Abstract
Purpose
In persons completing exhaustive daily exercise, sleep and energy restriction have been highlighted as risk factors for hypothermia in cold environments. The present study therefore sought to determine the effect of sleep deprivation (SDEP), with and without energy restriction, on the thermal response to cold.
Methods
In a random order, ten recreationally active men (mean ± SD: age 25 ± 6 years, body fat 17 ± 5 %) completed three 53 h trials: a control (CON: 436 min/night sleep), SDEP (0 min sleep), and sleep deprivation and energy restriction (SDEP + ER: 0 min sleep and 10 % daily energy requirements). Exhaustive exercise was completed after 5 and 29 h. After 53 h participants completed a semi-nude seated cold air test (CAT, 0 °C), for 4 h or until rectal core temperature (T re) reached 36 °C.
Results
Two nights of sleep and energy restriction did not impair the thermal response to cold (T re, CON 36.15 ± 0.20 °C, SDEP 36.30 ± 0.15 °C, SDEP + ER 36.25 ± 0.20 °C, P = 0.25). Rewarming was also similar as indicated by 1 h post-CAT T re (P = 0.78). In contrast, perceived thermal discomfort during the initial hour of the CAT tended to be greater after SDEP and SDEP + ER (P ≤ 0.1).
Conclusion
Sleep and energy restriction, at least as evaluated within this experiment, should be considered minimal risk factors for hypothermia. The greater perception of cold discomfort at the same body temperature suggests that sleep and energy restriction may actually reduce cold injury risk, as people are likely to engage earlier in normal behavioral cold adaptation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cold-induced injuries, including whole body hypothermia, are a recurrent medical problem for the military, emergency services, and outdoor enthusiasts such as walkers, mountaineers, and ultra-endurance athletes (Pugh 1966; Moran et al. 2003). In addition to cold exposure, these persons are routinely exposed to multiple stressors, such as exhaustive exercise, energy restriction, and sleep loss, which are frequently cited in reviews and position statements to increase the risk of hypothermia (Rintamäki 2000; Castellani et al. 2006; Cappaert et al. 2008). Unfortunately, it is not possible to determine the independent effects of these variables on thermoregulation and hypothermia risk from previous studies that used multiple stressors simultaneously (Young et al. 1998; Castellani et al. 2003).
The heightened hypothermia risk reported in the aforementioned multi-stressor studies (Young et al. 1998; Castellani et al. 2003) may be related to disrupted sleep, as sleep deprivation precludes normal behavioral cold adaptation (e.g., increased bedding for insulation) that prevents heat loss during the normal nocturnal increase in skin blood flow (Van Someren 2006). Further, during cold exposure, core temperature has been shown to decline more quickly after one night of sleep loss than after a normal nights sleep (Landis et al. 1998). Whether sleep loss alters thermal responses or impairs cold tolerance is, however, unclear as other studies report no effect of one night’s sleep loss on thermal responses during cold exposure (Caine-Bish et al. 2004). Moreover, as these sleep loss studies have examined the effect of one night’s sleep loss only, the effect of more prolonged sleep disruption remains unclear.
The studies examining the effect of a single night’s sleep loss on thermal responses to cold have included participants that were well rested and fed before the cold exposure. This contrasts the multi-stressor studies that suggest increased hypothermia risk where participants were not only sleep deprived but also in negative energy balance because of exhaustive exercise and inadequate energy intake (Young et al. 1998; Castellani et al. 2003). As chronic underfeeding, short-term fasting and hypoglycaemia have previously been reported to impair thermal and metabolic responses to cold, i.e., poorer peripheral vasoconstriction and shivering thermogenesis (Gale et al. 1981; Macdonald et al. 1984; Mansell and Macdonald 1989; Mansell et al. 1990), it is possible the impaired thermal responses observed in the multi-stressor studies are related to a combination of sleep loss and energy restriction. Determining the relative influence of these stressors is necessary if clear cold injury risk guidelines and countermeasures are to be developed.
The aim of the present study therefore was to examine the effect of 2 nights (53 h) sleep deprivation, with and without energy restriction, on the thermal response to cold air exposure in a controlled laboratory setting. In this setting, using the random allocation of trials and precise prescription and monitoring of exercise, diet and sleep, the confounders of the previous multi-stressor field studies could be reduced (Young et al. 1998; Castellani et al. 2003). Further, the effect of sleep deprivation could be isolated, and with the addition of energy restriction in a separate trial, it could be determined whether the multi-stressor scenario of sleep loss and negative energy balance further impairs thermal responses to cold. To better simulate active populations such as soldiers and rescue workers, participants also completed exhaustive exercise each day. To assess the thermal response, we chose in this study to use a combination of thermometry (core and skin temperatures), indirect calorimetry (metabolic heat production), plasma glucose and catecholamine responses (where norepinephrine was used to estimate peripheral vasoconstriction function), and subjective measures of thermal discomfort. We hypothesised that 53 h of sleep deprivation would impair the thermal response to cold and that energy restriction would exacerbate this response reducing cold tolerance.
Methods
Participants
Ten healthy, recreationally active men (mean ± SD: age 25 ± 6 years, height 178 ± 4 cm, nude body mass 78.9 ± 8.2 kg, body fat 17 ± 5 %, maximal oxygen uptake (VO2max) 57.4 ± 8.4 ml/kg/min) volunteered to participate in the study. Participants gave written informed consent before the study, which received local University Ethics Committee approval. Participants reported no symptoms of infection, and did not take medication or nutritional supplements during the study, or in the 6 preceding weeks. Participants were also asked to refrain from alcohol and caffeine for 72 h, and exercise for 24 h before preliminary testing and each experimental trial. All procedures were in accordance with current local ethics guidelines and the declaration of Helsinki.
Preliminary testing
Before the main experimental trials, a familiarization was performed. Participants were transported to the laboratory for the familiarization arriving at 0800 h after an overnight fast. After bowel and bladder voiding, participants’ height, nude body mass, and body composition were obtained by stadiometer, weighing scales, and dual-energy x-ray absorptiometry (QDR1500, Hologic QDR1500, Bedford MA, USA). Resting metabolic rate was determined by indirect calorimetry (Compher et al. 2006) and adjusted by a general daily physical activity and diet-induced thermogenesis factor coefficient of 1.2 (Todorovic and Micklewright 2004). Participants were then familiarized with a 20-min cold air test (CAT), which was conducted in an environmental chamber (WIR Series, Design Environmental Ltd., Ebbw Vale, UK) set at 0 °C and 40 % relative humidity (RH).
After a 30 min rest, VO2max was estimated by means of indirect calorimetry (Cortex Metalyser 3B, Biophysik, Leipzig, Germany) during a continuous incremental exercise test to volitional exhaustion on a motorized treadmill (h/p/cosmos Mercury 4.0, Nussdorf-Traunstein, Germany). The treadmill walking speed (6.0 ± 0.5 km/h) and gradient (6.9 ± 2.0 %) that elicited 50 % VO2max, for the participants’ steady state exercise during trials, was then determined for each individual. In addition, each participant completed a time trial familiarization. Blinded to the treadmill speed, participants controlled the speed of the motorized treadmill, set at a 1 % gradient, and were instructed to complete 5 km as quickly as possible. Estimated energy expenditure for steady state exercise and the time trial was predicted by indirect calorimetry (Weir 1949), and was combined with the adjusted resting metabolic rate to predict daily energy expenditure. This energy expenditure was then used to calculate energy intake for the experimental trials.
Experimental trials
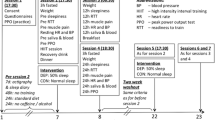
In a randomized, repeated measures design, participants completed three experimental trials separated by 12 days (Fig. 1). The three experimental trials involved a control trial (CON), a sleep deprivation trial (SDEP), and a sleep deprivation and energy restriction trial (SDEP + ER). Participants were allowed normal nocturnal sleep on the CON (436 ± 21 min/night), but were deprived of sleep for 53 h on SDEP and SDEP + ER (0 min/night). Dietary intake was provided to meet predicted total daily energy requirements (13.9 ± 0.7 MJ, carbohydrate 54 ± 2 %, fat 32 ± 1 %, protein 14 ± 1 %) during CON and SDEP, with energy intake restricted by 90 % for 53 h during SDEP + ER (total energy deficit 27.3 MJ). Water was provided during each experimental trial, at 2-h intervals (divided equally over 16 h; 0700–2300 h), equivalent to 35 ml/kg body mass/day (2785 ± 300 ml/day, Todorovic and Micklewright 2004), with estimated fluid losses during exercise added to this total. Daily physical activity was monitored via electronic pedometers (Digi-walker SW-200, Yamax, Tokyo, Japan), and the participants’ sleep wake cycles were monitored by accelerometry (GT1 M, ActiGraph LLC, Florida, USA, Ancoli-Israel et al. 2003). Participants remained in the laboratory building, complete with living quarters, for the entire duration of each experimental trial and they were supervised at all times. When not in the laboratory for measurements participants resided in comfortable living quarters and completed deskwork, played board and video games and watched television.
Schematic of trial events. Adapted from Costa et al. 2010. Samples, nude body mass, urine and blood samples, and nude body mass blood; TT time trial, RH relative humidity
Experimental procedures
The day before each experimental trial, participants were provided with their estimated daily energy and fluid intake requirements in order to standardize dietary intake and hydration status. The sleep duration on the night before trials was also monitored by accelerometry. After being woken at 0700 h, participants were transported to the laboratory. Upon arriving at the laboratory and after 15 min seated rest, a blood sample was collected without venestasis by venepuncture from an antecubital vein at 0800 h. Participants then voided their bladders into 24 h urine collection containers. Nude body mass was then recorded. Thereafter, nude body mass, blood, and urine samples were collected at 24 h, 48 h, immediately before the CAT, and immediately after the CAT. The blood samples obtained were predominantly for the assessment of immune function as reported previously (Costa et al. 2010). At 1200 h on day one (5 h into each trial) and day two (29 h into each trial), participants performed a 90 min steady state walk at 50 % VO2max, followed by a 15-min seated rest and then a 5-km time trial. During this exercise, ratings of perceived exertion (RPE) were obtained. The exercise protocol was performed in an air-conditioned laboratory (20 ± 1 °C, 59 ± 7 % RH) with a fan that generated a wind velocity of 2.3 m/s placed one meter in front of the participant. Water was consumed ad libitum during the steady state walks in all trials. No fluids were permitted during the time trial.
Cold air test
At 1100 h on day 3, participants were fitted with contact skin thermistors (Grant EUS-U thermistors; Grant 2020 Squirrel data logger, Shepreth, UK) affixed with tape to the right side of the body at four sites (chest, thigh, biceps, and calf). To monitor core temperature, participants also inserted rectal thermistor 12 cm beyond the external anal sphincter (Grant REC soft insertion probe; Grant 2020 Squirrel data logger, Shepreth, UK). After the pre-CAT blood draw and before entering the environmental chamber rectal core temperature (T re), skin temperature and ratings of perceived thermal comfort (McGinnis 13-point scale, 1 = so cold I am helpless to 7 = comfortable to 13 = so hot I am sick and nauseated, Hollies and Goldman 1977) and pain sensation to cold (10-point scale, 1 = barely cool to 10 = unbearable pain, Chen et al. 1998) were recorded. These readings were taken after a 15-min seated rest where participants were clothed in athletic shorts, shoes, and socks only. A baseline 2-min resting expired gas sample was then collected into a 150 L Douglas bag and analyzed by indirect calorimetry.
In the same attire, at 1200 h (53 h into each trial), participants were assisted onto a standard wooden laboratory chair in the environmental chamber. Ambient conditions throughout the CAT were regulated at 0 °C, 40 % RH and 0.2 m/s wind velocity. During the CAT, T re was recorded at 5-min intervals. Skin temperatures and Douglas bag expired gas samples were acquired at 10-min intervals, as were thermal comfort and pain sensation ratings. Participants were instructed to minimize any movement, including behavioral cold adaptation (i.e., huddling and fidgeting) during the CAT and assumed a standardized seated position, with hands on their knees. Participants remained in the environmental chamber for 4 h or until a time that T re reached 36 °C. Cold tolerance was therefore defined as the ability to maintain T re above 36 °C.
During the first hour after participants exited the environmental chamber, T re was recorded at 5-min intervals, whilst participants remained in an air-conditioned laboratory (20 ± 1 °C, 59 ± 7 % RH) seated and wrapped tightly in a blanket. One hour after the CAT recovery period, participants showered, re-clothed, and consumed a standardized meal (5.2 MJ, 58 % carbohydrate, 28 % fat, 14 % protein). 2 h after the CAT the trial was complete and participants were transported home.
Calculations
Four skin surface temperatures were used to calculate mean skin temperature (mean T sk) using an area-weighted equation, adjusted for regional proportions (Ramanathan 1964):
From the Douglas bag expired gas samples, values for respiratory exchange ratio (RER) and VO2 were obtained and used along with body surface area (A D) to estimate metabolic heat production (M) in W/m2 during the CAT as follows (Gagge and Gonzalez 1996):
Blood analyses
Blood samples were collected into four separate vacutainer tubes (Becton–Dickinson, Oxford, UK), two containing EDTA, and two containing lithium heparin. Blood in one of the tubes containing EDTA was used to determine hemoglobin concentration in triplicate using a hematology analyzer (Beckman Coulter Gen S, Fullerton, CA). Hematocrit (heparinized blood) was determined in triplicate using the capillary method, and plasma volume changes were estimated (Dill and Costill 1974). The second EDTA tube and the second lithium heparin tube were centrifuged at 1500 g for 10 min at 4 °C. Plasma was aspirated and then stored at −80 °C for further analysis. Plasma concentration of glucose (heparinized plasma) was determined using a spectrophotometric kit (Randox, County Antrim, UK). Aliquots of K3EDTA plasma were used for the determination of epinephrine and norepinephrine using high-pressure liquid chromatography (Clinrep complete kit for catecholamines, Recipe Chemicals, Munich, Germany) as described previously (Chudalla et al. 2006).
Data and statistical analyses
Based on the typical standard deviation of T re of 0.25 °C (Consolazio et al. 1963), and using standard alpha (0.05) and beta values (0.8), a sample size of ten was calculated (G*Power, Version 3.1.2) and estimated to have adequate statistical precision to detect a 0.25 °C difference in T re during the CAT between CON and either SDEP or SDEP + ER (two-tailed). A 0.25 °C difference in core temperature is also within a level of detection that is clinically important. For example, the upper clinical thresholds for mild hypothermia are 2 °C lower than typical resting core temperatures (Zafren et al. 2014). All statistical analyses were completed using a computerized statistical software package (GraphPad Prism version 6 for Windows, GraphPad Software, La Jolla California USA). Statistical significance was accepted at P < 0.05. Pre-CAT and CAT thermal variables were analyzed using repeated measures analyses of variance (ANOVA) with appropriate post hoc tests. Initial CAT thermal responses were compared between trials by two-way within-groups ANOVA using the first 60 min of the CAT because all participants completed at least this duration. To compare later CAT thermal responses between trials, a one-way ANOVA was also used. To achieve these comparisons, each individual’s shortest CAT duration was determined (105 ± 35 min, range 66–162 min), and the final thermal response before this time compared by one-way ANOVA. To determine if cold tolerance was different between trials, Kaplan–Meier survival curves were also generated and log-rank (Mantel-Cox χ 2) test completed. One-way within-groups ANOVA was also used to compare trial data including sleep duration, body mass, urine osmolality, trial physical activity, 90 min walk, and time trial. Unless otherwise stated all data are presented as mean ± SD.
Results
Pre-trial sleep duration, body mass, and hydration status
Pre-trial sleep duration, monitored by accelerometry, was similar and averaged 444 ± 30 min/night (P = 0.41). Also similar before trials began was nude body mass (78.8 ± 8.2 kg, P = 0.63) and urine osmolality (503 ± 195 mOsmol/kg P = 0.32).
Trial sleep duration and physical activity
Sleep duration during CON was 432 ± 25 min on night one and 440 ± 16 min on night two and was similar to the pre-trial sleep duration (P = 0.61). It was also confirmed by accelerometry that all participants had 0 min of sleep on SDEP and SDEP + ER. Ambulatory physical activity, as assessed by total trial pedometer counts, was also greater on SDEP (49,798 ± 7581 steps, P = 0.04) and SDEP + ER (50,184 ± 7230 steps, P = 0.002) than CON (43,621 ± 4334 steps). On day one, 5 h into each trial, 90 min walk RPE (10 ± 2, P = 0.60), 5 km time trial RPE (19 ± 1, P = 0.16) and 5 km time trial performance (1432 ± 327 s, P = 0.50) were similar on all trials. On day two, 29 h into each trial, 90 min walk RPE were similar on CON and SDEP (11 ± 2 and 12 ± 2, P = 0.13); however, RPE was higher than CON after SDEP + ER (15 ± 3, P < 0.01). Time taken to complete the 5 km time trial was longer after SDEP + ER (1961 ± 682 s, P = 0.04) and SDEP (1465 ± 278 s, P = 0.01) than CON (1401 ± 290 s), which agrees with similar studies in our laboratory to examine the effects of sleep loss and energy restriction on endurance performance (Oliver et al. 2007, 2009). As on day 1, final 5 km time trial RPE on day 2 was similar on all trials (19 ± 1, P = 0.16), indicating maximal or very near maximal effort during the daily exercise.
Pre-cold air test
Before the CAT, body mass was lower and plasma norepinephrine higher on SDEP + ER than CON and SDEP (Table 1). Urine osmolality, plasma glucose, plasma epinephrine, Mean T sk, M, and T re were, however, similar before the CAT.
Cold air test tolerance and thermal responses
After CON, SDEP and SDEP + ER cold tolerance times were similar (Table 2; Fig. 2 Mantel-Cox χ2 P = 0.29). Participants only finished the CAT early if core temperature fell below 36 °C. Participants did not leave the CAT early for other reasons (e.g., hands feeling too cold).
Sleep deprivation, with or without energy restriction, before the CAT also did not alter Mean T sk, M, or T re during the first 60 min (Fig. 3a mean T sk, main effect of condition P = 0.52; Fig. 3b M, main effect of condition P = 0.36; Fig. 3c T re main effect of condition P = 0.68). During the first 60 min of the CAT, RER and V̇O2 were also not different between the trials (main effect of conditions: RER, P = 0.08, VO2, P = 0.34). Comparable thermal responses after CON, SDEP, and SDEP + ER were also evident later in the CAT and T re was also similar one hour after participants had finished the CAT (Table 3).
After the CAT, plasma glucose and epinephrine were alike on all trials (Table 2). Plasma norepinephrine was also similar after the CAT on SDEP but it tended to be greater after the CAT on SDEP + ER than CON (P = 0.07). To determine the effect of prior SDEP and SDEP + ER on these plasma responses to the CAT, and because differences in norepinephrine existed between trials before the CAT, plasma responses were also compared between trials once post-CAT responses were corrected for pre-CAT. When compared in this manner, plasma glucose (P = 0.75), epinephrine (P = 0.24), and norepinephrine (P = 0.19) responses were similar irrespective of prior sleep deprivation and energy restriction. This indicates the trend (P = 0.07) for higher norepinephrine immediately after the CAT on SDEP + ER was a result of the higher pre-CAT concentration. In summary, plasma glucose, epinephrine, and norepinephrine responses to the CAT were similar.
Cold air test perceived thermal discomfort
Prior sleep deprivation, with and without energy restriction, tended to lead to greater perceived thermal discomfort during the first 60 min of the CAT (Fig. 4a thermal comfort, main effect of condition P = 0.07; Fig. 4b pain sensation to cold, main effect of condition P = 0.10). Indeed, compared with CON, thermal comfort was less after SDEP (P = 0.05) and cold pain sensation tended to be greater after SDEP + ER (P = 0.06). Later in the CAT perceived discomfort was, however, similar on all trials where thermal comfort declined to severe cold discomfort and pain sensation to cold increased to nearly unbearable pain (Table 3).
Discussion
This study examined the thermal response during cold exposure after 2 nights of sleep deprivation with and without energy restriction in young healthy men completing daily exhaustive exercise. The principle finding was that 53 h of sleep deprivation, with or without energy restriction, did not impair thermal responses during cold exposure. This was evident from the similar cold tolerance times and proportion of participants completing the CAT. Further, body temperatures, metabolic, and perceptual responses were similar during the CAT irrespective of prior sleep or energy restriction. In contrast, perceived thermal discomfort during the initial hour tended to be greater after SDEP and SDEP + ER. This greater perception of cold discomfort at the same body temperature suggests that sleep and energy restriction may actually reduce cold injury risk, as people are likely to engage earlier in normal behavioral cold adaptation, for example, the addition of further clothing or movement to a warmer environment. One hour after the CAT, core temperature was similar suggesting rewarming is also not impaired after 2 days of sleep and energy restriction combined with exhaustive exercise. These findings challenge the belief that sleep and energy restriction impair thermal responses to cold stress. This is important as sleep and energy restriction are often cited in reviews and position statements as possible risk factors for cold injury (Rintamäki 2000; Castellani et al. 2006; Cappaert et al. 2008).
The present study is the first to thoroughly examine the effect of more than 1 nights sleep loss on cold tolerance and thermal responses during cold. Our findings are consistent, however, with the majority of studies that examine the effect of 1 nights sleep loss on thermal responses to cold (Fiorica et al. 1968; Savourey and Bittel 1994; Caine-Bish et al. 2004). Major methodological differences, including prior pre-heating and an all-female study population, likely explain the differences between the majority of studies and the single study that suggests sleep loss leads to greater core cooling (Landis et al. 1998). Our data are consistent with the only other study to examine the effect of more than 1 nights sleep loss on thermal responses during cold (Fiorica et al. 1968); however, the present study more thoroughly examines the effects as we employed a repeated measures design, where participants acted as their own controls. In comparison, the earlier study used a between-groups design that made interpreting the effect of prolonged sleep loss difficult, particularly as the baseline core temperatures of the control group progressively increased during the 4-day trial (Fiorica 1968). As perceived thermal discomfort was greater during cold exposure after 2 nights of sleep loss, the current study also outlines for the first time that prolonged sleep loss is unlikely to impair behavioral cold adaptation. Additionally, rewarming after cold exposure was not impaired after 2 days of sleep loss with energy restriction and exhaustive exercise. The current study therefore extends previous research that reported rewarming was not affected by 2 nights of sleep loss only (Esmat et al. 2012). One important additional distinction between the current and previous sleep loss and cold thermoregulation studies is that participants in this study completed exhaustive daily exercise, whereas previous study participants completed only low levels of physical activity. Therefore, in combination, these data suggest 2 nights of sleep loss, even in persons completing exhaustive daily exercise, does not impair the thermal response to cold and therefore sleep loss may not be a risk factor for hypothermia.
Previous multi-stressor studies suggest heightened hypothermia risk after training and operations that combine exhaustive exercise, sleep and energy restriction (Young et al. 1998; Castellani et al. 2003). When compared with these previous multi-stressor studies, a particularly novel aspect of the current study is that, using a repeated measures design, we were able to isolate the effects of sleep deprivation, with and without energy restriction, on thermal responses during cold in persons completing daily exhaustive exercise. In contrast with the previous multi-stressor studies, we indicate that 53 h of sleep loss, with or without energy restriction, does not impair cold tolerance or thermal responses to cold. Daily energy expenditure was similar and the daily energy deficit greater in this study compared with previous multi-stressor studies. Therefore, the poorer cold tolerance in previous multi-stressor studies is most likely explained by the longer duration of the stressors causing greater subcutaneous fat loss and body mass loss, which subsequently increased heat loss and impaired heat production during the CAT (Young et al. 1998; Castellani et al. 2003). That substantial insulative tissue loss (subcutaneous fat loss) was responsible for increased heat loss during cold exposure in the previous 61-day multi-stressor study (Young et al. 1998) is supported by studies that show the heat conservation mechanism peripheral vasoconstriction is preserved during cold exposure in severely underweight persons (Fellows et al. 1985; Mansell et al. 1990). Further, based on skin temperature and plasma norepinephrine responses to the CAT in the present study, short-term sleep and energy restriction does not appear to impair cold-induced peripheral vasoconstriction. Similarly, the poorer metabolic heat production during cold exposure in previous multi-stressor studies maybe explained by the longer duration of the stressors causing greater reductions in metabolic active tissue such as lean mass. Indeed, lower metabolic heat production during cold exposure has been shown in undernourished persons with less than 90 % ideal bodyweight (Mansell et al. 1990). To date, no studies have demonstrated that acute energy restriction, including a complete 48-hour fast, impairs metabolic heat production during cold exposure (Macdonald et al. 1984). This is likely because the predominant fuel source for prolonged, low intensity, shivering thermogenesis is lipid, which is an abundant fuel source accounting for 95 % of the total energy stores (Haman et al. 2002). Moreover, the majority of studies to manipulate participant nutritional status before or during mild cold exposure, by muscle glycogen depletion or acute carbohydrate ingestion, report the same thermal responses to cold (Young et al. 1989; Glickman-Weiss et al. 1994; Haman et al. 2004). The same thermogenic response to mild cold is possible due to a greater reliance on lipid and protein metabolism (Haman et al. 2004).
This study identifies the independent and combined effects of sleep and energy restriction on cold-induced thermal response suggesting that neither impairs cold tolerance or thermal responses to cold in young, health, and fit men. For the experiment duration, the severity of stressors was very high and greater sleep and energy restriction is unlikely to occur within 2 days. The conclusions should, however, be limited to the duration of the current experiment where sleep and energy restriction occurred for 2 days and nights and the cold air test evoked modest shivering (< 25 %VO2max). Given the results of the previous multi-stressor studies (Young et al. 1998; Castellani et al. 2003), it is plausible that longer durations of sleep and energy restriction before cold exposure may impair the thermal response to cold and increase cold injury risk. These stressors may also have much greater negative effects on cold tolerance in children, women, and the elderly because compared with healthy young men these populations are at a thermoregulatory disadvantage due to greater surface area and smaller total body mass and musculature (Castellani et al. 2006). Further, compared with younger men, peripheral vasoconstriction and thermogenesis are impaired in older persons (Frank et al. 2000; Thompson-Torgerson et al. 2008) and after a 48 h fast thermal and metabolic impairments were greater in women (Macdonald et al. 1984; Mansell and Macdonald 1989). Given the greater cold injury risk in these populations it is not recommended to generalise the findings of the present study beyond young, healthy, and fit men. We chose to study this population as they reflect the majority of persons likely to be exposed to leisure activities and occupations that involve exhaustive exercise, energy restriction, and sleep loss. Finally, the present study examined whole body responses to cold, and therefore we are unable to discount negative effects of sleep loss and energy restriction on peripheral cold injury. However, as thermal discomfort tended to be greater during cold exposure after sleep loss, with or without energy restriction, cold injury risk may actually be lower after these stressors in scenarios where persons are free to engage in normal behavioral cold adaptation, for example, add additional clothes or move to a warmer room.
In summary, 2 nights sleep loss, with or without 90 % restriction in energy intake, and exhaustive daily exercise did not alter cold tolerance or thermal responses to cold air exposure lasting up to 4 hours. However, both sleep loss and energy restriction did increase the perceived thermal discomfort at the same given core body temperature. It would therefore appear that active persons, such as military personnel, emergency services, ultra-endurance athletes and search and rescue teams, are under no greater risk of hypothermia from cold air exposure of up to 4 hours when sleep deprived for 2 nights and severely energy restricted, than when they are well rested and fed.
Abbreviations
- ANOVA:
-
Analysis of variance
- A D :
-
Body surface area
- CAT:
-
Cold air test
- CON:
-
Control trial
- EDTA:
-
Ethylenediaminetetraacetic acid
- ER:
-
Energy restriction
- M :
-
Metabolic heat production
- Mean T sk :
-
Mean skin temperature
- RER:
-
Respiratory exchange ratio
- RPE:
-
Ratings of perceived exertion
- SDEP:
-
Sleep deprivation
- SDEP + ER:
-
Sleep deprivation and energy restriction
- T bicep :
-
Bicep skin temperature
- T calf :
-
Calf skin temperature
- T chest :
-
Chest skin temperature
- T re :
-
Rectal core temperature
- T thigh :
-
Thigh skin temperature
- RH:
-
Relative humidity
- VO2 :
-
Oxygen uptake
- VO2max :
-
Maximal oxygen uptake
References
Ancoli-Israel S, Cole R, Alessi C et al (2003) The role of actigraphy in the study of sleep and circadian rhythms. Sleep 26:342–392
Caine-Bish NL, Potkanowicz ES, Otterstetter R, Glickman EL (2004) Thermal and metabolic responses of sleep deprivation of humans during acute cold exposure. Aviat Space Environ Med 75:964–968
Cappaert TA, Stone JA, Castellani JW et al (2008) National Athletic Trainers’ Association position statement: environmental cold injuries. J Athl Train 43:640–658
Castellani JW, Stulz DA, Degroot DW et al (2003) Eighty-four hours of sustained operations alter thermoregulation during cold exposure. Med Sci Sports Exerc 35:175–181
Castellani JW, Young AJ, Ducharme MB et al (2006) American College of Sports Medicine position stand: prevention of cold injuries during exercise. Med Sci Sport Exerc 38:2012–2029
Chen AC, Rappelsberger P, Filz O (1998) Topology of EEG coherence changes may reflect differential neural network activation in cold and pain perception. Brian Topogr 11:125–132
Chudalla R, Baerwalde S, Schneider G, Maassen N (2006) Local and systemic effects on blood lactate concentration during exercise with small and large muscle groups. Pflugers Arch 452:690–697
Compher C, Frankenfield D, Keim N, Roth-Yousey L (2006) Best practice methods to apply to measurement of resting metabolic rate in adults: a systematic review. J Am Diet Assoc 106:881–903
Consolazio CF, Johnson RE, Pecora LJ (1963) Physiological variability in young men. Physiol Meas Metab Funct man. McGraw Hill, New York, pp 453–480
Costa RJS, Smith AH, Oliver SJ et al (2010) The effects of two nights of sleep deprivation with or without energy restriction on immune indices at rest and in response to cold exposure. Eur J Appl Physiol 109:417–428
Dill DB, Costill DL (1974) Calculation of percentage changes in volumes of blood, plasma and red-cells in dehydration. J Appl Physiol 37:247–248
Esmat TA, Clark KE, Muller MD, Juvancic-Heltzel JA, Glickman EL (2012) Fifty-three hours of total sleep deprvation has no effect on rewarming from cold air exposure. Wilderness Environ Med 23:349–355
Fellows IW, Macdonald IA, Bennett T, Allison SP (1985) The effect of undernutrition on thermoregulation in the elderly. Clin Sci 69:525–532
Fiorica V, Higgins E, Iampietro P et al (1968) Physiological responses during sleep deprivation of men. J Appl Physiol 24:167–176
Frank SM, Raja SN, Bulcao C, Goldstein DS (2000) Age-related thermoregulatory differences during core cooling in humans. Am J Physiol Regul Integr Comp Physiol 279:R349–R354
Gagge AP, Gonzalez R (1996) Mechanisms of heat exchange: biophysics and physiology. In: Fregly MJ, Blatteis CM (eds) Handb Physiol Sect. 4, Environ Physiol. Oxford University Press, New York, pp 45–85
Gale EAM, Bennett T, Green JH, Macdonald IA (1981) Hypoglycaemia, hypothermia and shivering in man. Clin Sci 61:463–469
Glickman-Weiss EL, Nelson AG, Hearon CM et al (1994) The thermogenic effect of a carbohydrate feeding during exposure to 8, 12 and 27C. Eur J Appl Physiol Occup Physiol 68:291–297
Haman F, Peronnet F, Kenny GP et al (2002) Effect of cold exposure on fuel utilization in humans: plasma glucose, muscle glycogen and lipids. J Appl Physiol 93:77–84
Haman F, Peronnet F, Kenny GP et al (2004) Effects of carbohydrate availability on sustained shivering I. Oxidation of plasma glucose, muscle glycogen, and proteins. J Appl Physiol 96:32–40
Hollies NRS, Goldman RF (1977) Clothing comfort: interaction of thermal, ventilation, construction, and assessment factors. 112
Landis CA, Savage MV, Lentz MJ, Brengelmann GL (1998) Sleep deprivation alters body temperature dynamics to mild cooling and heating not sweating threshold in women. Sleep 21:101–108
Macdonald IA, Bennett T, Sainsbury R (1984) The effect of a 48 h fast on the thermoregulatory responses to graded cooling in man. Clin Sci 67:445–452
Mansell PI, Macdonald IA (1989) Effects of underfeeding and of starvation on thermoregulatory responses to cooling in women. Clin Sci 77:245–252
Mansell PI, Fellows IW, Macdonald IA, Allison SP (1990) Defect in thermoregulation in malnutrition reversed by weight gain. Physiological mechanisms and clinical importance. Q J Med 76:817–829
Moran DS, Heled Y, Shani Y, Epstein Y (2003) Hypothermia and local cold injuries in combat and non-combat situations–the Israeli experience. Aviat Space Environ Med 74:281–284
Oliver SJ, Laing SJ, Wilson S et al (2007) Endurance running performance after 48 h of restricted fluid and/or energy intake. Med Sci Sport Exerc 39:316–322
Oliver SJ, Costa RJS, Laing SJ et al (2009) One night of sleep deprivation decreases treadmill endurance performance. Eur J Appl Physiol 107:155–161
Pugh LGCE (1966) Accidental hypothermia in walkers, climbers, and campers: report to the medical commission on accident prevention. Br Med J 1:123–129
Ramanathan NL (1964) A new weighting system for mean surface temperature of the human body. J Appl Physiol 19:531–533
Rintamäki H (2000) Predisposing factors and prevention of frostbite. Int J Circumpolar Health 59:114–121
Savourey G, Bittel J (1994) Cold thermoregulatory changes induced by sleep deprivation in men. Eur J Appl Physiol 69:216–220
Thompson-Torgerson CS, Holowatz LA, Kenney WL (2008) Altered mechanisms of thermoregulatory vasoconstriction in aged human skin. Exerc Sport Sci Rev 36:122–127
Todorovic V, Micklewright A (2004) The parenteral and enteral nutrition group of British Dietetics Association: a pocket guide to clinical nutrition. British Dietetics Association, pp 1–12
Van Someren EJW (2006) Mechanisms and functions of coupling between sleep and temperature rhythms. Prog Brain Res 153:309–324
Weir JB (1949) New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol 109:1–9
Young AJ, Sawka MN, Neufer PD et al (1989) Thermoregulation during cold water immersion is unimpaired by low muscle glycogen levels. J Appl Physiol 66:1809–1816
Young A, Castellani J, O’Brien C et al (1998) Exertional fatigue, sleep loss, and negative energy balance increase susceptibility to hypothermia. J Appl Physiol 85:1210–1217
Zafren K, Giesbrecht GG, Danzl DF et al (2014) Wilderness Medical Society practice guidelines for the out-of-hospital evaluation and treatment of accidental hypothermia. Wilderness Environ Med 25:S86–S95
Acknowledgments
The authors wish to acknowledge the Headquarters Army Recruiting and Training Division, Upavon, UK, for supporting the study.
Conflict of interest
The authors declare they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by George Havenith.
Rights and permissions
About this article
Cite this article
Oliver, S.J., Harper Smith, A.D., Costa, R.J.S. et al. Two nights of sleep deprivation with or without energy restriction does not impair the thermal response to cold. Eur J Appl Physiol 115, 2059–2068 (2015). https://doi.org/10.1007/s00421-015-3184-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-015-3184-y