Abstract
Purpose
To conduct a long-term follow-up study evaluating the efficacy and safety of transplantation of preserved limbal allograft and amniotic membrane for recurrent pterygium.
Methods
This was a retrospective, non-comparative, interventional case series conducted at a private eye hospital. Eighty-four eyes of 80 patients with recurrent pterygium were included in the study. The mean number of previous surgeries for pterygium was 1.36 ± 0.98 (range, 1–8). All subjects received transplantation of preserved limbal allograft and amniotic membrane.
Results
The mean follow-up period was 73.0 ± 38.1 months (range, 12–154 months). Pterygium recurred in 10 eyes (11.9 %). The mean period to recurrence was 16.3 ± 11.3 months (range, 5–33 months). Symblepharon was cured in 21 eyes, persisted in 2 eyes, and newly occurred in 3 eyes. Diplopia was cured in eight eyes, persisted in five eyes, and newly occurred in one eye. As for complications, intraocular pressure elevations over 21 mmHg were recognized in ten eyes of nine cases, in which the intraocular pressure was controlled by reduction of topical steroid in four eyes and by addition of topical prostaglandin derivatives in six eyes. Twenty-four eyes (28.6 %) gained two lines or more of Landolt best spectacle-corrected visual acuity (BSCVA), 56 eyes (66.7 %) stayed within one line from preoperation, and four eyes (4.8 %) lost two lines or more. There were no major complications and no graft rejection.
Conclusions
Transplantation of preserved limbal allograft and amniotic membrane is a safe and effective procedure for recurrent pterygium.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although various surgical approaches for pterygium have been reported, recurrence remains a major concern. Recurrent pterygium is more difficult to treat than primary pterygium because it is often accompanied by increased conjunctival inflammation and accelerated corneal involvement. Surgical procedures for the treatment of recurrent pterygium reported so far include lamellar keratoplasty [1–3], conjunctival autograft [4–13], limbal autograft [9, 10, 14–17], amniotic membrane transplantation [8, 18, 19], and lamellar scleroplasty [20, 21]. The recurrence rate varies depending on the surgical procedure and the duration of follow-up (Table 1).
Limbal allograft and preserved amniotic membrane transplantation has been successfully performed for the treatment of limbal stem cell deficiency, such as chemical burns [22], Stevens–Johnson syndrome [23, 24], and aniridic keratopathy [25]. Recurrent pterygium is a condition in which partial limbal stem cell deficiency and inflammation coexist, and for which limbal allograft and preserved amniotic membrane transplantation is expected to be effective. Previous studies reported that lamellar scleroplasty that included limbal transplantation was effective for the treatment of recurrent pterygium [20, 21]. Previously, we reported a pilot study demonstrating the efficacy and safety of transplantation of preserved limbal allograft and amniotic membrane for the treatment of recurrent pterygium in 12 eyes with a mean follow-up period of 21.6 months [26]. In the current study, we report the results of this surgery for recurrent pterygium in 84 eyes with a mean follow-up period of 73.0 months.
Methods
Subjects
This study was conducted in accordance with the Declaration of Helsinki. The ethics committee of Miyata Eye Hospital approved the entire operative procedure and use of human amniotic membrane for this surgery. Patients with recurrent pterygium were included in this study. The exclusion criteria were uncontrolled glaucoma, loss of vision as a result of other causes, intercurrent severe systemic disease, or any condition affecting follow-up or documentation. A consecutive series of 84 eyes of 80 patients (35 male and 45 female) with recurrent pterygium were treated with transplantation of preserved limbal allograft and amniotic membrane, and intraoperative mitomycin C (MMC) at the Miyata Eye Hospital from February 2002 to February 2014. The patients’ demographic data are shown in Table 2. Symblepharon was observed in 23 eyes and diplopia was observed in 13 eyes. Informed consent was obtained from all subjects before surgery.
Surgical procedure
Informed consent was obtained from pregnant donors of the amniotic membrane used for clinical ophthalmic application. Amniotic membranes were prepared for use in ophthalmic surgery as described previously [26]. All corneas used for limbal allograft were obtained from the Rocky Mountain Lions Eye Bank (Aurora, CO, USA). A central 7-mm or 7.5-mm graft was used for penetrating keratoplasty in other patients and sliced in half horizontally using a sclerotome blade (Becton Dickinson, Walthan, MA, USA). The epithelial side was used for the surgery.
The surgical procedure is described in our previous study [26]. Briefly, the pterygium head was dissected bluntly and fibrous tissues were removed carefully as not to damage the medial rectus muscle. Marginal conjunctiva and subconjunctival fibrovascular tissues were thoroughly dissected. Several surgical sponges soaked with 0.02 % MMC were placed beneath the conjunctival tissue for 1 minute and the area was irrigated with 500 ml of saline. The amniotic membrane was sutured with a 10–0 polyglycolic acid suture (BioSorb®, Alcon, Fort Worth, TX, USA) to fully cover the bare sclera. The limbal allograft was trimmed to cover the limbal-deficient area. The graft was fixed tightly on top of the amniotic membrane on the sclera with a 10–0 nylon suture (Alcon).
Examinations
Pre- and postoperative examination included visual acuity, intraocular pressure measurement, and slit-lamp examination. Recurrence was defined as fibrovascular tissue invasion beyond the limbus. Symblepharon formation and diplopia occurrence were also evaluated before and after surgery. Graft rejection was defined as occurrence of cellular infiltration and epithelial defect on the graft area without an infectious focus. Topical 0.1 % betamethasone sodium phosphate eye drops (Shionogi Pharmaceutical, Osaka, Japan) and 0.5 % levofloxacin eye drops (Santen Pharmaceutical, Osaka, Japan) were used four times daily postoperatively and were tapered off. After topical betamethasone phosphate was stopped, topical 0.1 % fluorometholone (Santen Pharmaceutical) was started and tapered off. The administration period of postoperative topical corticosteroids was recorded. The endpoint of topical corticosteroid usage was determined based on sufficient disappearance of inflammation, as determined by slit-lamp findings. The efficacy and safety of this treatment was determined by comparing the recurrence rate and the postoperative complications with those in previous studies. All data here are means ± standard deviations unless otherwise specified.
Results
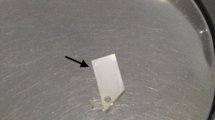
The representative cases are shown in Fig. 1a–i. During the mean follow-up period of 73.0 ± 38.1 months (range, 12–154 months), pterygium recurred in 10 eyes (11.9 %). The mean period to recurrence was 16.3 ± 11.3 months (range, 5–33 months).
Pre- and postoperative slit views in representative cases. Case 1. (a) 66-year-old male. Preoperative left eye with recurrent pterygium (arrow) after two surgeries. Inflammatory injection was observed (arrow head). Best spectacle-corrected visual acuity (BSCVA) was 20/15. (b) One month after surgery. Moderate injection was observed (arrow head). (c) Five years after surgery. Inflammation had thoroughly subsided. There was no pterygium recurrence. BSCVA was 20/12. Case 2. (d) 62-year-old female. Preoperative left eye with recurrent pterygium (arrow) after surgery. Mild injection was observed (arrow head). BSCVA was 20/200. (e) Two weeks after surgery. Moderate injection was observed (arrow head). (f) Four years after surgery. Inflammation had thoroughly subsided. There was no pterygium recurrence. BSCVA was 20/15. Case 3. (g) 57-year-old male. Preoperative left eye with recurrent pterygium after two surgeries (arrow). Inflammatory injection was observed (arrow head). BSCVA was 15/20. (h) One month after surgery. Mild injection was observed (arrow head). (i) Five years after surgery. Recurrence of fibrovascular tissue invasion at limbus of 6–10 o’clock position was recognized (arrows). Mild injection was observed (arrow head). BSCVA was 20/12.
Preoperatively, symblepharon was observed in 23 eyes and diplopia was observed in 13 eyes. Symblepharon was cured in 21 eyes, persisted in two eyes, and newly occurred in three eyes. Diplopia was cured in eight eyes, persisted in five eyes, and newly occurred in one eye.
As for complications, intraocular pressure elevations over 21 mmHg were recognized in ten eyes of nine patients. The intraocular pressure was controlled by reduction of topical steroid in four eyes and topical prostaglandin derivatives in six eyes. Glaucoma surgeries were not necessary in any eyes. After the pterygium surgery, cataract surgery was performed in 27 eyes (32.1 %) during the follow-up period. Graft rejection and scleral melting related to MMC use were not observed in any eyes.
Twenty-four eyes (28.6 %) gained two lines or more on Landolt best spectacle-corrected visual acuity (BSCVA), 56 eyes (66.7 %) stayed within one line from preoperation, and 4 eyes (4.8 %) lost two lines or more. The decrease in BSCVA was a result of the progression of cataract in the four eyes.
The mean period of postoperative topical betamethasone and fluorometholone usage was 9.1 ± 6.7 months (range, 0.5–35.7 months) and 21.5 ± 19.0 months (range, 0–96.2 months), respectively.
Discussion
In our previous pilot study, we investigated the efficacy and safety of transplantation of preserved limbal allograft and amniotic membrane for the treatment of recurrent pterygium in 12 eyes with a mean follow-up period of 21.6 months, and there was no recurrence of pterygium and major complications during the follow-up period. Since then, we have performed the same surgery in 84 eyes with recurrent pterygium and reported the results in the current study. The results show that pterygium recurred in 10 eyes (11.9 %) during the mean follow-up period of 73.0 months after this surgery and the mean period to recurrence was 16.3 months. There were no major complications, confirming the safety of this treatment. Among various surgical procedures proposed for the treatment of recurrent pterygium, conjunctival or limbal autografts with or without an amniotic membrane have a relatively low recurrence rate of 0–25 % [4–17]. Some of these previous studies reported low recurrence rate less than 10 % [4–6, 8, 12, 14, 16]. However, all of them were small studies with subjects less than 40 and most of them had a short follow-up period of 6 months or less [4–6, 8, 12, 16]. As shown in the current study, the mean period to recurrence was over 1 year. Thus, it is highly likely that the recurrence rate in the previous studies would have been much higher if the follow-up period were long enough. Taken together, the recurrence rate of 11.9 % in 84 eyes during the minimum follow-up period of 12 months confirmed that this surgery is effective for recurrent pterygium. As discussed in our previous report [26], there are a couple of possible mechanisms for the low recurrence rate of our surgical procedure and adjunctive therapy. Firstly, limbal allografts serve as a barrier to the invasion of conjunctival fibrovascular tissue [22–25]. Secondly, the amniotic membrane, having anti-fibrotic [27] and anti-inflammatory [28] properties, reduces proliferation of subconjunctival fibrovascular tissue. Finally, adjunctive therapy of topical steroids and intraoperative MMC might also attenuate inflammatory and proliferative processes in the subconjunctival tissue, contributing to the prevention of recurrence.
Compared with conjunctival autografts, limbal allografts have advantages and disadvantages. Recurrent pterygium is usually more extensive than a primary pterygium; therefore, a large enough barrier to stop invading conjunctival tissue is necessary for the treatment of recurrent pterygium. In this regard, limbal allografts have an advantage over conjunctival autografts because limbal autografts can supply a greater amount of tissue than conjunctival autografts. Additionally, amniotic membranes can cover large areas of bare sclera after thorough removal of the recurring pterygium, thereby decreasing inflammatory and proliferative processes. Thus, the combination of limbal allograft and amniotic membrane transplantation can supply a large enough barrier and anti-inflammatory effect after the surgery. On the other hand, rejection is a major concern of limbal allograft transplantation. In this series, the epithelial defect of the corneal and conjunctival area recovered within 2 weeks following surgery and there were no recurrences of the epithelial defects. There was no apparent limbal allograft rejection during the follow-up period of at least 12 months. Topical corticosteroids might have prevented rejection. It is also possible that transplanted epithelial cells were gradually replaced with surrounding host corneal or conjunctival epithelial cells without apparent rejection. Another major concern is the adverse effects of prolonged use of topical steroids such as intraocular pressure rise and cataract progression. Ten eyes (11.9 %) showed intraocular pressure elevations greater than 21 mmHg, which were controlled by reduction of the topical steroid or the addition of topical prostaglandin derivatives, and glaucoma surgeries were not necessary in any eyes. After the pterygium surgery, cataract surgery was performed in 27 eyes (32.1 %) during the follow-up period. Topical steroids might contribute to the progression of cataract in some of those cases, but all of them were successfully treated with surgery.
In this study, 24 eyes (28.6 %) gained two lines or more on the Landolt BSCVA, 56 eyes (66.7 %) stayed within one line from preoperation, and four eyes (4.8 %) lost two lines or more. Our previous study [29] showed that pterygium removal decreases corneal irregular astigmatism. Decreased irregular astigmatism as well as removal of opacity in the pupillary area might have increased best-corrected visual acuity in most cases.
In the present study, pterygium recurred in ten eyes (11.9 %). For the eyes with recurrent pterygium, the same surgery can be performed because a limbal allograft is available. On the other hand, when recurrence occurred in eyes in which a large conjunctival autograft was used, the same surgery using a conjunctival autograft is sometimes difficult to perform because the available conjunctiva is limited. Thus, repeatability may be one of the advantages of surgery using a limbal allograft over surgery that uses a conjunctival autograft.
There were several limitations in this study. First, due to its retrospective nature, the follow-up period ranged from 12 to 154 months. Because the mean period to recurrence was 16.3 months (range, 5–33 months), the follow-up period of 12 months may not be long enough in some eyes to observe recurrences of pterygium. Second, one surgical procedure alone was evaluated in this study. A comparison with some of the more common surgeries such as conjunctival or limbal autograft would have provided more information on the benefits of this surgical technique. Third, the subjects included in this study consisted solely of Asian patients. In Caucasian eyes with weaker wound healing, the evaluation of this surgery in comparison with other surgical procedures might yield different results. Fourth, the mechanism of this treatment was not confirmed. We supposed that the limbal grafts serve as barriers to conjunctival tissue, and amniotic membranes have anti-fibrotic and anti-inflammatory effects. But these possible mechanisms were not investigated in the current study. A future study measuring cytokines in the tear before and after the treatment may elucidate the mechanisms of this treatment.
In conclusion, transplantation of preserved limbal allograft and amniotic membrane is a safe and effective procedure for recurrent pterygium. The superiority of this surgery over more common surgeries such as conjunctival or limbal autograft should be evaluated in future studies.
References
Busin M, Halliday BL, Arffa RC et al (1986) Precarved lyophilized tissue for lamellar keratoplasty in recurrent pterygium. Am J Ophthalmol 102:222–227
Laughrea PA, Arentsen JJ (1986) Lamellar keratoplasty in the management of recurrent pterygium. Ophthalmic Surg 17:106–108
Golchin B, Butler TK, Robinson LP et al (2003) Long-term follow-up results of lamellar keratoplasty as a treatment for recurrent pterygium and for scleral necrosis induced by beta-irradiation. Cornea 22:612–618
Kenyon KR, Wagoner MD, Hettinger ME (1985) Conjunctival autograft transplantation for advanced and recurrent pterygium. Ophthalmology 92:1461–1470
Riordan-Eva P, Kielhorn I, Ficker LA et al (1993) Conjunctival autografting in the surgical management of pterygium. Eye (Lond) 7:634–638
Tan DT, Chee SP, Dear KB et al (1997) Effect of pterygium morphology on pterygium recurrence in a controlled trial comparing conjunctival autografting with bare sclera excision. Arch Ophthalmol 115:1235–1240
Figueiredo RS, Cohen EJ, Gomes JA et al (1997) Conjunctival autograft for pterygium surgery: how well does it prevent recurrence? Ophthalmic Surg Lasers 28:99–104
Prabhasawat P, Barton K, Burkett G et al (1997) Comparison of conjunctival autografts, amniotic membrane grafts, and primary closure for pterygium excision. Ophthalmology 104:974–985
Mutlu FM, Sobaci G, Tatar T et al (1999) A comparative study of recurrent pterygium surgery: limbal conjunctival autograft transplantation versus mitomycin C with conjunctival flap. Ophthalmology 106:817–821
Shimazaki J, Kosaka K, Shimmura S et al (2003) Amniotic membrane transplantation with conjunctival autograft for recurrent pterygium. Ophthalmology 110:119–124
Luanratanakorn P, Ratanapakorn T, Suwan-Apichon O et al (2006) Randomised controlled study of conjunctival autograft versus amniotic membrane graft in pterygium excision. Br J Ophthalmol 90:1476–1480
Hirst LW (2009) Recurrent pterygium surgery using pterygium extended removal followed by extended conjunctival transplant: recurrence rate and cosmesis. Ophthalmology 116:1278–1286
Katircioglu YA, Altiparmak U, Engur Goktas S et al (2015) Comparison of two techniques for the treatment of recurrent pterygium: amniotic membrane vs conjunctival autograft combined with mitomycin C. Semin Ophthalmol 30:321–327
Nabawi KS, Ghonim MA, Ali MH (2003) Evaluation of limbal conjunctival autograft and low-dose mitomycin C in the treatment of recurrent pterygium. Ophthalmic Surg Lasers Imaging 34:193–196
Shimazaki J, Shinozaki N, Tsubota K (1998) Transplantation of amniotic membrane and limbal autograft for patients with recurrent pterygium associated with symblepharon. Br J Ophthalmol 82:235–240
Fallah MR, Golabdar MR, Amozadeh J et al (2008) Transplantation of conjunctival limbal autograft and amniotic membrane vs mitomycin C and amniotic membrane in treatment of recurrent pterygium. Eye (Lond) 22:420–424
Yao YF, Qiu WY, Zhang YM et al (2006) Mitomycin C, amniotic membrane transplantation and limbal conjunctival autograft for treating multirecurrent pterygia with symblepharon and motility restriction. Graefes Arch Clin Exp Ophthalmol 244:232–236
Solomon A, Pires RT, Tseng SC (2001) Amniotic membrane transplantation after extensive removal of primary and recurrent pterygia. Ophthalmology 108:449–460
Ma DH, See LC, Hwang YS et al (2005) Comparison of amniotic membrane graft alone or combined with intraoperative mitomycin C to prevent recurrence after excision of recurrent pterygia. Cornea 24:141–150
Poirier RH, Fish JR (1976) Lamellar keratoplasty for recurrent pterygium. Ophthalmic Surg 7:38–41
Süveges I (1992) Sclerokeratoplasty in recurrent pterygium. Ger J Ophthalmol 1:114–116
Meallet MA, Espana EM, Grueterich M et al (2003) Amniotic membrane transplantation with conjunctival limbal autograft for total limbal stem cell deficiency. Ophthalmology 110:1585–1592
Gomes JA, Santos MS, Ventura AS et al (2003) Amniotic membrane with living related corneal limbal/conjunctival allograft for ocular surface reconstruction in Stevens-Johnson syndrome. Arch Ophthalmol 121:1369–1374
Shimazaki J, Shimmura S, Fujishima H et al (2000) Association of preoperative tear function with surgical outcome in severe Stevens-Johnson syndrome. Ophthalmology 107:1518–1523
Holland EJ, Djalilian AR, Schwartz GS (2003) Management of aniridic keratopathy with keratolimbal allograft: a limbal stem cell transplantation technique. Ophthalmology 110:125–130
Miyai T, Hara R, Nejima R et al (2005) Limbal allograft, amniotic membrane transplantation, and intraoperative mitomycin C for recurrent pterygium. Ophthalmology 112:1263–1267
Tseng SC, Li DQ, Ma X (1999) Suppression of transforming growth factor-beta isoforms, TGF-beta receptor type II, and myofibroblast differentiation in cultured human corneal and limbal fibroblasts by amniotic membrane matrix. J Cell Physiol 179:325–335
Solomon A, Rosenblatt M, Monroy D et al (2001) Suppression of interleukin 1alpha and interleukin 1beta in human limbal epithelial cells cultured on the amniotic membrane stromal matrix. Br J Ophthalmol 85:444–449
Tomidokoro A, Oshika T, Amano S et al (1999) Quantitative analysis of regular and irregular astigmatism induced by pterygium. Cornea 18:412–415
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of Interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Financial support
None.
Additional information
The authors have no commercial or proprietary interest in the products or companies mentioned in this article.
Rights and permissions
About this article
Cite this article
Ono, T., Mori, Y., Nejima, R. et al. Long-term follow-up of transplantation of preserved limbal allograft and amniotic membrane for recurrent pterygium. Graefes Arch Clin Exp Ophthalmol 254, 2425–2430 (2016). https://doi.org/10.1007/s00417-016-3483-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-016-3483-y