Abstract
Purpose
To evaluate the feasibility, safety, and biocompatibility of intravitreal injection of human mesenchymal stem cells (MSCs) in immunocompetent pigmented rabbits.
Materials and methods
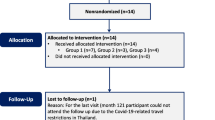
Thirty-two pigmented rabbits (24 females, 8 males; Chinchilla-New Zealand White) were divided into 8 groups of 4 animals. Commercially prepared human MSCs were injected (0.05 ml) into the post-lens vitreous of the right eyes. Groups 1 and 4 received isotonic medium (Ringer lactate-based), groups 2, 5, 7, and 8 received a low dose of 15 × 106 cells/ml. Groups 3 and 6 received a high dose of 30 × 106 cells/ml. Clinical signs were evaluated and scored before MSCs injection and weekly for 2 or 6 weeks. Animals were sacrificed at 2 or 6 weeks after injection. Eyes, liver, spleen, and gonads were assessed by histology and by fluorescent in situ hybridization to evaluate survival and extraocular migration of MSCs.
Results
There were no relevant clinical findings between control and MSC-injected rabbit eyes at any time point. There were also no relevant histological findings between control and MSC-injected rabbits related to ocular, liver, spleen, or gonad tissues modifications. MSCs survived intravitreally for at least 2 weeks after injection. Extraocular migration of MSCs was not detected.
Conclusions
MSCs are safe and well-tolerated when administered intravitreally at a dose of 15 × 106 cells/ml in pigmented rabbits. These findings enable future research to explore the intravitreal use of commercially prepared allogenic human MSCs in clinical trials of retinal diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neurodegenerative diseases of the retina and optic nerve affect approximately 40 million people worldwide [1]. Non-arteritic ischemic optic neuropathy (NAION) constitutes the most prevalent ischemic optic neuropathy and produces irreversible unilateral visual loss in people over 50 years of age [2]. This disease is caused by an infarct of the optic nerve head (ONH) and is clinically characterized by sudden and painless loss of vision in one eye, with visual field defects, dyschromatopsia, and optic disc swelling followed by optic nerve atrophy at 6–8 weeks [3]. Fellow eye involvement is described in 15–25% of patients at 5 years, and no effective treatments are currently available. Various medical approaches have been used such as acetylsalicylic acid [4, 5], optic nerve decompression surgery [6], corticosteroids [7], levodopa [8], diphenylhydantoin, estrogens [9], erythropoietin [10], brimonidine [11], and ranibizumab [12]. None of them have proven to be effective in enhancing visual function of patients with NAION, and there is no therapy for prevention of fellow eye involvement. One option that has not been fully explored is cell-based therapy, which could provide an all-encompassing approach to treat NAION [13].
Mesenchymal stem cells (MSCs) are multipotent and self-renewing cells that are derived from bone marrow, adipose tissue, umbilical cord, placenta, and other mesenchymal tissues. They can be induced to differentiate into bone marrow, cartilage, muscle, lipid, myocardial, glial cells, and neurons [14, 15]. MSCs therapy includes the ability to replace lost cells [16] and, furthermore, provide neurotrophic factors with paracrine actions to the damaged area. These factors can modulate the microenvironment of diseased tissues, promote cell survival, and activate endogenous repair mechanisms [17]. MSCs have some features that make them interesting for cell therapy application. They are easy to isolate and expand rapidly after a short period of dormancy [18]. They are free of ethical issues associated with the harvesting of embryonic stem cells [19]. Also, MSCs are considered to be “immunoprivileged” because they do not express on their surfaces major histocompatibility complex class II antigens, which are associated with transplant rejection [20]. This advantage allows the use of either autologous or allogenic MSCs [21].
There are two major options for the clinical application of MSCs in retinal and optic nerve diseases: cell replacement and neuroprotection via paracrine effects. However, cell replacement remains untenable, as the required massive differentiation of MSCs into functional retina cells is not currently feasible. On the other hand, neuroprotective use to rescue degenerating optic nerve and retinal cells is already available by autologous transplantation [18]. Cytokines and growth factors secreted by MSCs have trophic, immunomodulatory, anti-apoptotic, and proangiogenic properties [22]. According to this approach, MSCs effectiveness may result from the production of factors that promote endogenous neuronal growth and angiogenesis, encourage synaptic connection and remyelination of damaged axons, decrease apoptosis, and regulate ion of inflammation [22]. MSCs express a variety of neurotrophic factors, such as brain-derived neurotrophic factor (BDNF), ciliary neurotrophic factor (CNTF), glial-derived growth factor (GDGF), insulin-like growth factor 1 (IGF1), nerve growth factor (NGF), and basic fibroblast growth factor (bFGF), among others, that have proven effectiveness in the protection of injured retinas and optic nerves [23, 24]. Recent experimental studies in mice were conducted to evaluate MSCs usefulness for treating retinal diseases [25, 26]. However, the mouse vitreous volume is very small compared to the human [27], and extrapolation of dose-efficacy data is complicated between those species. In the current study, we evaluated the feasibility, safety, and potential extraocular migration of human allogenic bone-marrow MSCs after intravitreal injection in immunocompetent pigmented rabbits. Successful outcomes regarding these three parameters are a prerequisite for attempting to introduce intravitreal cell therapy into clinical practice.
Materials and methods
Cells
Bone-marrow MSCs from adult human donors, cryopreserved and reexpanded ex vivo, were provided under the trade name MSV® by Citospin S.L. (Valladolid, Spain). These cells have been approved by the Spanish Drug Agency (AEMPS) for autologous and allogenic use in several clinical trials of traumatology, ophthalmology, and cardiology (Eudra-CT 2005–005498-36, 2008–001191-68, 2009–0170450-11, 2010–023535-43, and 2011–005321-51). The company operates under Good Manufacturing Practice (GMP) regulations and holds a protocol registered as PEI 15–007 by the AEMPS. The cells were provided in syringes (1 ml, Luerlook; Becton Dickinson, Huesca, Spain) pre-filled with either 15 × 106 cells/ml or 30 × 106 cells/ml, in a volume of 0.1 ml of isotonic medium. This medium is composed of Ringer lactate (B. Braun, Barcelona, Spain) supplemented with 0.1% human albumin (CSL Behring S.A., Barcelona, Spain) and 5 mM glucose (B. Braun).
Experimental animals
The use of animals in this study was in accordance with the recommendations of the Association for Research in Vision and Ophthalmology (ARVO) for the Use of Animals in Ophthalmic and Vision Research. This study was approved by the Animal Research and Welfare Ethics Committee of the University of Valladolid (Spain) in agreement with European (Council Directive 2010/63/UE) and Spanish regulations (RD 53/2013). Female (n = 24) and male (n = 8) pigmented rabbits between 3 and 4 kg and 26- to 30-week-old Chinchilla-New Zealand White (Granja Riera, Barcelona, Spain) were included in the study. The animals were not immunosuppressed and showed normal findings upon complete ophthalmic examination and systemic evaluation before starting the study. To determine the best tolerated dose, the female rabbits were randomly divided into groups 1, 2, and 3, with 42 days of follow-up, and groups 4, 5, and 6, with 14 days of follow-up. Groups 1 and 4 were controls and received an intravitreal injection of isotonic medium. Groups 2 and 5 received an intravitreal dose of 15 × 106 cells/ml (low dose). Groups 3 and 6 received an intravitreal dose of 30 × 106 cells/ml (high dose). In all cases, the injected volume was 0.05 ml. The male rabbits were randomly divided into groups 7 and 8, with 42 and 14 days of follow-up, respectively, and received only the dose best tolerated by the female rabbits. Weight assessment during the follow-up was taken as a general marker of animal welfare.
Intravitreal injection technique
In a single-blind experimental study, intravitreal injections were carried out by a trained ophthalmologist (SLV) under a surgical microscope (Leica M844, Leica Microsystems, Wetzlar, Germany). The injection of control or MSV® media was performed on the right eye of each rabbit. The animals were anesthetized by an intramuscular injection of ketamine (30 mg/kg; Imalgene 1000, Merial, Lyon, France) and xylacine (6 mg/kg; Rompún 2%, Bayer HealthCare, Kiel, Germany). Pinna and pedal reflexes were used to monitor the level of anesthesia. Prophylactic antibiotic treatment was established with bencilpenicillin procaine/benzathine (7 IU/kg; Shotapen LA, VIRBAC, Carros, France). Analgesia was applied by subcutaneous injection of butorphanol (0.1 mg/kg; Torbugesic® Vet, Fort Dodge Animal Health, Fort Dodge, IA, USA). The periorbital area was cleansed by a solution of povidone iodine (5% Betadine®; Meda Manufacturing, Bordeaux, France). Topical anesthesia (Colircusí Anestésico Doble®; Alcon Cusí SA, Barcelona, Spain) was applied on the right eye prior to the intravitreal injection.
An eyelid speculum was placed to retract the eyelids, and eye proptosis was mechanically induced prior to injection. Intravitreal injections were performed with a 25-gauge needle at 4 mm from the corneoscleral limbus in the temporal upper quadrant of the sclera. Injections were carried out at an adequate angle and depth to avoid touching the lens or damaging the retina. The content of the injection was introduced slowly, without changing the position of the needle inside the eye. Before removing the needle, the conjunctiva and sclera were pinched with a tying forceps for 1 min to minimize backflow. Finally, ophthalmic tobramycin ointment (Tobrex® ungüento; Alcon Cusí SA) was applied.
Clinical evaluation
Clinical evaluations were performed by a trained ophthalmologist (SDL) and a veterinarian (MLA). Clinical evaluations were performed before and after intravitreal injection (day 0) and on days 1, 7, 14, 21, 28, 35, and 42 after the procedure. Complete ophthalmic examinations of the animals were performed. The anterior pole was evaluated by slit-lamp biomicroscopy (Kowa SL-15; Kowa Optimed, Inc., Torrance, CA, USA). The posterior pole was evaluated by inverted ophthalmoscopy using a non-contact lens (Volk Optical, Inc., Mentor, OH, USA) after pharmacological mydriasis (Tropicamida Colirio; Alcon Cusí SA). Intraocular pressure (IOP) was measured by applanation tonometry (Tonopen®, Reichert, Inc., Depew, NY, USA). Clinical findings of the conjunctiva, cornea, anterior chamber, lens, vitreous cavity, retina, and optic nerve were graded and scored by a modification of the Hackett-McDonald method [28]. The severity of these clinical signs was identified and graded as none (0), mild (1), moderate (2), or severe (3) on each day of examination.
Histological evaluation
Endpoint observations were performed at days 14 (groups 4, 5, 6, and 8) and 42 (groups 1, 2, 3, and 7) after intravitreal injection. Rabbits were anesthetized as previously described and the euthanasia was performed with an intravenous injection of sodium pentobarbital (200 mg/kg; Dolethal®, Vetoquinol, Cedex, France). The entire right ocular globe of each rabbit was enucleated. One untreated left eye per experimental group was also enucleated as a further control. A 5–0 polyglactin suture was placed at the central superior sclera to facilitate sample orientation during tissue processing. Also, a necropsy of each animal was performed and liver, spleen, and gonads (ovaries or testicles) were extracted for histological analysis.
Each tissue sample was fixed at least 12 h in 10% formalin. The tissues were processed in an automatic tissue processor (Leica ASP300; Leica Microsystems, Wetzlar, Germany). Paraffin blocks from each organ were prepared and then cut in the sagittal plane at several levels, obtaining multiple 3-μm-thick microscope sections. Hematoxylin and eosin (Merck KGaA, Darmstadt, Germany)-stained slides were examined by standard light microscopy. The ocular target tissues were cornea, iridocorneal angle, retina, and optic nerve.
Immunochemical evaluation
Fluorescence in situ hybridization (FISH) was performed in samples of the targeted tissues to detect and localize the presence or absence of specific DNA sequences on chromosomes [29]. In this context, specific probes (Vysis CEP X SpectrumOrange/Y SpectrumGreen Direct Labeled Fluorescent DNA Probe Kit, Abbott Molecular, Inc., Lake Forrest, IL, USA) were used to detect human DNA and thus determine the presence or absence of MSV® cells in the evaluated rabbit tissues. Human liver samples were processed in parallel as positive controls.
Statistical analysis
All data were collected in a database created in Excel (Microsoft Office Excel 2013, Microsoft Corporation, Redmond, WA, USA) and subsequently analyzed using SPSS (version 24.0, SPSS, Inc., Chicago, IL, USA). The statistical significance level was set at 5% (p < 0.05). Data were expressed as mean ± standard deviation (SD). Due to similarities in female and male responses to each treatment protocol, when possible, female and male rabbit data were combined for statistical analysis. Body weights were compared with the Student’s t test for paired samples. Means of IOP of the left, untreated eyes were taken as normal values. Analysis of IOPs at follow-up times was performed by repeated measures analysis of variance (ANOVA) with Bonferroni correction for multiple testing. Qualitative variables were expressed in percentages of frequency (%).
Results
Animals
Two animals from the control group 4 died before the intravitreal injection. Those animals were not replaced because similar age/weight rabbits were not available at the study start point. For the control groups, the final body weights were 3.48 ± 0.71 kg and 3.87 ± 0.58 kg at days 14 and 42, respectively. For rabbits receiving the low dose of MSV®, the weights were 3.34 ± 0.64 kg and 3.53 ± 0.71 kg on days 14 and 42, respectively. For rabbits receiving the high dose of MSV®, the weights were 3.58 ± 0.34 kg and 3.93 ± 0.65 kg on days 14 and 42, respectively. For each group, the increase in body weight at days 14 and 42 was significant compared to the weight at day 0 (p < 0.05 for each comparison).
Clinical results
Clinical findings of the anterior pole
There was mild or moderate conjunctival congestion in ≤33% of each group on days 1, 7, and 21 after the intravitreal injection (Table 1A). There was neither conjunctival swelling nor conjunctival discharge in any group during the follow-up. Only 12.5% of the low-dose group had a mild loss of transparency of the cornea at day 21. No Tyndall effect was present in any group during the follow up. Between days 14–21, 6.0–12.5% of the low-dose group and 12.5–50.0% of the high-dose group had mild to moderate injection of the iridial vessels (Table 1B). In the control group, <25% of the eyes had mild opacities in the posterior capsule of the lens, which did not change during the follow-up period (Table 1C). The lens of eyes receiving the low dose of MSV appeared normal on days 1 and 7, but mild pseudo-opacities (Fig. 1A) were evident on days 14 (18.75%), 21 (37.5%), 28 (50%), 35 (37.5%), and 42 (12.5%). For eyes receiving the high dose, mild pseudo-opacities were observed in the posterior lens capsule on days 7 (25%), 14 (63%), 21 (50%), 28 (25%), 35 (75%), and 42 (75%). The position of these pseudo-opacities changed during the follow-up period. Upon closer histological examination (Fig. 1B), the apparent lens pseudo-opacities could be attributed to the presence of accumulated cells in the vitreous immediately behind the lens.
Anterior pole image and histology of an eye intravitreally injected with 15 × 106 MSV cells/ml. A. Apparent opacity (pseudo-opacity) in the posterior capsule of the lens (white arrow). B. Histological examination of the posterior lens and adjacent vitreous of the same eye revealed the presence of accumulated cells in the vitreous (black arrow). There was no apparent rupture of the lens capsule (*)
Clinical findings of the posterior pole
The vitreous was normal in all groups, and there were some localized opacities near the optic nerve, corresponding with the cells injected in the low- and high-dose groups. The retina had a normal appearance in all groups, with no retinal detachment, retinal hemorrhage, or vascular congestion. The optic nerve in all three groups was normal during the follow-up period, and there was no evidence of ischemia or inflammation of the ONH.
Intraocular pressure
The IOP of the left, untreated eyes on day 0 was 9.17 ± 1.42 mmHg (range: 6.0–12.0 mmHg), and there were no significant changes during the follow-up period. IOP increased in all groups within minutes after the intravitreal injection (p < 0.05, Fig. 2). On day 1, the IOP for the control and low-dose group had returned to pre-injection values, while that for the high-dose group remained slightly, but not significantly, elevated. By day 14, the IOP of all groups was at the pre-injection level.
Pre- and post-intravitreal injection intraocular pressure (IOP). Immediately after the intravitreal injection (IV) of all groups, the IOP was significantly elevated compared to the pre-IV IOP (*, p < 0.05, ANOVA with repeated measures and Bonferroni correction for multiple testing). By post-IV day 1 and thereafter, the IOPs were not significantly different from the pre-IV values. Means and standard deviation intervals of IOP for the control group (IV of saline solution), low-dose group (IV of 15 × 106 cells/ml), and high-dose group (IV of 30 × 106 cells/ml) by time point
Histological evaluation
There were no relevant histological findings in the ocular tissues of any group at days 14 and 42 (Fig. 3). The corneal epithelium, stroma, and endothelium were normal. The iridocorneal angle was open and without synechia. The retinal layers were intact and had no pyknotic nuclei, and there was no disruption of the ONH formed by axons of the retinal ganglion cell layer. There were also no histological modifications of liver, spleen, or gonads, and there was no evidence of abnormal cell growth in any group (data not shown).
Histologic images of the cornea, iridocorneal (IC) angle, retina, and optic nerve head 6 weeks after intravitreal injection. For each group, the corneal epithelium, stroma, and endothelium were normal, the iridocorneal IC angle was open, and there were no iridial synechiae. All the retinal layers were intact and without pyknotic nuclei. The separation of the photoreceptors from the retinal pigmented epithelium routinely occurs during the processing of eyes for histology. The optic nerve head, formed by axons of the retinal ganglion cell layer, was normal in appearance. There was no abnormal or disorganized growth of cells into the ocular globe. Control = vehicle injected; low dose = 15 × 106 cells/ml; high dose = 30 × 106 cells/ml; hematoxylin and eosin staining
FISH evaluation
Analysis of the ocular tissues by FISH showed that on day 14, MSV® cells injected in both low and high doses were present only in the vitreous cavity, near the posterior capsule of the lens, and the inner limiting membrane of the retina (Fig. 4). MSV® cells were not detected inside other ocular tissues. At the same time, MSV® cells were not detected in the spleen, liver, or gonads. At day 42, MSV® cells were not detected in any of the ocular or extraocular tissues evaluated.
Intraocular distribution of MSV® cells. A. MSV® cells injected in the low-dose group were detected by fluorescent in situ hybridization (FISH) technique in the vitreous cavity adjacent to the peripheral retina at day 14. B. MSV® cells in the vitreous cavity. C. MSV® cells adjacent to the retina. Yellow arrow, MSV® cells; red, human chromosome X; green, human chromosome Y; blue, cell nuclei (DAPI); GCL, ganglion cell layer; INL, inner nuclear layer; IPL, inner plexiform layer
Discussion
Some retinal diseases, such as NAION, affect a great number of people worldwide and produce irreversible visual loss. Currently, there is neither treatment for the affected eye nor prophylaxis for the fellow eye. Cellular therapy has the potential to expand the therapeutic options for retinal neuroprotection needed for NAION and other retinal diseases. The purpose of this study was to evaluate the safety and biocompatibility of MSCs injected into the vitreous cavity of healthy, immunocompetent pigmented rabbits. We found that MSCs, in the form of the MSV® cells used in this study, were safe and biocompatible with the rabbit tissues. These findings enable future studies to now explore their use in human clinical trials. Currently, MSV® cells are approved for allogenic and autologous clinical use by the AEMPS (PEI n°15–007) in the areas of traumatology, ophthalmology, and cardiology [21, 30].
Preclinical studies of intraocular MSC injection have been conducted in mice, but to our knowledge this is the first study in rabbits. The vitreous volume of the mouse eye (5 μL) is only 0.1% of that in human eyes [27]. Studies in small eyes require the use of small injection volumes. This is a critical parameter because the size of cells to be injected is the same regardless of the size of the recipient eye. Thus, it is risky to infer that the results obtained by MSCs injection into very small eyes will produce similar results in human eyes. Therefore, in the present study, we used immunocompetent pigmented rabbits that have a vitreous volume of 1.15 ml [31], which is more similar to that of humans (with a vitreous volume of 4 ml) [31]. The larger rabbit eye, compared to mice, allows the administration of a larger intravitreal injection (50 μL) and therefore a greater number of cells. Furthermore, there is currently no good model of NAION, even though several models are described in the literature [32], and the primate model is very difficult to use due to ethical issues.
Based upon the more rapid stabilization of IOP after the injection and the lower frequencies of clinical changes and aggregations of cells in the vitreous cavity, we concluded that for the female rabbits, the low dose of 15 × 106 cells/ml was better tolerated than the high dose (30 × 106 cells/ml). For that reason, the male rabbits (groups 7 and 8) received only the low dose to confirm that as a “best tolerated dose” and to corroborate absence of extraocular MSCs migration with similar tolerance observed in female rabbits. We did not designate and use a separate control group of male rabbits following the guiding principles known as “The three Rs” (replace, reduce, and refine) [33], underpinning the humane use of animals in scientific research.
The administration of MSCs for retinal diseases in animal models has utilized three main routes: intravitreal injection, sub-retinal injection, or intravenous systemic administration [18]. We used only intravitreal injection because this route seems to be less damaging to the eye than sub-retinal injection [18]. Intravitreal injections deliver a larger volume and therefore more cells than can be delivered by the sub-retinal route, and the cells are closer to the retina and ONH than when delivered intravenously. Also, intravitreal injection is more suitable for research on the neurotrophic properties of MSCs because neurotrophins secreted from MSCs can penetrate into the retina through the inner limiting membrane, while the MSCs themselves cannot [18].
There is no specific formula to calculate the number of cells that should be injected to achieve a specific result such as minimal side effects and/or optimal beneficial effects. Thus, the cellular dose used in the present study was based on preclinical and clinical studies accessed through PubMed (accessed January 2016) [25, 26, 34, 35]. In murine models of retinal diseases, the cell doses ranged between 4 × 108 and 180 × 108 cells/ml [25, 26], while the cell doses used in clinical trials of several retinal and optic nerve diseases ranged between 10 × 107 and 36 × 107 cells/ml [34, 35]. Some studies used higher concentrations comprised of different types of mononuclear cells from bone marrow, while we specifically used MSCs produced as MSV® cells, which are larger in size than other cell types found in bone marrow. The large size of MSCs make it difficult to employ higher doses of the MSV® cells for intravitreal injection in rabbits. Thus, we decided to use a low dose (15 × 106 cells/ml) and a high dose (30 × 106 cells/ml) after taking into consideration the higher number of cells per volume to be injected and simultaneously trying to avoid cell damage by agglutination or crowding when the cells passed through the 25-gauge needle.
The clinical results, such as the significant increase in animal weight for each group and the absence of signs of systemic disease, confirm the absence of major untoward effects in the rabbits. In the anterior pole, mild opacities appeared to be present in the posterior lens capsule or near it in the anterior vitreous. In the control group that received isotonic medium injections without MSV® cells, the opacities were localized within the lens itself and did not change position during the follow-up period. For eyes receiving MSV® cell injections, the opacities were not actually localized within the lens; therefore, we used the term “pseudo-opacities” to describe apparent association with the posterior lens capsule. These pseudo-opacities appeared to change position during the follow-up period and occurred more often in the high-dose group. We speculate that the pseudo-opacities developed because of the placement of the needle tip just posterior to the bulky lens and the accumulation of injected cells in that location. This is consistent with our histological evaluation showing that each lens was normal in appearance with an intact posterior capsule. To assess if injected cells interfere with vision, future studies will include assessment of visual function. The injected cells may also have had some preference/tropism to migrate behind the lens and near the retina's inner limiting membrane, without affecting the structure of these tissues. No retinal functional assessments were performed in this study. Other relevant findings were not observed in the anterior and posterior poles of the eye.
IOP increased immediately after intravitreal injection in all groups, probably due in part to the increased volume associated with the injection and possibly due to the physical trauma associated with the penetration of the needle through the conjunctiva and sclera into the vitreous, withdrawal of the needle, and the pinching of the conjunctival and sclera with the tying forceps. One day later, the IOP had returned to normal values. These findings are consistent with intravitreal injection prospective studies of antiangiogenic treatments often administered by this route [36].
The histological findings of the present study showed that MSV® cells did not affect the structure of the cornea, iridocorneal angle, retina, or optic nerve. Further, examination of the liver, spleen, and gonads also revealed no unusual findings.
Several studies in rodent models of retinal pathologies revealed that MSCs injected into the vitreous cavity survived, matured, and secreted BDNF, CNTF, and bFGF for at least 4 to 5 weeks [25, 26]. In our study, to determine whether the cells remained alive beyond 5 weeks, survival of the MSV® cells was evaluated at 2 and 6 weeks after the injection. The results showed that cells were present at at least 2 weeks but were not detected by FISH at 6 weeks. FISH did not show the presence of MSV® cells outside of the vitreous cavity. It is probable that the size of the MSCs (average diameter = 17.9 μm) [37], prevented their passage through the small pores of the inner limiting membrane (average diameter = 13.5 nm) [38], thus preventing the entry of these cells into the retina. Additionally, the normal blood-retinal barrier may not allow the systemic migration of intraocular injected cells [39]. In murine models of NAION, 50% of the retinal ganglion cells die within 2 weeks of the ischemia onset [40]. Thus, a survival time of 2 weeks for the injected MSV cells could be sufficient for them to secrete neurotrophic factors that could effectively treat or at least mitigate this pathology and perhaps other retinal diseases as well.
In summary, MSV® cells are human MSCs derived from bone marrow and are approved for allogenic or autologous use in several clinical trials by AEMPS (PEI: 15–007). Thus, MSV® is a product suitable for cell therapy and can be administered by intravitreal injection. These cells are safe and well-tolerated by healthy, immunocompetent pigmented rabbits when administered intravitreally at a dose of 15 × 106 cells/ml. Hence, we proposed that intravitreal MSV® cells are biocompatible and can be safely evaluated in clinical studies to modulate the microenvironment of diseased tissues, promote cell survival, and activate endogenous repair mechanisms of the retina and optic nerve.
References
Mariotti SP (2010) Global data on visual impairments 2010. World Health Organization, http://www.who.int/blindness/GLOBALDATAFINALforweb.pdf, pp. 17. Accessed Jul 2016
Hayreh SS, Jonas JB, Zimmerman MB (2007) Nonarteritic anterior ischemic optic neuropathy and tobacco smoking. Ophthalmology 114:804–809. https://doi.org/10.1016/j.ophtha.2006.07.062
Hayreh SS, Zimmerman MB (2007) Optic disc edema in non-arteritic anterior ischemic optic neuropathy. Graefes Arch Clin Exp Ophthalmol 245:1107–1121. https://doi.org/10.1007/s00417-006-0494-0
Kupersmith MJ, Frohman L, Sanderson M, Jacobs J, Hirschfeld J, Ku C, Warren FA (1997) Aspirin reduces the incidence of second eye NAION: a retrospective study. J Neuroophthalmol 17:250–253
Beck RW, Hayreh SS, Podhajsky PA, Tan ES, Moke PS (1997) Aspirin therapy in nonarteritic anterior ischemic optic neuropathy. Am J Ophthalmol 123:212–217
Group IONDTR (2000) Ischemic optic neuropathy decompression trial: twenty-four-month update. Arch Ophthalmol 118:793–798
Hayreh SS, Zimmerman MB (2008) Non-arteritic anterior ischemic optic neuropathy: role of systemic corticosteroid therapy. Graefes Arch Clin Exp Ophthalmol 246:1029–1046. https://doi.org/10.1007/s00417-008-0805-8
Beck RW (2000) Does Levodopa improve visual function in NAION? Ophthalmology 107: 1431-1434; discusson 1435-1438
Bernstein SL, Mehrabyan Z, Guo Y, Moianie N (2007) Estrogen is not neuroprotective in a rodent model of optic nerve stroke. Mol Vis 13:1920–1925
Modarres M, Falavarjani KG, Nazari H, Sanjari MS, Aghamohammadi F, Homaii M, Samiy N (2011) Intravitreal erythropoietin injection for the treatment of non-arteritic anterior ischaemic optic neuropathy. Br J Ophthalmol 95:992–995. https://doi.org/10.1136/bjo.2010.191627
Wilhelm B, Ludtke H, Wilhelm H, Group BS (2006) Efficacy and tolerability of 0.2% brimonidine tartrate for the treatment of acute non-arteritic anterior ischemic optic neuropathy (NAION): a 3-month, double-masked, randomised, placebo-controlled trial. Graefes Arch Clin Exp Ophthalmol 244:551–558. https://doi.org/10.1007/s00417-005-0102-8
Pece A, Querques G, Quinto A, Isola V (2010) Intravitreal ranibizumab injection for nonarteritic ischemic optic neuropathy. J Ocul Pharmacol Ther 26:523–527. https://doi.org/10.1089/jop.2010.0053
Lamba DA, Karl MO, Reh TA (2009) Strategies for retinal repair: cell replacement and regeneration. Prog Brain Res 175:23–31. https://doi.org/10.1016/S0079-6123(09)17502-7
Abdallah BM, Kassem M (2008) Human mesenchymal stem cells: from basic biology to clinical applications. Gene Ther 15:109–116. https://doi.org/10.1038/sj.gt.3303067
Phinney DG, Isakova I (2005) Plasticity and therapeutic potential of mesenchymal stem cells in the nervous system. Curr Pharm Des 11:1255–1265
Bull ND, Martin KR (2009) Using stem cells to mend the retina in ocular disease. Regen Med 4:855–864. https://doi.org/10.2217/rme.09.59
Parekkadan B, Milwid JM (2010) Mesenchymal stem cells as therapeutics. Annu Rev Biomed Eng 12:87–117. https://doi.org/10.1146/annurev-bioeng-070909-105309
Xu W, Xu GX (2011) Mesenchymal stem cells for retinal diseases. Int J Ophthalmol 4:413–421. https://doi.org/10.3980/j.issn.2222-3959.2011.04.19
McLaren A (2001) Ethical and social considerations of stem cell research. Nature 414:129–131. https://doi.org/10.1038/35102194
Nauta AJ, Fibbe WE (2007) Immunomodulatory properties of mesenchymal stromal cells. Blood 110:3499–3506. https://doi.org/10.1182/blood-2007-02-069716
Vega A, Martin-Ferrero MA, Del Canto F, Alberca M, Garcia V, Munar A, Orozco L, Soler R, Fuertes JJ, Huguet M, Sanchez A, Garcia-Sancho J (2015) Treatment of knee osteoarthritis with Allogeneic bone marrow Mesenchymal stem cells: a randomized controlled trial. Transplantation 99:1681–1690. https://doi.org/10.1097/TP.0000000000000678
Seo JH, Cho SR (2012) Neurorestoration induced by mesenchymal stem cells: potential therapeutic mechanisms for clinical trials. Yonsei Med J 53:1059–1067. https://doi.org/10.3349/ymj.2012.53.6.1059
Labouyrie E, Dubus P, Groppi A, Mahon FX, Ferrer J, Parrens M, Reiffers J, de Mascarel A, Merlio JP (1999) Expression of neurotrophins and their receptors in human bone marrow. Am J Pathol 154:405–415. https://doi.org/10.1016/S0002-9440(10)65287-X
Lin N, Hu K, Chen S, Xie S, Tang Z, Lin J, Xu R (2009) Nerve growth factor-mediated paracrine regulation of hepatic stellate cells by multipotent mesenchymal stromal cells. Life Sci 85:291–295. https://doi.org/10.1016/j.lfs.2009.06.007
Li N, Li XR, Yuan JQ (2009) Effects of bone-marrow mesenchymal stem cells transplanted into vitreous cavity of rat injured by ischemia/reperfusion. Graefes Arch Clin Exp Ophthalmol 247:503–514. https://doi.org/10.1007/s00417-008-1009-y
Levkovitch-Verbin H, Sadan O, Vander S, Rosner M, Barhum Y, Melamed E, Offen D, Melamed S (2010) Intravitreal injections of neurotrophic factors secreting mesenchymal stem cells are neuroprotective in rat eyes following optic nerve transection. Invest Ophthalmol Vis Sci 51:6394–6400. https://doi.org/10.1167/iovs.09-4310
Kaplan HJ, Chiang CW, Chen J, Song SK (2010) Vitreous volume of the mouse measured by quantitative high-resolution MRI. Invest Ophthalmol Vis Sci 51:4414–4414
Hackett R (1991) Eye irritation. In: Marzulli F, Maibach H (eds) Advances in modern toxicology: Dermatoxicology. Hemisphere Publishing Corporation, Washington, DC, pp 749–815
Makki JS (2016) Diagnostic implication and clinical relevance of ancillary techniques in clinical pathology practice. Clin Med Insights Pathol 9:5–11. https://doi.org/10.4137/CPath.S32784
Ramirez BE, Sanchez A, Herreras JM, Fernandez I, Garcia-Sancho J, Nieto-Miguel T, Calonge M (2015) Stem cell therapy for corneal epithelium regeneration following good manufacturing and clinical procedures. Biomed Res Int 2015:408495. https://doi.org/10.1155/2015/408495
Del Amo EM, Urtti A (2015) Rabbit as an animal model for intravitreal pharmacokinetics: clinical predictability and quality of the published data. Exp Eye Res 137:111–124. https://doi.org/10.1016/j.exer.2015.05.003
Bernstein SL, Johnson MA, Miller NR (2011) Nonarteritic anterior ischemic optic neuropathy (NAION) and its experimental models. Prog Retin Eye Res 30:167–187. https://doi.org/10.1016/j.preteyeres.2011.02.003
Griffin G, Clark JM, Zurlo J, Ritskes-Hoitinga M (2014) Scientific uses of animals: harm-benefit analysis and complementary approaches to implementing the three Rs. Rev Sci Tech 33:265–272
Siqueira RC, Messias A, Voltarelli JC, Scott IU, Jorge R (2011) Intravitreal injection of autologous bone marrow-derived mononuclear cells for hereditary retinal dystrophy: a phase I trial. Retina 31:1207–1214. https://doi.org/10.1097/IAE.0b013e3181f9c242
Jonas JB, Witzens-Harig M, Arseniev L, Ho AD (2008) Intravitreal autologous bone marrow-derived mononuclear cell transplantation: a feasibility report. Acta Ophthalmol 86:225–226. https://doi.org/10.1111/j.1600-0420.2007.00987.x
Lee JW, Park H, Choi JH, Lee HJ, Moon SW, Kang JH, Kim YG (2016) Short-term changes of intraocular pressure and ocular perfusion pressure after intravitreal injection of bevacizumab or ranibizumab. BMC Ophthalmol 16:69. https://doi.org/10.1186/s12886-016-0255-8
Ge J, Guo L, Wang S, Zhang Y, Cai T, Zhao RC, Wu Y (2014) The size of mesenchymal stem cells is a significant cause of vascular obstructions and stroke. Stem Cell Rev 10:295–303. https://doi.org/10.1007/s12015-013-9492-x
Nishihara H (1989) Studies on the ultrastructure of the inner limiting membrane of the retina. I. Surface replication study on the inner limiting membrane of the retina. Nippon Ganka Gakkai Zasshi 93:429–438
Shen J, Durairaj C, Lin T, Liu Y, Burke J (2014) Ocular pharmacokinetics of intravitreally administered brimonidine and dexamethasone in animal models with and without blood-retinal barrier breakdown. Invest Ophthalmol Vis Sci 55:1056–1066. https://doi.org/10.1167/iovs.13-13650
Zhang C, Guo Y, Slater BJ, Miller NR, Bernstein SL (2010) Axonal degeneration, regeneration and ganglion cell death in a rodent model of anterior ischemic optic neuropathy (rAION). Exp Eye Res 91:286–292. https://doi.org/10.1016/j.exer.2010.05.021
Acknowledgements
This work was supported by grants from the Consejería de Educación de la Junta de Castilla y León (grant number VA118U14); and the Centro en Red de Medicina Regenerativa y Terapia Celular de la Junta de Castilla y León, Spain. The FISH technique was performed by the Cytogenetics Oncology Unit (University of Salamanca, Spain) following the protocol provided by the manufacturer. I Fernandez-Bueno, GK Srivastava and S Tabera-Bartolomé were supported by RETICS (RD12/0034/0001), Instituto de Salud Carlos III, Spain; Centro en Red de Medicina Regenerativa y Terapia Celular de la Junta de Castilla y Leon, Spain; and Red de Terapia Celular (RD12/0019/0036), Instituto de Salud Carlos III, Spain, respectively. Sonia Labrador Velandia and María L Alonso-Alonso were supported by the Consejería de Educación de la Junta de Castilla y León and the Fondo Social Europeo. This study was presented in part at The Association for Research in Vision and Ophthalmology (ARVO) Annual Meeting 2015, and at the European College of Veterinary Ophthalmologists (ECVO) Annual Scientific Meeting 2015.
Funding
This work was supported by grants from the Consejería de Educación de la Junta de Castilla y León (grant number VA118U14); and the Centro en Red de Medicina Regenerativa y Terapia Celular de la Junta de Castilla y León, Spain.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest, or non-financial interest in the subject matter or materials discussed in this manuscript.
Statement on the welfare of animals
All procedures performed in studies involving animals were in accordance with the ethical standards of the institution or practice at which the studies were conducted in agreement with European (Council Directive 2010/63/UE) and Spanish regulations (RD 53/2013).
Rights and permissions
About this article
Cite this article
Labrador Velandia, S., Di Lauro, S., Alonso-Alonso, M.L. et al. Biocompatibility of intravitreal injection of human mesenchymal stem cells in immunocompetent rabbits. Graefes Arch Clin Exp Ophthalmol 256, 125–134 (2018). https://doi.org/10.1007/s00417-017-3842-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-017-3842-3