Abstract
Objectives
As studies on mental disorders in victims of occupational injury or disease are limited, this study aims to evaluate the risk of, and factors associated with, the development of mental illness in patients with occupational injury or disease using insurance claims data from Taiwan.
Methods
This retrospective cohort study analyzed insurance records in Taiwan to identify 18,285 adults who experienced occupational injury or disease in 2002–2013 and 18,285 adults without occupational injury or disease who were matched by propensity score. The risks of mental disorders during a follow-up period of up to 2 years were estimated and compared between the two cohorts.
Results
After controlling for other variables, the odds of mental illness in patients with occupational injury or disease was significantly higher compared to patients without occupational injury or disease. Additional factors associated with higher odds of mental disorders included female gender, age ≥ 30 years (vs. 20–29 years), Charlson comorbidity index ≥ 1, occupation category of labor union member, soldier, insured by social security, religious group member (vs. private or government employee), lower premium-based monthly salary (≤ 576 US$), treatment at a district hospital or clinic (vs. medical center), treatment at a publically-owned or consortium-owned hospital (vs. private hospital), and central or southeast geographic location (vs. Taipei). The main types of mental illness were anxiety disorder (2.79%) and other psychoses (3.29%).
Conclusion
The risk of mental illness slightly increased during the 2-year period after the diagnosis of occupational injury or disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Accidents are an important cause of morbidity and mortality worldwide and the sixth leading cause of deaths in Taiwan (Ministry of Health and Welfare 2017). Occupational injuries are estimated to account for more than 300,000 deaths annually and a substantial number of disability-adjusted life years globally (Rushton 2017; Takala et al. 2014). In Taiwan, the occupational accident rate in 2012 was 4.0 per 1000 full-time workers, and the occupational fatality rate was 2.9 per 100,000 full-time workers (Occupational Safety and Health Administration 2018). Occupational injuries can result in detrimental physical and psychological effects on the people affected and place economic burdens on individuals, industries and health care systems.
Several studies have provided evidence that occupational injury increases the risk of mental disorders (Lin et al. 2014). The reported rates of psychiatric disorders in workers who have suffered an occupational injury range from 1.5% during the first 3 months after injury to 9.5% during the first year after injury (Lin et al. 2017; Asfaw and Souza 2012). Importantly, the rate of mental illness is around 50% higher in individuals with occupational injury than in control populations without occupational injury or with other medical conditions (Lin et al. 2017; Asfaw and Souza 2012). The average cost of outpatient treatment of depression is also higher for injured workers than for non-injured workers (Asfaw and Souza 2012). The psychiatric illnesses diagnosed in people with an occupational injury include major depressive disorder (MDD), post-traumatic stress disorder (PTSD) and anxiety disorder (Lin et al. 2017; Asfaw and Souza 2012). The risk of mental illness after occupational injury is associated with various factors, including female gender, lower education level, longer hospitalization, and physical appearance related to residual injury (e.g. to the face) (Lin et al. 2017; Berecki-Gisolf et al. 2015). A worker may develop a mental illness within one year after occupational injury, and psychological distress can persist for up to 2 years after injury (Fauerbach et al. 2007). Furthermore, a mental disorder after occupational injury is an important factor delaying the return to work (Lin et al. 2013; Palmu et al. 2015).
Occupational injury and the subsequent mental disorders related to it are important public health challenges and studies on the associated factors and the types of mental disorders that develop are limited (Lin et al. 2017). The present study aims to evaluate the risk and associated factors of developing a mental disorder after occupational injury or disease in Taiwan. In addition, it analyzes the types of mental disorder that occurred.
Methodology
Study design and study cohorts
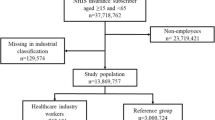
We sourced the data from the National Health Insurance Research Database, obtained from the National Health Research Institutes of Taiwan, to conduct a retrospective cohort study. Diseases were coded in the insurance database using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) (Medicode 1996). From the insurance claims data, people diagnosed with occupational injury or disease during the period 2003–2012 were identified as the injury cohort. The inclusion criteria were: (1) age ≥ 20 years; (2) a recorded diagnosis of occupational injury or disease (payment category: GAVE_KIND); (3) no evidence of mental illness preceding the diagnosis of occupational injury; and (4) baseline information on demographic status and medical care received was available.
The propensity score was calculated for each person in the injury cohort. We further identified a non-injury cohort of the same sample size, matched by the propensity score and inclusion criteria to the injury cohort from the insurance claims data by people who were diagnosed with occupational injury or disease during the period 2003–2012. This statistical approach enabled us to reduce selection bias and confounding effects in our observational study (Joffe and Rosenbaum 1999). A propensity score for each person was determined using a multivariate logistic regression model that adjusted for the following baseline covariates: age range (based on subgroups of 20–29, 30–39, 40–49, 50–59 and ≥ 60 years), gender, degree of urbanization of the region in which they resided, Charlson comorbidity index (CCI) and year of diagnosis of injury or disease (Charlson et al. 1987).
The National Health Research Institutes changed all personal identifications into surrogate numbers before releasing the database to researchers to protect the privacy of the insured people. This study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The NHIRD encrypts patient personal information to protect privacy and provides researchers with anonymous identification numbers associated with relevant claims information, including sex, date of birth, medical services received, and prescriptions. Therefore, patient consent is not required to access the NHIRD. This study was approved to fulfill the condition for exemption by the Institutional Review Board (IRB) of China Medical University (CMUH104-REC2-115-CR3). The IRB also specifically waived the consent requirement.
Baseline characteristics
We considered variables used to estimate propensity score as the baseline factors that could be associated with the development of mental disorders. We also took in account of occupation, household income, type of medical care provider, and insurance sub-bureau as additional factors potentially associated with the development of mental disorders. In particular, the need for considering different categories in the type of health care providers in terms of level of hospital and ownership of hospital was due to an appreciation for the existence of inherent differences in the type and overall quality of health care services offered by different providers (Cid Pedraza et al. 2015; De Moraes et al. 2010). As noted by Lin et al. (2017), type and quality of care services for patients with occupational injury impact their psychological health outcomes in the long term. In line with research findings confirming differences in the profiles of occupational injury and related outcomes across occupations, insurance plans, and labor representation arrangements (Concha-Barrientos et al. 2005; Brede et al. 2012), data on occupation were grouped into five categories: private or government employee, union or non-union, farmer or fisherman, military or social security insured, and religious or non-religious group.
Follow-up and outcome measures
Individuals included in this study were followed up for a maximum of 2 years or until being diagnosed with a mental disorder or censored because of lack to follow-up or withdrawal from the insurance database. Follow-up time in person-years was estimated for each person. Identification of mental illnesses was based on insurance claims data from the insurance database by participants for mental disorder related diagnoses and/or treatment. Types of mental illnesses were categorized as substance-related disorders, emotional disorder, anxiety disorder (Appendix 1 ICD Code) and other psychoses using the International Standard Diagnostic Classification of Diseases for Mental Illness (Medicode 1996).
Statistical analyses
Data analyses were performed using SAS 9.3 software (SAS Institute, Cary, NC, USA). For enrollment into the control group, PSM was used to control for potential confounders (age, gender, degree of urbanization, CCI and year of diagnosis of injury or disease), as described above. A descriptive statistical approach was employed (Lin et al. 2017). Continuous data are presented as the mean, standard deviation (SD) and range. Count data are presented as n (%). In reference to Hou et al. (2011), the chi-square test for independence was used to determine whether there was an association between each baseline parameter and the occurrence of mental illness during the 2-year follow-up period. Binary logistic regression analysis, with the calculation of crude odds ratios (ORs), adjusted ORs (aORs), and 95% CIs, was used to identify factors, health, demographics, health provider, and geographic characteristics, that were associated with the occurrence of mental illness during the 2-year observation period. Multinomial logistic regression analysis was carried out to identify factors associated with the occurrence of different subtypes of mental illness during the 2-year follow-up period. P < 0.05 was taken to indicate statistical significance.
Results
Prevalence of mental disorders after occupational morbidity stratified by health, demographics, health provider and geographic characteristics
A total of 18,285 participants with occupational injury or disease were included in the analysis. The prevalence of mental disorders stratified by various baseline characteristics is presented in Table 1. The vast majority of participants who had been diagnosed with occupational injury (97.4%), 65.8% were male and 66.8% were aged 20–39 years. The CCI was 0 points in approximately half the participants (51.1%), and 60.5% were categorized as having occupation category 1 (private employee or government employee). The premium amount was ≤ 576 US$ in 57.7% of cases, and 64.5% of participants were treated in a private medical institution.
A total of 1494 participants (8.2%) developed a mental illness during the follow-up period (Table 1). The time interval between the diagnosis of occupational injury or disease and the diagnosis of mental illness was 9.51 ± 7.20 months. As shown in Table 1, the prevalence of mental disorders showed significant differences between subcategories of CCI (increasing prevalence with increasing CCI; P < 0.001), gender (higher prevalence in women; P < 0.001), age (increasing prevalence with increasing age; P < 0.001), occupation (highest prevalence for soldiers or those insured by social security; P < 0.05), premium-based monthly salary (highest prevalence for the 960–1210 US$ category; P < 0.001), level of hospital (higher prevalence for medical centers and clinics; P < 0.001) and ownership of hospital (highest prevalence for publically-owned hospitals; P < 0.001). The prevalence of mental disorders did not vary significantly with type of occupational morbidity (occupational disease or occupational injury) or geographic characteristics (urbanization level or region).
Binary logistic regression analysis of health, demographics, health provider and geographic factors associated with mental disorders in the entire study cohort
Further analyses were performed for the entire study cohort, consisting of 18,285 people with occupational morbidity and 18,285 people without occupational morbidity who were propensity score-matched for gender, age, CCI, urbanization level and year of diagnosis. Binary logistic regression analysis revealed that occupational injury or disease was associated with significantly higher odds of mental illness (aOR: 1.098; 95% CI 1.008–1.196; P = 0.032; see Table 2). Additional factors identified as being associated with higher odds of mental illness included female gender, age ≥ 30 years vs. 20–29 years, CCI score ≥ 1, occupation categories 2 (labor union member), 4/5 (soldier or insured by social security) or 6 (religious group member) vs. occupation type 1 (private or government employee), lower premium-based monthly salary (≤ 576 US$), treatment at a district hospital or clinic vs. a medical center, treatment at a publically-owned or consortium-owned hospital vs. a private hospital, and central or southeast geographic location vs. Taipei (Table 2). In particular, age ≥ 30 years was identified as having a significantly linear association with increased odds of mental illness, while salary was identified as having a significantly inverse association with increased odds of mental illness regardless of gender and occupation type. In line with the results from the descriptive statistical analysis (Table 1), the binary logistic regression analysis indicated that the urbanization level did not significantly impact the prevalence of mental illnesses associated with occupational injury or disease.
Multinomial logistic regression analysis of factors associated with different types of mental illness in the occupational injury/disease cohort
Table 3 presents the factors associated with each type of mental illness in the occupational injury/disease cohort. Notably, male gender was associated with higher odds of substance-related disorder but lower odds of emotional disorder, anxiety disorder or other psychoses (Table 3). Furthermore, CCI score ≥ 1 was an important factor associated with increased odds of all subtypes of mental illness (Table 3). The odds of a substance-related disorder in particular increased if treatment was given at a local medical service provider, while the odds of all four subtypes of mental illness dropped if treatment was at a private medical service provider, whereas urbanization level did not significantly impact the odds of any of the subtypes of mental illness (Table 3).
Discussion
A notable finding of the present study was that 8.2% of people who had experienced occupational injury or disease developed a mental disorder during the 2-year follow-up period. The average time from the diagnosis of occupational injury or disease to the development of mental illness was around 9.5 months. Risk factors for the development of mental illness included gender, age ≥ 30 years (vs. 20–29 years), Charlson comorbidity index ≥ 1, occupation category of labor union member, soldier, insured by social security, veteran or religious group member (vs. private or government employee), lower premium-based monthly salary (≤ US$576), treatment at a district hospital or clinic (vs. medical center), treatment at a publically-owned or consortium-owned hospital (vs. private hospital), and central or southeast geographic location (vs. Taipei). The main types of mental illness were anxiety disorder (2.79%) and other psychoses (3.29%). Additionally, although female gender was associated with higher odds of emotional disorder, anxiety disorder or other psychoses, men were at greater risk of developing substance-related disorder after occupational injury or disease. These novel findings regarding risk factors for mental illness after occupational injury or disease should be taken into consideration during the long-term management of people who experience occupational injury or disease.
In this study, the average time interval between the diagnosis of occupational injury or disease and the diagnosis of mental illness was 9.5 months, which is consistent with published data (Lin et al. 2014; Asfaw and Souza 2012; Palmu et al. 2015). Previous investigations have reported that occupational injury elevates the risk of mental disorders (Lin et al. 2014; Kim 2013). The rates of mental disorders after occupational injury range from 1.5% during the first 3 months to 9.5% during the first 12 months after injury (Lin et al. 2014, 2017, 2012; Asfaw and Souza 2012; Kim 2013). Moreover, mental illness occurs more often in individuals with occupational injury than in people without occupational injury (Lin et al. 2014, 2017, 2012; Asfaw and Souza 2012). Stress caused by occupational injury is a potential risk factor for mental illness. Some studies have pointed out that the causes of greater psychological stress in workers with occupational injury might include physical pain, unsatisfactory rehabilitation, sudden changes in disease condition, aggravation of injury caused by an early return to work, aggravation of a local injury, difficulties experienced during applications for occupational injury compensation or related resources, lack of employment security, inability to return to the place of employment, and a lack of social support from employers (Lin et al. 2014, 2017; Asfaw and Souza 2012; Dersh et al. 2006; Qin et al. 2014). Although it was not possible to assess potential stressors in the present study, some or all of the above factors may have contributed to the development of mental illness in the occupational injury/disease cohort.
In this study, females were much more likely than males to suffer from mental illness after occupational injury or disease. This is in good agreement with previous research showing that women were at higher risk than men in suffering from mental illness after occupational injury or disease (Lin et al. 2017; Asfaw and Souza 2012; Berecki-Gisolf et al. 2015). An important finding of our analysis was that males were at substantially higher risk of substance-related disorders whereas females were at greater risk of emotional disorders, anxiety disorders or other psychoses. This observation mirrors the general trends seen in population studies since women exhibit a lower rate of substance abuse but higher rates of many other mental illnesses, including mood and anxiety disorders (Becker and Hu 2008; McLean et al. 2011; Steel et al. 2014).
The results of the present analysis showed that older patients with occupational injury, particularly those aged 30–59 years, were more likely to suffer from mental illness. In general agreement with our finding, a previous study reported that the highest risk of mental illness after occupational injury was in people aged 31–40 years (Asfaw and Souza 2012). Moreover, another investigation also concluded that older age increased the risk of mental illness after occupational injury (Lin et al. 2017). Older age was also found to be associated with failure to retain work 1 year after an occupational injury and a higher rate of PTSD after military service (Brede et al. 2012; Armenta et al. 2018). Thus, older people may be more susceptible to the development of mental illness after occupational injury or other traumatic events. Interestingly, the subgroup analyses revealed that only anxiety disorders showed an association with older age, with a significantly elevated risk in those aged 40–59 years. However, this finding can also be explained by the general understanding that older age is associated with individuals having an increased risk of occupational injury and feeling of being vulnerable (Qin et al. 2014; Takala et al. 2014), which are elements that might contribute to higher odds of anxiety disorders among older people. This finding in people with occupational injury or disease is not entirely consistent with data on the general population, which indicate that anxiety disorders peak at 25–44 years (Martin 2003). The reasons for this apparent discrepancy are unknown and merit further research.
A notable finding of this study was that people with a higher degree of comorbidity (higher CCI score) were at greater risk of developing mental illness, and this association was consistently observed for all four subtypes of mental disorder. This observation is in agreement with other investigations showing that a higher CCI is associated with a greater long-term risk of anxiety or depression in patients with traumatic spinal cord injury and with higher anxiety scores in orthopedics and trauma inpatients (Lim et al. 2017; de Moraes et al. 2010). Furthermore, chronic illnesses have also been reported to elevate the risks of mood disorders such as depression (Patten 2001; Gadalla 2008). Thus, particular attention should be paid to the mental health status of people with comorbidities after occupational injury or disease, since these individuals are at higher risk for the development of mental illness.
Low levels of household income are known to be associated with mental illness and suicide attempts, and a reduction in household income is a risk for incident mood disorders (Sareen et al. 2011). A notable finding of our research was that patients with occupational morbidity and lower premium-based monthly salary were more likely to suffer from mental illness. Consistent with our data, salary as a percentage of total family income was found to be a risk factor for major depression or PTSD in people in Taiwan with occupational injury (Lin et al. 2017), while higher pre-injury income was associated with lower depressive symptoms in a Canadian cohort (O'Hagan et al. 2012). In addition, part-time work and shorter job tenure were associated with the development of depression after occupational injury (Kim 2013). Previous research has indicated that work-related injury or disease can have profound financial effects on those affected due to medical care-related costs, other ongoing expenses and reduced income, and that this can force individuals to use up their savings, borrow money, deplete retirement funds or even declare bankruptcy (Lax and Klein 2008). Thus, the psychological impact of occupational injury or disease may be greater on people with lower income.
Among the people with occupational morbidity analyzed in this study, the risk of mental illness was higher if they had occupations in categories 4/5 (soldier or insured by social security) or 6 (veteran or religious group member) as compared with category 1 (private employee or government employee). Other research has identified occupation type as a factor influencing the risk of depression after occupational injury (Asfaw and Souza 2012). This effect of occupation type on the risk of mental illness after occupational injury or disease may be related to differences in salary, since previous studies have shown that people with lower income are more likely to suffer from mental illness or have poor mental health (Sareen et al. 2011; Mangalore and Knapp 2012).
Although the degree of urbanization did not influence the risk of mental disorders, people who suffered occupational injury or disease in the Taipei sub-bureau had a lower risk of developing mental illness, most notably anxiety and emotional disorders. This may reflect better accessibility to medical resources that are concentrated in metropolitan areas with better economic conditions. A similar argument may underlie our observation that the risk of mental illness after occupational injury or disease was higher for patients treated in publically-owned medical institutions or local medical centers (clinics), since private medical institutions may have a greater array of medical resources. In support of this, previous studies have suggested that high-level medical institutions provide better medical care and that mortality rates are lower for private hospitals than for public hospitals (Hou et al. 2011; Cid Pedraza et al. 2015).
This study has some limitations. First, it sourced data from the National Health Insurance Research database issued by the Taiwan National Institutes of Health. However, this database only contains data for insured persons who have used medical resources; it does not contain data for people who have not used medical resources or who paid for their medical treatment. Therefore, it was not possible to assess the development of mental disorders in people without disease or those who paid for their treatment. Second, certain potential risk factors for mental disorder after occupational injury or disease, such as personality traits, past history of mental illness or family history of mental illness, could not be analyzed because they could not be obtained from the database. Third, the follow-up period was only 2 years, so we did not compare the long-term rates of mental illness between those with and without occupational injury or disease. Fourth, it was not possible to evaluate whether the severity of occupational injury was a risk factor for mental illness as relevant information was unavailable. Fifth, traffic accidents on the way to and from work are included as occupational injuries in Taiwan, so direct comparisons with other published data not including traffic accidents as occupational injuries could not be made.
Conclusion
An analysis of data from the National Health Insurance Research Database for 2003–2013 revealed that 8.2% of people with occupational injury or disease developed a mental illness during the 2-year follow-up period, with an average time of 9.5 months between the diagnosis of occupational injury or disease and the diagnosis of mental illness. Risk factors for the development of mental illness included gender, age ≥ 30 years, low income and high CCI score. Although female gender was associated with a higher risk of emotional disorder, anxiety disorder or other psychoses, men were at higher risk of substance-related disorder. The results of this study provide useful reference information for government health organizations and unions that could help to develop preventive interventional measures for people at high risk of mental illness after occupational injury or disease.
References
Asfaw A, Souza K (2012) Incidence and cost of depression after occupational injury. J Occup Environ Med 54:1086–1091
Armenta RF, Rush T, LeardMann CA, Millegan J, Cooper A, Hoge CW, Millennium CST (2018) Factors associated with persistent posttraumatic stress disorder among U.S. military service members and veterans. BMC Psychiatry 18:48
Becker JB, Hu M (2008) Sex differences in drug abuse. Front Neuroendocrinol 29:36–47
Berecki-Gisolf J, Smith PM, Collie A, McClure RJ (2015) Gender differences in occupational injury incidence. Am J Ind Med 58:299–307
Brede E, Mayer TG, Gatchel RJ (2012) Prediction of failure to retain work 1 year after interdisciplinary functional restoration in occupational injuries. Arch Phys Med Rehabil 93:268–274
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Cid Pedraza C, Herrera CA, Prieto Toledo L, Oyarzún F (2015) Mortality outcomes in hospitals with public, private not-for-profit and private for-profit ownership in Chile 2001–2010. Health Policy Plan 1:i75–81
Concha-Barrientos M, Nelson DI, Fingerhut M, Driscoll T, Leigh J (2005) The global burden due to occupational injury. Am J Ind Med 48:470–481
Dersh J, Gatchel RJ, Mayer T, Polatin P, Temple OR (2006) Prevalence of psychiatric disorders in patients with chronic disabling occupational spinal disorders. Spine (Phila Pa 1976) 31:1156–1162
De Moraes VY, Jorge MR, Faloppa F, Belloti JC (2010) Anxiety and depression in Brazilian orthopaedics inpatients: a cross sectional study with a clinical sample comparison. J Clin Psychol Med Settings 17:31–37
Fauerbach JA, McKibben J, Bienvenu OJ, Magyar-Russell G, Smith MT, Holavanahalli R, Patterson DR, Wiechman SA, Blakeney P, Lezotte D (2007) Psychological distress after major burn injury. Psychosom Med 69:473–482
Gadalla T (2008) Association of comorbid mood disorders and chronic illness with disability and quality of life in Ontario, Canada. Chronic Dis Can 28:148–154
Hou YH, Lin SP, Chiu YL, Hsu YJ, Cheng LL (2011) Investigating the quality of outpatient care for diabetic patients in different health care organizations in Taiwan. Cheng Ching Med J 7:32–41
Joffe MM, Rosenbaum PR (1999) Invited commentary: propensity scores. Am J Epidemiol 150:327–333
Kim J (2013) Depression as a psychosocial consequence of occupational injury in the US working population: findings from the medical expenditure panel survey. BMC Public Health 13:303
Lax MB, Klein R (2008) More than meets the eye: social, economic, and emotional impacts of work-related injury and illness. New Solut 18:343–360
Lim SW, Shiue YL, Ho CH, Yu SC, Kao PH, Wang JJ, Kuo JR (2017) Anxiety and depression in patients with traumatic spinal cord injury: a nationwide population-based cohort study. PLoS ONE 12:e0169623
Lin KH, Guo NW, Shiao SC, Liao SC, Hu PY, Hsu JH, Hwang YH, Guo YL (2013) The impact of psychological symptoms on return to work in workers after occupational injury. J Occup Rehabil 23:55–62
Lin KH, Guo NW, Liao SC, Kuo CY, Hu PY, Hsu JH, Hwang YH, Guo YL (2012) Psychological outcome of injured workers at 3 months after occupational injury requiring hospitalization in Taiwan. J Occup Health 54:289–298
Lin KH, Chu PC, Kuo CY, Hwang YH, Wu SC, Guo YL (2014) Psychiatric disorders after occupational injury among National Health Insurance enrollees in Taiwan. Psychiatry Res 219:645–650
Lin KH, Shiao JS, Guo NW, Liao SC, Kuo CY, Hu PY, Hsu JH, Hwang YH, Guo YL (2017) Long-term psychological outcome of workers after occupational injury: prevalence and risk factors. J Occup Rehabil 24:1–10
Mangalore R, Knapp M (2012) Income-related inequalities in common mental disorders among ethnic minorities in England. Soc Psychiatry Psychiatr Epidemiol 47:351–359
Martin P (2003) The epidemiology of anxiety disorders: a review. Dialogues Clin Neurosci 5:281–298
McLean CP, Asnaani A, Litz BT, Hofmann SG (2011) Gender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illness. J Psychiatr Res 45:1027–1035
Ministry of Health and Welfare (2017) Taiwan’s leading causes of death in 2016. https://www.mohw.gov.tw/cp-3425-33347-2.html. Accessed 1 Aug 2018
Medicode (1996) ICD-9-CM: International classification of diseases, 9th revision, Clinical Modification. Salt Lake City
Occupational Safety and Health Administration, Ministry of Labor, Republic of China (2018) National Occupational Safety and Health Profile of Taiwan. https://she.mcu.edu.tw/sites/default/files/u3/National%2520Occupational%2520Safety%2520and%2520Health%2520Profile%2520of%2520Taiwan.pdf. Accessed 1 Aug 2018
O'Hagan FT, Ballantyne PJ, Vienneau P (2012) Mental health status of Ontario injured workers with permanent impairments. Can J Public Health 103:e303–e308
Palmu R, Partonen T, Suominen K, Vuola J, Isometsä E (2015) Return to work six months after burn: a prospective study at the Helsinki Burn Center. Burns 41:1152–1160
Patten SB (2001) Long-term medical conditions and major depression in a Canadian population study at waves 1 and 2. J Affect Disord 63:35–41
Qin J, Kurowski A, Gore R, Punnett L (2014) The impact of workplace factors on filing of workers' compensation claims among nursing home workers. BMC Musculoskelet Disord 15:29
Rushton L (2017) The global burden of occupational disease. Curr Environ Health Rep 4:340–348
Sareen J, Afifi TO, McMillan KA, Asmundson GJ (2011) Relationship between household income and mental disorders: findings from a population-based longitudinal study. Arch Gen Psychiatry 68:419–427
Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, Patel V, Silove D (2014) The global prevalence of common mental disorders: a systematic review and meta-analysis 1980–2013. Int J Epidemiol 43:476–493
Takala J, Hämäläinen P, Saarela KL, Yun LY, Manickam K, Jin TW, Heng P, Tjong C, Kheng LG, Lim S, Lin GS (2014) Global estimates of the burden of injury and illness at work in 2012. J Occup Environ Hyg 11:326–337
Author information
Authors and Affiliations
Contributions
Conceptualization: M-HL, J-YW, Y-LY. Data curation: C-SL, C-HL, F-CS. Investigation: all authors. Methodology: all authors. Validation: C-SL, C-HL, F-CS. Resources: Y-LY, J-YW. Supervision: J-YW. Writing—original draft: M-HL, J-YW. Writing—review and editing: all authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Ethical approval
This study was approved by the Research Ethics Committee at China Medical University and Hospital (CMUH104-REC2-115-CR3). Informed consent was waived due to data anonymization. This study was financially supported by Ministry of Science and Technology of Taiwan (Grant no. MOST104-2410-H-039-006) and China Medical University in Taiwan (Grant no. CMU107-S-18).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lin, MH., Yang, YL., Sung, FC. et al. Risk of mental illness after the diagnosis of occupational injury or disease: a retrospective cohort study. Int Arch Occup Environ Health 94, 55–68 (2021). https://doi.org/10.1007/s00420-020-01558-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-020-01558-x