Abstract
Purpose
This study compared the outcomes of a limbal conjunctival autograft (LCAG) with those of an amniotic membrane graft (AMG) followed by intraoperative 0.02 % mitomycin C (MMC) to treat recurrent pterygium.
Methods
In this randomized controlled trial, ninety-six eyes with recurrent pterygium were enrolled and randomly allocated into two groups using a computer-generated random number table. Pterygium removal was followed by intraoperative 0.02 % MMC for 3 min and then either LCAG or AMG transplantation. The major outcomes were recurrence rate, conjunctival inflammation grade, healing time of the corneal epithelial defect, eye-movement amplitude (EMA), uncorrected distance visual acuity (UDVA), and complications.
Results
A follow-up of 12 months was conducted for 93 eyes of 82 patients. Grade D (recurrence) presented in one eye of the LCAG group and five eyes of the AMG group, with no between-group difference (p = 0.196). However, Grades A, B, and C presented in 46, zero and zero eyes of the LCAG group respectively, and in 37, two and two eyes of the AMG group respectively, with the surgical bed generally showing a better appearance in the LCAG group than in the AMG group (p = 0.008). Compared with baseline values, the postoperative EMA improved significantly in both groups (p < 0.001 for the LCAG group; p = 0.001 for the AMG group), as did UDVA (p = 0.005 for the LCAG group; p = 0.012 for the AMG group). No between-group differences were found in terms of the healing time for epithelial defect, conjunctival inflammation grade, or the frequency of complications such as punctate epithelial keratitis, episcleral melting, corneal pannus, and delayed corneal epithelium healing.
Conclusions
LCAG transplantation with intraoperative 0.02 % MMC is as efficacious in treating recurrent pterygium as AMG transplantation with MMC. The former procedure results in an attractive cosmetic appearance but might result in limbal damage in some eyes. The surgeon’s familiarity with these procedures should determine the method of treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pterygium is a common eye disease worldwide with an incidence that varies by location. Various surgical procedures exist for pterygium; however, recurrence is a major complication after pterygium removal [1]. Recurrent pterygium is more difficult to treat than primary pterygium because recurrence is often accompanied by conjunctival fornix shortening, symblepharon [2], the extension of the scar tissue to the rectus muscles [3], and accelerated corneal involvement [4].
Surgical treatments for recurrent pterygium include pterygium excision, covering the defect, and other adjunctive therapies. A high recurrence rate ranging from 48 to 82 % [5, 6] was found when recurrent pterygium was treated with excision alone. Although a single intraoperative dose of low-concentration mitomycin C (MMC) was effective in reducing recurrence in vivo, the recurrence rate remained high, ranging from 12.5 to 66.7 % when using intraoperative MMC alone [7, 8]. Therefore, the closure of the defect using a conjunctival autograft (CA) with or without the limbus and amniotic membrane has become a popular technique over recent years [9]. Nevertheless, in treating recurrent pterygium, recurrence rates remain high, ranging from 0 to 18.2 % when treated with limbal CA (LCAG) transplantation alone [4, 10–14] and from 9.5 to 37.5 % when treated with amniotic membrane graft (AMG) transplantation alone [15–18]. Recent studies [15, 17–22] have suggested that a combination therapy of intraoperative MMC and a graft is more successful for treating recurrent pterygium. However, the recurrent rates varied greatly in different reports of intraoperative MMC combined with a graft for treating recurrent pterygium. Moreover, the LCAG procedure can be vary technically demanding. Furthermore, no consensus exists regarding the use of a conjunctival graft for pterygium surgery, including the necessity of limbal transplantation [10, 23, 24] and the application of MMC [14, 19, 24, 25].
To date, no randomized clinical trial has been conducted regarding MMC with a graft for recurrent pterygium. To assess the effectiveness and complications of two combined approaches to treat recurrent pterygium, we designed a randomized trial of recurrent pterygium excision with intraoperative MMC application to compare LCAG with AMG.
Patients and methods
Study design
This prospective, randomized, and controlled study included patients who presented with one or two eye(s) with unilateral recurrent pterygium and were consecutively enrolled at the Cornea Division of the Zhongshan Ophthalmic Center. These eyes were randomly assigned to 2 treatment groups using a random number table via blocked randomization: the LCAG group received intraoperative 0.02 % MMC for 3 min plus LCAG transplantation, and the AMG group received intraoperative 0.02 % MMC for 3 min plus AMG transplantation. If both eyes were enrolled, then the eyes were separately randomized. This clinical trial was registered at http://www.clinicaltrials.gov (ClinicalTrials.gov identifier: NCT01319721). Informed consent was obtained from each participant after a thorough explanation of the procedures and its risk according to the Declaration of Helsinki. The medical ethics committee of Zhongshan Ophthalmic Center in Guangzhou also approved this study (No. 2012KYNL038).
Population
Recurrent pterygium was defined as an encroachment of fibrovascular tissue onto the cornea for any distance in the position of a previous pterygium. This condition was assessed using standardized photographs of the ocular surface, and was validated by an author. The inclusion criteria for patient selection were recurrent pterygium, age ranging from 18 to 80 years old, no ocular or systemic contraindications for surgery, and a willingness to participate in the study. Patients were excluded from this study if they presented with collagen vascular diseases or other autoimmune diseases, any evidence of stem cell deficiency, a known allergy to MMC, tobramycin, or dexamethasone, or glaucoma that might require future filtering surgery. Pregnant or lactating women were also excluded.
The required study sample size was determined based on the recurrence results reported by previous studies [18, 21]: 0 % for the LCAG group and 12.8 % for the AMG group. To achieve a confidence level of 95 % and a study power of 80 %, at least 86 eyes were needed. Taking into consideration an expected loss of 10 % of the patients due to follow-up, a minimum number of 96 eyes was required for this study. Thus, a sample size of 48 eyes per group was necessary.
The eyes with recurrent pterygium were allocated using a computer-generated randomization sequence with variable block sizes of four patients prepared by a biostatistician (Futian Luo). Allocation was concealed using sequentially numbered, sealed envelopes prepared by a research assistant not otherwise involved in the study.
Surgical procedure
Patient demographic data were documented preoperatively. Before surgery, patient clinical data were collected through detailed ophthalmic examinations that included noncontact tonometry, slit-lamp biomicroscopy, ophthalmoscopy, a measurement of eye-movement amplitude (EMA), and uncorrected distance visual acuity (UDVA). UDVA was measured using a Standard Logarithmic Visual Acuity Chart, and the results were converted to the logarithm of the minimal angle of resolution (logMAR) for analysis. The preoperative characteristics of the recurrent pterygium included the size of encroachment on the cornea and the degree of vascularization. The former was described as the pterygium region, including the length on the cornea and the limbal cord width (Fig. 1a). The latter was described as follows: grade 1, pale in color with mild vascularization; grade 2, intermediate red in color with marked vascularization; and grade 3, scarlet in color with marked vascularization [18].
The surgical procedure used was based on previous descriptions [26]. The same surgeon (Shiyou Zhou) performed all operations. After the administration of a local anesthetic, the recurrent pterygium head was first separated from the limbus and dissected toward the central cornea via a gentle scraping with a no. 15 Bard–Parker blade, keeping the plane of dissection as superficial as possible. Subconjunctival fibrovascular tissue was then excised extensively until reaching the margin of the caruncle, and scar tissue was dissected from the episclera and rectus muscle. After applying gentle cauterization to seal any bleeding vessels, a moist sponge with 0.02 % MMC (Kyowa®, Tokyo, Japan; 2 mg/vial) was applied to the bare sclera and the undersurface of the surrounding residual conjunctival bed for 3 min, and the eye was then washed with 150 ml of balanced salt solution.
In the LCAG group, a caliper was used to measure the area of the conjunctival defect. The intended graft area, which was 0.5 mm larger in all dimensions than the conjunctiva defect, was marked in the superotemporal zone with a gentian violet marking pen. Then, the graft was carefully dissected from the underlying Tenon’s tissue up to the limbus, including 0.5 mm of the peripheral corneal limbus, which was equal in arc length to the bared limbus. To help ensure correct tissue orientation, the free graft was spread out on the cornea and transferred to the scleral bed. The LCAG donor site was left alone with the Tenon’s tissue exposed. In the AMG group, cryopreserved amniotic membrane was prepared as previously described [27]. The graft was fashioned into pieces of similar size and shape as the bared scleral area and then used to cover the episclera and rectus muscle. At this stage, the grafts were sutured using interrupted 10-0 nylon sutures (Alcon®, Alcon Laboratories, Inc., Fort Worth, TX, USA), and the symblepharon was removed, resulting in the formation of the fornix. At the end of surgery, a 0.3 % tobramycin ointment (Tobrex®, Alcon, Couvreur, Belgium) was applied, and the eyes were patched for 1 day.
Starting on the first postoperative day, all eyes in both study groups received 0.5 % levofloxacin eye drops (Cravit®, Santen Pharmaceutical Co., Osaka, Japan) and 0.1 % sodium hyaluronate eye drops (Hialid®, Santen) during the day and 0.3 % tobramycin ophthalmic ointment (Tobrex®, Alcon, Couvreur, Belgium) at bedtime until the corneal epithelial defect healed. Both groups received 0.1 % pranoprofen ophthalmic solution (Pranopulin®, Sunju Pharmaceutical Co., Ltd., Japan) at the end of the first week. Cravit and Tobrex were then replaced with 0.3 % tobramycin/0.1 % dexamethasone eye drops and ointment (TobraDex®, Alcon, Couvreur, Belgium), respectively, and the frequency of TobraDex eye drops was tapered as follows: 6 times daily for 3 days, 4 times daily for 1 week, 3 times daily for 1 week, and twice daily for 2 weeks. The TobraDex eye drops and ointment were then stopped, together with Hialid and Pranopulin. The interrupted sutures were removed 2 weeks after surgery in both groups.
Postoperative follow-up and outcomes
The follow-up points were 1 day, 3 days, 14 days, 3 months, 6 months, and 12 months postoperatively. If the clinical course suggested any acute problems, the patients dropped out of the study and underwent supplementary follow-up visits. Patients who failed to return for the recommended follow-up appointments were telephoned to encourage compliance with follow-up. As with the preoperative assessment, ophthalmic examinations were performed to evaluate the postoperative outcomes.
Recurrence
According to the classification of Prabhasawat et al. [16], recurrence (grade D) was defined as the presence of fibrovascular tissue in the surgical area and invasion onto the cornea. The appearance of the surgical bed in successful cases was graded as follows: grade A was defined as the operated eye being indistinguishable from a normal eye, grade B was defined as the presence of fine episcleral vessels without fibrous tissue in the surgical area extending up to the limbus but not beyond, and grade C was defined as the presence of fibrovascular tissue in the surgical area but without invasion onto the cornea.
EMA
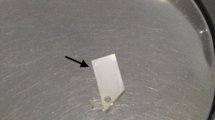
EMA was measured before and after surgery. As shown in Fig. 1, length I (Fig. 1b) was measured from the canthus to the corneal limbus using a millimeter rule while the participants gazed at a central fixed point, and length U (Fig. 1c) was measured whlie patients gazed to the opposite side of the pterygium site. Then, EMA was calculated by subtracting I from U. Concurrent symblepharon was also documented preoperatively.
Healing time of the corneal epithelial defect
Fluorescein staining is a method of visual observation (via a cobalt blue light) used to reveal the defect in the epithelial surface of the cornea postoperatively and the characteristic pattern of corneal re-epithelialization.
Conjunctival inflammation
Within 1 month after surgery, the presence of conjunctival inflammation around the surgical site was assessed and graded as 0 (none), i (mild), ii (moderate), or iii (severe) as described by Kheirkhah et al. [28].
Complications
From the time of informed consent to 12 months after surgery, standard ophthalmic examinations were performed to monitor adverse events, especially vision-threatening complications such as scleral thinning or ulceration, corneal perforation, iritis, cataract formation, and glaucoma. In addition, attention was paid to the risk of limbal damage at the donor site of the LCAG, and localized pannus formation or pseudopterygium was recorded.
Because the surgeon could not be blind to the results, another author (Rongxin Chen) confirmed all of the above outcomes during the follow-up period.
Statistical analyses
A statistician, Professor Futian Luo from the School of Public Health of Sun Yat-sen University, performed all of the statistical analyses using SPSS version 20 (IBM/SPSS Inc., Chicago, IL, USA). The mean ± standard deviation or frequency (percentage) was calculated for each parameter. Intergroup comparisons were performed using an independent-samples t-test, chi-square test, or Mann–Whitney U test. Within-group comparisons from the preoperative to the final postoperative visits were performed using a paired-sample t-test. Comparisons were 2-sided, and results were considered as significant when the p-value was 0.05 or less.
To avoid bias and ensure the comparability of the two treatment groups, the distributions of the baseline characteristics between the per-protocol population and the randomized population were compared.
Results
Patient characteristics
A total of 96 eyes (85 patients) were enrolled in this study between December 2010 and May 2013. To ensure that significant bias due to patient dropout did not exist, the baseline characteristics were compared between the per-protocol population and the randomized population. No significant differences were observed between these populations (each p > 0.05, Table 1). After the exclusion of three eyes from three patients who were lost to follow up (dropout rate = 3.1 %), the complete data for 93 eyes of 82 patients (37 men and 45 women) were obtained, including 11 patients with bilateral eyes with recurrent pterygium. These eyes were assigned to two different treatment groups for eight of these 11 patients, whereas the remaining three patients received the AMG group treatment for both eyes.
Of the patients who completed the follow-up assessment, 47 eyes and 46 eyes were assigned to the LCAG and AMG groups respectively. No significant differences were observed between the two groups in terms of sex, age, characteristics of recurrent pterygium, concurrent symblepharon, or number of previous excisions (each p > 0.05, Table 2).
Recurrence
At 12 months after treatment, one eye (2.1 %) in the LCAG group developed grade D recurrence, whereas five eyes (10.9 %) in the AMG group developed grade D recurrence; this difference was not significant (p = 0.196). However, the surgical site showed a better appearance in the LCAG group (Fig. 2a-d) than in the AMG group (Fig. 2e-l; p = 0.005, Table 3). In addition, the recurrences in both groups that had been noted 3 months postoperatively showed no progression at the 12-month follow-up assessment.
Preoperative appearance and grading of the surgical outcomes after MMC application with either LCAG or AMG. In the LCAG group, the eyes with recurrent pterygium (a) presented grade A with normal appearance (b) after surgery, whereas only one eye with recurrent pterygium involving the corneal stroma (c) showed grade D recurrence (d) postoperatively. In the AMG group, for recurrent pterygium (e), most of the eyes had grade A with attractive cosmetic appearance (f) postoperatively. After the removal of the recurrent pterygium (g, i) in the AMG group, the grade B appearance of fine episcleral vessels (h) and the grade C appearance of fibrovascular tissue in growth (j) in the excised area were observed. After surgery, the eyes with recurrent pterygium (k) also presented grade D recurrence (l)
Postoperative conjunctival inflammation
As Table 3 shows, no significant differences were observed between the two groups in terms of conjunctival inflammation around the surgical site at 1 month after surgery (p = 0.194).
Epithelial defect healing
No significant difference was observed with regard to the time for corneal epithelial defect healing between the LCAG (Fig. 3a-d) and AMG (Fig. 3e-h) groups (2.78 ± 0.73 days vs 3.23 ± 2.69 days, p = 0.500). Regardless of LCAG or AMG transplantation, the same healing process was shown for the corneal epithelial wounds in both groups (Fig. 3i-l) — specifically, epithelialization proceeded from the wounded margin of the corneal epithelium onto the corneal surface — moreover, the renewed epithelium covered the corneal defect earlier than the epithelium that covered the limbal defect. Furthermore, the re-epithelialization of the LCAG harvesting area and AMG surface were complete within 2 weeks.
The same pattern of re-epithelialization for corneal epithelium defect in eyes with LCAG or AMG transplantation. After surgery, epithelialization occurred in the LCAG group (a–d) from the defect edge of the preserved corneal epithelium to the epithelium defect, with the limbal region being the last to heal. The same healing process for the epithelial defect was observed in the AMG group (e–h). The schema (i–l) shows the same epithelial healing pattern for the two groups
EMA
Compared with the preoperative EMAs, postoperative ocular motility improved significantly, with EMAs of 8.35 ± 1.38 mm (vs 6.67 ± 1.84 mm; p < 0.001) and 7.85 ± 1.94 mm (vs 6.79 ± 2.01 mm; p = 0.001) in the LCAG and AMG groups respectively. No between-group differences were observed with regard to preoperative or postoperative EMA.
Visual acuity
UDVA significantly improved after treatment in both groups. The mean preoperative UDVAs were 0.28 ± 0.34 and 0.35 ± 0.45 in the LCAG group and AMG groups respectively, and no between-group difference was found (p = 0.512). Twelve months after treatment, the UDVA in both the LCAG and AMG groups improved significantly, to 0.15 ± 0.26 (p = 0.005) and 0.23 ± 0.48 (p = 0.012) respectively.
Postoperative complications
The frequency of postoperative complications was similar for the two groups (p = 0.236). Transient punctate epithelial keratitis (Fig. 4a, d), which was observed via fluorescein staining, appeared postoperatively in six eyes in each group. Local episcleral melting with graft melting presented in two eyes (Fig. 4b) in the LCAG group and one eye (Fig. 4e) in the AMG group. Local superficial melting resolved after the application of lubrication and a topical antibiotic for 2 weeks, and the use of Pranopulin and TobraDex was stopped. Localized pannus formation at the donor site of the LCAG was noted in five eyes in the LCAG group (Fig. 4c), but this change was limited to the donor site, with no progression over the cornea during the 12-month follow-up period. In the AMG group, the delayed healing of a corneal epithelial defect occurred in one eye (Fig. 4f) in which more than one-fourth of the limbus was involved in recurrent pterygium. The corneal wound defect was re-epithelialized after the application of a bandage contact lens.
Complications in eyes with intraoperative MMC followed by LCAG or AMG transplantation. Six eyes exhibited superficial punctuate epithelial defects in both groups (a–d). Episcleral melting developed in two eyes in the LCAG group (b) and in one eye in the AMG group (e). Localized pannus formation at the donor site of LCAG was observed in five eyes in the LCAG group (c). Delayed corneal epithelialization was noted in one eye in the AMG group (f)
Discussion
Recurrent pterygium presents a significant surgical problem. Conjunctival shortening or the symblepharon caused by multiple surgeries is especially challenging. The major difficulty in recurrent pterygium treatment is the high rate of recurrence. The complete removal of the subconjunctival fibrovascular tissue and fibroblast cells is almost impossible, especially in cases of recurrent pterygium. Although there is consensus that intraoperative MMC or graft coverage of bare sclera helps to prevent the recurrence of pterygium [9], controversy remains with regard to the most appropriate study size and graft composition. This controversy is partially because of the unresolved histological pathophysiology of pterygium. The CA with limbus seems to yield better results than the bulbar CA [23, 24], whereas the recurrence rate under AMG was similar to that under LCAG [29]. To achieve a lower incidence of recurrence, the current study evaluated the efficacy and safety of an intraoperative MMC application combined with LCAG or AMG transplantation to treat recurrent pterygium.
During a 12-month follow-up assessment after surgery with an MMC application, the current study had total recurrence rates of 2.1 and 10.9 % associated with the LCAG and AMG groups respectively. When each procedure was considered separately, these results were comparable with those of previous studies. A previous report found recurrence rates ranging from 0 to 18.2 % for free LCAG transplantation [4, 10–14] and from 9.5 to 37.5 % for AMG transplantation to treat recurrent pterygium without the application of MMC [16–18]. Few studies have used adjunctive MMC for surgery with LCAG to treat recurrent pterygium or have compared this protocol with other techniques. Nabawi et al. [21] applied intraoperative MMC for 3 min combined with LCAG, and did not find any recurrence 18 months later in 34 eyes with recurrent pterygium surgery. Moreover, Fakhry [19] showed that the preoperative injection of MMC before LCAG resulted in significantly less recurrence than LCAG alone. Therefore, the additive effects of combined use appear to effectively reduce recurrence rates to treat recurrent pterygium, and might be one of the reasons for the relatively low recurrence rates in both groups.
After the removal of pterygium, the rationale for using intraoperative MMC is that it inhibits the replication of DNA during mitosis, and slows fibrovascular tissue regrowth. The advantages of this approach are its relatively low cost and technical ease. Disadvantages are rare; however, devastating complications including scleral ulceration and necrosis, secondary glaucoma, corneal perforation, cataract formation, iritis, and irreversible damage to stem cells can occur. As in our study and based on the reported data [9], intraoperative 0.02 % MMC was applied for 3 min to reduce the recurrence of pterygium and avoid complications. According to previous reports [7, 18], the recurrence rate after intraoperative MMC was applied only on the bared sclera ranged from 12.5 to 19.2 %. The various rates of recurrence after MMC application have been attributed to the concentration and patching time of the MMC cotton applicator, as well as to the surgical technique. In addition to intraoperative MMC, this study used LCAG or AMG to evaluate whether the combination of these treatments further reduced the recurrence rate of recurrent pterygium. The addition of AMG or LCAG to MMC might also enable ocular surface reconstruction, even after extensive fibrovascular tissue removal.
Although different studies have adopted various definitions of pterygium recurrence, the current study used a previously reported grading system [16]. According to this grading system, grades B and C presented in two eyes and two eyes respectively of the AMG group, but in no eyes of the LCAG group. We concluded that MMC combined with LCAG to treat recurrent pterygium resulted in a better cosmetic appearance, in accordance with a previous study by Hirst et al. [26]. However, in the current randomized study, one of 47 eyes experienced corneal recurrence (grade D appearance) 12 months after the intraoperative application of 0.02 % MMC for 3 min combined with LCAG transplantation, whereas 5 of 46 eyes showed recurrence in the AMG group, without a significant between-group difference. Previously, Kheirkhah et al. [24] studied the outcomes of pterygium surgery with MMC application using CA versus LCAG. With a minimum follow-up time of 12 months, one of 31 eyes (3.2 %) with primary pterygium and one of eight eyes (12.5 %) with recurrent pterygium in the CA group showed true corneal recurrence. No eye in the LCAG group developed recurrence. No significant differences in recurrence rates were observed between the CA and LCAG groups, or between the primary and recurrent subgroups. Although the AMG cannot provide stem cells, it can provide a basement membrane substrate that facilitates the migration of epithelial cells. Furthermore, it has anti-inflammatory properties, which serve to decrease angiogenesis and fibroblastic activities [30]. Katircioglu et al. [31] reported that AMG combined with MMC has a similar recurrence rate (8 %) compared with CA combined with MMC, probably because of the favorable effects of decreased angiogenesis and fibroblastic activities. In accordance with these studies, no significant between-group differences in recurrence rates were observed in the present study; however, these results might well be related to the relatively low number of patients.
Furthermore, this comparative study did not find an additional effect of intraoperative MMC application with either LCAG or AMG transplantation with regard to recurrent pterygium surgery. Although recurrence of this disease is multifactorial, there were no significant differences in sex distribution, average age, or size, side, or degree of vascularization of pterygium before surgery between the two groups. In addition to the dose and time of MMC application and the type of surgical technique, early postoperative inflammation stimulated by sutures might be associated with recurrence, as it is more commonly observed following suture surgery than following fibrin adhesive surgery [32].
In addition to the lack of significant superiority to prevent pterygium recurrence, LCAG is more time-consuming and requires greater surgical expertise to harvest the limbal tissue. Moreover, pannus formation developed at the area of the donor limbus in five eyes (10.6 %) in the LCAG group, which is similar to the incidence rate of 12.8 % reported by Kheirkhah et al. [24]. Although an impression cytologic analysis was not performed in our study, this pannus formation might be explained by focal limbal stem cell deficiency previously reported in the donor limbus [12, 33]. Although the pannus remained confined within the area of limbal resection without additional progression, this condition might compromise future responses of the limbal stem cell reserve to additional stress. Additional research is needed to evaluate the incidence of limbal stem cell deficiency at the donor site of LCAG and its effect on ocular surface health.
Traditionally, the corneal limbus is thought to be a stem cell supplier of the corneal epithelium; given that the delayed healing of the corneal wound presented in one eye with limbal large involvement in the AMG group, this relationship might also be because of the intraoperative MMC application [9].
Beyond the application of intraoperative MMC or a graft, the degree of conjunctival inflammation might affect the outcome of recurrent pterygium surgery, as the results for primary pterygium surgery suggested. Previous studies reported persistent conjunctival inflammation around the surgical site after pterygium surgery in 15 % of patients who underwent CA transplantation [34] and in 31.5 to 40.7 % of eyes that received an AMG [17, 28]. Under postoperative treatment with Pranopulin and TobraDex, no significant between-group difference was observed in the distribution of eyes with conjunctival inflammation, and the improvement of EMA was equal in both groups. Therefore, the treatment of postoperative inflammation probably played a role in pterygium recurrence.
Moreover, no significant between-group difference was found in terms of the duration of corneal epithelial wound healing in this study. The healing pattern in both groups was similar to a previous description [35], in which the corneal epithelial defect was covered by the regenerated corneal epithelium from the junction of the defect and healthy epithelium, toward the center of the epithelial defect, and finally to the excised limbal area. This finding conflicts with the healing pattern of limbal transplantation for people with limbal stem cell deficiency, in which the defective corneal epithelium is covered by the proliferation and differentiation of stem cells residing in the transplanted limbus [36]. Our study implies that the transplanted limbal tissue that was included in LCAG does not supply the corneal epithelium during the stage of epithelial wound healing; rather, it corrects limbal dysfunction by acting as a barrier against the invasion of subconjunctival fibrovascular tissue.
Although many surgeons currently favor some form of cover for the bare sclera followed by intraoperative MMC, as well as the closure of the conjunctiva to prevent complications, three eyes were noted with graft melting and subsequent surgical episcleral melting in this study. Episcleritis commonly recurs and can spread to the sclera, leading to scleral necrosis that may progress to melting or perforation of the sclera [37]. Nonetheless, our patients were all healthy, without conditions predisposing to ulceration or poor wound healing, such as collagen vascular disease or autoimmune diseases. We suspect that such complications might be related to the intraoperative use of MMC [38] and excessive cautery with the avascular bed [39]. Moreover, punctate epithelial keratitis was noted in 12 eyes. After the appropriate pharmaceutical treatment adjustment, these minor complications did not influence the patients’ vision as reported by Young et al. [25]. Therefore, the intraoperative use of topical MMC is without risk or need for concern.
This study was prospective and randomized, and no significant difference was found between the two groups with regard to treating recurrent pterygium. Furthermore, this study was performed with a large sample size. In addition, the postoperative follow-up assessment in all cases was 12 months, which was long enough to evaluate pterygium recurrence [40]. However, a longer follow-up period is needed to observe the late complications of MMC, which can include necrotizing scleritis, corneal perforation and scleral calcification. Moreover, different recurrence rates (2.1 % vs 10.9 %) are often found between the two groups. Because the sample size affects statistical power, more patients should be enrolled in order to compare the two treatments in future studies.
References
Hirst LW (2003) The treatment of pterygium. Surv Ophthalmol 48:145–180. doi:10.1016/S0039-6257(02)00463-0
Shimazaki J, Shinozaki N, Tsubota K (1998) Transplantation of amniotic membrane and limbal autograft for patients with recurrent pterygium associated with symblepharon. Br J Ophthalmol 82:235–240. doi:10.1136/bjo.82.3.235
Shimazaki J, Kosaka K, Shimmura S, Tsubota K (2003) Amniotic membrane transplantation with conjunctival autograft for recurrent pterygium. Ophthalmology 110:119–124. doi:10.1016/S0161-6420(02)01453-7
Dekaris I, Gabrić N, Karaman Z, Mravicić I, Kastelan S (2002) Limbal-conjunctival autograft transplantation for recurrent pterygium. Eur J Ophthalmol 12:177–182
Tan DT, Chee SP, Dear KB, Lim AS (1997) Effect of pterygium morphology on pterygium recurrence in a controlled trial comparing conjunctival autografting with bare sclera excision. Arch Ophthalmol 115:1235–1240. doi:10.1001/archopht.1997.01100160405001
Verma N, Garap JA, Maris R, Kerek A (1998) Intraoperative use of mitomycin C in the treatment of recurrent pterygium. P N G Med J 41:37–42
Mastropasqua L, Carpineto P, Ciancaglini M, Enrico Gallenga P (1996) Long term results of intraoperative mitomycin C in the treatment of recurrent pterygium. Br J Ophthalmol 80:288–291. doi:10.1136/bjo.80.4.288
Lam DS, Wong AK, Fan DS, Chew S, Kwok PS, Tso MO (1998) Intraoperative mitomycin C to prevent recurrence of pterygium after excision: a 30-month follow-up study. Ophthalmology 105:901–904. doi:10.1016/S0161-6420(98)95034-5 [Discussion:904–905]
Kaufman SC, Jacobs DS, Lee WB, Deng SX, Rosenblatt MI, Shtein RM (2013) Options and adjuvants in surgery for pterygium: a report by the American Academy of Ophthalmology. Ophthalmology 120:201–208. doi:10.1016/j.ophtha.2012.06.066
Al Fayez MF (2002) Limbal versus conjunctival autograft transplantation for advanced and recurrent pterygium. Ophthalmology 109:1752–1755. doi:10.1016/S0161-6420(02)01160-0
Dekaris I, Gabrić N, Karaman Z, Mravicić I, Kastelan S, Spoljarić N (2001) Pterygium treatment with limbal-conjunctival autograft transplantation. Coll Anthropol 25(Suppl):7–12
Gris O, Güell JL, del Campo Z (2000) Limbal–conjunctival autograft transplantation for the treatment of recurrent pterygium. Ophthalmology 107:270–273. doi:10.1016/S0161-6420(99)00041-X
Rao SK, Lekha T, Mukesh BN, Sitalakshmi G, Padmanabhan P (1998) Conjunctival–limbal autografts for primary and recurrent pterygia: technique and results. Indian J Ophthalmol 46:203–209
Mutlu FM, Sobaci G, Tatar T, Yildirim E (1999) A comparative study of recurrent pterygium surgery: limbal conjunctival autograft transplantation versus mitomycin C with conjunctival flap. Ophthalmology 106:817–821. doi:10.1016/S0161-6420(99)90172-0
Salman AG, Mansour DE (2011) The recurrence of pterygium after different modalities of surgical treatment. Saudi J Ophthalmol 25:411–415. doi:10.1016/j.sjopt.2010.10.013
Prabhasawat P, Barton K, Burkett G, Tseng SC (1997) Comparison of conjunctival autografts, amniotic membrane grafts, and primary closure for pterygium excision. Ophthalmology 104:974–985. doi:10.1016/S0161-6420(97)30197-3
Solomon A, Pires RT, Tseng SC (2001) Amniotic membrane transplantation after extensive removal of primary and recurrent pterygia. Ophthalmology 108:449–460. doi:10.1016/S0161-6420(00)00567-4
Ma DH, See LC, Hwang YS, Wang SF (2005) Comparison of amniotic membrane graft alone or combined with intraoperative mitomycin C to prevent recurrence after excision of recurrent pterygia. Cornea 24:141–150. doi:10.1097/01.ico.0000141237.71837.d8
Fakhry MA (2011) The use of mitomycin C with autologous limbal-conjunctival autograft transplantation for management of recurrent pterygium. Clin Ophthalmol 5:123–127. doi:10.2147/OPTH.S16474
Yao Y-F, Qiu W-Y, Zhang Y-M, Tseng SC (2006) Mitomycin C, amniotic membrane transplantation and limbal conjunctival autograft for treating multirecurrent pterygia with symblepharon and motility restriction. Graefes Arch Clin Exp Ophthalmol 244:232–236. doi:10.1007/s00417-005-0010-y
Nabawi KS, Ghonim MA, Ali MH (2003) Evaluation of limbal conjunctival autograft and low-dose mitomycin C in the treatment of recurrent pterygium. Ophthalmic Surg Lasers Imaging 34:193–196
Katircioğlu YA, Altiparmak UE, Duman S (2007) Comparison of three methods for the treatment of pterygium: amniotic membrane graft, conjunctival autograft and conjunctival autograft plus mitomycin C. Orbit 26:5–13. doi:10.1080/01676830600972724
Zheng K, Cai J, Jhanji V, Chen H (2012) Comparison of pterygium recurrence rates after limbal conjunctival autograft transplantation and other techniques: meta-analysis. Cornea 31:1422–1427. doi:10.1097/ICO.0b013e31823cbecb
Kheirkhah A, Hashemi H, Adelpour M, Nikdel M, Rajabi MB, Behrouz MJ (2012) Randomized trial of pterygium surgery with mitomycin C application using conjunctival autograft versus conjunctival-limbal autograft. Ophthalmology 119:227–232. doi:10.1016/j.ophtha.2011.08.002
Young AL, Ho M, Jhanji V, Cheng LL (2013) Ten-year results of a randomized controlled trial comparing 0.02% mitomycin C and limbal conjunctival autograft in pterygium surgery. Ophthalmology 120:2390–2395. doi:10.1016/j.ophtha.2013.05.033
Hirst LW (2009) Recurrent pterygium surgery using pterygium extended removal followed by extended conjunctival transplant: recurrence rate and cosmesis. Ophthalmology 116:1278–1286. doi:10.1016/j.ophtha.2009.01.044
Zhou S, Chen J, Feng J (2003) The effects of amniotic membrane on polymorphonuclear cells. Chin Med J (Engl) 116:788–790
Kheirkhah A, Casas V, Sheha H, Raju VK, Tseng SC (2008) Role of conjunctival inflammation in surgical outcome after amniotic membrane transplantation with or without fibrin glue for pterygium. Cornea 27:56–63. doi:10.1097/ICO.0b013e31815873da
Wei S, Chan L, Cui Y (2005) Limbal epithelial autograft and amniotic membrane transplantation for pterygium in 107 cases. Int J Ophthalmol 5:583–585
Sippel KC, Ma JJ, Foster CS (2001) Amniotic membrane surgery. Curr Opin Ophthalmol 12:269–281. doi:10.1097/00055735-200108000-00006
Katırcıoglu YA, Altiparmak U, Engur Goktas S, Cakir B, Singar E, Ornek F (2015) Comparison of two techniques for the treatment of recurrent pterygium: amniotic membrane vs conjunctival autograft combined with mitomycin C. Semin Ophthalmol 30:321–327. doi:10.3109/08820538.2013.874468
Ratnalingam V, Eu AL, Ng GL, Taharin R, John E (2010) Fibrin adhesive is better than sutures in pterygium surgery. Cornea 29:485–489. doi:10.1097/ICO.0b013e3181c29696
Sridhar MS, Vemuganti GK, Bansal AK, Rao GN (2001) Impression cytology-proven corneal stem cell deficiency in patients after surgeries involving the limbus. Cornea 20:145–148. doi:10.1097/00003226-200103000-00005
Kheirkhah A, Nazari R, Nikdel M, Ghassemi H, Hashemi H, Behrouz MJ (2011) Postoperative conjunctival inflammation after pterygium surgery with amniotic membrane transplantation versus conjunctival autograft. Am J Ophthalmol 152:733–738. doi:10.1016/j.ajo.2011.04.013
Dua HS (1998) The conjunctiva in corneal epithelial wound healing. Br J Ophthalmol 82:1407–1411. doi:10.1136/bjo.82.12.1407
Dua HS, Azuara-Blanco A (2000) Autologous limbal transplantation in patients with unilateral corneal stem cell deficiency. Br J Ophthalmol 84:273–278. doi:10.1136/bjo.84.3.273
McCluskey P, Powell RJ (2004) The eye in systemic inflammatory diseases. Lancet 364(9451):2125–2133. doi:10.1016/S0140-6736(04)17554-5
Tsai YY, Lin JM, Shy JD (2002) Acute scleral thinning after pterygium excision with intraoperative mitomycin C: a case report of scleral dellen after bare sclera technique and review of the literature. Cornea 21:227–229. doi:10.1097/00003226-200203000-00022
Karalezli A, Kucukerdonmez C, Borazan M, Akova YA (2010) Successful treatment of necrotizing scleritis after conjunctival autografting for pterygium with amniotic membrane transplantation. Orbit 29:88–90. doi:10.3109/01676830903297563
Hirst LW, Sebban A, Chant D (1994) Pterygium recurrence time. Ophthalmology 101:755–758. doi:10.1016/S0161-6420(94)31270-X
Acknowledgments
The study was supported in part by “Sun Yat-Sen University Clinical Research 5010 Program” in China (grant number: 2014015). This funding organization played no role in the design or performance of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The “Sun Yat-Sen University Clinical Research 5010 Program” in China (grant number: 2014015) funded this study.
Conflict of interest
The authors declare no financial or non-financial conflicts of interest. The authors had full control over the primary data, and they agree to allow Graefe’s Archive for Clinical and Experimental Ophthalmology to review their data upon request.
Ethical approval
All of the procedures performed in studies involving human participants were conducted in accordance with the ethical standards of the institutional and/or national research committees and in light of the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all participants included in this study.
Additional information
This study was registered at http://www.clinicaltrials.gov (ClinicalTrials.gov identifier: NCT01319721).
Rongxin Chen, Guofu Huang, and Shu Liu contributed equally to this work.
Rights and permissions
About this article
Cite this article
Chen, R., Huang, G., Liu, S. et al. Limbal conjunctival versus amniotic membrane in the intraoperative application of mitomycin C for recurrent pterygium: a randomized controlled trial. Graefes Arch Clin Exp Ophthalmol 255, 375–385 (2017). https://doi.org/10.1007/s00417-016-3509-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-016-3509-5