Abstract
Purpose
To report electroretinographic (ERG) findings in advanced glaucoma treated with a single intravitreal injection of bone marrow-derived mesenchymal stem cells (MSCs).
Methods
Intravitreal injection of autologous MSCs (1 × 106 cells) was performed in 2 eyes from 2 patients with open-angle glaucoma in advanced stage of optic neuropathy (ClinicalTrials.gov, NCT02330978, 01.05.2015): cup/disk ratio worse than 0.9, visual field mean deviation index lower than − 15 dB, visual acuity of light perception, but controlled intraocular pressure. ERG tests were recorded at baseline and week 1, 4 and 48 after injection, using DTL electrodes following the ISCEV standard: After dark adaptation, ERG was elicited using white flashes of 0.01 cd.s/m2 and 3.0 cd.s/m2, followed by 10-min light adaptation (30 cd/m2) and stimuli of 3.0 cd.s/m2 and 30 Hz flicker.
Results
Patients did not show improvement on visual acuity or visual field after treatment. At baseline, ERG responses showed typical findings for advanced glaucoma, with a- and b-wave amplitude and latency within normative range, but reduced photopic negative responses. No noteworthy changes were observed on ERG responses for both cases up to 1 week after treatment, but at day 15, one patient showed retinal detachment with proliferative vitreoretinopathy and was removed from the trial. The other patient kept ERG responses stable throughout study period.
Conclusion
Although no ERG response changes were observed after MSCs injection in one case, the complication observed on the second one, along with the lack of visual function improvement, warrants further studies involving modified MSCs to treat ocular disorders, including glaucoma.
Trial registration: ClinicalTrials.gov, NCT02330978- missed in pdf
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
There is no definitive treatment to either prevent or restore retinal ganglion cells damage responsible for the permanent loss of vision in glaucoma. Recently, in vitro studies suggest that mesenchymal stem cells (MSCs) might induce cell-mediated retinal ganglion cell neuroprotection [1], and several reports indicate the potential of MSCs as a regenerative therapy for glaucoma [2, 3].
There are mainly two approaches under investigation for MSCs in glaucoma: implanting the cells into the ocular anterior chamber, targeting regeneration of trabecular meshwork [4] or as a neuroprotective cellular therapy [3, 5, 6]. Although viable MSCs have been identified up to 30 days after intravitreal injections [7], there is no report on the use of MSCs in glaucomatous human eyes as a neuroprotective therapeutic option.
This report describes, for the first time, the retinal function outcomes after bone marrow-derived MSCs injection in two patients with advanced glaucoma during a 1-year follow-up period.
Methods
We conducted a clinical trial (ClinicalTrials.gov, NCT02330978) at the Ribeirão Preto Medical School, University of São Paulo (USP, Brazil), on safety of the use of autologous, bone marrow-derived MSCs for treating selected cases of advanced primary open-angle glaucoma (POAG).
The study was approved by the local ethical committee (process number 14151/2010), and two blinded adults - with baseline visual acuity of light perception on their right eyes (OD) due exclusively to open-angle glaucoma - were included and signed the informed consent. The norms of the Declaration of Helsinki and the International Conference on Standardization Note for Guidance on Good Clinical Practice (ICH, Topic E6, 1995) were followed accordingly.
Patients (both male; 53 and 75 years old) showed bilateral cup/disk ratio worse than 0.9, visual field (VF) mean deviation index lower than − 15 dB, but controlled intraocular pressure (IOP), and no systemic comorbidities. They showed baseline visual acuity of hand motion on their left eyes (OS). All eyes were pseudophakic.
A single intravitreal injection of 0.1 ml of a suspension containing 1 × 106 autologous bone marrow MSCs (prepared at the Blood Center of Ribeirão Preto - USP) was performed in the superior temporal region of the worst eyes (OD). According to the approved protocol, bone marrow cells were aspirated from the patient’s iliac crest, under anesthesia, separated, and cultured.
Follow-up visits were proposed at six time points: 1 and 2 weeks, 1, 3, 6, and 12 months after baseline. In all visits, participants underwent a comprehensive ophthalmic examination, including visual acuity, slit-lamp biomicroscopy, IOP measurement (Goldmann tonometry), dilated funduscopic examination and fundus imaging, standard automated perimetry with the 24–2 Swedish interactive threshold algorithm (Carl Zeiss Meditec, Inc., Dublin, California, USA), and spectral-domain optical coherence tomography (sdOCT) with circumpapillary RNFL thickness protocol (Spectralis, Heidelberg Engineering, Heidelberg, Germany). Electroretinographic tests (ERG) were recorded at baseline and week 1 and 4, and at 12 months after injection, using DTL electrodes following the ISCEV standard [8]: After dark adaptation (25 min), ERGs were elicited using white flashes of 0.01 cd.s/m2 and 3.0 cd.s/m2 for rod and combined response, respectively, followed by 10-min light adaptation (30 cd/m2) and stimuli of 3.0 cd.s/m2 (cone) and 30 Hz flicker.
Results
Patients did not show improvement on either visual acuity (light perception) or VF sensitivities after treatment, and also, they did not refer changes on any subjective aspect of their visual perception in the treated eye.
The slit-lamp examination did not show signs of eye inflammatory reaction: Neither anterior chamber cells nor corneal changes were noticed. No remarkable change in IOP and sdOCT measures was noted during the follow-up period (Table 1). Fundus examination presented no vitreous or retinal abnormalities up to 15-day follow-up compared to baseline.
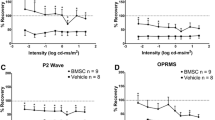
At baseline, dark- and light-adapted ERG responses showed typical findings for advanced glaucoma, with a- and b-wave amplitude and latency within the normative range, but reduced photopic negative responses (Fig. 1). No noteworthy changes were observed on ERG responses for both cases up to 7 days after treatment, but on day 14, one patient showed an inferior retinal detachment with proliferative vitreoretinopathy (Fig. 2). The other patient kept ERG responses stable throughout the study period with no signs of retinal abnormalities (Figs. 1 and 3).
Fundus images (left images) and retina fluorescein angiography (right images) of patient 2 taken after 30 days of the intravitreal injection of autologous bone marrow mesenchymal stromal cells (right eye, 1.106 cells). Top images: total retinal detachment including the macular region, with mild folds observed in the inferior retina and no hemorrhages or significant vitreous haze. Bottom images: inferotemporal images showing more evident retinal folds and a yellowish diffuse subretinal exudative fluid, with fluorescein pooling in the periphery. Note: a moderate vitreoretinal proliferation in this region was detected during the pars plana vitrectomy
Color fundus images (top), retina fluorescein angiography (middle), and optical coherence tomography results (bottom) of patient 1, before (left) and after 4 weeks (center), and 48 weeks (right) the intravitreal injection of autologous bone marrow mesenchymal stromal cells (right eye, 1.106 cells). Besides the advanced cup/disk ratio, no differences were detected between the three moments of all these examinations. Note segmentation artifacts in the retinal nerve fiber layer thickness analyses of the temporal region (right eye, red arrows)
Retinal detachment was promptly treated with a successful pars plana vitrectomy and silicone oil tamponade, but the patient was removed from the trial, and ERG was no longer performed. At the final follow-up period (12 months), he remained with no retinal detachment and visual acuity measured as light perception.
Discussion
We described two different outcomes observed after intravitreal injections of bone marrow MSCs in human eyes, highlighting the concerns related to this procedure's safety. Although MSCs therapy has been previously associated with improvements in the retinal function, as in experimental retinal dystrophy [9] and assessed by ERG in glaucoma [10], the safety of MSCs injections in humans was still unknown.
After bone marrow-derived MSCs treatment, ERG outcomes showed no functional improvement that could have been detected, for instance, with an increase in the photopic-negative response amplitude. Although some PhNR variation was detected during follow-up in patient 1, our study was not designed to evaluate such effects since only two advanced glaucoma cases were included. Nonetheless, ERG did not deteriorate up to 7 days after injection for both cases, indicating retinal safety of intravitreal MSCs.
The vitreous-retinal proliferative changes observed in the second case seem to be responsible for the retinal detachment. The intravitreal injection was done uneventfully in the superior temporal quadrant - with no bleeding or retinal breaks observed after the procedure - and the retinal detachment was observed in the inferior region two weeks later when vitreous-retinal proliferative changes were also present.
A proinflammatory effect might have been the cause and has previously been reported after autologous stem cells injected into the vitreous cavity, including retinal detachment and severe proliferative vitreoretinopathy [2, 11]. In this context, it would be rational to think that pluripotent stem cells injected intravitreally may differentiate into myofibroblast-like cells [12], which could contribute to vitreous fibrosis and contraction, facilitating eventual vitreoretinal tractions. Nevertheless, this cellular differentiation could be controlled in future trials.
Of interest, since ERG responses were kept stable until the retinal detachment was observed in one case and throughout the other case's follow-up, we believe that products from MSCs are well tolerated into the vitreous cavity. They might have an eventual neuroprotective effect on the retina (not observed here) and caused no function damage, but the complications observed may be attributed to the cellular proliferation and fibrosis observed in the vitreous of patient 2.
Even with the ERG not showing retinal function loss after intravitreal MSCs, the risk of severe adverse effects and the absence of any visual improvement suggest that further studies using modified MSCs are required before considering their clinical use in ocular neurodegenerative diseases, including glaucoma.
Availability of data and material
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
References
Johnson TV, DeKorver NW, Levasseur VA et al (2014) Identification of retinal ganglion cell neuroprotection conferred by platelet-derived growth factor through analysis of the mesenchymal stem cell secretome. Brain 137(2):503–519
Park SS, Moisseiev E, Bauer G et al (2017) Advances in bone marrow stem cell therapy for retinal dysfunction. Prog Retin Eye Res 56:148–165
Harrell CR, Fellabaum C, Arsenijevic A, Markovic BS, Djonov V, Volarevic V (2019) Therapeutic potential of mesenchymal stem cells and their secretome in the treatment of glaucoma. Stem Cells Int 2019:7869130
Castro A, Du Y (2019) Trabecular meshwork regeneration—a potential treatment for glaucoma. Curr Ophthalmol Rep 7(2):80–88
Roubeix C, Godefroy D, Mias C et al (2015) Intraocular pressure reduction and neuroprotection conferred by bone marrow-derived mesenchymal stem cells in an animal model of glaucoma. Stem Cell Res Ther 6:177
Mead B, Hill LJ, Blanch RJ et al (2016) Mesenchymal stromal cell-mediated neuroprotection and functional preservation of retinal ganglion cells in a rodent model of glaucoma. Cytotherapy 18(4):487–496
Vilela CAP, Souza LEB, Siqueira RC, Calado RT, Covas DT, Paula JS (2018) Ex vivo evaluation of intravitreal mesenchymal stromal cell viability using bioluminescence imaging. Stem Cell Res Ther 9(1):155
McCulloch DL, Marmor MF, Brigell MG et al (2015) ISCEV Standard for full-field clinical electroretinography (2015 update). Doc Ophthalmol 130(1):1–12
Tzameret A, Sher I, Belkin M et al (2014) Transplantation of human bone marrow mesenchymal stem cells as a thin subretinal layer ameliorates retinal degeneration in a rat model of retinal dystrophy. Exp Eye Res 118:135–144
Mead B, Amaral J, Tomarev S (2018) Mesenchymal stem cell-derived small extracellular vesicles promote neuroprotection in rodent models of glaucoma. Invest Ophthalmol Vis Sci 59(2):702–714
Kuriyan AE, Albini TA, Townsend JH et al (2017) Vision loss after intravitreal injection of autologous “stem cells” for AMD. N Engl J Med 376(11):1047–1053
Pennock S, Haddock LJ, Eliott D, Mukai S, Kazlauskas A (2014) Is neutralizing vitreal growth factors a viable strategy to prevent proliferative vitreoretinopathy? Prog Retin Eye Res 40:16–34
Acknowledgements
We would kindly like to acknowledge Dr. Diego Villa Clé for performing the iliac crest aspiration to collect the bone marrow samples, as well as Prof. Rodrigo Jorge and Prof. Maria de Lourdes Veronese Rodrigues for discussing specific points of the methodology. We also acknowledge the CNPq - Brazil for the research Grant (Process # 401181/2013-8).
Funding
This study received a research Grant from CNPq - Brazil (Process # 401181/2013–8).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Statement of human rights
Informed consent was obtained from all individual participants included in the study.
Consent for publication
All authors have had full access to the entire review and agree with the decision to submit for publication.
Conflict of interest
Authors do not have any commercial or proprietary conflicting, competing interests in the materials or products described (directly or indirectly related to) in the article. The results presented in this manuscript were not presented at any previous scientific meeting.
Ethics approval
All procedures performed in this study were approved by the Ribeirão Preto Clinical Hospital Ethical Committee (process number 14151/2010) and were in accordance with Helsinki Declaration (1964) and its later amendments.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vilela, C.A.P., Messias, A., Calado, R.T. et al. Retinal function after intravitreal injection of autologous bone marrow-derived mesenchymal stromal cells in advanced glaucoma. Doc Ophthalmol 143, 33–38 (2021). https://doi.org/10.1007/s10633-021-09817-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10633-021-09817-z