Abstract
Purpose
Occupational stress and obesity are very prevalent in emergency workers. Some studies have also associated high tobacco consumption rates with occupational stress. Each of these factors is known to increase cardiovascular risk. The aim of this study was to evaluate the prevalence of occupational stress, overweight and tobacco consumption in paramedics.
Methods
This cross-sectional study of paramedics consisted in a self-report survey of 44 questions divided into two sections. The first section collected demographic information and the second evaluated occupational stressors. The questions were designed to determine the prevalence of work-related psychosocial factors, overweight (body mass index ≥ 25 kg/m2) and tobacco consumption (cig/day ≥ 1). The demand-control-social support model and the effort–reward model were used to estimate job strain, iso-strain and imbalance in effort and reward.
Results
More than 88 % of paramedics reported at least one cardiovascular risk factor, with males reporting more risk factors than females. Ninety percent of male paramedics reported occupational stress, 12 % reported smoking, and 79 % were overweight or obese by self-report. The prevalence of occupational stress and smoking was similar for female paramedics, but with a lower prevalence of overweight (37 %).
Conclusion
By self-report, nine out of ten paramedics are at risk of developing cardiovascular disease. Both individual and organizational efforts should be made to educate and support paramedics and their organizations in reducing these workers’ cardiovascular risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Paramedics face challenging work conditions, requiring them to perform a wide range of pre-hospital emergency care on demand and in unpredictable environments. These workers are exposed to stressful events in the line of duty that may affect their physical and emotional health and performance (Alexander and Klein 2001; Backé et al. 2011; Bennett et al. 2004; Dallman et al. 2006; Hegg-Deloye et al. 2014a; Sterud et al. 2006, 2008).
In 2008, cardiovascular disease accounted for 29 % of all deaths worldwide. The World Health Organization estimates that this figure could reach 35 % by 2030 if prevention and detection of cardiovascular disease do not improve (World Health Organization 2013). One study reported that 18 % of on-duty deaths in paramedics from the USA resulted from cardiovascular events (Maguire et al. 2002).
It is widely accepted that age, sex, overweight and obesity, hypertension, smoking, dyslipidemia and diabetes are major risk factors for the development of cardiovascular disease (World Health Organization 2013). It is also recognized that both high job strain and iso-strain can increase cardiovascular risk (Johnson et al. 1989; Karasek 1985; Kivimaki et al. 2012). Further, a combination of high effort and low recognition elicits pathological reactions associated with cardiovascular risk (Aboa-Éboulé et al. 2011; Bourbonnais et al. 2007; Park 2009). Having more than one of these risk factors adds to an individual’s risk of developing cardiovascular disease (Jackson et al. 2005; Poulter 1999).
Several risk factors for cardiovascular disease have been observed in paramedics. In a study of paramedics from the USA, Barrett et al. (2000) found that 48 % were at high or very high risk of developing cardiovascular disease. Elevated cortisol levels and work-related decreases in cardiac parasympathetic activity have also been observed in on-duty paramedics (Aasa et al. 2006; Backé et al. 2009; Mitani et al. 2006). These alterations are significant as they may contribute to the development of several pathologies, such as arterial hypertension and cardiovascular diseases (Selye 1978). In a Canadian sample, arterial hypertension and hyperlipidemia were reported in 13 and 31 % of paramedics, respectively (Koehoorn et al. 2011). Tsismenakis et al. (2009) reported a high body mass index (BMI) in paramedic recruits (mean of 28.5 kg/m2), with a high proportion of their subjects being overweight. In addition, one study reported that 19 % of paramedics smoke more than one cigarette per day (Koehoorn et al. 2011).
To date, no study has explored the cardiovascular risk profile of paramedics in relation to sex and years of employment. The aim of this study was to evaluate occupational stress, BMI and tobacco consumption in male and female paramedics in relation to years of employment.
Methods
Participants
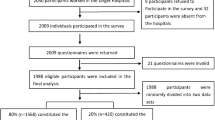
The study was conducted during the fall and winter of 2011 among paramedics in the province of Quebec, Canada. Participants were recruited via an electronic mailing list and word of mouth. Male and female active workers (at least 20 h/week) aged 18 years and older were included in this study. In the province of Quebec, the paramedic population totals approximately 4,650 workers, including 23.4 % females (Service Canada 2013). A sample of 300 respondents was sought. The final sample included 295 paramedics. Ethical approval for the study was obtained from the institutional ethics committee, and informed consent was obtained from all participants.
Questionnaire
The self-report questionnaire consists of 44 items. Participants were instructed to complete the questionnaires independently at home.
Age, sex, years of employment, number of cigarettes per day, body weight and height were extracted from the questionnaire. Subjects were grouped according to years of employment (<9, 10–19, and 20 years or more). BMI, defined as weight in kilograms divided by the square of the height in meters (kg/m2), was calculated. Subjects were considered overweight if their BMI was <25 kg/m2. Subjects were considered to be current smokers if they reported smoking one or more cigarettes per day.
Occupational stress was evaluated with both the Job Content Questionnaire and the effort–reward imbalance model (Johnson et al. 1989; Karasek 1985; Karasek and Theorell 1990; Niedhammer et al. 2000; Siegrist 1996). The Job Content Questionnaire contains measures of psychological demand, decision latitude and social support. Questions regarding psychological demand refer to the quantity of work, intellectual requirements and time constraints. Psychological demand scores range between −6 and 21; scores <7 correspond to a high psychological demand (Vézina et al. 2011). Questions regarding decision latitude evaluate opportunities to make decisions, be creative, and use and develop one’s abilities at work. Decision latitude scores range between 24 and 96; scores lower than 72 correspond to low decision latitude (Vézina et al. 2011). Questions on social support evaluate both peer and hierarchical support. Social support is considered to moderate tensions at work (Johnson et al. 1989). Social support scores range between 11 and 44; scores lower than 34 correspond to a low social support (Vézina et al. 2011). The high-job-strain group was defined as reflecting a combination of high psychological demand and low decision latitude, and the iso-strain group was defined as individuals with high psychological demand, low decision latitude and low social support (Aboa-Éboulé et al. 2007; Collins et al. 2005).
The effort–reward imbalance model was used to measure imbalance between effort at work and reward (Siegrist 1996). Effort refers to the psychological and physical constraints and behaviors associated with excessive involvement in work. Reward refers to salary, esteem and control over professional status (i.e., opportunities for promotion, job security). When the effort–reward ratio is <1, an imbalance between effort and reward exists. If this ratio is <1, effort and reward are considered balanced and the risk to the worker’s physical and mental health is reduced (Aboa-Éboulé et al. 2011; Bourbonnais et al. 2007; Park 2009).
Statistical analyses
A descriptive approach was used to determining the prevalence of indicators of occupational stress (high strain or high iso-strain or effort–reward imbalance), overweight (BMI ≥ 25 kg/m2) and tobacco consumption (cigarettes/day ≥ 1) in paramedics.
A multivariate analysis of variance (ANOVA), including sex and years of employment as between factors, was performed to identify mean differences for each of the dependent variables. Confidence interval (CI) estimation of the population proportion was calculated using a 95 % confidence level (score method with continuity correction). These proportions were then compared for sex and years of employment (Chi-square test). Computations were performed using Statistica version 7.0 (Statsoft Inc., Tulsa, OK). Statistical significance was set at p < .05. Each indicator of occupational stress was also compared to the median score for the Quebec population as reported in the EQCOTESST (Vézina et al. 2011).
Results
Of the 295 paramedics (26.4 % of whom were female) who responded to the questionnaire, none had missing data and all subjects were included in the statistical analysis. The mean age of participants was 35.8 ± 0.6 years. The mean BMI (with standard deviation), stratified by years of employment and sex, is reported in Table 1. Both BMI and number of cigarettes per day differed significantly with years of employment (p < .05). Paramedics with <10 years of experience had lower BMIs and smoked fewer cigarettes per day. Female paramedics had lower BMIs than male paramedics (24.6 vs. 28.7 kg/m2; p < .05). Similarly, male paramedics were more likely to be overweight than female paramedics after 10 years in employment (p < .001; Fig. 1). Overall, 37.1 % of females (95 % CI 26.7–48.9) and 78.8 % of males (95 % CI 72.6–83.9) reported a BMI < 25 kg/m2 (p < .001). Also, 16.7 % of females (95 % CI 9.5–27.2) and 14.3 % of males (95 % CI 10.0–19.8) reported smoking at least one cigarette per day in all years of employment groups (p = .61; Fig. 1).
No difference between male and female paramedics was found in mean values of occupational stress indicators nor was there any difference based on years of employment (p > .05). Among male paramedics, those with <10 years of experience were less likely to report job strain and iso-strain (p < .05; Fig. 2). No such difference based on years of employment was observed in female paramedics (p > .05).
For male and female paramedics, the prevalence of job strain, iso-strain and effort–reward imbalance is high: 90.8 % of males (95 % CI 85.9–94.1) and 87.2 % of females (95 % CI 77.2–93.3) (p = .51; Fig. 2). The prevalence of all three occupational stress indicators in male paramedics is higher than in the general population of Quebec (Table 2). For female paramedics, only effort–reward imbalance is higher than in the general population of Quebec.
The prevalence of one or more self-reported cardiovascular risk factors was higher in male paramedics than in female paramedics (p < .01; Fig. 3a). Across all years of experience categories, 98.4 % (95 % CI 95.7–99.6) of male and 88.6 % (95 % CI 79.0–94.5) of female paramedics reported one or more cardiovascular risk factors. The difference in prevalence between male and female paramedics was still observed when the effort–reward imbalance variable was excluded from the analysis [83.8 % (95 % CI 78.9–88.7) vs. 55.1 % (95 % CI 44.1–66.1); p < .001; Fig. 3b]. Moreover, 12.0 % of male (95 % CI 8.1–17.2) and 7.7 % of female paramedics (95 % CI 3.1–16.6) reported at least three cardiovascular risk factors (p = .17). No significant difference was observed between groups with different levels of experience (p = .17).
Discussion
This study examined the prevalence of cardiovascular risk factors in paramedics. More than 88 % of paramedics reported at least one cardiovascular risk factor; males were more likely to do so than females. The results also demonstrated that the prevalence of occupational stress and smoking was similar in male and female paramedics, but a higher rate of overweight was observed in male paramedics. As well, cardiovascular risk factors among paramedics increased with years of experience, mainly due to the increase in the prevalence of overweight and occupational stress. These results are alarming because, despite a number of public health measures, many paramedics appear to be continuing their high-risk lifestyle. In addition, the nature of their job may expose them to the complications of cardiovascular disease (Barrett et al. 2000; Hegg-Deloye et al. 2014a; Koehoorn et al. 2011).
Body mass index
This study demonstrated a higher prevalence of overweight in both male and female paramedics than in the general population (World Health Organization 2013). In 2013, an estimated 40 % of males and 26 % of females in Canada were overweight, which is an important risk factor for diabetes, hypertension and cardiovascular disease (Bonnet and Laville 2005; Cornier et al. 2011). These results are similar to those obtained in previous studies showing a particularly high prevalence of overweight (>50 %) in male paramedics (Gerace and George 1996; Tsismenakis et al. 2009). The prevalence of overweight in female paramedics is lower than in male paramedics. This sex difference could be due to attitudinal and behavioral differences toward weight and weight control. Studies have revealed that many women believe that overweight is both portrayed and perceived as “unattractive”; women feel increasing pressure to be slim and recognize the negative stereotyping of fatness (Craig and Caterson 1990; Shoneye et al. 2011). This could be particularly true of female paramedics considering that their employment includes physically demanding tasks and they must constantly adapt to the physical and mental challenges of the job because every day at work is different and unpredictable (Corbeil and Prairie 2012). Further studies are needed to confirm these hypotheses (Bellisle et al. 2004; Provencher et al. 2003).
The high prevalence of overweight among both male and female paramedics may also mean that they experience the impact of acute and chronic stress in similar ways. Acute and chronic stress may either inhibit or increase hunger, thus affecting regular meal timing and regulation of body weight (Arial et al. 2009; Foss and Dyrstad 2011; Jakubowicz et al. 2011; Selye 1978). Disinhibition eating behavior, defined as the tendency to overeat in response to a stimulus (e.g., occupational stress), is strongly associated with weight gain over time and with obesity in adult life (Hays et al. 2002; Hays and Roberts 2008). Moreover, our recent study showed that disinhibition was positively associated with the level of obesity in paramedics (Hegg-Deloye et al. 2014c). Excess body weight could have significant implications for the health of paramedics and compromise their own safety, as well as that of their colleagues and the community (Tsismenakis et al. 2009).
Daily smoking and tobacco use
The prevalence of smoking in the current study was similar to that in the general population (Bernier and Hamel 2006; World Heart Federation 2011). Smoking indirectly increases the risk of cardiovascular disease or coronary events by two to four times, secondary to increased rates of atherosclerosis, dyslipidemia, diabetes and arterial hypertension (Bazzano et al. 2003). Tobacco use could be a coping mechanism that paramedics adopt to mitigate stress (Heikkilä et al. 2012; Kouvonen et al. 2005). Higher rates of tobacco consumption (+3 cigarettes/week) have been reported in current smokers who experience occupational stress than in those who do not (Heikkilä et al. 2012). Paramedics with more than 10 years of experience smoked more cigarettes per day, but the prevalence of daily smokers who smoked at least one cigarette per day did not differ between the various years of employment groups. It is possible that occupational stress among paramedics may explain, at least in part, the increase in the number of cigarettes smoked, but it would not appear to be linked with the appearance of new smokers among older paramedics. No differences were observed between men and women in this study. These results suggest that occupational stress has a similar effect on tobacco use in male and female paramedics.
Occupational stress
In the paramedic population, the prevalence of job strain, iso-strain and effort–reward imbalance is higher than in the general population of Quebec (Aboa-Éboulé et al. 2011). These results are in accordance with other studies of paramedics that report poor mental health, high stress levels before interventions, high risk of post-traumatic stress and overinvestment (Arial and Benoît 2011; Backé et al. 2009; Bennett et al. 2004). It has been shown that chronic job strain is associated with recurrent coronary events, and high effort–reward imbalance scores have been reported in both males and females with a history of myocardial infarction (Aboa-Éboulé et al. 2007, 2011). The occupational stressors observed in our study may increase cardiovascular risk in paramedics. In accordance with Selye’s (1978) theory, occupational stress may progressively lead to over-activity of the autonomic nervous system, resulting in a variety of maladaptive outcomes such as the development of mental health impairments, cardiovascular diseases, metabolic syndrome and obesity (Backé et al. 2009; Sluiter et al. 2003).
The increase in the prevalence of job strain beyond 10 years of employment seems to be mainly caused by high psychological demands (Hegg-Deloye et al. 2014b). It is possible that physical deconditioning associated with age and sedentary behavior, ultimately paired with physical, sensory and cognitive regressions due to normal aging, may affect paramedics’ perception of their workload.
The increase in the prevalence of the iso-strain after 10 years of employment is mainly due to the lack of social support of the hierarchy (Hegg-Deloye et al. 2014b). The literature confirms the crucial role of support for the health of workers since it acts as an important moderator in the onset of work-related health problems. The presence of social support to ensure dialogue and exchanges among workers and between workers and management increases the possibility of relieving tensions at work at the time they happen (Johnson et al. 1989). Lack of time and space for discussion represents a predisposing factor for a lack of social support. Sometimes, the subject is “taboo” in the sense that individuals will not risk communicating their emotions and feelings in order to avoid looking weak or unsuitable for the job. At other times, it is difficult to obtain social support because the colleague applied to is also in emotional overload (Bourbonnais et al. 2011).
Sex differences
To our knowledge, the present study is the first to evaluate cardiovascular risk factors in female paramedics. Our results showed that, over time, fewer female than male paramedics self-reported one or more cardiovascular risk factors. From a historical perspective, it is not surprising that the workforce has been male dominated. In recent decades, some progress has been made in the recruitment process, allowing for equal opportunity employment. According to census data (Service Canada 2013), women held more than 23 % of the jobs in this occupation in 2006, a percentage that had increased significantly since 1991 (16 %). It is possible that the stressors experienced by the first women to enter the workforce were different than those experienced by more recent female recruits. Moreover, many paramedics of both sexes leave their jobs to seek less demanding careers as they grow older (Ohman et al. 2002; Rodgers 1998; Sterud et al. 2006). It is possible that female paramedics are more prone to early retirement because of the physical and psychological demands of the job and the high risk of occupational injuries.
Individual and organizational strategies
Several individual strategies exist to reduce body weight, tobacco consumption and stress such as diet, exercise, muscle relaxation and meditation. However, each of these strategies depends on individual volition and persistence to achieve success. Moreover, individual actions may provide only temporary relief if work represents the source of the problem. Thus, organizational interventions can address the roots of the stress process (Denissen 2000). With regard to the Job Content Questionnaire and the effort–reward imbalance model, organizational interventions could focus on social support, psychological demands, decision latitude and effort versus reward. However, the nature of the intervention must be specific and depends on the target group and its organizational requirements.
Many empirical studies have found evidence of the effect of psychosocial constraints at work on physical and emotional health outcomes including cardiovascular disease, depression and burnout (Stansfeld and Candy 2006; Van der Doef and Maes 1999). With respect to cardiovascular risk factors, several studies have reported an unexpected positive impact on employees’ sleeping problems and systolic blood pressure after organizational interventions were implemented (Bourbonnais et al. 2011; Guimont et al. 2006). For example, 3 years after the implementation of an intervention to reduce adverse psychosocial work factors (psychological demands, decision latitude, social support and effort–reward imbalance), positive effects on the health status of workers receiving the intervention were observed, while the control group’s health deteriorated (Bourbonnais et al. 2011). As well, Guimont et al. (2006) found that systolic blood pressure decreased in white-collar male and female workers with low job strain. These positive effects were probably observed because the underlying stress process was removed by the organizational interventions; however, stress factors may still be present when individual strategies are applied (Denissen 2000). This emphasizes the importance of focusing on organizational intervention in addition to interventions at the level of the individual.
Limitations
The present study has a number of limitations that should be addressed. The questionnaire was self-administered, and therefore the results are subject to participants’ self-awareness. It is also possible that BMI values and tobacco consumption rates were underestimated (Shields et al. 2011). The number of female participants in each work experience category was relatively low, and this may have limited the statistical power. However, to our knowledge, this is the first study reporting on cardiovascular risk factors in female paramedics. In addition, this study is prone to volunteer bias. It is possible that unfit or inactive paramedics, who may have refused to participate, would exhibit a higher BMI, higher tobacco consumption and more occupational stress. If this were the case, then an even higher percentage of paramedics would be at great risk of cardiovascular disease. Shiftwork and long shifts are frequent components of paramedic work schedules. The workers’ history and level of exposure to shift work were not evaluated in this study. Given their known relationship with cardiovascular risk factors and other health problems (Esquirol et al. 2011; Ntawuruhunga et al. 2008), these factors would be relevant to investigate in more detail in this population; the current work schedule alone does not account for all risk.
Conclusion and perspectives
The results of this study are alarming, especially considering that similar observations were made 16 years ago (Gerace and George 1996); they suggest that no action has been taken to reduce cardiovascular risk in paramedics. Furthermore, each individual factor explored in this study represents a risk factor for cardiovascular disease. The main findings suggested that most paramedics present one or more of these factors at some point during their career. To reduce the high risk of cardiovascular disease in paramedics, two complementary approaches are necessary—indeed, urgently required. First, organizational strategies should address occupational stressors; second, individual prevention strategies should aim at increasing paramedics’ awareness of the risks associated with obesity, tobacco use and psychological stress.
References
Aasa U, Kalezic N, Lyskov E, Ängquist KA, Barnekow-Bergkvist M (2006) Stress monitoring of ambulance personnel during work and leisure time. Int Arch Occup Environ Health 80(1):51–59
Aboa-Éboulé C, Brisson C, Maunsell É, Bourbonnais R, Vézina M, Milot A, Théroux P, Dagenais G (2007) Job strain and risk of acute recurrent coronary heart disease events. JAMA 298(14):1652–1660
Aboa-Éboulé C, Brisson C, Blanchette C, Maunsell É, Bourbonnais R, Abdous B, Vézina M, Milot A, Dagenais G (2011) Effort–reward imbalance at work and psychological distress: a validation study of post-myocardial infarction patients. Psychosom Med 73(6):448–455
Alexander DA, Klein S (2001) Ambulance personnel and critical incidents: impact of accident and emergency work on mental health and emotional well-being. Br J Psychiatry 178(1):76–81
Arial M, Benoît D (2011) Apprendre dans l’urgence. Rev Econ Soc 69(2):53–60
Arial M, Pichonnaz L, Benoît D, Danuser B (2009) Rapport court: facteurs et stratégies favorisant la préservation de la santé chez les ambulanciers. Institut universitaire romand de Santé au Travail, Epalinges
Backé E, Kaul G, Klubmann A, Liebers F, Thim C, Mabbeck P, Steinberg U (2009) Assessment of salivary cortisol as stress marker in ambulance service personnel: comparison between shifts working on mobile intensive care unit and patient transport ambulance. Int Arch Occup Environ Health 82(9):1057–1064
Backé E-M, Seidler A, Latza U, Rossnagel K, Schumann B (2011) The role of psychosocial stress at work for the development of cardiovascular diseases: a systematic review. Int Arch Occup Environ Health 85(1):67–69
Barrett TW, Norton VC, Busam M, Boyd J, Maron DJ, Slovis CM (2000) Self-reported cardiac risk factors in emergency department nurses and paramedics. Prehosp Disaster Med 15(2):14–17
Bazzano L, He J, Muntner P, Vupputuri S, Whelton P (2003) Relationship between cigarette smoking and novel risk factors for cardiovascular disease in the United States. Ann Intern Med 138(11):891–897
Bellisle F, Clement K, Le Barzic M, Le Gall A, Guy-Grand B, Basdevant A (2004) The eating inventory and body adiposity from leanness to massive obesity: a study of 2509 adults. Obes Res 12(12):2023–2030
Bennett P, Williams Y, Page N, Hood K, Woollard M (2004) Levels of mental health problems among UK emergency ambulance workers. EMJ 21(2):235–236
Bernier S, Hamel D (2006) Évolution de l’usage de la cigarette chez les Québécois de 15 ans et plus 1994–1995 à 2003. Gouvernement du Québec, Institut national de santé publique du Québec, Québec
Bonnet F, Laville M (2005) Le syndrome métabolique: définition, épidémiologie, complications. Spectra Biol 145:27–29
Bourbonnais R, Jauvin N, Dussault J, Vézina M (2007) Psychosocial work environment, interpersonal violence at work and mental health among correctional officers. Int J Law Psychiatry 30(4–5):355–368
Bourbonnais R, Brisson C, Vézina M (2011) Long-term effects of an intervention on psychosocial work factors among healthcare professionals in a hospital setting. Occup Environ Med 68(7):479–486
Collins SM, Karasek RA, Costas K (2005) Job strain and autonomic indices of cardiovascular disease risk. Am J Ind Med 48(3):182–193
Corbeil P, Prairie J (2012) Bilan de connaissances sur les risques pour la santé liés au métier de technicien ambulancier paramédical [Literature review of job related health risks for paramedics]. Trav Santé 28(3):S3–S10
Cornier M-A, Després J-P, Davis N, Grossniklaus DA, Klein S, Lamarche B, Lopez-Jimenez F, Rao G, St-Onge M-P, Towfighi A, Poirier P (2011) Assessing adiposity. Circulation 124(18):1996–2019
Craig PL, Caterson ID (1990) Weight and perceptions of body image in women and men in a Sydney sample. Community Health Stud 14(4):373–383
Dallman MF, Pecoraro NC, La Fleur SE, Warne JP, Ginsberg AB, Akana SF, Laugero KC, Houshyar H, Strack AM, Bhatnagar S, Bell ME (2006) Glucocorticoids, chronic stress, and obesity. Prog Brain Res 153:75–105
Denissen J (2000) Effectiveness of preventive stress interventions: a quantitative and qualitative review of effect and its predictors. Diploma thesis, University of Nijmegen, Netherlands
Esquirol Y, Perret B, Ruidavets JB, Marquie JC, Dienne E, Niezborala M, Ferrieres J (2011) Shift work and cardiovascular risk factors: new knowledge from the past decade. Arch Cardiovasc Dis 104(12):636–668
Foss B, Dyrstad SM (2011) Stress in obesity: cause or consequence? Med Hypotheses 77(1):7–10
Gerace TA, George VA (1996) Predictors of weight increases over 7 years in fire fighters and paramedics. Prev Med 25(5):593–600
Guimont C, Brisson C, Dagenais GR, Milot A, Vézina M, Masse B, Moisan J, Laflamme N, Blanchette C (2006) Effects of job strain on blood pressure: a prospective study of male and female white-collar workers. Am J Public Health 96(8):1436–1443
Hays NP, Roberts SB (2008) Aspects of eating behaviors “disinhibition” and “restraint” are related to weight gain and BMI in women. Obesity 16(1):52–58
Hays NP, Bathalon GP, McCrory MA, Roubenoff R, Lipman R, Roberts SB (2002) Eating behavior correlates of adult weight gain and obesity in healthy women aged 55–65 y. Am J Clin Nutr 75(3):476–483
Hegg-Deloye S, Brassard P, Jauvin N, Prairie J, Larouche D, Poirier P, Tremblay A, Corbeil P (2014a) Current state of knowledge of post-traumatic stress, sleeping problems, obesity and cardiovascular disease in paramedics. Emerg Med J 31(3):242–247
Hegg-Deloye S, Brassard P, Prairie J, Larouche D, Jauvin N, Tremblay A, Corbeil P (2014b) Portrait global de l’exposition aux contraintes psychosociales au travail des paramédics québécois. PISTES 16(3)
Hegg-Deloye S, Corbeil P, Brassard P, Prairie J, Larouche D, Jauvin N, Carmichael P, Poirier P, Tremblay A (2014c) Work-related and dietary factors associated with weight gain over the period of employment in paramedics. Occup Med Health Aff 2(4):173. doi:10.4172/2329-6879.1000173
Heikkilä K, Nyberg ST, Fransson EI, Alfredsson L, De Bacquer D, Bjorner JB, Bonenfant S, Borritz M (2012) Job strain and tobacco smoking: an individual-participant data meta-analysis of 166 130 adults in 15 European studies. PLoS One 7(7):354–363
Jackson R, Lawes CM, Bennett DA, Milne RJ, Rodgers A (2005) Treatment with drugs to lower blood pressure and blood cholesterol based on an individual’s absolute cardiovascular risk. Lancet 365(9457):434–441
Jakubowicz D, Froy O, Wainstein J, Boaz M (2011) Meal timing and composition influence ghrelin levels, appetite scores and weight loss maintenance in overweight and obese adults. Steroids 77(4):323–331
Johnson JV, Hall EM, Theorell T (1989) Combined effects of job strain and social isolation on cardiovascular disease morbidity and mortality in a random sample of the Swedish male working population. Scand J Work Environ Health 15(4):271–279
Karasek R (1985) Job content questionnaire and user’s guide. University of Southern California, Los Angeles
Karasek R, Theorell T (1990) Healthy work; stress, productivity and the reconstruction of working life. Basic Books, New York
Kivimaki M, Nyberg ST, Batty GD, Fransson EI, Heikkila K, Alfredsson L, Bjorner JB, Borritz M, Burr H, Casini A, Clays E, De Bacquer D, Dragano N, Ferrie JE, Geuskens GA, Goldberg M, Hamer M, Hooftman WE, Houtman IL, Joensuu M, Jokela M, Kittel F, Knutsson A, Koskenvuo M, Koskinen A, Kouvonen A, Kumari M, Madsen IE, Marmot MG, Nielsen ML, Nordin M, Oksanen T, Pentti J, Rugulies R, Salo P, Siegrist J, Singh-Manoux A, Suominen SB, Vaananen A, Vahtera J, Virtanen M, Westerholm PJ, Westerlund H, Zins M, Steptoe A, Theorell T (2012) Job strain as a risk factor for coronary heart disease: a collaborative meta-analysis of individual participant data. Lancet 380(9852):1491–1497
Koehoorn M, Demers PA, Wong I, Kirkham T, Du W, Rempel K, Karlen B, Davies H, Talling D (2011) Cardiovascular disease among British Columbia paramedics. WorkSafeBC, Richmond
Kouvonen A, Kivimäki M, Virtanen M, Pentti J, Vahtera J (2005) Work stress, smoking status, and smoking intensity: an observational study of 46 190 employees. J Epidemiol Community Health 59(1):63–69
Maguire BJ, Hunting KL, Smith GS, Levick NR (2002) Occupational fatalities in emergency medical services: a hidden crisis. Ann Emerg Med 40(6):625–632
Mitani S, Fujita M, Shirakawa T (2006) Circadian variation of cardiac autonomic nervous profile is affected in Japanese ambulance men with a working system of 24-h shifts. Int Arch Occup Environ Health 79(1):27–32
Niedhammer I, Siegrist J, Landre MF, Goldberg M, Leclerc A (2000) Étude des qualités psychométriques de la version française du modèle du déséquilibre Efforts/Récompenses. Rev Epidemiol Santé Publique 48:419–437
Ntawuruhunga E, Chouanière D, Danuser B, Praz-Christinaz SM (2008) Effects of shift work on health. Rev Med Suisse 4(181): 2581–2582, 2584–2585
Ohman U, Bylund P, Bjornstig U (2002) Impairing injuries among medical personnel. West J Nurs Res 24(7):788–802
Park J (2009) Obesity on the job. Statistics Canada 75-001-X, http://www.statcan.gc.ca/pub/75-001-x/2009102/article/10789-eng.htm
Poulter N (1999) Coronary heart disease is a multifactorial disease. Am J Hyper 12(10 Pt 2):92S–95S
Provencher V, Drapeau V, Tremblay A, Despres JP, Lemieux S (2003) Eating behaviors and indexes of body composition in men and women from the Quebec family study. Obes Res 11(6):783–792
Rodgers LM (1998) A five-year study comparing early retirements on medical grounds in ambulance personnel with those in other groups of health service staff. Occup Med 48(1):7–16
Selye H (1978) The stress of life. McGraw Hill, New York
Service Canada (2013) Ambulance attendants and other paramedical occupations. http://www.servicecanada.gc.ca/eng/qc/job_futures/statistics/3234.shtml. Accessed 7 October 2014
Shields M, Connor Gorber S, Janssen I, Tremblay MS (2011) Bias in self-reported estimates of obesity in Canadian health surveys: an update on correction equations for adults. Statistics Canada 82-003-X, http://www.statcan.gc.ca/pub/82-003-x/2011003/article/11533-eng.htm
Shoneye C, Johnson F, Steptoe A, Wardle J (2011) A qualitative analysis of black and white British women’s attitudes to weight and weight control. J Hum Nutr Diet 24(6):536–542
Siegrist J (1996) Adverse health effects of high effort low-reward conditions. J Occup Health Psychol 1(1):27–41
Sluiter JK, Van der Beek AJ, Frings-Dresen MHW (2003) Medical staff in emergency situations: severity of patient status predicts stress hormone reactivity and recovery. Occup Environ Med 60(5):373–375
Stansfeld S, Candy B (2006) Psychosocial work environment and mental health—a meta-analytic review. Scand J Work Environ Health 32:443–462
Sterud T, Ekeberg O, Hem E (2006) Health status in the ambulance services: a systematic review. BMC Health Serv Res 6(82). doi:10.1186/1472-6963-6-82
Sterud T, Hem E, Ekeberg O, Lau B (2008) Health problems and help-seeking in a nationwide sample of operational Norwegian ambulance personnel. BMC Public Health 8(3). doi:10.1186/1471-2458-8-3
Tsismenakis AJ, Christophi CA, Burress JW, Kinney AM, Kim M, Kales SN (2009) The obesity epidemic and future emergency responders. Obesity 17:1648–1650
Van der Doef M, Maes S (1999) The job demand-control(-support) model and psychological well-being: a review of 20 years of empirical research. Work Stress 13(2):87–114
Vézina M, Cloutier E, Stock S, Lippel K, Fortin É, Delisle A, St-Vincent M, Funes A, Duguay P, Vézina S, Prud’homme P (2011) Enquête québécoise sur des conditions de travail, d’emploi et de SST [Quebec survey on working and employment conditions and occupational health and safety] (EQCOTESST). Institut de recherche Robert-Sauvé en Santé et en Sécurité du Travail, Montreal
World Health Organization (2013) Cardiovascular diseases (CVDs). http://www.who.int/mediacentre/factsheets/fs317/en/. Accessed 28 March 2014
World Heart Federation (2011) Cardiovascular disease risk factors. http://www.world-heart-federation.org/press/fact-sheets/cardiovascular-disease-risk-factors/. Accessed 20 May 2013
Acknowledgments
We gratefully acknowledge the editing work and suggestions by Zofia Laubitz. This study was supported by a Grant from the Institut de recherche Robert-Sauvé en santé et en sécurité du travail (IRSST). Dr. Poirier is a senior clinician-scientist with the Fonds de recherche du Québec—Santé (FRQS). Dr. Brassard is a Junior 1 Research Scholar with the FRQS.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hegg-Deloye, S., Brassard, P., Prairie, J. et al. Prevalence of risk factors for cardiovascular disease in paramedics. Int Arch Occup Environ Health 88, 973–980 (2015). https://doi.org/10.1007/s00420-015-1028-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-015-1028-z