, time trial performance, and BLa. The Greenhouse–Geisser correction was used to account for the sphericity assumption of unequal variances across groups. If a significant F ratio occurred, Tukey’s post hoc test was used to identify differences between means. Cohen’s d was used as an estimate of effect size, and 95% confidence intervals (95% CI) were used as appropriate. Pearson pairwise correlation was used to determine relationships between variables. Statistical significance was set as p < 0.05.
Results
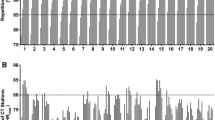
There was 100% compliance to HIIT. The average intensity of training was equal to 89.8 ± 5.4%PPO (range 79.2–96.0%PPO). Figure 1 shows that heart rate gradually increased (p = 0.02) during training, and that participants trained at workloads surpassing 90%HRmax. Enjoyment as measured with PACES did not change from session 1 to 9 (104.4 ± 14.8 versus 101.8 ± 19.4, p = 0.34).
Change in VO2max and gas exchange data
Data showed a significant time × group interaction for relative (p = 0.002) and absolute VO2max (p = 0.007), as it was increased by 0.16 ± 0.13 L/min (95% CI − 0.08 to 0.23 L/min) with HIIT which was higher (p = 0.005) than the change seen in CON (0.008 ± 0.12 L/min, 95% CI − 0.06 to 0.08 L/min). Post hoc analyses showed that the post-training value was higher than at baseline. In CON, only two participants showed changes in VO2max (0.15 and 0.29 L/min, respectively) which were greater than TE. Similar time × group interactions were revealed for PPO (p = 0.016), VCO2 (p = 0.002), and O2 pulse (p = 0.018). There was no time × group interaction for VE (p = 0.14), HR (p = 0.53), RER (p = 0.95), or BLa (p = 0.36). Our results from the ramp and verification test are shown in Table 2.
Change in time trial performance
There was a significant time × group interaction (p = 0.003) for cycling performance as it was improved with HIIT (936 ± 80 s versus 913 ± 78 s, d = 1.13) versus CON (915 ± 99 s versus 928 ± 88 s, d = 0.68). The mean change was different (p = 0.003) between HIIT (− 23 ± 20 s, 95% CI − 35 to − 11 s) and CON (14 ± 27 s, 95% CI − 8 to 35 s). Eight of 14 individuals in CON showed slower time trial performance at the post-test versus baseline, although one exhibited improved performance by 57 s. A similar interaction (p = 0.004) was shown for mean power output which was significantly increased in HIIT (171 ± 42 W versus 184 ± 41 W, d = 1.04) compared to CON (187 ± 45 W versus 180 ± 40 W, d = 0.70).
Change in ventilatory threshold
Compared to CON, absolute VT (p = 0.005) and VT expressed as %HRmax increased (p = 0.014) in response to HIIT. However, VT relative to %VO2max did not change (p = 0.30). The change in VT (p = 0.005 versus CON) was equal to 9 ± 12 W (95% CI 2 to 16 W) with HIIT and − 6 ± 14 W (95% CI − 14 to 2 W) in CON, respectively. No participant in CON showed a meaningful change in absolute VT between pre- and post-testing.
Individual responses
Table 3 shows individual changes in our outcomes for all 14 participants in both the HIIT and CON groups. Of those who performed HIIT, the frequency of participants showing a change in VO2max, time trial performance, and VT that was greater than 2 × TE was 8/14, 8/14, and 5/14, respectively. One participant showed a change in all outcomes, and 50% of participants showed a meaningful change in 2 of 3 outcomes. In contrast, two participants showed no change in all outcome measures.
Change in blood lactate concentration
Results showed a significant increase in BLa during HIIT (p < 0.001), yet there was no change in exercise BLa (p = 0.91) from session 1 (1.4 ± 0.5, 9.6 ± 2.6, 11.9 ± 2.2 mM) to session 9 of HIIT (1.3 ± 0.5, 9.5 ± 2.4, 11.6 ± 2.3 mM).
Correlation analyses
There was no correlation between the %PPO attained during HIIT and the absolute change in VO2max (r = 0.07, p = 0.82), VT (r = 0.19, p = 0.52), or time trial performance (r = 0.38, p = 0.18). Similar lack of relationships were shown between peak HR attained during HIIT and change in VT (r = − 0.35, p = 0.21) and time trial performance (r = 0.02, p = 0.96), although there was an association for change in VO2max (r = 0.61, p = 0.02). No correlation was shown (r = 0.33, p = 0.25) between baseline VO2max and the absolute change observed in response to HIIT.
Change in habitual physical activity and dietary intake
Physical activity decreased (p = 0.03) from baseline to post-testing, yet there was no group × time interaction (p = 0.07). Post hoc analyses showed a maintenance of physical activity in HIIT (5.6 ± 1.7 h/week versus 5.3 ± 1.8 h/week, d = 0.16), yet a decline in physical activity in CON (5.8 ± 2.0 h/week versus 4.8 ± 1.9 h/week, d = 0.55). There was no change in overall energy or macronutrient intake (p = 0.39–0.69) or group × time interaction (p = 0.57–0.95). Calorie intake as well as carbohydrate, fat, and protein intake were not different from pre- to post-testing in HIIT (2,050 ± 686 kcal and 251 ± 103, 69 ± 26, 109 ± 49 g to 2074 ± 639 kcal and 248 ± 96, 71 ± 26, 119 ± 55 g) or CON (2,333 ± 587 kcal and 308 ± 91, 72 ± 23, and 117 ± 42 g to 2,358 ± 557 kcal and 305 ± 93, 74 ± 24, 122 ± 44 g).
Discussion
In the present study, we examined changes in cardiorespiratory fitness and cycling performance in response to nine sessions of HIIT which was personalized for each participant based on their ventilatory threshold. This approach opposes how HIIT is traditionally implemented using a specific percentage of PPO or HRmax, which may elicit a dissimilar metabolic stimulus to training. Our aggregate results demonstrate significant increases in VO2max, cycling performance, and VT in response to our regime, which elicited intensities characteristic of HIIT (85–100%HRmax, Gibala et al. 2014), versus a non-exercising control group. However, some participants showed no change in each variable, which corroborates existing findings denoting individual responses to HIIT. It is plausible that a greater volume of HIIT should be implemented to elicit responses in all participants.
Results from a recent systematic review of 32 studies (Weston et al. 2014b) report a mean improvement in VO2max equal to 6.2% in response to low-volume HIIT ranging in duration from 2 to 10 weeks. Our data exhibited a 6% increase in VO2max, which is similar to that reported in two recent studies (Boyd et al. 2013; Raleigh et al. 2016) in which 9 and 12 sessions of HIIT were performed over a 3 week period. Although we did not measure stroke volume or cardiac output, the significant increase in O2 pulse, which has been shown to be associated with stroke volume (Bhambhani et al. 1994), suggests that oxygen delivery was increased in response to HIIT, leading to the increases in VO2max. This contention is supported by data from studies (Warburton et al. 2004; Astorino et al. 2017) in active men and women showing significant increases in stroke volume and cardiac output in response to chronic low-volume HIIT.
Despite the overall increase in VO2max demonstrated, 6 of 14 participants showed no meaningful change in VO2max in response to HIIT (Table 3). This finding is corroborated by previous studies showing that many participants do not exhibit increases in VO2max in response to HIIT (Boyd et al. 2013; Astorino and Schubert 2014) or SIT (Gurd et al. 2016). In sedentary men (Boyd et al. 2013), 9 sessions of HIIT at 100%PPO led to a greater increase in VO2max as well as lower frequency of non-response (0%) than HIIT conducted at 70%PPO (44%). Gurd et al. (2016) reported VO2max non-response rates ranging from 30 to 50% in response to SIT regimes performed 3 days per week for 4 weeks, which is similar to the frequency reported in the present study. However, when SIT was performed 4 days per week (Ma et al. 2013; Scribbans et al. 2014), there was no incidence of non-response in VO2max. Exercise intensity (Ross et al. 2015) and volume (Sisson et al. 2009) have been shown to be key mediators of the magnitude of response to MICT, although it is unclear if this relationship also exists for HIIT. For example, Raleigh et al. (2016) showed that 3 weeks of lower-intensity interval training (83%PPO) led to a lower increase in VO2max than more intense regimes completed at 112 and 130%PPO, although these data are refuted by other studies (Astorino et al. 2013; Matsuo et al. 2014) in which no differences in VO2max response were shown between HIIT regimes differing in intensity. However, the latter two studies were 8 and 12 weeks in duration, and it is possible that the greater volume of training led to these discrepant results. We encourage scientists to initiate studies attempting to identify whether modifying training intensity or volume is key to minimizing non-response. Overall, these results suggest that an adequate volume of HIIT or SIT must be attained to ameliorate non-response to a small dose of training, and it is likely that every individual has a different sensitivity to training.
Our results show a 2.5% improvement in cycling performance in response to HIIT. Fifty-seven percent of participants reported a meaningful increase in this outcome, ranging from a 23–59 s improvement in performance post-training. Of those individuals who did not show improvement for this variable, only two exhibited no absolute increase in performance, and in fact, those two participants showed no change in all outcome measures. Nevertheless, our aggregate data corroborate previous studies showing improved cycling performance with various HIIT regimes. In active men and women (Perry et al. 2008), time to exhaustion at 90%VO2max was increased by 111% in response to 18 sessions of high-volume HIIT. Increased cycling performance was also shown in response to low-volume SIT (Hazell et al. 2010) and low-volume HIIT (Little et al. 2010). Measures obtained in the present study do not explain why cycling performance was improved, although it is likely that oxidative capacity was enhanced in our participants as previously shown (Little et al. 2010). In addition, increased buffering capacity has been repeatedly shown in men and women undergoing 2 weeks of SIT (Gibala et al. 2006) as well as in cyclists undergoing HIIT (Weston et al. 1997), which is related to greater tolerance of high-intensity exercise and in turn, enhanced exercise performance (Weston et al. 1997).
Over 30 years ago, Poole and Gaesser (1985) showed that 8 weeks of high-volume HIIT performed by untrained men led to significant increases in VT which were superior to the change shown with MICT. In active women, 7 weeks of high-volume HIIT also enhanced VT by a similar magnitude (Burke et al. 1994). Similarly, only 4 sessions of high-volume HIIT increased VT in trained cyclists (Laursen et al. 2002). The mechanisms explaining the increase in VT reported in the current study are beyond the scope of this paper, yet are likely due to improvements in oxidative capacity demonstrated with HIIT (Henriksson and Reitman 1976). Despite our aggregate increase in absolute VT, only 5/14 participants exhibited a meaningful change in this measure. Part of this result is likely due to the large typical error seen in this variable (11% of the pre-training value), which meant that our participants needed to exhibit a more substantial change for this response to be meaningful. In fact, five participants showed increases in VT between 6 and 12 W in response to HIIT. Poole and Gaesser (1985) reported an ICC = 0.96 for repeated determinations of VT using the ventilatory equivalents method (Caiozzo et al. 1982) which was similar to our value (ICC = 0.95) obtained in the control group. Further study is merited to measure HIIT-derived changes in VT based on the relationship between VT and exercise tolerance (Rusko et al. 1980).
The current study has some limitations. Our data were acquired in a young and active population, so our results cannot be applied to older or inactive individuals. We chose a training intensity equal to 130%VT, which represented approximately 90%PPO in our sample. Preliminary testing demonstrated that this intensity would be challenging for our habitually active population, yet will not elicit extreme fatigue which may decrease their tolerance to training. Whether a slightly lower or higher intensity will elicit the same effects is unknown. The HIIT group was comprised of more women than men; however, the effect of gender on magnitude of response to interval training is likely small, considering that short- and long-term training studies conducted in healthy adults as well as clinical populations (Astorino et al. 2011, 2017; Metcalfe et al. 2016; Phillips et al. 2017; Storen et al. 2017) show no difference in response between men and women. In addition, Skelly et al. (2017) showed that men and women exhibit significant albeit similar increases in various genes encoding mitochondrial biogenesis, metabolic control, and structural remodeling in response to a single bout of SIT. We chose not to recruit a comparator group of persons completing HIIT at a specific %PPO or %HRmax, as individual responses have repeatedly been shown in previous studies in active adults (Astorino and Schubert 2014; Gurd et al. 2016). Lastly, this was a feasibility study testing the utility of HIIT based on ventilatory threshold, and additional long-term studies are needed to clarify efficacy of personalized HIIT prescription using this approach. Despite these limitations, our study is strengthened by the use of best practices (Hopkins 2000; Poole and Jones 2017) for assessment of time trial performance and VO2max, which enhances reliability of these measures. In addition, we monitored habitual physical activity and dietary patterns during the study which may alter training responsiveness (Mann et al. 2014). Following previous recommendations (Atkinson and Batterham 2015), typical error was computed from repeated testing of individuals of similar fitness and age versus the intervention group, and this value was computed from data obtained in our lab versus using typical error values acquired by other authors who use different methodologies. Moreover, it was determined over the same time frame as those who performed HIIT (Atkinson and Nevill 1998), which should lead to a similar degree of random variation in our measures. Nevertheless, standard deviation of the change scores for VT and time trial performance in the control group were slightly greater than values in the intervention group, which is likely attributed to the gender disparity between groups. We recommend that scientists repeat baseline testing in the intervention group, which would allow examination of training responsiveness based on individual variability rather than that of a comparator (control) group.
Conclusion
Our results demonstrate the feasibility of short-term HIIT prescribed using ventilatory threshold, which led to significant improvements in VO2max and cycling performance in young adults compared to a control group. Nevertheless, this personalized approach to HIIT led to individual response in select variables, in that some participants showed meaningful increases in our measures; whereas, others showed a maintenance of their values, which supports recent findings and is likely due to an inadequate quantity of training. Compared to previous studies showing significant increases in VO2max and cycling performance in response to similar albeit standardized HIIT regimes, our results do not demonstrate a superior effect of personalized HIIT based on ventilatory threshold.
Abbreviations
- BLa:
-
Blood lactate concentration
- CON:
-
Control group
- HIIT:
-
High-intensity interval training
- MICT:
-
Moderate-intensity continuous training
- PPO:
-
Peak power output
- SIT:
-
Sprint interval training
- TE:
-
Typical error
- VT:
-
Ventilatory threshold
- VO2max :
-
Maximal oxygen uptake
References
American College of Sports Medicine (2018) Guidelines for exercise testing and prescription. 9th edn. Lippincott, Williams, and Wilkins, Philadelphia
Astorino TA, Schubert MM (2014) Individual responses to completion of short-term and chronic interval training: a retrospective study. PLoS One 9(5):e97638
Astorino TA, Allen RP, Roberson DW et al et al (2011) Adaptations to high-intensity training are independent of gender. Eur J Appl Physiol 111(7):1279–1286
Astorino TA, Schubert MM, Palumbo E et al (2013) Magnitude and time course of changes in maximal oxygen uptake in response to distinct regimens of chronic interval training in sedentary women. Eur J Appl Physiol 113(9):2361–2369
Astorino TA, Edmunds RM, Clark A et al (2017) High intensity interval training increases cardiac output and VO2max. Med Sci Sports Exerc 49(2):265–273
Atkinson G, Batterham AM (2015) True and false interindividual differences in the physiological response to an intervention. Exp Physiol 100:577–588
Atkinson G, Nevill AM (1998) Statistical methods for assessing measurement error (reliability) in variables relevant to sports medicine. Sports Med 26:217–238
Bhambhani Y, Norris S, Bell G (1994) Prediction of stroke volume from oxygen pulse measurements in untrained and trained men. Can J Appl Physiol 19(1):49–59
Boyd JC, Simpson CA, Jung ME, Gurd BJ (2013) Reducing the intensity and volume of interval training diminishes cardiovascular adaptation but not mitochondrial biogenesis in overweight/obese men. PLoS One 8(7):e68091
Buford TW, Roberts MD, Church TS (2013) Toward exercise as personalized medicine. Sports Med 43(3):157–165
Burgomaster KA, Howarth KR, Phillips SM et al (2008) Similar metabolic adaptations during exercise after low volume sprint interval and traditional endurance training in humans. J Physiol 586(1):151–160
Burke J, Thayer R, Belcamino M (1994) Comparison of effects of two interval-training programmes on lactate and ventilatory thresholds. Br J Sports Med 28(1):18–21
Caiozzo VJ, Davis JA, Ellis JF, Azus JL, Vandagriff R, Prietto CA, McMaster WC (1982) A comparison of gas exchange indices used to detect the anaerobic threshold. J Appl Physiol 53(5):1184–1189
Centers for Disease Control and Prevention (2014) Press release: one in five adults meet physical activity guidelines. Department of Health and Human Services. Atlanta, GA: U.S
Coffey VG, Hawley JA (2007) The molecular bases of training adaptation. Sport Med 37:737–763
Dalleck LC, Haney DE, Buchanan CA, Weathermax RM (2016) Does a personalized exercise prescription enhance training efficacy and limit training unresponsiveness? A randomized controlled trial. J Fit Res 5(3):15–27
Garber CE, Blissmer B, Deschenes MR et al (2011) Quantity and quality of exercise for developing and maintaining cardio-respiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc 43:1334–1359
Gibala MJ, Little JP, van Essen M et al (2006) Short-term sprint interval versus traditional endurance training: similar initial adaptations in human skeletal muscle and exercise performance. J Physiol 575(3):901–911
Gibala MJ, Gillen JB, Percival ME (2014) Physiological and health-related adaptations to low-volume interval training: influences of nutrition and sex. Sports Med 44(2):127–137
Green N, Wertz T, LaPorta Z, Mora A, Serbas J, Astorino TA (2017) Comparison of acute physiological and psychological responses between moderate intensity continuous exercise and three regimes of high intensity training. J Str Cond Res (in press)
Gurd BJ, Giles MD, Bonafiglia JT et al (2016) Incidence of non-response and individual patterns of response following sprint interval training. Appl Physiol Nutr Metab 41(3):229–234
Hazell TJ, MacPherson REK, Gravelle BMR, Lemon PW (2010) 10 or 30-s sprint interval training bouts enhance both aerobic and anaerobic performance. Eur J Appl Physiol 110:153–160
Henriksson J, Reitman JS (1976) Quantitative measures of enzyme activities in type I and type II muscle fibres of man after training. Acta Physiol Scand 97(3):392–397
Hopkins WG (2000) Measures of reliability in sports medicine and science. Sports Med 30(1):1–15
Jelleyman C, Yates T, O’Donovan G et al (2015) The effects of high-intensity interval training on glucose regulation and insulin resistance: a meta-analysis. Obes Rev 16(11):942–961
Katch V, Weltman A, Sady S, Freedson P (1978) Validity of the relative percent concept for equating training intensity. Eur J Appl Physiol 39:219–227
Kendzierski D, DeCarlo KJ (1991) Physical activity enjoyment scale: two validation studies. J Sport Exerc Psychol 13(1):50–64
Laursen PB, Blanchard MA, Jenkins DG (2002) Acute high-intensity interval training improves Tvent and peak power output in highly trained males. Can J Appl Physiol 27(4):336–348
Little JP, Safdar A, Wilkin GP, Tarnopolsky MA, Gibala MJ (2010) A practical model of low-volume high-intensity interval training induces mitochondrial biogenesis in human skeletal muscle: potential mechanisms. J Physiol 588(6):1011–1022
Ma JK, Scribbans TD, Edgett BA et al (2013) Extremely low-volume, high-intensity interval training improves exercise capacity and increases mitochondrial protein content in human skeletal muscle. Open J Molec Integr Physiol 3:202–210
Mann TN, Lamberts RP, Lambert MI (2014) High responders and low responders: factors associated with individual variation in response to standardized training. Sports Med 44(8):1113–1124
Matsuo T, Saotome K, Seino S et al (2014) Effects of a low-volume aerobic-type interval exercise on VO2max and cardiac mass. Med Sci Sports Exerc 46(1):42–50
Metcalfe RS, Tardif N, Thompson D, Vollaard NB (2016) Changes in aerobic capacity and glycaemic control in response to reduced-exertion high-intensity interval training (REHIT) are not different between sedentary men and women. Appl Physiol Nutr Metab 41(11):1117–1123
Milanovic Z, Sporis G, Weston M (2015) Effectiveness of high-intensity interval training (HIT) and continuous endurance training for VO2max improvements: a systematic review and meta-analysis of controlled trials. Sports Med 45(10):1469–1481
Perry CGR, Heigenhauser GJF, Bonen A, Spriet LL (2008) High-intensity aerobic interval training increased fat and carbohydrate metabolic capacities in human skeletal muscle. Appl Physiol Nutr Metab 33(6):1112–1123
Phillips BE, Kelly BM, Lilja M et al (2017) A practical and time-efficient high-intensity interval training program modifies cardio-metabolic risk factors in adults with risk factors for type II diabetes. Front Physiol 8:229
Poole DC, Gaesser GA (1985) Response of ventilatory and lactate thresholds to continuous and interval training. J Appl Physiol 58(4):1115–1121
Poole DC, Jones AM (2017) Measurement of the maximum oxygen uptake (VO2max): VO2peak is no longer acceptable. J Appl Physiol 122(4):997–1002
Raleigh JP, Giles MD, Scribbans TD et al (2016) The impact of work-matched interval training on V̇O2peak and V̇O2 kinetics: diminishing returns with increasing intensity. Appl Physiol Nutr Metab 41(7):706–713
Ross R, de Lannoy L, Stotz PJ (2015) Separate effects of intensity and amount of exercise on interindividual cardiorespiratory fitness response. Mayo Clin Proc 90(11):1–9
Rusko H, Rahkila P, Karvinen E (1980) Anaerobic threshold, skeletal muscle enzymes and fiber composition in young female cross-country skiers. Acta Physiol Scand 108(3):263–268
Scharhag-Rosenberger F, Meyer T, Gässler N, Faude O, Kindermann W (2010) Exercise at given percentages of VO2max: heterogeneous metabolic responses between individuals. J Sci Med Sport 13(1):74–79
Scribbans TD, Edgett BA, Vorobej K et al (2014) Fibre-specific responses to endurance and low volume high intensity interval training: striking similarities in acute and chronic adaptation. PLoS One 9(6):e98119
Sisson SB, Katzmarzyk PT, Earnest CP, Bouchard C, Blair SN, Church TS (2009) Volume of exercise and fitness nonresponse in sedentary, postmenopausal women. Med Sci Sports Exerc 41(3):439–445
Skelly LE, Gillen JB, MacInnis MJ et al (2017) Effect of sex on the acute skeletal muscle response to sprint interval exercise. Exp Physiol 102(3):354–365
Støren Ø, Helgerud J, Sæbø M et al (2017) The effect of age on the VO2max response to high-intensity interval training. Med Sci Sports Exerc 49(1):78–85
Tamburus NY, Kunz VC, Salviati MR, Castello Simões V, Catai AM, Da Silva E (2016) Interval training based on ventilatory anaerobic threshold improves aerobic functional capacity and metabolic profile: a randomized controlled trial in coronary artery disease patients. Eur J Phys Rehabil Med 52(1):1–11
Trost SG, Owen N, Bauman AE, Sallis JF, Brown W (2002) Correlates of adults’ participation in physical activity: review and update. Med Sci Sports Exerc 34:1996–2001
Warburton DER, Haykowsky MJ, Quinney HA et al (2004) Blood volume expansion and cardiorespiratory function: effects of training modality. Med Sci Sports Exerc 36(6):991–1000
Weston AR, Myburgh KH, Lindsay FH, Dennis SC, Noakes TD, Hawley JA (1997) Skeletal muscle buffering capacity and endurance performance after high-intensity interval training by well-trained cyclists. Eur J Appl Physiol 75(1):7–13
Weston KS, Wisloff U, Coombes JS (2014a) High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: a systematic review and meta-analysis. Br J Sports Med 48(16):1227–1234
Weston M, Taylor KL, Batterham AM, Hopkins WG (2014b) Effects of low-volume high-intensity interval training (HIT) on fitness in adults: a meta-analysis of controlled and non-controlled trials. Sports Med 44(7):1005–1017
Wolpern AE, Burgos DJ, Janot JM, Dalleck LC (2015) Is a threshold-based model a superior method to the relative percent concept for establishing individual exercise intensity? a randomized controlled trial. BMC Sports Sci Med Rehabil 7:16
Wood KA, LaValle K, Greer K, Bales B, Thompson H, Astorino TA (2016) Effects of two regimens of high intensity interval training (HIIT) on acute physiological and perceptual responses. J Str Cond Res 30(1):244–250
Acknowledgements
The authors thank the participants for their dedication to the study as well as Anders Rosland Nordstrand for assistance with data collection.
Funding
No funding for this work was received from the National Institutes of Health or other entities.
Author information
Authors and Affiliations
Contributions
The corresponding author TAA conceived the study, recruited participants, collected and analyzed data, and wrote the manuscript. JR and TA assisted the corresponding author with development of the study protocol and helped him collect data and read and approved the final manuscript. EK, PH, SR, and NG helped the research team collect data and read and approve the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
There was no conflict of interest in the completion of this study.
Additional information
Communicated by I. Mark Olfort.
Rights and permissions
About this article
Cite this article
Astorino, T.A., deRevere, J., Anderson, T. et al. Change in VO2max and time trial performance in response to high-intensity interval training prescribed using ventilatory threshold. Eur J Appl Physiol 118, 1811–1820 (2018). https://doi.org/10.1007/s00421-018-3910-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-018-3910-3