Abstract
Purpose
To introduce a novel technique for small-incision levator resection in ptosis surgery and evaluate its efficacy in a pilot study among patients affected by congenital or aponeurotic ptosis.
Methods
We prospectively enrolled congenital and aponeurotic ptosis patients if their levator function was not poor (≥5 mm) from June 2021 through October 2022. Surgical technique involved a 1-cm lid crease incision, minimal dissection, and creating a loop passing through the tarsus and levator aponeurosis. Success was defined as postoperative MRD-1 ≥3 mm and inter-eyelid MRD-1 difference ≤1 mm. Eyelid contour quality was scored excellent, good, fair, and poor according to its curvature and symmetry.
Results
Sixty-seven eyes (35 congenital and 32 aponeurotic) were included in the study. Mean age was 34±19 years (range, 5–79 years). Mean preoperative levator function and levator resection amount were 9.53 mm and 8.39 mm in the congenital group and 12.34 mm and 4.15 mm in the aponeurotic group, respectively. Mean pre- and postoperative MRD-1 was 1.61 mm and 3.27 mm respectively (P<0.001). The overall success rate was 82.1% (95% C.I: 71.7–89.8%); the result was failure in 12 cases, of which 11 had under-correction. Preoperative MRD-1 was correlated with a success rate (P=0.017).
Conclusion
The described technique shows non-inferior results to the previously described surgical methods and also it shows very good lid contour outcome and minimal lag. The findings suggest that the double mattress single suture technique can be used in both congenital and aponeurotic ptosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction

Blepharoptosis is a condition in which the upper eyelid is lower than normal. This condition narrows the vertical dimension of the palpebral fissure. It may be congenital or acquired. Ptosis may either be unilateral or bilateral and can be seen either alone or in conjunction with other ocular or systemic conditions [1]. Ptosis severity is categorized according to the drooping of the upper eyelid which can be mild (1–2 mm), moderate (3–4mm), or severe (>4mm), covering the pupil entirely [2]. Surgical correction is recommended not only for cosmetic reasons but also for the prevention of visual deficits. Beard subdivided levator function (LF) into 4 levels: excellent (≥12 mm), good (8 to 11 mm), fair (5 to 7 mm), and poor (≤4 mm) [3]. Patients with poor LF (less than 5 mm of levator excursion) were classically offered frontalis sling procedures. Several types of surgeries can be used in the treatment of congenital ptosis, according to its severity and levator muscle function. Good or excellent LF can usually be corrected by levator resection, levator advancement, or Muller’s Muscle-Conjunctival Resection (MMCR) procedures [4]. Another procedure for correcting mild to moderate ptosis with a similar degree of levator function is the levator plication technique [5].
External levator resection/advancement procedure involves an incision on the upper eyelid crease. Traditionally, it was performed through a large total crease length incision and repaired with three separate sutures [6], but in recent years small-incision procedures with less manipulation and reduced scar have been introduced and gained popularity, which was first described by Lucarelli and Lemke [7,8,9].
Here we describe a new technique to less invasive, small-incision ptosis repair with a specific manner of one double mattress suture placement and report the preliminary results on the aponeurotic and congenital ptosis patients. We expected less intraoperative manipulation and edema, less visible scar, less lagophthalmos, and a better and smoother contour forming and yet a comparable success rate; on the other hand, single suture technique can decrease surgery costs.
Methods
Patient selection and study design
This prospective case series study included 67 congenital and aponeurotic ptosis patients which presented to the Farabi eye hospital from June 2021, through October 2022. Patients were offered the new small-incision surgery technique, and the likely post-treatment results and potential complications were explained to all patients. Written consent was obtained from all patients, which included permission to publish their photos. All included patients were operated by a single oculoplastic surgeon (S.M.R.) in a single center.
Patients aged 5 years or more whose LF was not poor (≥5 mm) with unilateral or bilateral, congenital, or aponeurotic ptosis were included in the study. Exclusion criteria included less than 5 years of age, poor LF (less than 5 mm), absent lid crease, poor Bell’s phenomenon, moderate to severe dry eye, decreased corneal sensation, lid masses, known neurologic or muscular syndromes, other associated developmental lid anomalies, or a history of previous lid surgery.
This research was approved by the ethical board of our institute and was adherent to the ethical principles outlined in the Declaration of Helsinki as amended in 2013.
Preoperative assessment
All patients provided a full medical history and received a detailed ophthalmological examination. Preoperative measurements for both eyes included MRD-1, levator function (LF), and lagophthalmos, all measured in millimeters. The factors considered for differentiation of congenital vs. aponeurotic ptosis included time of onset of ptosis based on patient’s history, position of lid margin in downward gaze (lid lag indicated congenital type, while lid drop indicated aponeurotic type), and unilateral elevated upper eyelid crease, which was in favor of aponeurotic rather than congenital ptosis.
Surgical technique
First of all, the lid crease is marked at length of 1 cm, approximately equal to the corneal diameter (white to white) and then local anesthetics consisting of 1 cc of lidocaine 2% mixed with adrenaline (with a concentration of 1:100,000) was injected under skin at the mark site. Then, a traction suture was placed in the upper eyelid margin by the 4.0 silk thread 17 mm 1/2 circle round.
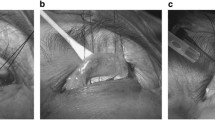
After that, skin incision was made on the mark site (Fig. 1A). The tissue dissection was performed under the orbicularis oculi muscle. The dissection was performed over the septum and also over the tarsus, then the septum was opened and the preaponeurotic fat prolapsed and the levator muscle was identified below it. Then the levator muscle was separated from the upper end of the tarsus (Fig. 1B).
One-centimeter skin incision in the crease of the left upper eyelid (A); dissection of the levator muscle (B); passing the Mersilene suture from the tarsus and the levator aponeurosis on the lateral side (C); the needle enters from the dorsal side of the levator aponeurosis and exits from its ventral side (D); passing the needle again through the tarsus on the medial side of the eyelid (E); the exit of the needle from the levator aponeurosis is a few millimeters away from the first arm, while both arms come out from under the created loop (F–H); resecting the levator aponeurosis after making the suture permanent (I)
The first suture was made as follows: a 5-0 Mersilene® (Polyester Fiber Suture) white 1×18" S-14 double-armed needle was passed between the central and upper third of the tarsal height about the lateral limbus level, and after passing through the aponeurosis of the levator muscle (according to the severity of ptosis and the amount of levator muscle function), it was temporarily tightened (Fig. 1C). In cases of local anesthesia, the patient was asked to sit and the correction of ptosis was checked. If the amount of correction on the lateral side as well as the contour of the eyelid was appropriate, the operation continued, but if it was not acceptable, it was corrected as follows:
-
1.
In cases where the amount of correction was still under, suture was transferred to a higher position at the levator muscle level.
-
2.
In cases where the amount of correction was over, the suture was moved to a lower area at the levator muscle level.
-
3.
Regarding the contour, if there was a deformed notch, the suture was removed from the tarsus and passed through a higher area of the tarsus, and in cases where the peak of the eyelid contour was moved too much toward the lateral or central area (instead of the lateral limbus), the suture was removed from the tarsus and repositioned toward the opposite side to bring the peak area to a cosmetically optimal lateral place over the lateral limbus.
After the place and the amount of modification of the first suture were found to be suitable, now we have reached the stage of making the second suture using the same thread. For this purpose, the outer arm of the thread is passed over the central arm of the thread and entered from the dorsal surface of the levator (the same levator height as the previous suture) and above the medial limbus and exited from the ventral surface of the levator (Fig. 1D); then after passing through the tarsus (from medial to lateral) around the medial limbus level (Fig. 1E), it was passed through levator again (on the opposite direction of the entrance) medial to the entry thread and the suture was temporarily tightened with the other end (both ends of the thread are exited under the created loop) (Fig. 1F, G and H).
After re-checking the amount of correction and the contour of the eyelid, the suture was permanently tightened. Then, the excess amount of levator muscle was resected (Fig. 1I) and the skin was repaired using 3–4, 6.0 nylon sutures which were also passed through the levator muscle in order to create a skin crease. Then, the eye was patched with erythromycin eye ointment. The next day of surgery, the dressing was removed and lubricant drops and antibiotic eye ointment were started (Fig. 2).
Follow-up and analysis
Patients had follow-up visits on the 10th day of surgery for skin suture removal, also at 6 weeks and 3 months after surgery. At follow-up visits, MRD-1, lagophthalmos, and lid contour quality were evaluated. Primary outcome variable was MRD-1 of the operated eye(s) after at least 3 months of surgery.
Success was defined as postoperative MRD-1 ≥3 mm, and inter-eyelid MRD-1 difference ≤1 mm in unilateral cases (Fig. 3). In bilateral cases, the same criteria were used, but if the inter-eyelid MRD-1 difference was greater than 1 mm, one eyelid was considered successful and the other a failure. Failure was defined as under correction; postoperative MRD-1 <3 mm or operated eyelid >1 mm lower than the fellow eye, or over-correction; postoperative MRD-1 >5 mm or operated lid >1 mm higher than the fellow eye [9].
Lid contour quality scoring (Fig. 4) was defined as follows: if the curvature was normal, without any irregularities, and symmetric with the fellow eye, it was labeled “excellent”; if the curvature was normal and smooth but had some asymmetry, it was called “good”; lower or higher placement of one side of the lid in comparison to the fellow eye was considered “fair”; and if there was notch, unexpected elevation, or depression, it was considered a “poor” eyelid contour. It was evaluated at final follow-up visit.
Lid contour quality scoring. OS: excellent, the curvature is normal, without any irregularities, and symmetric with the fellow eye (A); OD: good, the curvature is normal and smooth but has some asymmetry (B); OS: fair, lower placement of the medial side of the lid in comparison to the fellow eye (C); none of the cases had a poor scored lid contour
Statistical analysis was performed using the software IBM SPSS Statistics version 26.0 (SPSS Inc. Chicago, IL), and P value of <0.05 was considered significant. For determination of the statistical significance of the difference between preoperative and postoperative values of MRD-1, paired t test was used. Non-parametric Mann-Whitney test results determined the significance of a positive correlation between success rate and the preoperative MRD-1 measurements.
Results
Sixty-seven eyes of 62 patients with significant blepharoptosis who were candidates for external levator resection (ELR) from June 2021 through October 2022 met the criteria to be included in this study. The mean patients’ age was 34±19 (range, 5–79 years). There were 23 (37.1%) males and 39 (62.9%) females. Five patients underwent bilateral surgery of whom one was male and the rest were females, and unilateral surgery was performed for the remaining 57 patients. Of unilateral cases, 33 and 24 were right- and left-sided respectively. Thirty-five eyes (52.2%) had congenital and 32 (47.8%) had aponeurotic ptosis.
The age of the congenital patients ranged from 5 to 56 years (median, 18 years, interquartile range: 13–30). Degree of ptosis was mild in 30 (44.8%) eyes, moderate in 21 (31.3%) eyes, and severe in 16 (23.9%) eyes. Of the total 62 patients, 51 (82.3%) and 11 (17.7%) patients were operated under local and general anesthesia, respectively. Mean preoperative levator function (LF) was 9.53±2.78 mm (range, 5.0–14.5 mm). Mean preoperative MRD1 was 1.80±0.83 mm (range, −0.7 to 3.0 mm), which increased to 3.28±0.41 mm postoperatively (range, 2.5–4.2 mm). Mean levator resection amount was 8.39±3.14 mm (range, 2–15 mm).
In the aponeurotic group, patients aged from 22 to 79 years (median, 51 years, interquartile range: 39–61). Mean preoperative levator function was 12.34±1.8 mm (range, 8.0–14.5 mm). Mean preoperative MRD1 was 1.39±1.02 mm (range, −1.0 to 3.0 mm), which was measured 3.25±0.83 mm postoperatively (range, 1.5–5.6 mm). Levator resection amount was 4.15±3.24 mm on average (range, 0–15 mm). All of the bilateral cases had aponeurotic ptosis.
Altogether mean preoperative levator function was 10.87±2.74 mm (range, 5.0–14.5 mm). Preoperative MRD-1 measurement for each ptotic eye on average was 1.61±0.94 mm, which increased to 3.27±0.64 mm postoperatively (paired t-test; P <0.001). Mean Levator resection amount was 6.39±3.81 mm (range, 0–15 mm).
The overall success rate on the last follow-up visit was 82.1% (95% C.I: 71.7–89.8%). The result was a failure in 12 cases (17.9%), of which 11 were under-corrected and one was overcorrected, also 2 were congenital, and 10 were aponeurotic. Among congenital cases, success was 88.6% (95% C.I: 75.1–96.0%) and between aponeurotic patients was 75% (95% C.I: 58.3–87.4%). Eyelid contour quality was excellent in 48 cases (71.6%), good in 18 cases (26.9%), fair in 1 case (1.5%), and none was poor.
According to the degree of ptosis, success rate was 96.7%, 81%, and 56.3% among mild, moderate, and severe cases, respectively, which is statistically significant (P=0.003, Fisher’s exact test). Success rate was 82.4% and 81.8% in the groups with local and general anesthesia, respectively, which was not statistically significant (P>0.05). Among failed surgeries, 10 eyes were operated under local anesthesia and 2 eyes under general anesthesia.
Mean preoperative MRD-1 in the subgroup with successful outcome was 1.73 mm which was significantly more than the failure subgroup, in which it was 1.00 mm (Mann-Whitney test; P=0.017). There was no significant correlation between age, preoperative LF, and amount of levator resection with final outcome (P >0.05).
There were no intraoperative complications. Postoperative complications were very rare, including lagophthalmos which was observed only in 4 cases (6.1%), all with congenital ptosis, and mild lid swelling and redness in two cases which was alleviated in the last follow-up visit. No exposure keratopathy was observed.
Discussion
Previously many surgical methods were reported to be effective and evolved the external ptosis repair such as the single-suture aponeurotic tuck by Liu [10], the single adjustable suture for aponeurosis plication by Meltzer et al. [11], small-incision ptosis repair in aponeurotic ptosis by Lucarelli and Lemke [7], minimal dissection in small-incision method for aponeurotic cases by Frueh et al. [8], and small-incision method for congenital cases by Eshraghi et al. [9].
Small-incision levator resection technique has many advantages over the traditional method, which have been discussed in detail in the literature previously, including improved accuracy due to reduced dissection, tissue edema, and hemorrhage, preserved anatomical structures, and less surgery time [7, 8].
Described techniques scarcely provided a clear suture placing protocol or even number of sutures. Lucarelli and Lemke [7] performed suture placement intraoperatively using toothed forceps to gauge appropriate placement. They placed single suture in most cases, but 7% required an additional suture. Frueh et al. [8] used a vertical line passing the center of the pupil as a guide to placing their suture and in 30% of patients they needed additional sutures to achieve appropriate contour. Baroody et al. [12] reported a large series by using levator aponeurosis excision and placing 2 to 3 sutures, but presented no precise manner for determining their placement. Also Bernardini et al. [13] described no specific suture placement algorithm in their small-incision ptosis repair using single-suture placement.
In this study, we presented a novel technique for suture placement in a small-incision surgery which has a stepwise standardized protocol and can easily adjust the lid contour and positioning during the surgery. Other advantages of this method are the use of one single Mersilene thread in a large loop (approximately equal to corneal diameter) which is not only cost beneficial, but also improves postoperative lid contour quality, due to distributing the force of elevation over the lid margin, instead of creating points of traction observed in other methods. Also, there will be no need for additional sutures for revising lid contour during surgery, which is sometimes encountered in other described techniques. This method also has all abovementioned advantages of minimally invasive, small-incision surgery. On the other hand, we showed in our series that this new technique is effective for both types of congenital and aponeurotic ptosis.
The results of our study are comparable with prior literature on small-incision external ptosis repair. Overall, the eyelids of 82.1% of patients met the criteria for success, which has a 95% confidence interval between 71.7 and 89.8%. In one study Frueh et al. [8] compared the outcome of their small incision, minimal dissection (SIMD) method with the traditional approach, and they reported a success rate of 66.7% which is inferior to our results; success criteria was defined as less than 0.5-mm difference in eyelid height and MRD-1 of 2 to 4 mm from the center of the pupil. Also, they reported a good lid contour in 97.6% of SIMD cases which was significantly better than the traditional approach. We reported a good or excellent contour quality in 98.5% of cases.
Lucarelli and Lemke [7] in their retrospective review of 28 eyelids with aponeurotic ptosis which had undergone small-incision (8 mm) levator repair reported satisfactory results of final eyelid position and contour in 25 cases (89.3%). The advantages mentioned for their surgical method included decreased amount of local anesthetic required and minimizing dissection and time of surgery, which results in less bleeding and edema during operation, so more accurate intraoperative assessment of eyelid position can be achieved. Also, they reported less scarring, which could facilitate further dissection if re-operation was indicated. Success rate in our series is less yet comparable to their report.
Ahuero et al. [14] reported a success rate of 74% of their 66 patients (defined as less than 1-mm difference of MRD-1 of the two eyes). The success rate is included in the 95% confidence interval of our study. Selected cases and criteria are almost similar in both studies.
In another study, Ranno et al. [6] retrospectively compared the outcome of standard levator advancement with small-incision technique. They defined success according to the criteria set by British Oculoplastic Surgery Society: postoperative MRD-1 between 3 and 5 mm, inter-lid MRD-1 difference of 1 mm or less, inter-lid crease difference of 2 mm or less, and the presence of symmetrical lid contour [15]. Success rate was statistically equal between two methods in cases with good levator function (>10 mm), but the small-incision technique was inferior in patients with moderate levator function (5 to 10 mm). They suggested wider surgical field, better exposure, and greater amount of resection as the possible rationalization.
Eshraghi et al. [9] in their series enrolled 50 congenital ptosis cases and reported a success rate of 74.5%. Their definition of success was similar to ours. The coverage of their reported rate in our 95% confidence interval shows non-inferiority of our technique. In their study, better levator function was associated with more successful results.
In a large retrospective 10-year review of congenital ptosis patients presented to the Birmingham children’s hospital, 19.67% of 110 eyes which had undergone external levator resection required reoperation [16]. Therefore, our results (17.9% failure) seem comparable to the latter study and are a reasonable failure rate. Our findings are also consistent with prior external ptosis repair studies with success rates ranging from 54 to 96% [7, 8, 10, 17, 18]. On the other hand, 10 out of 12 cases with failure were old patients (over 50 years of age) and had aponeurotic ptosis. It seems dehiscent tissue which has caused the ptosis itself can be the reason of failure in these cases. The other 2 cases were congenital ptosis which were operated under general anesthesia. This can be a possible reason for miscorrection. Limitations of our study include the limited sample size, short follow-up period, and its preliminary nature, which makes it difficult to compare the efficiency of our technique to others.
Conclusion
Our new technique of small-incision levator resection with one double mattress suture using a Mersilene thread shows non-inferior results to the previously described surgical techniques and also it shows very good lid contour results and minimal lag. This method has several advantages, including using a single thread, lower costs, simplicity, and ease of reversibility when adjusting the eyelid height, and acceptable cosmetic results. The findings suggest that the double mattress single suture technique can be used in both congenital and aponeurotic ptosis.
Data availability
The dataset generated during this study is available upon reasonable request.
References
SooHoo JR, Davies BW, Allard FD, Durairaj VD (2014) Congenital ptosis. Surv Ophthalmol 59:483–492. https://doi.org/10.1016/j.survophthal.2014.01.005
Finsterer J (2003) Ptosis: causes, presentation, and management. Aesthet Plast Surg 27:193–204. https://doi.org/10.1007/s00266-003-0127-5
C. B (1976) Ptosis. CV Mosby Co.
Göncü T, Çakmak S, Akal A, Karaismailoğlu E (2015) Improvement in levator function after anterior levator resection for the treatment of congenital ptosis. Ophthalmic Plast Reconstr Surg 31:197–201. https://doi.org/10.1097/iop.0000000000000242
Hong SP, Song SY, Cho IC (2014) Under–through levator complex plication for correction of mild to moderate congenital ptosis. Ophthalmic Plast Reconstr Surg 30:468–472. https://doi.org/10.1097/iop.0000000000000135
Ranno S, Sacchi M, Gonzalez MO, Ravula MT, Nucci P (2014) Evaluation of levator function for efficacy of minimally invasive and standard techniques for involutional ptosis. Am J Ophthalmol 157:209–213.e201. https://doi.org/10.1016/j.ajo.2013.08.005
Lucarelli MJ, Lemke BN (1999) Small incision external levator repair: technique and early results. Am J Ophthalmol 127:637–644. https://doi.org/10.1016/s0002-9394(99)00064-1
Frueh BR, Musch DC, McDonald HM (2004) Efficacy and efficiency of a small-incision, minimal dissection procedure versus a traditional approach for correcting aponeurotic ptosis. Ophthalmology 111:2158–2163. https://doi.org/10.1016/j.ophtha.2004.07.019
Eshraghi B, Ghadimi H (2018) Small-incision levator resection for correction of congenital ptosis: a prospective study. Graefes Arch Clin Exp Ophthalmol 256:1747–1750. https://doi.org/10.1007/s00417-018-4008-7
Liu D (1993) Ptosis repair by single suture aponeurotic tuck. Ophthalmology 100:251–259. https://doi.org/10.1016/s0161-6420(93)31662-3
Meltzer MA, Elahi E, Taupeka P, Flores E (2001) A simplified technique of ptosis repair using a single adjustable suture. Ophthalmology 108:1889–1892. https://doi.org/10.1016/s0161-6420(01)00712-6
Baroody M, Holds JB, Sakamoto DK, Vick VL, Hartstein ME (2004) Small incision transcutaneous levator aponeurotic repair for blepharoptosis. Ann Plast Surg 52:558–561. https://doi.org/10.1097/01.sap.0000123354.69226.45
Bernardini FP, de Conciliis C, Devoto MH (2006) Mini-invasive ptosis surgery. Orbit 25:111–115. https://doi.org/10.1080/01676830600671425
Ahuero AE, Winn BJ, Sires BS (2012) Standardized suture placement for mini-invasive ptosis surgery. Arch Facial Plast Surg 14:408–412. https://doi.org/10.1001/archfacial.2012.388
Scoppettuolo E, Chadha V, Bunce C, Olver JM, Wright M (2008) British Oculoplastic Surgery Society (BOPSS) National Ptosis Survey. Br J Ophthalmol 92:1134–1138. https://doi.org/10.1136/bjo.2007.132746
Berry-Brincat A, Willshaw H (2009) Paediatric blepharoptosis: a 10-year review. Eye (Lond) 23:1554–1559. https://doi.org/10.1038/eye.2008.311
Bartley GB, Lowry JC, Hodge DO (1996) Results of levator-advancement blepharoptosis repair using a standard protocol: effect of epinephrine-induced eyelid position change. Trans Am Ophthalmol Soc 94:165–173 discussion 174-167
Shore JW, Bergin DJ, Garrett SN (1990) Results of blepharoptosis surgery with early postoperative adjustment. Ophthalmology 97:1502–1511. https://doi.org/10.1016/s0161-6420(90)32384-9
Author information
Authors and Affiliations
Contributions
Study design and material preparation were performed by Seyed Mohsen Rafizadeh. Data analysis was performed by Mahdi Soleymanzadeh. Kosar Esmaili and Mahdi Soleymanzadeh collected the data of this paper. The first draft of the manuscript was written by Mahdi Soleymanzadeh, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This research was approved by the ethical board of the Tehran University of Medical Sciences and was adherent to the ethical principles outlined in the Declaration of Helsinki as amended in 2013.
Consent to participate
Written informed consent was obtained from all the study participants.
Consent for publication
The informed consent included the permission to publish their photos.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Soleymanzadeh, M., Esmaili, K. & Rafizadeh, S.M. A novel technique for small-incision levator resection with a double mattress suture for ptosis correction. Graefes Arch Clin Exp Ophthalmol 261, 3607–3613 (2023). https://doi.org/10.1007/s00417-023-06126-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-023-06126-w