Abstract
Purpose
Our purpose was to determine the effectiveness of vitrectomy in resolving the macular retinoschisis in an eye with glaucomatous optic neuropathy and also to determine the natural course of macular retinoschisis.
Methods
This was a retrospective case series of patients who were diagnosed with macular retinoschisis and glaucomatous optic neuropathy. Fourteen eyes of 13 patients were studied. Patients with high myopia, vitreomacular traction syndrome, and the pit macular syndrome were excluded.
Results
There were three men and ten women, and 12 had unilateral and one had bilateral macular retinoschisis. Vitrectomy was performed for a serous retinal detachment, macular hole, or severe visual loss in five eyes. The mean follow-up time was 68.8 months in these five eyes, and the macular retinoschisis was resolved and the best-corrected visual acuity (BCVA) at the final visit was significantly improved in all eyes (P = 0.007). However, two of these fiv e eyes developed a macular hole and required a second vitrectomy. Of the nine eyes without treatment with a mean follow-up time of 29.0 months, the BCVA at the final visit remained unchanged from the baseline BCVA in all eyes. The macular retinoschisis was resolved or reduced in three eyes without treatment.
Conclusions
Vitrectomy was effective for the resolution of macular retinoschisis in eyes with glaucomatous optic neuropathy and serous retinal detachment or macular hole or severe reduction of the BCVA. Macular retinoschisis can be resolved without a reduction of the BCVA in some cases without treatment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Retinoschisis is a retinal disorder characterized by an abnormal splitting of the neurosensory layers of the retina, and it can be associated with optic disc pits, high myopia, optic disc hypoplasia, and vitreomacular traction [1,2,3,4,5,6,7,8].
There have also been several single case reports of a retinoschisis in glaucomatous eyes [9,10,11,12,13,14] and the retinoschisis tends to be located in the peripapillary area and cause a dissection of the circumpapillary retinal nerve fiber layer (RNFL). These findings are usually made by examining the spectral domain optical coherence tomographic (SD-OCT) images [15,16,17]. A peripapillary retinoschisis is found in 3.1% to 5.9% of patients with glaucoma [15,16,17]. These peripapillary retinoschisis generally do not need to be treated, because they do not cause visual disturbances [18].
In contrast, macular retinoschisis in patients with glaucoma can be located not only in the peripapillary area but also in the fovea. They are occasionally accompanied by serous retinal detachment (SRD), outer retinal hole, and a macular hole (MH) [9,10,11,12,13,14]. The conventional treatment of macular retinoschisis with visual disturbances is vitrectomy. One case series study demonstrated that all cases that had vitrectomy for a macular retinoschisis with glaucomatous optic neuropathy had a significant improvement in the visual acuity [9]. However, the natural course of the macular retinoschisis in eyes with glaucomatous optic neuropathy has not been definitively determined.
The aim of this study was to determine the clinical characteristics of eyes with macular retinoschisis and glaucomatous optic neuropathy and to examine the effectiveness of vitrectomy or no treatment in resolving the retinoschisis.
Methods
This was a retrospective, multicenter study. The procedures conformed to the tenets of the Declaration of Helsinki, and the procedures and study protocol were approved by the Institutional Review Board of Nara Medical University (No.1366), Tokushima University (No.2733), Tsukuba University (No.H28-207), and Sapporo City General Hospital (No.H28-053-309).
Subjects
The medical charts of 14 eyes of 13 patients with a macular retinoschisis and with glaucomatous optic neuropathy were reviewed. All of the patients had a comprehensive ophthalmologic examination including indirect ophthalmoscopy, slit-lamp biomicroscopy with and without a contact lens, spectral domain optical coherence tomography (SD-OCT; Spectralis, Heidelberg Engineering, Heidelberg, Germany; or Cirrus, Carl Zeiss Meditec Inc., Dublin, CA; or Topcon 3D OCT-1000, TOPCON Corporation, Tokyo, Japan), measurements of the IOP, and perimetry for the diagnosis of glaucoma. Of the 13 patients, nine patients had fluorescein angiography to try to determine the cause of the macular retinoschisis.
Definition of macular retinoschisis
A macular retinoschisis was defined as being present when a splitting of the retina that extended from the glaucomatous optic disc to the fovea was detected in the SD-OCT images. We excluded eyes with high myopia defined as refractive errors equal or greater than −6.0 diopters (D) or an axial length longer than 26.0 mm. Eyes with the vitreomacular traction syndrome or the pit macular syndrome as determined by SD-OCT and indirect ophthalmoscopy, were also excluded. In addition, eyes with a retinoschisis without a connection to the optic disc were excluded. The presence of an optic disc pit was confirmed by stereoscopic fundus examinations and OCT images.
Definition of glaucomatous optic neuropathy
Glaucomatous optic neuropathy was defined to be present in an eye with a vertical cup-to-disc ratio > 0.6, an asymmetrical rim-to-disc ratio < 0.2, rim notching, and the presence of retinal nerve fiber layer defects in the stereoscopic fundus examination and/or OCT. The visual field sensitivity was measured by the Humphrey field analyzer (Humphrey, Carl Zeiss Meditec, Dublin, CA) using the 30-2 Swedish interactive threshold algorithm (SITA) or a Goldmann perimeter. Eyes with unreliable visual fields that were defined as those with false negatives >33%, false positive >33%, and fixation loss >20% were also excluded.
Treatment for macular retinoschisis
Of the 14 eyes, five eyes were treated by vitrectomy alone. Nine eyes were followed without treatment because the visual acuity was not reduced or the patients declined vitrectomy. These nine eyes allowed us to determine the natural course of a retinoschisis in an eye with a glaucomatous optic disc. Only one patient (Case 7) declined vitrectomy for macular retinoschisis and was followed without treatment. All vitrectomies were performed under local retrobulbar anesthesia, and the internal limiting membrane (ILM) was peeled in all eyes, and a gas tamponade was used in four eyes. None of the eyes had fovea-sparing ILM peeling. Four of the five eyes treated with vitrectomy also underwent cataract surgery with intraocular lens implantation.
Measurements of visual acuity and retinal thickness
The best-corrected visual acuity (BCVA) was measured with a standard Japanese decimal visual acuity chart. The decimal BCVA was converted to the logarithm of the minimum angle of resolution (logMAR) units for the statistical analyses. An improvement or worsening of the BCVA was defined as a change of ±0.3 logMAR units or more from the baseline BCVA. A significant improvement or worsening of the foveal thickness was defined as a change of ±25% in the SD-OCT images from the initial value.
Statistical analyses
The significance of the changes in the visual acuity was determined by paired t tests. A P value <0.05 was accepted as significant.
Results
Of the 13 macular retinoschisis patients with glaucomatous optic neuropathy, 12 had unilateral retinoschisis and one had bilateral retinoschisis. There were three men and ten women, and the mean ± standard deviation (SD) age of the patients was 63.6 ± 12.3 years. The mean ± SD BCVA at the initial visit was 0.33 ± 0.51 logMAR units, and the mean ± SD refractive error (spherical equivalent) was −0.9 ± 1.6 diopters (D) with a range of −3.0 to +2.0 D. The mean ± SD axial length was 24.5 ± 1.1 with a range of 22.5 to 25.8 mm in ten eyes; the axial length was not measured in the other four phakic eyes with refractive errors ranging from −3.0 to 0 D. The mean ± SD IOP was 14.9 ± 3.1 mmHg. None of the eyes had an acute elevation of the IOP. In addition, none of the eyes required filtration surgery for uncontrolled glaucoma during the follow-up period.
All of the 14 eyes were followed for more than 6 months. The mean ± SD follow-up time of the all eyes, five eyes with vitrectomy, and nine eyes without treatment was 43.2 ± 40.0, 68.8 ± 48.23, and 29.0 ± 25.2 months, respectively. Of the five eyes that had vitrectomy for a SRD, MH, or severe visual loss, two eyes required a second surgery because of the formation of a full thickness MH or failure to close the MH (Cases 2 and 5). The MH in these two eyes was closed after the second vitrectomy with gas tamponade. The final BCVA was significantly improved compared to that of before the surgery in all vitrectomized eyes (P = 0.007), and the SD-OCT images showed a resolution of the retinoschisis and SRD (Cases 1-5).
In the nine untreated eyes, the final BCVA was not significantly different from that at the initial examination. Seven of the untreated eyes were followed for more than 12 months, and the macular retinoschisis was resolved or reduced in three eyes without treatment (Tables 1 and 2).
Representative cases
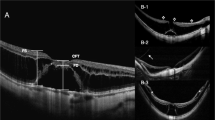
Case 2. Case 2 was a 65-year-old-woman who had macular retinoschisis with an outer retinal hole, SRD, and glaucomatous optic neuropathy in the right eye (Fig. 1a and b). Her BCVA at the initial visit was 20/200. Fundus photographs showed a defect in the retinal nerve fiber layer (RNFL) at the inferior temporal quadrant of the optic disc (Fig. 1a). The patient underwent vitrectomy with ILM peeling. Ten days after the vitrectomy, the macular retinoschisis with outer retinal hole remained unchanged (Fig. 1c and d). One month after the vitrectomy, the fundus photographs and SD-OCT images showed a MH (Figs. 1e and f). After a second vitrectomy with gas tamponade, the MH was closed and her BCVA improved to 20/67 (Figs. 1g and h). Perimetry showed a decrease in sensitivity extending from the nasal to center area (Fig. 1i, j, and k).
Case 2. Fundus photographs and optical coherence tomographic (OCT) images of a patient with macular retinoschisis and glaucomatous optic neuropathy. a and b. Preoperative fundus photographs and horizontal OCT images of the right eye at the initial visit showing a retinal nerve fiber layer (RNFL) defect (black arrowheads) at the lower temporal sector of the optic disc. An outer retinal hole is present at the fovea, and retinoschisis of the outer plexiform layer connected to the optic disc and the fovea can be seen. The scanned OCT line shown in Fig. 1b is shown as a black line. c. and d. Post-vitrectomy images after 10 days showing that the macular retinoschisis and outer retinal hole remained unchanged, and the RNFL defect (black arrowheads) has expanded. e. and f. Post-vitrectomy images after 1 month showing that the eye has developed a macular hole and the retinal thickness is reduced. g. and h. OCT image showing a closed macular hole and resolution of the macular retinoschisis at the final visit. i., j., and k. Post-vitrectomy visual field (gray scale, total deviation, and pattern deviation) showing decreased threshold sensitivity consistent with the RNFL defect
Case 6. Case 6 was a 50-year-old woman with glaucomatous optic neuropathy and macular retinoschisis that divided the retina into two layers (Fig. 2a to c). Nevertheless, her BCVA at the initial visit was 20/17 and she had no complaints. She was closely followed without treatment for the macular retinoschisis. After 4 years, the macular retinoschisis was markedly reduced (Fig. 2d), and after 5 years, the macular retinoschisis was completely resolved and no recurrences have occurred (Fig. 2e). Perimetry showed decreased sensitivity at superior nasal quadrant (Fig. 2f to k).
Case 6. Fundus photograph and optical coherence tomographic (OCT) images of a patient with macular retinoschisis and glaucomatous optic neuropathy. a. Fundus photograph showing retinal nerve fiber layer (RNFL) defect (black arrowheads) at the inferior temporal sector of the optic disc. The scanned OCT direction shown in Fig. 2c as a black line. b. Retinal thickness map showing a thickened retina between the optic disc and fovea. c. Horizontal OCT image shows retinoschisis in the outer plexiform layer and inner nuclear layer connecting the optic disc to the fovea at the initial examination. d. Retinoschisis of the inner nuclear layer is completely resolved after 4 years from initial visit. The retinal thickness has decreased. e. OCT image at the final examination shows a complete resolution of the macular retinoschisis. f., g., and h Visual field (gray scale, total deviation, and pattern deviation) at the initial examination indicates a decrease in the threshold sensitivity consistent with RNFL defect
Case 7. Case 7 was a 77-year-old woman with macular retinoschisis, SRD, an outer retinal hole, and glaucomatous optic neuropathy in the right eye (Fig. 3a and b). Her BCVA at the initial visit was 20/200. Fluorescein angiography (FA) showed a pooling of dye in the inferior nasal quadrant of the right optic disc, and SD-OCT showed a dilated subarachnoid space consistent with the fluorescein pooling (Fig. 3c to g). The patient declined vitrectomy and was followed without treatment. Twelve months after the initial visit, SD-OCT revealed that the retinoschisis and retinal thickness had decreased (Fig. 3h). However, her BCVA had remained unchanged from the initial visit.
Case 7. Fundus photograph, optical coherence tomographic (OCT) images, and fluorescein angiograms (FA) of patient with macular retinoschisis and glaucomatous optic neuropathy. a. Fundus photograph shows outer retinal hole and retinal nerve fiber layer (RNFL) defect at the lower sector of the optic disc. The scanned OCT direction in Fig. 3b is shown as a black line. b. Horizontal OCT image shows an outer retinal hole and retinoschisis of the outer plexiform layer, inner nuclear layer, and retinal nerve fiber layer connecting the optic disc to the fovea. c. (early phase) and d. (late phase) fluorescein angiograms. FA shows pooling at the lower temporal margin of the optic disc. e. The scanned OCT line and expanded subarachnoid space in Fig. 3 g (upper side) and f. (lower side) are shown as a green line and yellow arrowheads, respectively. f and g. There is a communication between the expanded retrobulbar subarachnoid space (yellow arrowheads) corresponding to the pooling of fluorescein and retinoschisis. h. Retinoschisis and outer retinal hole has decreased 15 months after the initial visit
Discussion
The presence of a micro hole in the RNFL can cause leakage, and/or vitreous traction on a defective RNFL around the optic disc can also cause leakage of vitreous fluids into the retina [11, 14, 19]. We did not find any optic disc pits, micro holes, and vitreous traction around the RNFL defect and optic disc. However, the degree of macular retinoschisis was reduced after the vitrectomy. Thus, it is possible that the vitrectomy may have closed undetected micro holes and/or released the vitreous traction on the retina.
We suggest other possible causes for the macular retinoschisis in our cases. The compromised optic disc in eyes with glaucoma may lead to a leakage of fluid from the subarachnoid space into the retina. Krivoy et al. described the OCT findings of ten eyes with congenital optic disc pits [20]. They suggested that the optic disc pit acted as a conduit for fluid to flow into the retina causing the retinoschisis or subretinal detachment from the subarachnoid space [20]. Katome et al. showed swept-source OCT images and identified connections between the vitreous cavity and the retrobulbar subarachnoid space in patients with an optic disc pit [21]. Our FA showed pooling of the fluorescein consistent with an expanded subarachnoid space at the optic disc margin detected by OCT (Case 7). These findings suggested that the spaces in the macular retinoschisis might be partially filled with cerebrospinal fluid.
The study of macular retinoschisis in eyes with glaucomatous optic neuropathy reported by Inoue et al. demonstrated that macular retinoschisis can be resolved or reduced by vitrectomy [9]. In cases of optic disc pit maculopathy, some authors have reported that a complete resolution of the foveal fluid was achieved in 88% to 94% after the vitrectomy [22,23,24]. These findings indicate that vitrectomy for a macular retinoschisis is effective. However, Inoue et al. described four eyes (36%) treated with vitrectomy that developed a MH or a MH retinal detachment [9]. In our patients, two eyes (40%) required a second surgery because of the development of a MH.
There have been two case reports on the natural course of macular retinoschisis in eyes with glaucoma [11, 14]. Because the follow-up periods were short in these case reports, it is unclear whether macular retinoschisis in eyes without treatment can be resolved or not. In our cases, three of nine eyes without treatment had a reduction of the foveal thickness with a mean follow-up time of 29.0 months. In Case 6, the macular retinoschisis had completely resolved despite the lack of treatment. We have also reported a case of macular retinoschisis with optic disc hypoplasia whose visual acuity and symptoms did not change significantly after a 17 year follow-up period without treatment [5]. Thus macular retinoschisis may also be resolved spontaneously in some of the eyes.
There are some limitations in this study. The number of patients was small, and a larger number of patients must be examined. However, the prevalence of macular retinoschisis with glaucomatous optic neuropathy is very rare. A second limitation was the retrospective nature of this study, and important information was missing in some of the medical charts. Thus, we were not able to determine whether a posterior vitreous detachment was present in some of the patients because the medical files did not include this information. The third limitation was the retrospective study design. Thus, there were differences in the BCVA at the initial visit or pre-operation among nine eyes without treatment and five eyes with vitrectomy. The untreated eight eyes, excluding Case 7 who declined vitrectomy for macular retinoschisis, had better BCVA than that of the eyes with vitrectomy at the initial visit or preoperatively.
In conclusion, vitrectomy for macular retinoschisis in eyes with glaucomatous optic neuropathy was effective. Macular retinoschisis can be spontaneously resolved in some cases without treatment. Thus, results of this study suggest that macular retinoschisis with glaucomatous optic neuropathy can be followed closely without therapy unless a MH or a SRD develops or a severe reduction of the BCVA occurs.
References
Sobol WM, Blodi CF, Folk JC et al (1990) Long-term visual outcome in patients with optic nerve pit and serous retinal detachment of the macula. Ophthalmology 97:1539–1542
Takano M, Kishi S (1999) Foveal retinoschisis and retinal detachment in severely myopic eyes with posterior staphyloma. Am J Ophthalmol 128:472–476
Gaucher D, Haouchine B, Tadayoni R et al (2007) Long-term follow-up of high myopic foveoschisis: natural course and surgical outcome. Am J Ophthalmol 143:455–462
Fujimoto M, Hangai M, Suda K et al (2010) Features associated with foveal retinal detachment in myopic macular retinoschisis. Am J Ophthalmol 150:863–870
Yoshikawa T, Nishimura T, Minamino K et al (2013) A long-term follow-up of peripapillary retinoschisis with optic disc hypoplasia. Int Ophthalmol 33:425–428
Hotta K, Hotta J (2004) Retinoschisis with macular retinal detachment associated with vitreomacular traction syndrome. Retina 24:307–309
Yamada N, Kishi S (2005) Tomographic features and surgical outcomes of vitreomacular traction syndrome. Am J Ophthalmol 139:112–117
Duker JS, Kaiser PK, Binder S et al (2013) The international Vitreomacular traction study group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology 120:2611–2619
Inoue M, Itoh Y, Rii T et al (2015) Macular retinoschisis associated with glaucomatous optic neuropathy in eyes with normal intraocular pressure. Graefes Arch Clin Exp Ophthalmol 253:1447–1456
Takashina S, Saito W, Noda K et al (2013) Membrane tissue on the optic disc may cause macular schisis associated with a glaucomatous optic disc without optic disc pits. Clin Ophthalmol 7:883–887
Zhao M, Li X (2011) Macular retinoschisis associated with normal tension glaucoma. Graefes Arch Clin Exp Ophthalmol 249:1255–1258
Farjad H, Besada E, Frauens BJ (2010) Peripapillary schisis with serous detachment in advanced glaucoma. Optom Vis Sci 87:205–217
Mavrikakis E, Lam WC (2011) Macular schisis and detachment secondary to large optic nerve head cup: a newly recognized syndrome amenable to vitrectomy. Acta Ophthalmol 89:95–96
Hollander DA, Barricks ME, Duncan JL et al (2005) Macular schisis detachment associated with angle-closure glaucoma. Arch Ophthalmol 123:270–272
Lee EJ, Kim TW, Kim M et al (2014) Peripapillary retinoschisis in glaucomatous eyes. PLoS One 9:e90129
Bayraktar S, Cebeci Z, Kabaalioglu M et al (2016) Peripapillary Retinoschisis in glaucoma patients. J Ophthalmol 2016:1612720
van der Schoot J, Vermeer KA, Lemij HG (2017) Transient Peripapillary Retinoschisis in glaucomatous eyes. J Ophthalmol 2017:1536030
Hwang YH, Kim YY, Kim HK et al (2014) Effect of peripapillary retinoschisis on retinal nerve fibre layer thickness measurement in glaucomatous eyes. Br J Ophthalmol 98:669–674
Zumbro DS, Jampol LM, Folk JC et al (2007) Macular schisis and detachment associated with presumed acquired enlarged optic nerve head cups. Am J Ophthalmol 144:70–74
Krivoy D, Gentile R, Liebmann JM et al (1996) Imaging congenital optic disc pits and associated maculopathy using optical coherence tomography. Arch Ophthalmol 114:165–170
Katome T, Mitamura Y, Hotta F et al (2013) Swept-source optical coherence tomography identifies connection between vitreous cavity and retrobulbar subarachnoid space in patient with optic disc pit. Eye 27:1325–1326
Taiel-Sartral M, Mimoun G, Glacet-Bernard A et al (1996) Vitrectomy-laser-gas for treating optic disk pits complicated by serous macular detachment. J Fr Ophtalmol 19:603–609
García-Arumí J, Guraya BC, Espax AB et al (2004) Optical coherence tomography in optic pit maculopathy managed with vitrectomy-laser-gas. Graefes Arch Clin Exp Ophthalmol 242:819–826
Rayat JS, Rudnisky CJ, Waite C et al (2015) Long-term outcomes for optic disc pit maculopathy after vitrectomy. Retina 35:2011–2017
Acknowledgments
The authors thank Professor Yoshinori Mitamura, Dr. Yoshifumi Okamoto, and Dr. Eiichi Yukawa for helpful advice and data collection, and Professor Emeritus Duco Hamasaki of the Bascom Palmer Eye Institute for discussions and manuscript revision. All members became a part of Japan Clinical Retina Study (J-CREST) group and researched.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Yoshikawa, T., Yamanaka, C., Kinoshita, T. et al. Macular retinoschisis in eyes with glaucomatous optic neuropathy: Vitrectomy and natural course. Graefes Arch Clin Exp Ophthalmol 256, 281–288 (2018). https://doi.org/10.1007/s00417-017-3855-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-017-3855-y