Abstract
Background
To determine the applicability of the ISNT (inferior>superior>nasal>temporal) and IST (inferior>superior>temporal) rules on retinal nerve fiber layer (RNFL) measurement on spectral-domain optical coherence tomography (SD-OCT) in normal children.
Methods
A prospective, cross-sectional study including consecutive subjects between the ages of 5–18 years who were born at term (≥37 weeks gestational age) and with a normal birth weight (≥2500 g) presenting to the out-patient department for refractive error examination. RNFL measurement was done on Spectralis SD-OCT. Exclusion criteria were best-corrected visual acuity less than 20/20, spherical equivalent (SE) > ± 5 diopter (D), applanation IOP >21 mmHg, cup-to-disc (C/D) ratio of >0.5, C/D ratio asymmetry of >0.2 between eyes and any retinal or optic disc anomaly as determined by mydriatic fundus examination. Subjects with amblyopia, strabismus, or family history of optic nerve or retinal disease were excluded. Poor cooperation for SDOCT imaging and lack of consent were other exclusion criteria.
Results
The ISNT rule on the RNFL was followed only by 30 eyes (23.8 %), while the IST rule was followed by 66 eyes (52.4 %) (p < 0.001). The superior RNFL was thicker than the inferior in 57 eyes (45.2 %) while the temporal RNFL was thicker than the nasal in 63 eyes (50 %). The age, gender, spherical equivalent, and disc size did not predict the followability of the ISNT and IST rules (p > 0.05).
Conclusions
The ISNT and the IST rules for RNFL are not universally followed by all normal eyes in children. All deviations should therefore not be considered pathological.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Glaucoma is characterized by a progressive degeneration of the retinal ganglion cells (RGCs) and their axons, leading to a reduction in the thickness of the retinal nerve fiber layer (RNFL) [1]. The RNFL forms the neuroretinal rim (NRR) as it leaves the eye in the form of the optic nerve. Jonas et al. [2] showed on disc photographs that the normal NRR follows a typical configuration in which the inferior NRR is the thickest, followed by the superior, nasal, and the temporal (ISNT rule), which is violated in glaucoma. Optical coherence tomography (OCT) has been widely used for diagnosis and follow-up of optic nerve and retinal disorders in children [3–5]. It allows objective measurement of the optic nerve head (ONH), retinal nerve fiber layer (RNFL) and macular thickness in a non-invasive manner [6]. Spectral-domain OCT (SD-OCT) is a further refinement of this technique which allows imaging with a faster scan rate and at a higher resolution [7, 8]. One important limitation for application of SD-OCT to children is the fact that a robust normative database does not exist for an age of less than 18 years. However, there have been some studies recently on deriving the normative for SD-OCT in children [9–14]. The applicability of the NRR rules in children has been tested before [15]. However, there are no studies that look into whether the classical ISNT (inferior>superior>nasal>temporal) rule is applicable to the RNFL in normal children on SD-OCT. Since the nasal rim is last to be affected in diseases such as glaucoma [16], we also tested the applicability of the IST rule (inferior>superior>temporal) on the RNFL. The purpose of the present study was to investigate the applicability of these rules on the RNFL measurement in normal children.
Methods
This was a prospective, cross-sectional study conducted at a tertiary care ophthalmic institute between January 2014 and June 2014. Consecutive subjects between the ages of 5–18 years who were born at term (≥37 weeks gestational age) and with a normal birth weight (≥2500 g) presenting to the out-patient department for refractive error examination were included in the study. A verbal consent was obtained from all subjects. An informed consent was obtained from the legal guardian of each participant. Additional written consent was obtained from all children who were at least 12 years old. The study protocol was prospectively approved by the institutional review board and health research ethics committee (Dr. TV Patel Eye Institute Ethics Committee).
The subjects underwent a full ophthalmic examination, including best-corrected visual acuity tested with age appropriate charts, cycloplegic refraction with cyclopentolate 1 % eye drops, intraocular pressure (IOP) measurement with Goldmann applanation tonometry (GAT), slit-lamp biomicroscopy, and fundus examination with indirect ophthalmoscopy. The OCT scanning for RNFL thickness was done using Spectralis OCT (Heidelberg Engineering, Carlsbad, CA, USA). All patient examination was performed by one of the authors (PD).
Exclusion criteria were best-corrected visual acuity less than 20/20, spherical equivalent (SE) > ± 5 diopter (D), applanation IOP >21 mmHg, cup to disc (C/D) ratio of >0.5, C/D ratio asymmetry of >0.2 between eyes, and any retinal or optic disc anomaly as determined by mydriatic fundus examination. Subjects with history of ocular abnormalities including amblyopia, strabismus, or family history of optic nerve or retinal disease were excluded.
In addition, children who could not cooperate for the SD-OCT examination or whose parents did not provide consent were also excluded from the study.
OCT measurements
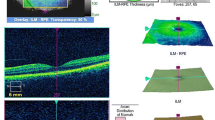
All images were acquired with the Spectralis SD-OCT (version 5.6.1) after pupillary dilation. The instrument has a scan speed of 40,000 A-scans per second, with a 12-degree diameter scan circle around the optic nerve. The scan circle diameter (mm) depends on the axial eye length of the eye, which is typically 3.5 to 3.6 mm. TruTrack image alignment software tracks for eye movement, and provides the ability to obtain multiple images from the exact same location.
All images were centered on the optic disc at the time of acquisition, and had a quality score of >25. Peripapillary RNFL thickness values were noted for the 4 quadrants: superior, temporal, inferior, and nasal (Fig. 1). The maximum vertical disc size was noted using the measuring tool on the Spectralis SD-OCT.
Statistical analysis
Descriptive and inferential statistics were performed using STATA version 12 for Windows (StataCorp LP, College Station, TX, USA). A p value <0.05 was considered statistically significant. Chi-square test was done to determine whether the difference in the followability of ISNT and IST rules was significant. Logistic regression analysis was done to see the effect of age, gender, SE, and disc size on the followability of the ISNT and IST rules.
Results
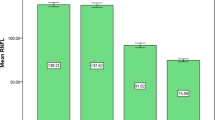
A total of 135 subjects were initially included. Nine subjects were unable to undergo SD-OCT imaging due to poor cooperation, and were excluded. Finally, 126 subjects completed the study. One eye of each subject was randomly selected for analysis by a random number table. This included 60 males and 66 females. The mean age of the participants was 11.42 ± 3.59 years with a mean SE of −0.4 ± 1.4 D. The age distribution of the participants is shown in Fig. 2. The mean GAT-measured IOP was 13.3 ± 1.9 mmHg. The average vertical disc size and RNFL thickness were 1.7 ± 0.6 mm and 100.3 ± 8.3 microns respectively. Table 1 summarizes the patient demographics and RNFL measurements in all the 4 quadrants. The ISNT rule on the RNFL was followed only by 30 eyes (23.8 %), while the IST rule was followed by 66 eyes (52.4 %) (p < 0.001) (Table 2). The superior RNFL was thicker than the inferior in 57 eyes (45.2 %) while the temporal RNFL was thicker than the nasal in 63 eyes (50 %). The age, gender, SE, and disc size did not predict the followability of the ISNT and IST rules on logistic regression analysis (p > 0.05).
Discussion
Subjective tools for evaluation of optic nerve function such as the visual field examination in the pediatric population is difficult because of the lack of comprehension of the testing methodology, rapid boredom, distraction, and fatigue. There is a dire need for tools aiding objective assessment in this age group that are quick, reliable, reproducible, and less invasive. SD-OCT is one such diagnostic tool for assessing the RNFL. The reproducibility for SD-OCT has already been established [17]. Serial changes in the OCT measurements may be an early sign of a disease. Knowledge of normal RNFL distribution pattern is therefore essential to avoid confusion with physiological variations. To the best of our knowledge, this is the first report on the applicability of NRR rules on the RNFL in children measured by SD-OCT.
The average RNFL measured in our study was 100.3 ± 8.3 microns. This is similar to what is reported by other studies [10, 11]. The average quadrant-wise RNFL thickness reported in studies have shown great variation as regards to following the ISNT rule with a number of reports demonstrating exceptions [11, 13, 18–22]. Though the average-quadrant-wise RNFL thickness values in our study followed the ISNT rule, it was not so for the individual eyes. The ISNT rule on the RNFL was followed only by 30 eyes (23.8 %). These results are in contradiction to another study where the ISNT rule on the NRR was followed in 30 eyes (56 %) of children between 5 and 16 years of age [15]. However, this study was done on Heidelberg retinal tomography, and hence cannot be directly compared to the results of our study. Hwang et al. [23] studied the neuroretinal rim thickness on SD-OCT in adults and found that the ISNT rule was applicable only in 10/80 normal eyes (13 %). Another study by Pradhan et al. [24] showed that the ISNT rule on the RNFL in normal adults was followed by 89/189 (47.1 %) of the normal eyes. This study was however done on a Stratus time-domain OCT. The IST rule was better followed in our study with 66 eyes (52.4 %) obeying it. Similar results have also been found in adults by Pradhan et al., who demonstrated an increase in the followability of the IST rule as compared to the ISNT rule on the RNFL (58.7 % vs 47.1 % respectively). Rao et al. [11] in their study on Indian eyes showed that their average superior quadrant RNFL measurements were greater than the inferior. A similar paradox was also seen in the average nasal and temporal RNFL measurements, where the thickness in the temporal quadrant was more than the nasal. Leung at al. [22] also found that the average RNFL thickness in their study reduced from superior to inferior to temporal to nasal quadrants. In our study, the superior RNFL was thicker than the inferior in 57 eyes (45.2 %), while the temporal RNFL was thicker than the nasal in 63 eyes (50 %). Three eyes in our cohort had a temporal RNFL thickness greater than the superior. The RNFL thickness in all these three eyes reduced from inferior to temporal to superior to nasal quadrants. However, the difference between the temporal and superior RNFL thickness in all three eyes was modest, with a maximum difference of only 4 microns.
Logistic regression analysis in our study showed that the followability of the ISNT and IST rules were not affected by age, gender, SE or disc size (p > 0.05). Alamouti et al. [25] studied the variation in the rate of RNFL decrease with age. They suggested that the reduction is slower in the younger age group which was the case in our study. Previous studies have found no relation of gender with the RNFL thickness [18, 21]. Salchow et al. [18] have shown an increase in the RNFL thickness with increase in hyperopia. Cheung et al. [26] similarly demonstrated a thinning of the RNFL with increased severity of myopia. We included only those children with SE within ±5 D. This would have eliminated high myopes and hyperopes in our study, thereby negating their effect on the measured RNFL thickness. All this explains why age, gender, and SE were not a significant predictor for followability of the ISNT and IST rules in our study. Though the Spectralis OCT scan diameter depends on the axial length, for a typical eye it is 3.5–3.6 mm in diameter. The optic disc size can influence the RNFL measurements, with a reduction in the measured RNFL thickness shown with increasing distance from the disc margin [27]. However, the potential error arising from it would likely affect the RNFL measurements in all quadrants, and therefore would not have changed the followability of the ISNT and IST rules in our study. Another study has shown that ISNT rule is increasingly not followed in large pediatric optic discs [28]. The average vertical disc size was 1.7 ± 0.6 mm (range, 1.35–2.00 mm) in our study. It is perhaps because of the absence of large discs in our cohort that the disc size did not significantly predict the followability of the ISNT and IST rules in this study (p > 0.05). Our study is also limited by the fact that it involved Indian eyes only. Alasil et al. [29] have shown that racial differences exist while measuring the RNFL on SD-OCT. They reported thinner RNFL thickness values in Caucasians compared to Hispanics and Asians. Hence, the results of our study may not be applicable to a population with different ethnicities.
To conclude, the ISNT and the IST rules for RNFL are not universally followed by all normal eyes in children. All deviations should therefore not be considered pathological.
References
Ajtony C, Balla Z, Somoskeoy S, Kovacs B (2007) Relationship between visual field sensitivity and retinal nerve fiber layer thickness as measured by optical coherence tomography. Invest Ophthalmol Vis Sci 48(1):258–263
Jonas JB, Gusek GC, Naumann GOH (1998) Optic disc, cup and neuroretinal rim size, configuration, and correlations in normal eyes. Invest Ophthalmol Vis Sci 29:1151–1158
Nadeau S, Gire J, Coste R, Cornand E, Denis E (2010) Papillary retinal nerve fiber layer thickness measurement using optical coherence tomography in children with ocular hypertension and juvenile glaucoma. J Fr Ophtalmol 33(4):249–257
Baker PS, Tasman W (2010) Optical coherence tomography imaging of the fovea in retinopathy of prematurity. Ophthalmic Surg Lasers Imaging 41(2):201–206
Chang L, El-Dairi MA, Frempong TA, Burner EL, Bhatti MT, Young TL, Leigh F (2010) Optical coherence tomography in the evaluation of neurofibromatosis type-1 subjects with optic pathway gliomas. J AAPOS 14(6):511–517
Medeiros FA, Zangwill LM, Bowd C, Vessani RM, Susanna R Jr, Weinreb RN (2005) Evaluation of retinal nerve fiber layer, optic nerve head, and macular thickness measurements for glaucoma detection using optical coherence tomography. Am J Ophthalmol 139(1):44–55
Nassif N, Cense B, Park B, Pierce M, Yun S, Bouma B, Tearney G, Chen T, de Boer J (2004) In vivo high-resolution video-rate spectral-domain optical coherence tomography of the human retina and optic nerve. Opt Express 12(3):367–376
Wojtkowski M, Srinivasan V, Ko T, Fujimoto J, Kowalczyk A, Duker J (2004) Ultrahigh-resolution, high-speed, Fourier domain optical coherence tomography and methods for dispersion compensation. Opt Express 12(11):2404–2422
Yanni SE, Wang J, Cheng CS, Locke KI, Wen Y, Birch DG, Birch EE (2013) Normative reference ranges for the retinal nerve fiber layer, macula, and retinal layer thicknesses in children. Am J Ophthalmol 155:354–360
Zhu BD, Li SM, Li H, Liu LR, Wang Y, Yang Z, Li SY, Kang MT, Fu J, Qi YH, Zhan SY, Wang N, Anyang Childhood Eye Study Group (2013) Retinal nerve fiber layer thickness in a population of 12-year-old children in central China measured by iVue-100 spectral-domain optical coherence tomography: the Anyang Childhood Eye Study. Invest Ophthalmol Vis Sci 54:8104–8111
Rao A, Sahoo B, Kumar M, Varshney G, Kumar R (2013) Retinal nerve fiber layer thickness in children <18 years by spectral-domain optical coherence tomography. Semin Ophthalmol 28(2):97–102
Turk A, Ceylan OM, Arici C, Keskin S, Erdurman C, Durukan AH, Mutlu FM, Altinsoy HI (2012) Evaluation of the nerve fiber layer and macula in the eyes of healthy children using spectral-domain optical coherence tomography. Am J Ophthalmol 153:552–559
Tsai DC, Huang N, Hwu JJ, Jueng RN, Chou P (2012) Estimating retinal nerve fiber layer thickness in normal schoolchildren with spectral-domain optical coherence tomography. Jpn J Ophthalmol 56(4):362–370
Al-Haddad C, Barikian A, Jaroudi M, Massoud V, Tamim H, Noureddin B (2014) Spectral domain optical coherence tomography in children: normative data and biometric correlations. BMC Ophthalmol 14:53
Larsson E, Nuija E, Alm A (2011) The optic nerve head assessed with HRT in 5–16-year-old normal children: normal values, repeatability and interocular difference. Acta Ophthalmol 89:755–758
Jonas JB, Burde WM (2002) Is the nasal optic disc sector important for morphometric glaucoma diagnosis? Br J Ophthalmol 86:1232–1235
Altemir I, Pueyo V, Elía N, Polo V, Larrosa JM, Oros D (2013) Reproducibility of optical coherence tomography measurements in children. Am J Ophthalmol 155:171–176.e1
Salchow DJ, Oleynikov YS, Chiang MF, Kennedy-Salchow SE, Langton K, Tsai JC, Al-Aswad LA (2006) Retinal nerve fiber layer thickness in normal children measured with optical coherence tomography. Ophthalmology 113:786–791
El-Dairi MA, Asrani SG, Enyedi LB, Freedman SF (2009) Optical coherence tomography in the eyes of normal children. Arch Ophthalmol 127:50–58
Huynh SC, Wang XY, Rochtchina E, Mitchell P (2006) Peripapillary retinal nerve fiber layer thickness in a population of 6-year-old children: findings by optical coherence tomography. Ophthalmology 113:1583–1592
Ahn HC, Son HW, Kim JS, Lee JH (2005) Quantitative analysis of retinal nerve fiber layer thickness of normal children and adolescents. Korean J Ophthalmol 19:195–200
Leung MM, Huang RY, Lam AK (2010) Retinal nerve fiber layer thickness in normal Hong Kong Chinese children measured with optical coherence tomography. J Glaucoma 19(2):95–99
Hwang YH, Kim YY (2013) Application of the ISNT rule to neuroretinal rim thickness determined using Cirrus HD optical coherence tomography. J Glaucoma. doi:10.1097/IJG.0000000000000015
Pradhan ZS, Braganza A, Abraham LM (2014) Does the ISNT rule apply to the retinal nerve fiber layer? J Glaucoma. doi:10.1097/IJG.0000000000000064
Alamouti B, Funk J (2003) Retinal thickness decreases with age: an OCT study. Br J Ophthalmol 87:899–901
Cheung CY, Chen D, Wong TY, Tham YC, Wu R, Zheng Y, Cheng CY, Saw SM, Baskaran M, Leung CK, Aumg T (2011) Determinants of quantitative optic nerve measurements using spectral domain optical coherence tomography in a population-based sample of non-glaucomatous subjects. Invest Ophthalmol Vis Sci 52:9629–9635
Savini G, Zanini M, Carelli V, Sadun AA, Ross-Cisneros FN, Barboni P (2005) Correlation between retinal nerve fibre layer thickness and optic nerve head size: an optical coherence tomography study. Br J Ophthalmol 89:489–492
Pogrebniak AE, Webrung B, Pogrebniak KL, Shetty RK, Crawford P (2010) Violation of the ISNT rule in nonglaucomatous pediatric optic disc cupping. Invest Ophthalmol Vis Sci 51:890–895
Alasil T, Wang K, Keane PA, Lee H, Baniasadi N, de Boer JF, Chen TC (2013) Analysis of normal retinal nerve fiber layer thickness by age, sex, and race using spectral domain optical coherence tomography. J Glaucoma 22:532–541
Grant support, research funding and proprietary interest
None
Presentation at meeting
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dave, P., Jethani, J. & Shah, J. Applicability of the ISNT and IST rules on retinal nerve fiber layer measurement on spectral-domain optical coherence tomography in normal Indian children. Graefes Arch Clin Exp Ophthalmol 253, 1795–1799 (2015). https://doi.org/10.1007/s00417-015-2980-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-015-2980-8