Abstract
Purpose
To produce an economic comparison of the iStent ab interno trabecular microbypass implant accompanying cataract surgery and selective laser trabeculoplasty (SLT) as first-line treatment versus topical medications for open-angle glaucoma in New Zealand in 2016.
Methods
The current annual costs of 19 available fully subsidised topical glaucoma medications by Pharmaceutical Management Agency (Pharmac) in 2016 were identified. Adjustments for pharmacist prescribing charges and previously described wastage levels were applied. The costs to perform iStent implantation and the cost to perform SLT were obtained from the local distributors, with the latter taking into account staff and consumable cost. Procedure costs divided by eye drops’ cost produced a break-even level in equivalent years of eye drops use.
Results
The range of annual eye drop cost was NZD$42.25 to NZD$485.11, with an average of NZD$144.81. Comparison of annual eye drop cost with iStent cost revealed 3 of 19 (15.8%) drops breaking even within 5 years, 9 of 19 (47.3%) within 10 years, and 12 of 19 (63.2%) within 15 years. The cost of bilateral SLT performed by a consultant was NZD$102.30 (breaking even in 0.71 years). The equivalent cost for a registrar was NZD$97.59 (breaking even in 0.67 years).
Conclusion
Economically, the iStent would appear to be a reasonably cost-effective treatment for glaucoma patients undergoing cataract surgery in a public healthcare setting in New Zealand, particularly for those using more expensive topical glaucoma medications, whilst SLT appears to be a worthwhile consideration as a first-line treatment for glaucoma in New Zealand.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glaucoma is a chronic progressive neurodegenerative disease characterised by optic nerve head axonal degeneration and retinal ganglion cell death. It is the global leading cause of irreversible blindness [1]. Its most prevalent form in the Western world is open-angle glaucoma (OAG). Glaucoma poses a major worldwide public health burden with prevalence in 60.5 million people as of 2010, and this is expected to rise to 80 million by 2020, with the majority remaining undiagnosed [2]. The significant costs to patients and health providers are undeniable in the form of direct financial burden, indirect expenses incurred by visual loss and deteriorated quality of life [3,4,5,6].
The current mainstay of glaucoma treatment is intraocular pressure (IOP) reduction. Topical IOP-lowering medications are usually first-line treatment; however, this could be complicated by patient noncompliance [3, 4, 7,8,9,10,11], inappropriate administration [12,13,14], as well as local and systemic side effects [15,16,17]. Invasive surgical techniques such as trabeculectomy and glaucoma drainage surgery are typically associated with various post-operative complications [18,19,20,21,22,23].
Newer, less-invasive surgical techniques termed minimally invasive glaucoma surgery (MIGS) are garnering worldwide attention for their ability to reduce patients’ dependence on topical glaucoma medications with reduced complication rates and shorter recovery times. One MIGS device, the iStent trabecular microbypass stent (Glaukos Corporation, CA, USA), is a one-piece heparin-coated titanium, nonferromagnetic device that is inserted into Schlemm’s canal either as a standalone procedure or following successful cataract surgery, through a temporal clear corneal incision, under direct gonioscopy. It lowers IOP by providing a direct aqueous outflow channel from the anterior chamber to the collector channels [24,25,26,27]. Current data shows iStent longevity of at least 5 years [28]. A recent meta-analysis by Malvankar-Mehta et al. showed weighted mean reduction in topical glaucoma medications following an iStent implant and phacoemulsification was 1.33, for a follow-up period of 1 to 5 years [28]. Another meta-analysis by Malvankar-Mehta et al. found 22% IOP reduction and mean reduction of 1.2 bottles per patient of topical medication achieved at 18 months after one iStent implant as a solo procedure [29].
Laser trabeculoplasty technology was introduced in 1979 with argon laser trabeculoplasty (ALT) [30]. Initial efficacy was similar to topical therapy, and it had an excellent safety profile. However, ALT did not replace topical therapy as first-line treatment, rather taking on an adjunctive role in glaucoma treatment and for failed topical therapy prior to surgical intervention. This was due to the introduction of more effective topical medications, prostaglandin analogues, as well as diminishing efficacy over time. The relatively new technology of selective laser trabeculoplasty (SLT) utilises a green (532 nm), Q-switched, frequency-doubled Nd:YAG laser [31] and employs the principle of selective photothermolysis at which laser thermal energy is directed at selected pigmented cells within an exposed area. Various theories have suggested the role of laser trabeculoplasty in thermal-induced trabecular tissue contraction and alteration of cellular activity resulting in increased aqueous outflow and decreased IOP [32]. SLT has been shown to be less histologically destructive to the trabecular meshwork compared with ALT, and as such, the benefit of repeatability has been suggested, with suggestion of similar repeat treatment efficacy compared to primary treatment efficacy [33,34,35,36]. Whilst maintaining similar initial efficacy compared to topical treatment [37,38,39], Li et al. showed that SLT is similar to glaucoma medication (latanoprost only as well as combination medication) in IOP reduction for a follow-up period of up to 5 years [38].
A difficulty in introducing both techniques to the public healthcare system has been the perceived cost, compared to traditional primary management with topical medications. With more and more public health systems developing cost-based models, cost analyses have gained more value alongside efficacy and safety analyses in planning services for a population.
Comparison of clinical effectiveness between eye drops, laser and surgery is also difficult partly because there is no universally accepted outcome measure for glaucoma treatment. Current applications for submission for new products to the Food and Drug Administration in the USA include showing non-inferiority to an established medication such as latanoprost. Li et al. showed an equivalence between SLT and eye drops [38], and a meta-analysis by Malvankar-Mehta et al. found iStent insertion combined with cataract surgery being equivalent to 1.33 eye drops [28]. The clinical effectiveness of these three interventions is therefore taken to be close enough for direct comparison of costs to become meaningful for a cost minimisation analysis to aid the planning of glaucoma care in a hospital eye services setting. This becomes relevant under several clinical settings, including choosing initial treatment for a newly diagnosed case, choosing between options when additional treatment is indicated in an established case, and knowledge of available options to treat glaucoma when a patient is to have cataract surgery. These are all common clinical scenarios and with equivalent clinical effectiveness for these three treatment modalities a comparison of their cost will help with clinical decision making and planning for service infrastructure development.
The setting for our analysis is an ophthalmic glaucoma service in a public hospital healthcare setting in New Zealand. Economic considerations are becoming increasingly important in the planning of departmental infrastructure, choosing whether to implement new treatments, and resource allocation including capital, staffing and clinic space. Cost minimisation analyses help address these issues currently and provide a basis for comparison of other treatments as they become available in the future.
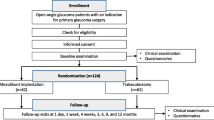
Methods
The Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement was used as a guide to report the study, including strategies for data analysis, result presentation, potential bias, data interpretation and writing [40].
Glaucoma treatment cost may be derived from many sources which may be direct or indirect, and to minimise variability in this relative cost minimisation analysis, we aimed to compare the direct relative cost of implanting the iStent post-cataract surgery and the direct relative cost of performing SLT within the public healthcare system versus direct costs incurred by the New Zealand Pharmaceutical Management Agency (Pharmac) for topical glaucoma medications. Our target population were patients newly diagnosed with glaucoma requiring initiation of treatment, and patients with previously diagnosed glaucoma using topical glaucoma medications, either requiring a change to their current treatment or undergoing cataract surgery to treat a symptomatic cataract.
First, we identified the 2016 per-bottle direct costs of all Pharmac-subsidised topical glaucoma medications [41]. These were categorised into six types, as listed in Table 1. Prostaglandin analogues and prostamides consisted of bimatoprost 0.03% (Bimatoprost Actavis), latanoprost 0.005% (Hysite) and travoprost 0.004% (Travatan). Beta-blockers were made up of betaxolol 0.25% (Betoptic S), betaxolol 0.5% (Betoptic), levobunolol 0.25 and 0.5% (Betagan), timolol 0.25 and 0.5% (Arrow-Timolol) and Timoptol-XE 0.25 and 0.5%. Beta-blocker compound preparations included brimonidine tartrate 0.2%/timolol 0.5% (Combigan) and dorzolamide 2%/timolol 0.5% (Arrow-Dortim). The only subsidised sympathomimetic was brimonidine tartrate 0.2% (Arrow-Brimonidine), and the only subsidised carbonic anhydrase inhibitor was brinzolamide 1% (Azopt). Miotics comprised of pilocarpine hydrochloride 0.5%, 1 and 2% (Isopto Carpine), as well as pilocarpine nitrate 2% (Minims Pilocarpine Nitrate). Non-fully subsidised medications were excluded.
Assuming each bottle lasted a month as per the manufacturers’ shelf life once opened, the annual cost for each medication was calculated by multiplying the per-bottle cost by 12. Adjustments applied were twofold; pharmacist prescribing charges were $5.30 per script per 3 months [42], whilst previously described wastage levels by Platt et al. increased the calculated annual cost by 21% to account for misadministration of medication and patient noncompliance [43]. The latter was a Canadian retrospective study that analysed the prescription refill frequency in 27,000 patients [43].
The number of Pharmac-subsidised community-dispensed glaucoma medication prescriptions was also obtained from the Ministry of Health to provide information on the frequency of different prescriptions.
For the iStent cost comparison arm, the 2016 cost of one iStent implant (model GTS-100) of $1200 was provided by the local distributor. This assumed that infrequent iStent insertion did not increase the overall cost for an operating session. The cost for a keratome and viscoelastic were excluded for iStent insertion as these would have been already included in routine cataract surgery. The cost of a goniolens was also not considered due to assumed long lens life and to avoid variability. The iStent cost divided by annual eye drop cost produced a break-even level in equivalent years of eye drop use.
For the SLT cost comparison arm, SLT cost was calculated from a total of staff cost, machine cost and consumable cost. The 2016 annual salary of a mid-level payscale consultant (Step 7), registrar (Year 4), and registered nurse (Step 3) were determined from their respective collective agreements with New Zealand’s District Health Boards [44,45,46]. The staff cost per half day clinical session, staffed by either a registrar or consultant and registered nurse were calculated. It was assumed that consultants performed seven SLT procedures per half day session whilst the less experienced registrars performed five similar procedures, and that each treatment was bilateral using 100 shots through 360° in each eye.
The cost of an appropriate SLT laser was obtained from the local distributor. Consumables included in standard SLT therapy at our centre were lens coupling solution, oxybuprocaine 0.4% topical ocular anaesthetic and one drop of brimonidine 0.2% into each eye post-procedure. Similar to the iStent cost analysis arm, the cost of a goniolens was not considered due to assumed long lens life and to avoid variability. Machine and consumable cost was added to staff cost to produce the total cost for a half day clinical session and subsequent cost for bilateral SLT treatment per patient.
Results
The individual annual eye drop costs are listed in increasing order in Table 1. Timolol (Arrow-Timolol) and latanoprost (Hysite) were notably the cheapest at $42.25 and $42.98 annually, respectively, with approximately 28 corresponding iStent $1200 equivalent years. The least cost-effective medications were brimonidine/timolol (Combigan) ($289.82 annually), travoprost (Travatan, $304.34 annually) and pilocarpine nitrate (Minims, $485.11 annually), all of which calculated to less than five iStent equivalent years.
In terms of average annual cost of medication categories in increasing order, sympathomimetics were the cheapest ($83.93), followed by beta-blockers ($99.75), prostaglandin analogues and prostamides ($140.51), carbonic anhydrase inhibitors ($163.06), beta-blocker compound preparations ($180.56) and miotics ($201.07). The overall average eye drop cost was $144.81.
Comparison of average eye drop cost with iStent cost revealed a break-even timescale of 2.47 to 28.40 years, with 3 of 19 (15.8%) drops breaking even within 5 years, 9 of 19 (47.3%) within 10 years, and 12 of 19 (63.2%) within 15 years (Figs. 1 and 2).
The cost of the SLT laser (Ellex Solo, Ellex, Adelaide, Australia) was NZD$65,000, and its longevity is an estimated 400,000 shots. For bilateral SLT treatments at 100 shots through 360° per eye a laser can be expected to perform 2000 treatments at a cost of NZD$32.50 per treatment. The mid-tier salaries of a consultant, registrar and nurse in New Zealand in 2016 were NZD$181,000, NZD$98,625 and NZD$56,865 respectively. With 261 working days in New Zealand in 2016 the salary per half day session were NZD$346.74, NZD$189.05 and NZD$108.94 for a consultant, registrar and nurse, respectively. This produces a combined medical staff salary cost per laser of NZD$65.10 for a seven-patient consultant clinic and NZD$59.60 for a five-patient registrar clinic. Consumable costs and the cost per SLT laser are shown in Table 2.
The cost of bilateral SLT performed by a consultant was NZD$102.30, and the cost of a registrar was NZD$97.59. Comparison of average eye drop cost with SLT cost revealed a break-even timescale of 0.71 years for SLT performed by a consultant and 0.67 years for SLT performed by a registrar, and versus latanoprost (our usual first-line eye drop) 2.38 years and 2.27 years for a consultant and registrar, respectively.
Table 3 shows the frequencies of prescriptions subsidised by Pharmac for each of the available glaucoma eye drops for the period 2007–2016 [47]. In 2016, Pharmac subsidised 217,680 community-dispensed prescriptions, of which 104,081 (47.8%) were for medications which cost up to NZD$49.99 per year, and 67,139 (30.8%) were for medications which cost NZD$50.00 to NZD$99.99 per year. Of the remaining 21.4% (46,480 prescriptions), 9.6% (20,878) were for medications costing NZD$100 to NZD$199.99 per year, 6.2% (13,489) were for medications costing between NZD$200 and NZD$299.99 per year, 5.6% (12,089) between NZD$300 and NZD$399.99, and 4 prescriptions were for pilocarpine minims at NZD$485.11 per year [47].
Discussion
Our study was one of cost analysis and not cost effectiveness, investigating the direct relative cost of iStent insertion at the time of cataract surgery, and the direct relative cost of performing SLT versus the direct cost of topical glaucoma medications to the public health system. Specifically, it fits best into a cost minimisation analysis (CMA) according to the definitions provided by the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement [40].
However, for this study, the consequences of compared interventions, iStent insertion post-cataract surgery, SLT and topical glaucoma medications, are only assumed to be equivalent. For the iStent, the cohort of patients addressed is patients with OAG already undergoing cataract surgery, and as such does not significantly modify their risks. A 2016 review by Song summarised a low complication rate of SLT, and these cases were generally transient and minor [48]. On the other hand, therapeutic equivalence between iStent insertion (with or without phacoemulsification) and SLT with topical glaucoma medications has been demonstrated, according to Malvankar et al. (up to 5 years) [28] and Li et al. (up to 5 years) [38].
About half of fully subsidised eye drops in New Zealand will “break-even” with the iStent $1200 cost after 10 years. Of interest, a 2014 Canadian cost analysis of the iStent versus glaucoma medications by Iordanous et al. showed that the cumulative average cost of one glaucoma medication equalised with the iStent cost (based on the use of two iStents) at 6 years, with the iStent actually providing a cost saving of CAD$249.32 by then [49]. However, in New Zealand, the more expensive topical glaucoma medications are less likely to be prescribed, with the exception of brinzolamide 1% (Azopt), brimonidine tartrate 0.2%/timolol 0.5% (Combigan) and travoprost 0.004% (Travatan), which accounted for 7.8%, 5.8%, and 5.6% of all glaucoma prescriptions in New Zealand in 2016, respectively [47].
The cost analysis for iStent insertion is different from the other two arms in this report. We have considered iStent insertion when a patient who has been listed for cataract surgery primarily to treat their cataract also has glaucoma. Under these circumstances, the patient will be attending theatre for cataract surgery, and the costs of this are already committed by the hospital. The addition of iStent insertion under those settings means that a patient spends an extra 5 to 10 min in surgery. This combination of modest case frequency and time required per case has meant that the number of operations booked for a list is unchanged whether there are cases requiring iStent insertion or not. We have therefore not included theatre facility and staffing costs, or productivity costs from introducing increased surgical time or surgical cases in the iStent arm of our study as we have assumed these will not change with the introduction of iStent insertion under these circumstances (which is in fact our experience at our regional centre with this, however, this may vary with larger centres). We have also not included any consumable costs as these are already incorporated into the cataract operation. We also assumed that an ophthalmic theatre will be equipped with the equipment required for iStent insertion: an operating microscope capable of tilting to 45° and an appropriate surgical goniolens. There are of course many other costs to intraocular surgery and to introducing a new technique to a service. These include ordering and storage, administrative costs, time with patients, training and professional development, as well as operating theatre costs. These include direct and indirect costs and have not been included in our analysis. We have also excluded any cases where cataract surgery is planned because changing the patient’s glaucoma treatment by insertion of an iStent is desired, which would increase the relative cost of iStent insertion in these cases. It is also noteworthy that even with phacoemulsification and iStent implantation, some patients will still be dependent on topical glaucoma medications after a mean reduction of 1.33 medications. Moreover, it must be taken into account that phacoemulsification alone has been shown to reduce a mean range of 0.23 (phacoemulsification as a solo procedure) to 1.01 (comparing iStent with and without concurrent phacoemulsification) topical glaucoma medications [28].
The duration of iStent effectiveness remains unknown. It has been shown that its effect can last at least 5 years [28], but 10-year data does not exist. Many of the procedures in the currently evolving MIGS field have the same issues. Also, the original iStent has been updated to an “iStent inject” GTS-400 model. This will alter its cost and the availability of longevity data on its clinical effectiveness. Our study is based on the original GTS-100 iStent which at the time of writing (2016–2017) is the only model available in New Zealand. For this device, the meta-analysis by Malvankar-Mehta et al. showed an equivalent clinical effect of iStent with cataract surgery to 1.33 eye drops [28], meaning that on average every third patient having iStent insertion will have a clinical response equivalent to two eye drops. These factors need to be taken into consideration when applying our results or methods to compare surgical glaucoma treatment costs against eye drops or SLT.
The calculated cost of bilateral SLT performed by either a consultant or registrar was less than the average annual eye drop cost to Pharmac, and broke even compared to latanoprost after just over 2 years. SLT is known to have a limited time of clinical effectiveness of between 1 and 5 years, with suggestion of initial SLT producing IOP control up to 5 years, and repeated SLT showing similar effect as initial treatment and sustaining IOP control for at least 2 years [33,34,35,36, 38]. This is relevant for an economic analysis and for planning service provision for glaucoma care. Our chosen setting of a public hospital allows simple calculation of staffing costs, and from this laser performed by a junior doctor can be seen to compare well economically despite fewer laser treatments being performed. A drawback for SLT is the timing for capital outlay: our analysis shows that when a laser is used to deliver many treatments then the overall cost per treatment is highly competitive compared with either eye drops or iStent insertion, but the cost for the laser is usually incurred when it is first delivered. Further costs not included in our analysis include infrastructure costs, laser maintenance, and costs to the patient and any accompanying person for attending the treatment and the recovery period afterwards.
Performing SLT as primary treatment for OAG may be a reasonable approach, especially in populations where eye drop supply or compliance is challenging. Likewise for SLT, higher quality studies are required and especially over longer durations. Our data differed from another Canadian cost analysis in 2006 by Lee and Hutnik which showed that the cumulative average cost of one glaucoma medication equalised with cumulative cost for SLT repeated at two-yearly intervals only at 6 years (with saving of CAD$206.54), and equalised at 2 years for SLT repeated at three-yearly intervals (with saving of CAD$68.85). This may be due to higher SLT costs in 2003 in Canada, with 180° bilateral SLT costing CAD$370 [50].
In terms of determining cost of glaucoma medications, we opted to examine only direct costs to Pharmac. Similar to the cost analyses by Iordanous et al. [49] and Lee and Hutnik [50], we did not attempt to approach various direct non-health and indirect costs, such as quality of life, treatment side effects or intolerance, and costs relating to post-operative follow-up or with ongoing treatment. In addition, only fully subsidised medications by Pharmac were included in this study as the other medications were less likely to be prescribed, and in the event they were, patients had to partially if not fully subsidise the difference, and patient costs have not been included in our analysis. Regarding cost borne by the patient, this can be complicated by various indirect costs such as the cost and time taken to travel to their appointments, the cost and time taken to renew a prescription with the general practitioner, the loss of productivity in instilling medications, the cost and time taken for assistance with instilling medications.
The figures from the Pharmac-subsidised prescriptions in 2016 show that more expensive medications are being prescribed with enough frequency to make investigating alternative glaucoma treatments worthwhile, with 21.4% of medications costing more than $100 per year, 11.8% of prescribed medications costing more than $200 per year, and 5.6% costing more than $300 per year. Alternatives such as SLT and iStent should be considered when aiming to minimise the cost of glaucoma care in a public healthcare setting in New Zealand. Both SLT and iStent have proven short-term efficacy and safety profiles; however, lack more vigorous and long-term evidence to compliment cost analyses. Further investigation is required into not only the direct health costs, but also direct non-health costs and indirect costs incurred by glaucoma treatment to assist development of patient-centred therapy.
References
Kingman S (2004) Glaucoma is second leading cause of blindness globally. Bull World Health Organ 82(11):887–888
Quigley HA, Broman AT (2006) The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol 90(3):262–267
Ocansey S, Kyei S, Diafo A, Darfor KN, Boadi-Kusi SB, Aglobitse PB (2016) Cost of the medical management and prescription pattern for primary open angle glaucoma (POAG) in Ghana-a retrospective cross-sectional study from three referral facilities. BMC Health Serv Res 16:282
Rouland JF, Berdeaux G, Lafuma A (2005) The economic burden of glaucoma and ocular hypertension: implications for patient management: a review. Drugs Aging 22(4):315–321
Traverso CE, Walt JG, Kelly SP, Hommer AH, Bron AM, Denis P et al (2005) Direct costs of glaucoma and severity of the disease: a multinational long term study of resource utilisation in Europe. Br J Ophthalmol 89(10):1245–1249
Varma R, Lee PP, Goldberg I, Kotak S (2011) An assessment of the health and economic burdens of glaucoma. Am J Ophthalmol 152(4):515–522
Kass MA, Gordon M, Morley RE Jr, Meltzer DW, Goldberg JJ (1987) Compliance with topical timolol treatment. Am J Ophthalmol 103(2):188–193
Okeke CO, Quigley HA, Jampel HD, Ying GS, Plyler RJ, Jiang Y et al (2009) Adherence with topical glaucoma medication monitored electronically the Travatan Dosing Aid study. Ophthalmology 116(2):191–199
Robin A, Grover DS (2011) Compliance and adherence in glaucoma management. Indian J Ophthalmol 59(Suppl1):S93–SS6
Schwartz GF (2005) Compliance and persistency in glaucoma follow-up treatment. Curr Opin Ophthalmol 16(2):114–121
Tsai JC (2009) A comprehensive perspective on patient adherence to topical glaucoma therapy. Ophthalmology 116(11 Suppl):S30–S36
Gupta R, Patil B, Shah BM, Bali SJ, Mishra SK, Dada T (2012) Evaluating eye drop instillation technique in glaucoma patients. J Glaucoma 21(3):189–192
Mohindroo C, Ichhpujani P, Kumar S (2015) How 'Drug Aware' are our glaucoma patients? Journal of current glaucoma practice 9(2):33–37
Tatham AJ, Sarodia U, Gatrad F, Awan A (2013) Eye drop instillation technique in patients with glaucoma. Eye (London, England) 27(11):1293–1298
Bartlett JD (1991) Adverse effects of antiglaucoma medications. Optometry clinics: the official publication of the prentice. Society 1(1):103–126
Detry-Morel M (2006) Side effects of glaucoma medications. Bull Soc Belge Ophtalmol 299(299):27–40
Schuman JS (2000) Antiglaucoma medications: a review of safety and tolerability issues related to their use. Clin Ther 22(2):167–208
Christakis PG, Kalenak JW, Tsai JC, Zurakowski D, Kammer JA, Harasymowycz PJ et al (2016) The Ahmed versus Baerveldt study: five-year treatment outcomes. Ophthalmology 123(10):2093–2102
Gedde SJ (2009) Results from the tube versus trabeculectomy study. Middle East African Journal of Ophthalmology 16(3):107–111
Gedde SJ, Schiffman JC, Feuer WJ, Herndon LW, Brandt JD, Budenz DL (2009) Three-year follow-up of the tube versus trabeculectomy study. Am J Ophthalmol 148(5):670–684
Heuer DK, Lloyd MA, Abrams DA, Baerveldt G, Minckler DS, Lee MB et al (1992) Which is better? One or two? A randomized clinical trial of single-plate versus double-plate Molteno implantation for glaucomas in aphakia and pseudophakia. Ophthalmology 99(10):1512–1519
Jampel HD, Musch DC, Gillespie BW, Lichter PR, Wright MM, Guire KE (2005) Perioperative complications of trabeculectomy in the collaborative initial glaucoma treatment study (CIGTS). Am J Ophthalmol 140(1):16–22
Nouri-Mahdavi K, Brigatti L, Weitzman M, Caprioli J (1995) Outcomes of trabeculectomy for primary open-angle glaucoma. Ophthalmology 102(12):1760–1769
Fea AM (2010) Phacoemulsification versus phacoemulsification with micro-bypass stent implantation in primary open-angle glaucoma: randomized double-masked clinical trial. J Cataract Refract Surg 36(3):407–412
Ferguson TJ, Berdahl JP, Schweitzer JA, Sudhagoni R (2016) Evaluation of a trabecular micro-bypass stent in pseudophakic patients with open-angle Glaucoma. J Glaucoma 25(11):896–900
Resende AF, Patel NS, Waisbourd M, Katz LJ (2016) iStent (R) trabecular microbypass stent: an update. J Ophthalmol 2016:2731856
Samuelson TW, Katz LJ, Wells JM, Duh YJ, Giamporcaro JE (2011) Randomized evaluation of the trabecular micro-bypass stent with phacoemulsification in patients with glaucoma and cataract. Ophthalmology 118(3):459–467
Malvankar-Mehta MS, Iordanous Y, Chen YN, Wang WW, Patel SS, Costella J et al (2015) iStent with phacoemulsification versus phacoemulsification alone for patients with glaucoma and cataract: a meta-analysis. PLoS One 10(7):e0131770
Malvankar-Mehta MS, Chen YN, Iordanous Y, Wang WW, Costella J, Hutnik CML (2015) iStent as a solo procedure for Glaucoma patients: a systematic review and meta-analysis. PLoS One 10(5):e0128146
Wise JB, Witter SL (1979) Argon laser therapy for open-angle glaucoma. A pilot study Arch Ophthalmol 97(2):319–322
Latina MA, Park C (1995) Selective targeting of trabecular meshwork cells: in vitro studies of pulsed and CW laser interactions. Exp Eye Res 60(4):359–371
Kagan DB, Gorfinkel NS, Hutnik CM (2014) Mechanisms of selective laser trabeculoplasty: a review. Clin Exp Ophthalmol 42(7):675–681
Avery N, Ang GS, Nicholas S, Wells A (2013) Repeatability of primary selective laser trabeculoplasty in patients with primary open-angle glaucoma. Int Ophthalmol 33(5):501–506
Francis BA, Loewen N, Hong B, Dustin L, Kaplowitz K, Kinast R et al (2016) Repeatability of selective laser trabeculoplasty for open-angle glaucoma. BMC Ophthalmol 16:128
Khouri AS, Lari HB, Berezina TL, Maltzman B, Fechtner RD (2014) Long term efficacy of repeat selective laser trabeculoplasty. J Ophthalmic Vis Res 9(4):444–448
Polat J, Grantham L, Mitchell K, Realini T (2016) Repeatability of selective laser trabeculoplasty. Br J Ophthalmol 100(10):1437–1441
De Keyser M, De Belder M, De Belder S, De Groot V (2016) Where does selective laser trabeculoplasty stand now? A review Eye and vision (London, England) 3:10
Li X, Wang W, Zhang X (2015) Meta-analysis of selective laser trabeculoplasty versus topical medication in the treatment of open-angle glaucoma. BMC Ophthalmol 15:107
Wong MO, Lee JW, Choy BN, Chan JC, Lai JS (2015) Systematic review and meta-analysis on the efficacy of selective laser trabeculoplasty in open-angle glaucoma. Surv Ophthalmol 60(1):36–50
Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D et al (2013) Consolidated Health Economic Evaluation Reporting Standards (CHEERS)—explanation and elaboration: a report of the ISPOR Health Economic Evaluation Publication Guidelines Good Reporting Practices Task Force. Value in health: the journal of the International Society for Pharmacoeconomics and Outcomes Research 16(2):231–250
MIMS (NZ) Ltd. MIMS Gateway (2017) http://www.mims.co.nz/MIMSGateway.aspx. Assessed January 2017
Foster R, Preval N, Blakely T, Wilson N, O'Dea D (2011) Costing of Pharmaceuticals in New Zealand for health economic studies: backgrounder and protocol for costing. Department of Public Health UoO, Wellington, Wellington
Platt R, Reardon G, Mozaffari E (2004) Observed time between prescription refills for newer ocular hypotensive agents: the effect of bottle size. Am J Ophthalmol 137(1 Suppl):S17–S23
New Zealand Nurses Organisation (2017) District Health Boards/NZNO Nursing And Midwifery Multi-Employer Collective Agreement 24 August 2015–31 July 2017. http://www.nzno.org.nz/Portals/0/Files/Documents/Support/CA/DHB%20MECA%2024%20Aug%202015%20-%2031%20July%202017WEB.pdf. Accessed July 2017
New Zealand Resident Doctors' Association.(2016) New Zealand Resident Doctors' Association And 20 District Health Boards Multi Employer Collective Agreement 21 January 2015 to 29 February 2016.http://www.nzrda.org.nz/?attachment_id=613. Accessed July 2017
The Association of Salaried Medical Specialists.(2016) New Zealand District Health Boards Senior Medical And Dental Officers Collective Agreement 1 July 2013 Until 30 June 2016. https://www.asms.org.nz/wp-content/uploads/2014/05/2013-16-DHB-MECA-signed_159277.6.pdf. Accessed July 2017
Ministry of Health.(2017) MoH pharmaceutical collection. Accessed September 2017
Song J (2016) Complications of selective laser trabeculoplasty: a review. Clinical ophthalmology (Auckland, NZ) 10:137–143
Iordanous Y, Kent JS, Hutnik CM, Malvankar-Mehta MS (2014) Projected cost comparison of Trabectome, iStent, and endoscopic cyclophotocoagulation versus glaucoma medication in the Ontario Health Insurance Plan. J Glaucoma 23(2):e112–e118
Lee R, Hutnik CM (2006) Projected cost comparison of selective laser trabeculoplasty versus glaucoma medication in the Ontario Health Insurance Plan. Can J Ophthalmol 41(4):449–456
Acknowledgements
The authors thank Scott Morgan for data and biostatistical consultation.
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with human participants performed by any of the authors.
Rights and permissions
About this article
Cite this article
Ngan, K., Fraser, E., Buller, S. et al. A cost minimisation analysis comparing iStent accompanying cataract surgery and selective laser trabeculoplasty versus topical glaucoma medications in a public healthcare setting in New Zealand. Graefes Arch Clin Exp Ophthalmol 256, 2181–2189 (2018). https://doi.org/10.1007/s00417-018-4104-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-018-4104-8