Abstract
Purpose
To determine the rate of success of small-incision levator resection technique for correction of congenital ptosis.
Methods
Patients with congenital ptosis who were candidates for levator resection were enrolled if their levator function was not poor (< 5 mm). Incisions were made on upper eyelid crease with a length of 10–12 mm. After resection of adequate length of levator muscle, two sutures were used to fix it to tarsal plate. Sliding the incision to medial and lateral sides provided a wider field of access to allow the surgeon to place the sutures above nasal and temporal borders of limbus. Success was defined as margin reflex distance-1 (MRD-1) ≥ 3 mm and inter-eyelid difference of MRD-1 less than 1 mm, which was considered excellent if inter-eyelid difference was < 0.5 mm and good if the latter parameter was between 0.5 and 1 mm.
Results
Fifty eyes of 47 congenital ptosis cases (16 males and 31 females) were included. Average age was 21.7 ± 9.7 years (range, 3–44 years). Mean preoperative levator function and MRD-1 were 11.26 ± 2.79 and 1.78 ± 0.92 mm, respectively, while postoperative MRD-1 increased to 3.95 ± 0.82 mm (P < 0.001). The result was failure (undercorrection) in 12 cases (25.5%), good in 9 patients (19.2%), and excellent in 26 cases (55.3%).
Conclusions
Small-incision levator resection has previously been studied for correction of aponeurotic ptosis and proved to yield successful outcome. The findings of this study suggest that small-incision technique can be effectively used in correction of congenital ptosis, as well.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
External levator resection/advancement is the classical approach to upper eyelid ptosis correction [1]. This procedure involves an incision on the upper eyelid crease. Considering the growing interest toward less invasive methods and the benefits mentioned for smaller incisions (including more rapid surgical time, faster wound healing, and reduced visibility of scar) [2], techniques with smaller incisions have gained popularity. Ptosis correction with small-incision external levator resection/advancement has been studied with remarkable success in aponeurotic ptosis [3,4,5,6,7,8]. However, to our knowledge, no other manuscript in the English-language literature applies the small-incision technique to congenital ptosis. Herein, we present our experience with small-incision levator resection for congenital ptosis cases.
Methods
We prospectively included all congenital ptosis patients who underwent small-incision levator resection in a single center by an oculoplastic surgeon (B.E.) between February 2016 and July 2017. The study was approved by ethical board of our institute and adhered to the tenets of the Declaration of Helsinki as amended in 2008. All patients or their legal guardians agreed to participate in the study by signing the informed consent form and were followed at least 3 months after surgery.
Indications for ptosis surgery in this study depended on severity of ptosis and patients’ age. Mild asymmetry of eyelid position (margin reflex distance-1 (MRD-1) difference < 2 mm between the two eyes) was not considered an indication for surgery in unilateral ptosis cases. Similarly, for cases with mild bilateral ptosis (MRD-1 > 3), this technique was not performed. For those older than 6 years, the patients’ (or their parents’) request to have a better appearance was considered significant, while in children under age 6 years, chin-up head posture was the indication for ptosis surgery. Inclusion criteria were congenital ptosis patients with indication for surgical intervention (as mentioned above) who had not undergone previous ptosis surgery and had at least moderate levator function (≥ 5 mm). Exclusion criteria were other types of ptosis, history of previous ptosis surgery, poor levator function (< 5 mm), impaired Bell’s reflex, decreased orbicularis oculi muscle force, poor corneal sensation, severe dry eye, and presence of Marcus-Gunn jaw winking phenomenon. Small children (younger than 3 years) who were at higher risk of amblyopia due to ptosis [9] (e.g., had occluded visual axis) were also excluded, because in this group, we preferred sling procedure.
Preoperative measurements for both eyes included MRD-1, palpebral fissure height (PF), levator function (LF), and lagophthalmos, all measured in millimeters. Levator function was defined as moderate for values between 5 and 10 mm and good for values above 10 mm. The factors considered for differentiation of congenital vs. aponeurotic ptosis included time of onset of ptosis based on patient’s history, position of lid margin in downward gaze (lid lag indicated congenital type, while lid drop indicated aponeurotic type), and unilateral elevated upper eyelid crease, which was in favor of aponeurotic rather than congenital ptosis.
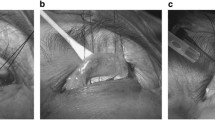
Anesthesia was either general or local, with subcutaneous injection of 1 mL of lidocaine 2%. Skin marking was drawn on actual or desired location of upper eyelid crease with a length of 10–12 mm. Silk traction suture was used to pull upper lid downwards and facilitate the procedure. Following skin incision, dissection toward lid margin underneath orbicularis oculi was performed to expose upper surface of tarsal plate for placement of two partial thickness 5-0 Mersilene sutures on the tarsus somewhere between the upper third and the middle third of the height of tarsal plate. Sliding the incision to medial and lateral sides, using skin hooks, provided a wider field of surgery. The lateral suture was located lateral to temporal limbus and the medial suture was placed medial to nasal limbus. Further dissection followed by opening orbital septum and exposing levator aponeurosis under preaponeurotic fat pad was performed. After incorporating enough length of levator muscle, the two sutures were temporarily tied. Amount of levator resection, hence the location of sutures tied on levator, was adjusted based on MRD-1 in supine and/or sitting position (in those operated under local anesthesia). Then, a strip of redundant levator was resected and hemostasis was achieved with bipolar cautery. During all the steps of surgery, sliding the incision to medial and lateral sides was performed with skin hooks in order to enable us to expose more length of upper lid and provide a wider field compared to the original skin incision. Finally, the skin incision was closed with three separate 6-0 Prolene sutures which involved levator stump in order to create an esthetically acceptable eyelid crease. Postoperative topical antibiotics and lubricating eye drops and ointments were prescribed. Patients were visited on postoperative days 1, 7, 30, and 90.
Primary outcome variable was MRD-1 of the operated eye(s) at 90th postoperative day visit. Excellent result was defined as MRD-1 ≥ 3 mm and the difference of MRD-1 of the two eyes ≤ 0.5 mm. Good result was defined as MRD-1 ≥ 3 mm and the difference of MRD-1 of the two eyes between 0.5 and 1 mm, exclusive. Failure was subdivided into under- and overcorrection. Undercorrection was defined as either MRD-1 < 3mm or MRD-1 of operated eye > 1 mm lower than that of fellow eye. Overcorrection was defined as either MRD-1 > 5mm or MRD-1 of operated eye > 1 mm higher than that of fellow eye.
Statistical analysis was performed using the software IBM SPSS Statistics version 20.0 (SPSS Inc. Chicago, IL), and P value of < 0.05 was considered significant. For determination of statistical significance of the difference between preoperative and postoperative values of MRD-1, paired t test was used. Fisher’s exact test results determined the significance of differences between success in the groups with moderate and good LF and in groups with operation under general or local anesthesia. Statistical significance of the difference between mean ages of patients who had success or failure after operation was determined using unpaired t test.
Results
Fifty eyes of 47 congenital ptosis patients were included in this study. Three cases were bilateral, 22 cases had an involvement of the right eye, and 22 patients had ptosis of the left eye. Sixteen patients were male, all with unilateral ptosis. Thirty-one patients were female, of whom three cases had bilateral ptosis. Patients aged 21.7 ± 9.7 years on average (range, 3–44 years). Operations were performed under general anesthesia in ten cases who were too young (age range 3–12 years) to cooperate in awake state. The rest (40 eyes of 37 patients) were operated with local anesthesia. Mean duration of operation for each ptotic eyelid was 23 min (range, 15–35 min).
Preoperative LF was 11.26 ± 2.79 mm on average (range, 5–15 mm), which was categorized as moderate in 15 eyelids (30%) and good in the remaining 35 eyelids (70%). Mean MRD-1 for each ptotic eyelid before surgery was 1.78 ± 0.92 mm which increased to 3.95 ± 0.82 mm postoperatively (P < 0.001). Among the 47 congenital ptosis patients, the result was failure (undercorrection) in 12 cases (25.5%), good in 9 patients (19.2%), and excellent in 26 cases (55.3%). Overall, success (good or excellent outcome) was achieved in 35 of 47 patients (74.5%). In the sub-group with moderate preoperative LF, seven cases (46.7%) had successful outcome, compared to 28 patients (87.5%) with successful results in the group with good LF (P = 0.009). Success was achieved in 31 (83.7%) of patients who had their operation performed under local anesthesia, compared to 4 (40%) of those who underwent general anesthesia (P = 0.014). Mean age was significantly higher in those with successful outcome (23.4 ± 8.9 years) than those who failed to achieve success (16.8 ± 10.7 years, P = 0.041).
Complications were infrequently observed including asymmetric lid crease in two cases (the difference between lid crease heights of the two eyes was < 2 mm) and eyelash ptosis in one case. In two other patients, the final position of medial side of upper lid was lower than that of lateral side. One patient had intermittent swelling of the operated eyelid that lasted 3 months and gradually resolved.
Discussion
In the present study, minimal incision levator resection was used for correction of congenital ptosis. Previous similar studies included aponeurotic ptosis cases [3,4,5,6,7,8], but to our knowledge, there was only one study (in French language) that enrolled congenital ptosis patients operated with this method [10]. It is noteworthy that some of our congenital ptosis patients were adults who had ptosis since birth but desired surgery in later years to gain better appearance, and not all of congenital ptosis cases were children in this series.
The length of standard incision for external levator resection/advancement is almost equal to the entire length of the eyelid crease, averaging 20–22 mm [11]. Small incisions have gained popularity for the procedure since introduction by Lucarelli and Lemke [3]. In their retrospective review of 28 eyelids of 17 patients with aponeurotic ptosis who had undergone small-incision (8 mm) levator repair, satisfactory results of final eyelid position and contour were achieved in 25 eyelids (89.3%). The advantages mentioned for their small-incision approach included decreased amount of local anesthetic required and minimizing dissection, hence less bleeding and edema in the site of operation, allowing more accurate intraoperative assessment of eyelid position. Other benefits included shorter operation time and less scarring, which could facilitate further dissection if re-operation was indicated for unsatisfactory results [3]. While the success of the operation in our series of congenital ptosis cases is lower, the rate of success among patients with good preoperative LF is comparable with the mentioned study (87.5 vs. 89.3%).
In another study by Frueh et al., the outcome of small-incision surgery was compared to the traditional approach for ptosis correction. The small-incision technique was superior in achieving better eyelid contour and shortening the operation time (from 56 to 26 min, on average). Rate of achievement of excellent result was not significantly different in the two groups (66.7% in small-incision method vs. 61.1% in traditional approach) and was slightly higher than in this study (55.3%) [4].
Ahuero et al. reported symmetric eyelid positions (defined as less than 1-mm difference of MRD-1 of the two eyes) in 74% of their 66 patients [7]. Both the definition of success and the final outcome are similar to our findings (74.5% overall success in this study), with the only difference being inclusion of aponeurotic ptosis in the study by Ahuero et al. and inclusion of congenital ptosis in our study.
In a retrospective comparison, Ranno et al. evaluated the outcome of standard levator advancement with small-incision technique [11]. They defined success according to the criteria set by British Oculoplastic Surgery Society: postoperative MRD-1 between 3 and 5 mm, inter-lid margin reflex distance difference of 1 mm or less, inter-lid crease difference of 2 mm or less, and the presence of symmetrical lid contour [12]. Based on the preoperative levator function, they categorized the patients into two groups: moderate levator function (between 5 and 10 mm) and good levator function (> 10 mm). The results of the study showed comparable outcomes between standard and small-incision methods in patients with good levator function (success rates 95.2 and 94.7%, respectively). However, in patients with moderate levator function, standard incision technique was superior in terms of outcome compared to the small-incision procedure (success rates 81.8 and 66.7%, respectively). An explanation suggested by the authors for superiority of standard incision was providing wider surgical field, allowing better exposure and visualization of anatomic structures, and facilitating greater amount of levator resection [11].
Similarly, the narrow field of surgery due to small incision was an issue we encountered. In the beginning of our experience with the small-incision approach, operations were performed with incision lengths of 8 mm and without sliding the incisions. However, in some cases (particularly in young children), the eyelid contour became dome-shaped, because the two levator sutures were located close to each other. After a while, for improving the results and having better visualization and wider field of operation, we used longer incisions (10–12 mm) as well as “the sliding technique” of displacing the incision to medial and lateral sides with traction by two skin hooks, like the method used for minimal incision external dacryocystorhinostomy in the study by Kashkouli et al. [13]. Sliding the incision is generally easier in older patients with laxer skin and facilitates access to the most temporal and nasal parts of the tarsus. On the contrary, in younger patients and children with stiffer skin, sliding is less feasible, although it still allows us to place the sutures on tarsal plate adjacent to the medial and lateral borders of the limbus and achieve better eyelid contours postoperatively. The patients included in the present study were those who underwent ptosis surgery after we had modified our operation technique (sliding the 10–12-mm incisions).
To our knowledge, the present study is the first in English-language literature on the outcome of small-incision levator resection for congenital ptosis. In our series, the success rate of congenital ptosis operations was 74.5%. In a 10-year review of congenital ptosis patients in the UK who were treated with various procedures, 19.67% of those operated with standard anterior approach levator resection required re-operation [14]. Therefore, our results (25.5% failure in congenital ptosis cases) seem comparable to the latter study.
In the only other study that evaluated the outcome of small-incision levator resection in 21 congenital ptosis cases, Gire et al. found no statistically significant difference in the need to re-operation between the mentioned technique and Whitnall’s sling [10]. However, the authors state that this technique is more suitable for mild or moderate congenital ptosis cases with good levator function, but is not as effective as traditional approaches for severe congenital ptosis with poor levator function. In our series, too, the latter group was excluded and was instead operated by frontalis sling method.
Our study had several limitations including a relatively small group of patients and short follow-up. However, a previous study by Doxanas showed that overcorrection or undercorrection is evident at 1 week post operation, and late recurrence was not seen in the 150 patients followed for at least 3 years [15]. Therefore, our 3-month follow-up period seems to be adequate.
In conclusion, the present study showed high success of small-incision levator resection in correction of congenital ptosis. However, scarcity of large-scale trials with long-term follow-up on effectiveness of small-incision levator resection particularly in congenital ptosis calls for larger studies before this technique could be strongly recommended in such cases.
References
Mehta S, Belliveau MJ, Oestreicher JH (2013) Oculoplastic surgery. Clin Plast Surg 40(4):631–651. https://doi.org/10.1016/j.cps.2013.08.005
Dortzbach R, Woog JJ (1990) Small-incision techniques in ophthalmic plastic surgery. Ophthalmic Surg 21(9):615–622
Lucarelli MJ, Lemke BN (1999) Small incision external levator repair: technique and early results. Am J Ophthalmol 127(6):637–644
Frueh BR, Musch DC, McDonald HM (2004) Efficacy and efficiency of a small-incision, minimal dissection procedure versus a traditional approach for correcting aponeurotic ptosis. Ophthalmology 111(12):2158–2163. https://doi.org/10.1016/j.ophtha.2004.07.019
Baroody M, Holds JB, Sakamoto DK, Vick VL, Hartstein ME (2004) Small incision transcutaneous levator aponeurotic repair for blepharoptosis. Ann Plast Surg 52(6):558–561
Bernardini FP, de Conciliis C, Devoto MH (2006) Mini-invasive ptosis surgery. Orbit 25(2):111–115. https://doi.org/10.1080/01676830600671425
Ahuero AE, Winn BJ, Sires BS (2012) Standardized suture placement for mini-invasive ptosis surgery. Arch Facial Plast Surg 14(6):408–412. https://doi.org/10.1001/archfacial.2012.388
Elabjer BK, Busic M, Elabjer E, Bosnar D, Sekelj S, Krstonijevic EK (2009) Microincision aponeurotic ptosis surgery of upper lid. Coll Antropol 33(3):915–918
Kasaee A, Yazdani-Abyaneh A, Tabatabaie SZ, Jafari AK, Ameri A, Eshraghi B, Samarai V, Mireshghi M, Rajabi MT (2010) Assessing amblyogenic factors in 100 patients with congenital ptosis. Int J Ophthalmol 3(4):328–330. https://doi.org/10.3980/j.issn.2222-3959.2010.04.12
Gire J, Robert PY, Denis D, Adenis JP (2011) Small-incision, minimal dissection procedure (Frueh’s procedure) in correction of involutional and congenital ptosis: a retrospective study of 119 cases. J Fr Ophtalmol 34(7):439–447. https://doi.org/10.1016/j.jfo.2011.01.017
Ranno S, Sacchi M, Gonzalez MO, Ravula MT, Nucci P (2014) Evaluation of levator function for efficacy of minimally invasive and standard techniques for involutional ptosis. Am J Ophthalmol 157 (1):209–213 e201. https://doi.org/10.1016/j.ajo.2013.08.005
Scoppettuolo E, Chadha V, Bunce C, Olver JM, Wright M, Bopss (2008) British Oculoplastic Surgery Society (BOPSS) national ptosis survey. Br J Ophthalmol 92 (8):1134–1138. https://doi.org/10.1136/bjo.2007.132746
Kashkouli MB, Jamshidian-Tehrani M (2014) Minimum incision no skin suture external dacryocystorhinostomy. Ophthal Plast Reconstr Surg 30(5):405–409. https://doi.org/10.1097/IOP.0000000000000131
Berry-Brincat A, Willshaw H (2009) Paediatric blepharoptosis: a 10-year review. Eye (Lond) 23(7):1554–1559. https://doi.org/10.1038/eye.2008.311
Doxanas MT (1992) Simplified aponeurotic ptosis surgery. Ophthalmic Surg 23(8):512–515
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval/research involving human participants
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Eshraghi, B., Ghadimi, H. Small-incision levator resection for correction of congenital ptosis: a prospective study. Graefes Arch Clin Exp Ophthalmol 256, 1747–1750 (2018). https://doi.org/10.1007/s00417-018-4008-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-018-4008-7