Abstract
Background
The phase 3 NEURO-TTRansform trial showed eplontersen treatment for 65 weeks reduced transthyretin (TTR), halted progression of neuropathy impairment, and improved quality of life (QoL) in adult patients with hereditary TTR-mediated amyloidosis with polyneuropathy (ATTRv-PN), vs. historical placebo.
Methods
NEURO-TTRansform enrolled patients with ATTRv-PN. A subset of patients were randomized to receive subcutaneous inotersen 300 mg weekly (Weeks 1–34) and subsequently switched to subcutaneous eplontersen 45 mg every 4 weeks (Weeks 37–81). Change in serum TTR and treatment-emergent adverse events (TEAEs) were evaluated through Week 85. Effects on neuropathy impairment, QoL, and nutritional status were also evaluated.
Results
Of 24 patients randomized to inotersen, 20 (83%) switched to eplontersen at Week 37 and four discontinued due to AEs/investigator decision. Absolute change in serum TTR was greater after switching from inotersen (−74.3%; Week 35) to eplontersen (−80.6%; Week 85). From the end of inotersen treatment, neuropathy impairment and QoL were stable (i.e., did not progress) while on eplontersen, and there was no deterioration in nutritional status. TEAEs were fewer with eplontersen (Weeks 37–85; 19/20 [95%] patients) compared with inotersen (up to Week 35; 24/24 [100%] patients). Mean platelet counts decreased during inotersen treatment (mean nadir reduction ‒40.7%) and returned to baseline during eplontersen treatment (mean nadir reduction, ‒3.2%).
Conclusions
Switching from inotersen to eplontersen further reduced serum TTR, halted disease progression, stabilized QoL, restored platelet count, and improved tolerability, without deterioration in nutritional status. This supports a positive benefit-risk profile for patients with ATTRv-PN who switch from inotersen to eplontersen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hereditary transthyretin amyloidosis with polyneuropathy (ATTRv-PN) is a rare, progressive, irreversible, and life-threatening autosomal dominant disorder predominantly caused by single-point mutations in the transthyretin (TTR) gene encoding TTR, a thyroxine and vitamin A transporter [1,2,3,4]. In ATTRv-PN, abnormal TTR proteins misfold and aggregate into extracellular amyloid deposits in peripheral and autonomic nerves and other major organs [4], leading to progressive polyneuropathic impairment, deterioration in quality of life (QoL), and poor prognosis. Death from complications of amyloid cardiomyopathy or cachexia typically occur within 12 years of symptom onset [2, 5,6,7,8,9].
In addition to liver transplantation, other therapeutic approaches have included tafamidis and diflunisal, which stabilize the native TTR tetrameric structure and slow disease progression [10, 11]. In addition, four gene-silencing treatments (patisiran, inotersen, vutrisiran, and most recently, eplontersen) are available. Patisiran requires intravenous infusion every 3 weeks and premedication with intravenous (IV) corticosteroid (e.g., dexamethasone or equivalent), oral acetaminophen, IV H1 blocker (e.g., diphenhydramine 50 mg or equivalent) and IV H2 blocker (e.g., famotidine 50 mg or equivalent) [12], while inotersen requires once-weekly (QW; 300 mg subcutaneous [SC]) dosing, and regular laboratory assessment for thrombocytopenia and glomerulonephritis [13]. Vutrisiran benefits from less frequent dosing than patisiran or inotersen but, like all TTR silencers, monitoring for ocular symptoms suggestive of vitamin A deficiency and use of vitamin A supplementation is advised [14]. More efficacious disease-modifying agents are needed providing more potent TTR silencing, greater convenience of use, and more favorable tolerability [15].
Eplontersen—an antisense oligonucleotide (ASO) recently approved in the United States for use in adults with ATTRv-PN—is a triantennary N-acetyl galactosamine (GalNAc)-conjugated ASO designed for receptor-mediated uptake by hepatocytes [16]. Significantly, GalNAc conjugation was shown to increase the potency of ASO molecules by 30- and 50-fold in mice expressing a mutated human genomic TTR sequence and in human hepatocyte cell culture, respectively [16], primarily due to increased uptake by hepatocytes [17]. Thus, eplontersen is used at a comparatively lower dose than the unconjugated inotersen (45 mg SC, every 4 weeks [Q4W] vs. 284 mg [free acid equivalent] SC, QW; ~ 25-fold) [18]. This provides potential for improved tolerability [17]. The phase 3 open-label NEURO-TTRansform trial (NCT04136184) met its primary endpoints, demonstrating that eplontersen treatment reduced serum TTR, halted progression of neuropathy impairment, and improved QoL in patients with ATTRv-PN, compared with historical placebo from the NEURO-TTR trial (NCT01737398) of inotersen [19, 20]. NEURO-TTRansform’s design included a randomized inotersen treatment reference group, which allowed cross-trial comparison of disease progression between NEURO-TTRansform and NEURO-TTR, supporting the use of the historical placebo [15, 19].
In this further analysis from NEURO-TTRansform, efficacy and safety in the subgroup of patients randomized to receive inotersen and who subsequently switched to eplontersen was investigated.
Methods
Trial design
The design, methodology, and characteristics of participants in the NEURO-TTRansform trial (NCT04136184/EudraCT 2019-001698-10) have been reported previously [15, 21]. The trial design is shown in Supplementary Fig. 1. Briefly, patients were randomized 1:6 to open-label inotersen 300 mg SC QW (Weeks 1–34) followed by a switch to eplontersen 45 mg SC Q4W (Weeks 37–81) or continuous eplontersen 45 mg SC Q4W (Weeks 1–81).
The relevant institutional review boards or independent ethics committees approved the trial protocol and amendments. NEURO-TTRansform was conducted in accordance with the International Council for Harmonisation and Good Clinical Practice guidelines, and relevant country-specific laws. All patients provided written informed consent before enrollment.
Patients
Eligible patients were aged 18–82 years, with ATTRv-PN Stage 1 or 2 according to the familial amyloid polyneuropathy or Coutinho stage, a documented genetic mutation in the TTR gene, and symptoms and signs consistent with neuropathy associated with TTR-mediated amyloidosis, including a Neuropathy Impairment Score of ≥ 10 and ≤ 130. Patients had to be willing to adhere to daily vitamin A supplementation, per protocol. Detailed inclusion and exclusion criteria have been reported previously [15]. The same eligibility criteria were used in the NEURO-TTR trial.
Assessments
Efficacy
Serum TTR
Mean percentage change from baseline in serum TTR concentration was evaluated at predefined intervals during the treatment period, at Weeks 5, 9, 13, 25, and 35 (inotersen treatment period), and at Weeks 49, 57, 65, 73, 81, and 85 (eplontersen treatment period). Analysis was performed using a novel validated electrochemiluminescence (ECL) assay.
Disease progression and QoL
Disease progression and QoL were assessed using validated instruments as change from baseline in the modified Neuropathy Impairment Score + 7 (mNIS + 7) composite score, and Norfolk Quality of Life-Diabetic Neuropathy (Norfolk QoL-DN) total score at Week 35 (inotersen treatment period), and at Weeks 66 and 85 (eplontersen treatment period). mNIS + 7 composite score ranges from − 22.3 to 346.3, with higher scores indicating poorer function; a decrease in score indicates improvement [22]. Norfolk QoL-DN total score ranges from − 4 to 136, with a higher score indicative of poorer QoL; a decrease in score indicates improvement [20].
Nutritional status
Nutritional status was assessed as change from baseline in modified body mass index (mBMI; BMI [kg/m2] × serum albumin [g/L]), where higher values are indicative of better nutritional status. mBMI was assessed at baseline, at Weeks 13 and 35 (inotersen treatment period), and Weeks 66 and 85 (eplontersen treatment period). mBMI was utilized to avoid potential discrepancies that can be seen with BMI measurement due to a low serum albumin level and fluid retention [23].
Safety
Safety assessments were evaluated throughout the study, as described previously [15, 19]. This included monitoring of treatment-emergent adverse events (TEAEs). TEAEs were further classified as being of special interest (ocular adverse events [AEs] related to vitamin A deficiency, thrombocytopenia, and glomerulonephritis) or as other AEs of interest (including injection-site reactions, flu-like symptoms, and abnormal liver function).
Clinical laboratory safety (including chemistry, hematology, urinalysis, thyroid panel, inflammatory panel, and coagulation) was evaluated along with vital signs and weight, physical examinations, electrocardiograms, and an ocular questionnaire.
Pharmacokinetics and immunogenicity
Plasma inotersen concentrations were measured at Weeks 1 through 35 using a validated quantitative hybridization-based enzyme-linked immunosorbent assay (ELISA) method (lower limit of quantification [LLOQ] 1 ng/mL). Plasma eplontersen concentrations, measured at Week 49 and thereafter, were determined using a validated and quantitative hybridization-based assay with ECL detection (hybridization ECL) assay (LLOQ 0.129 ng/mL). Concentrations measured during the eplontersen treatment period reflected total oligonucleotide concentration. Analyses were performed by PPD Bioanalytical Laboratory, Richmond, VA, USA.
Non-compartmental pharmacokinetic analysis of inotersen and eplontersen concentrations was conducted. Limited intensive plasma pharmacokinetic samples were collected following dosing on Days 1, 225, and 449. Plasma trough concentration (Ctrough) and post-treatment plasma concentrations of inotersen and eplontersen were evaluated in all patients, while area under the concentration–time curve (AUC0–6h), maximum plasma concentration (Cmax), and time to Cmax (Tmax) were evaluated in a subset of 35 patients (28 who were randomized to eplontersen and seven who were randomized to inotersen); Cmax and Tmax were obtained directly from concentration–time data.
Plasma samples collected throughout the study (predose [baseline, Day 1], and on Days 29, 85, 225, 337, 449, 589, and 729, including early termination samples) were analyzed for inotersen and eplontersen antidrug antibodies (ADAs) using validated qualitative ELISA methods (QPS Holdings LLC, Newark, USA [inotersen] and Charles River Laboratories, Quebec, Canada [eplontersen]) in a multitiered approach, which consisted of screening, and confirmatory and titer assays. Plasma samples collected at baseline (predose on Day 1) were analyzed for both anti-inotersen and anti-eplontersen antibodies. During the inotersen treatment period (Weeks 1‒34), plasma samples were analyzed for anti-inotersen antibodies. Following the switch to eplontersen treatment (Week 37 onwards), samples were analyzed for both anti-inotersen and anti-eplontersen antibodies.
Statistical analysis
All outcomes are summarized descriptively by treatment received before and after treatment switch. Immunogenicity status was summarized using descriptive statistics, and range by treatment and dose, and ADA levels as peak titer quartiles.
Results
Patients
Of the 24 patients randomized to inotersen, four patients discontinued study drug due to AEs (n = 3) or investigator decision (n = 1); 20 (83.3%) patients switched from inotersen to eplontersen at Week 37; there were no notable differences in baseline demographics and clinical characteristics following exclusion of these four patients from the analysis (Table 1).
In those patients initially randomized to inotersen (n = 24), most were male (66.7%) and White (82.6%), with V30M TTR variant (66.7%); 62.5% had received prior treatment with tafamidis or diflunisal. For patients randomized to inotersen, mean (standard deviation [SD]) age was 51.1 (14.4) years, BMI was 26.4 (5.4) kg/m2, mBMI was 1101.7 (246.5) kg/m2 × albumin level (g/L), and median duration of disease from onset of symptoms was 3.5 (range 0.7–47.3) years. At baseline, mNIS + 7 and Norfolk QoL-DN scores were lower for the inotersen randomized group relative to the eplontersen randomized or historical placebo groups (Table 1).
All patients received concomitant vitamin A supplementation, as per the study protocol.
Outcomes
Efficacy
Serum TTR
Following initiation of treatment with inotersen, mean serum TTR levels were reduced from baseline by − 52.3%, − 79.7%, − 78.8%, and − 74.3% at Weeks 5, 13, 25, and 35, respectively. Following switch to eplontersen at Week 37, mean serum TTR levels were further reduced, with mean percentage reductions from baseline of − 79.9% and − 80.6% at Weeks 65 and 85, respectively.
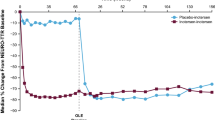
Disease progression and QoL
Assessment of neuropathy impairment based on mNIS + 7 composite scores is shown in Fig. 1A. Disease progression appeared slowed during treatment with inotersen (baseline to Week 35) and was halted during eplontersen treatment (Weeks 37‒85), in contrast to the historical placebo group, which showed progressive decline. Measurement of patient QoL (Norfolk QoL-DN total score) showed stabilization with inotersen that was maintained with eplontersen treatment after switching (Fig. 1B).
Change from baseline in A mNIS + 7 composite score, B Norfolk QoL-DN total score, and C mBMI over time with inotersen and after switching to eplontersen. mNIS + 7 composite scores range from − 22.3 to 346.3; higher scores indicate poorer function, while a decrease in score indicates improvement. *Week 85 is based on nominal visit; includes all data collected at the Week 85 visit without a visit window. Norfolk QoL-DN total scores range from − 4 to 136; higher scores are indicative of poorer QoL, while a decrease in score indicates improvement. mBMI increase is indicative of improved nutritional status, while a decrease denotes worsening. Historical placebo is from the NEURO-TTR study [20]. mBMI modified body mass index, mNIS + 7 modified Neuropathy Impairment Score + 7, Norfolk QoL-DN Norfolk Quality of Life-Diabetic Neuropathy, QoL quality of life, SE standard error
Nutritional status
During the inotersen treatment period, nutritional status (mBMI) markedly declined from baseline with the same trend and magnitude as the historical placebo group. Marked improvement in mBMI was subsequently seen with eplontersen treatment, post switching with return to baseline (Fig. 1C).
Safety
AEs
The incidence of TEAEs before and after switching was similar despite differences in the inotersen and eplontersen treatment periods; events were reported in all 24 patients (100%) randomized to inotersen (Weeks 1‒37), and in 19 of 20 patients (95%) after switching to eplontersen treatment (Weeks 37‒85 + ; onset after the first eplontersen dose to discontinuation from post-Week 85 follow-up regardless of inclusion in long-term extension study, or if completed 20-week follow-up) (Table 2). The incidence of serious TEAEs was also similar between the pre-switch inotersen (three patients; 12.5%) and post-switch eplontersen (three patients; 15.0%) treatment periods.
Patient distribution by TEAE maximum severity was broadly similar during the inotersen or eplontersen treatment periods, and comparable with the other treatment groups. TEAEs of special interest (those leading to discontinuation/withdrawal from the study) were reported in eight (33%) patients during the inotersen treatment period and in three (15%) patients during the eplontersen treatment period. Notably, there were no cases of thrombocytopenia reported during the eplontersen treatment period. There were no cases of glomerulonephritis reported in patients randomized to inotersen or after switching to eplontersen. Ocular events related to vitamin A deficiency were reported in four (17%) patients during the inotersen treatment period and in three (15%) patients during the eplontersen treatment period (Table 2). During the eplontersen treatment period, there were no reports of injection-site reaction or flu-like symptoms reported, and one reported event of elevated transaminases.
Three (13%) patients discontinued inotersen treatment early due to a TEAE; none discontinued following switch to eplontersen. Similarly, one (4%) patient discontinued inotersen treatment due to a serious TEAE (n = 3: hyperthyroidism, drug eruption, nephroangiosclerosis; n = 1: investigator judgment, persistent tubulointerstitial nephritis, and proteinuria) with none in the post-switch eplontersen group. One patient who switched to eplontersen discontinued treatment early (voluntary withdrawal; reason not reported).
Laboratory safety measures
At baseline, mean (SD) platelet count was 228.6 (67.0) × 109/L. During the inotersen treatment period, a gradual reduction in platelet count was seen, with a mean (SD) reduction in platelet count at Week 35 from baseline of – 18.8 (22.8)% (– 44.5 [58.8] 109/L) (Fig. 2). Mean nadir reduction was ‒ 40.7%. After switching to eplontersen, mean platelet count increased over a 22-week period to baseline level and remained stable thereafter (mean nadir reduction, ‒ 3.2%). The incidence of patients with a platelet count below the lower limit of normal (< 140 × 109/L) at any time post-baseline was 54.2% (13/24 patients) during the inotersen treatment period and 35.0% (7/20 patients) during the eplontersen treatment period. No patient, regardless of treatment received, had a platelet count < 25 × 109/L and no patient discontinued treatment or was withdrawn from the study due to low platelet count.
In patients randomized to inotersen, there was an observed reduction in mean estimated glomerular filtration rate (eGFR), reaching a nadir of ~ 10 mL/min/1.73 m2 below baseline; following the switch to eplontersen, mean eGFR remained stable at the level at switch; ~ 5 mL/min/1.73 m2 below [inotersen] baseline (Supplementary Fig. 2).
Pharmacokinetics and immunogenicity
On Day 225 of the inotersen treatment period, Cmax and AUC0–6 h (exposure to study drug) was 8.47 μg/mL and 46.1 μg*h/mL, respectively. On Day 449 of the eplontersen treatment period, these values were 0.27 μg/mL and 1.21 μg*h/mL, respectively; mirroring the 6.3-fold lower dose and 4-fold lower frequency of dosing of eplontersen (Table 3). At the same timepoints, plasma Ctrough level was 55.6 ng/ml for inotersen and 1.35 ng/ml for eplontersen, while median Tmax was 3.5 h (range: 3.0–4.0 h) and 3.1 h (range: 2.1–6.0 h), respectively.
Inotersen ADAs were detected in 66.7% (16/24) of patients, with treatment-emergent ADAs detected in 62.5% (15/24) of patients (nearly all persistent), with levels remaining stable through to Week 85. Eplontersen ADAs were detected in 58.3% (14/24) of patients, with treatment-emergent ADAs in 54.2% (13/24) of patients. During the inotersen treatment period, time to steady-state (from plasma Ctrough in immunogenic-negative patients) appeared to be reached by Day 85 (Fig. 3), while during the eplontersen treatment period, Ctrough was decreased by nearly two orders of magnitude; collectively mirroring change in dosage and frequency. Notably, eplontersen plasma concentration–time profiles in the first 6 h after dose administration were similar between ADA-negative and ADA-positive patients on all examined days (Days 1, 225, and 449), indicating that ADA had minimal effect on peak exposure (data not shown).
Plasma trough concentration of inotersen and eplontersen over time by IM status (pharmacokinetic set). Values are presented as mean (SD). If plasma concentration was < LLOQ (0.129 ng/mL eplontersen; 1 ng/mL inotersen), value was deemed to be 0; any summary mean < LLOQ was excluded. Samples were excluded for large deviations between scheduled and actual sampling times (difference > 30%) or for large deviations between actual dose and nominal dose (difference > 30%). IM status was defined as positive if any sample from a patient was positive to anti-eplontersen or anti-inotersen antibodies at any time during the treatment or post-treatment evaluation periods (the converse is true for negative IM). IM immunogenicity, LLOQ lower limit of quantitation, Q4W once every 4 weeks, QW once weekly, SD standard deviation
Discussion
This prespecified analysis of the phase 3 NEURO-TTRansform trial demonstrates over 85 weeks a clear positive benefit-risk profile in the subset of patients with ATTRv-PN who were switched from inotersen to eplontersen. Following the switch from inotersen to eplontersen, there was further reduction in mean serum TTR levels (− 80.6%) at Week 85, which was consistent with the reduction seen for eplontersen treatment in the NEURO-TTRansform trial at Week 85 (− 81.8%) [19], and apparent benefit towards neuropathy impairment, QoL, nutritional status, and overall safety and tolerability, including restoration of platelet count to baseline levels.
Significantly, relative to historical placebo which showed a progressive decline, disease progression measured as mNIS+7 composite score was halted rather than slowed following the switch to eplontersen. Similarly, in contrast to historical placebo which showed progressive decline, patient QoL (Norfolk QoL-DN total score) appeared stabilized and maintained during the eplontersen treatment period, consistent with eplontersen treatment in NEURO-TTRansform and inotersen treatment in NEURO-TTR [19, 20]. mBMI was used to evaluate nutritional status to avoid potential discrepancies that can occur with BMI measurement due to a low serum albumin level and fluid retention [23]. In this analysis, the evident decline in nutritional status with inotersen was similar to that seen for historical placebo while the dramatic return of nutritional status to baseline following switch to eplontersen was consistent with that seen in the NEURO-TTRansform trial, where mBMI was maintained at baseline levels during 85 weeks of eplontersen treatment [19].
The general improvement in safety and tolerability profile following the switch to eplontersen treatment was likely associated with more efficient delivery to target tissues despite a lower drug dose (25-fold), lower exposure, and need for less frequent administration, while still providing comparative efficacy both to inotersen and GalNAc-conjugated ASOs as a class [24]. Specifically, in the present analysis, post-dose plasma Ctrough levels with eplontersen were 50‒100-fold lower relative to those seen for inotersen, while virtually superimposable plasma eplontersen concentration-time profiles in the first 6 h after dose administration on Days 1, 225, and 449, suggested no accumulation of eplontersen following repeated dosing. Moreover, the pharmacokinetic profile of eplontersen was unaffected by ADAs. As the ASO-moiety of eplontersen has a virtually identical sequence and similar chemistry to inotersen, inevitably, cross-talk was evident between the inotersen and eplontersen ADA assays. Inotersen ADAs could be detected by the eplontersen ADA assay, while eplontersen ADAs against the ASO-moiety of eplontersen could be detected by the inotersen ADA assay; here, 11/13 patients with inotersen ADAs also had eplontersen ADAs while, similarly, 11/13 patients with eplontersen ADAs also had inotersen ADAs.
It is also possible that, relative to eplontersen, the comparatively poorer tolerability of inotersen might relate to high non-specific interaction/binding with proteins and potential generation of pro-inflammatory plasma cytokines; providing a milieu of immunologic dysregulation–promoting AEs such as thrombocytopenia [25]. There were very notable but opposing effects on platelet count before and following switch to eplontersen. The marked reduction in count seen during the inotersen treatment period was consistent with the NEURO-TTR trial, and the recognized risk of reduced platelet count (thrombocytopenia) with inotersen treatment [13]. In contrast, there was a gradual return to baseline level during the eplontersen treatment period, likely associated with decay of the inotersen-associated inhibitory process and the production of new platelets [20]. Similarly, this was consistent with minimal change from baseline seen for the eplontersen treatment group in the NEURO-TTRansform trial. The nature of the inhibitory process associated with ASOs that results in mild thrombocytopenia is unclear, but likely relates to innate immune activation leading to platelet sequestration [25], which differs from the mechanism underlying severe thrombocytopenia where production of antiplatelet antibodies can occur in patients with immune dysregulation [25]. Although no cases of glomerulonephritis were reported in patients randomized to inotersen, or after switching to eplontersen, a modest reduction in eGFR from baseline was seen during the inotersen treatment period (nadir ~ 5–10 mL/min/1.73 m2), which appeared to stabilize with no further change apparent during the eplontersen treatment period. Collectively, these observations suggest that treatment with eplontersen is not associated with any notable adverse effect on platelet count or eGFR, suggesting the possibility of foregoing the need to monitor platelet count, with a potentially significant benefit to long-term adherence to treatment.
The small study population and consequent lack of formal statistical testing might be considered limitations of this analysis. However, good similarity between observations in patients randomized to inotersen in the NEURO-TTRansform trial and to inotersen in the NEURO-TTR trial, and also between the eplontersen post-switch treatment group and patients initially randomized to eplontersen in the NEURO-TTRansform trial, provides confidence that the findings of this analysis are robust.
In summary, this prespecified analysis supports a positive benefit-risk profile for patients with ATTRv-PN who were switched from inotersen treatment to eplontersen treatment; specifically, further reduction in serum TTR concentration, benefit toward halting of neuropathy impairment and stabilization of QoL, greater nutritional status, and a more tolerable safety profile (with confirmation through more extended follow up) including restoration of platelet count to baseline.
Data availability
Aggregated data may be shared with researchers following formal requests of methodologically sound proposals, under data use agreements and to the extent permissible by the informed consent documents.
References
Skrahina V, Grittner U, Beetz C, Skripuletz T, Juenemann M, Krämer HH, Hahn K, Rieth A, Schaechinger V, Patten M, Tanislav C, Achenbach S, Assmus B, Knebel F, Gingele S, Skrahin A, Hartkamp J, Förster TM, Roesner S, Pereira C, Rolfs A (2021) Hereditary transthyretin-related amyloidosis is frequent in polyneuropathy and cardiomyopathy of no obvious aetiology. Ann Med 53(1):1787–1796. https://doi.org/10.1080/07853890.2021.1988696
Dyck PJB, Coelho T, Waddington Cruz M, Brannagan TH 3rd, Khella S, Karam C, Berk JL, Polydefkis MJ, Kincaid JC, Wiesman JF, Litchy WJ, Mauermann ML, Ackermann EJ, Baker BF, Jung SW, Guthrie S, Pollock M, Dyck PJ (2020) Neuropathy symptom and change: Inotersen treatment of hereditary transthyretin amyloidosis. Muscle Nerve 62(4):509–515. https://doi.org/10.1002/mus.27023
Ando Y, Adams D, Benson MD, Berk JL, Planté-Bordeneuve V, Coelho T, Conceição I, Ericzon BG, Obici L, Rapezzi C, Sekijima Y, Ueda M, Palladini G, Merlini G (2022) Guidelines and new directions in the therapy and monitoring of ATTRv amyloidosis. Amyloid 29(3):143–155. https://doi.org/10.1080/13506129.2022.2052838
Adams D, Algalarrondo V, Polydefkis M, Sarswat N, Slama MS, Nativi-Nicolau J (2021) Expert opinion on monitoring symptomatic hereditary transthyretin-mediated amyloidosis and assessment of disease progression. Orphanet J Rare Dis 16(1):411. https://doi.org/10.1186/s13023-021-01960-9
Adams D, Ando Y, Beirao JM, Coelho T, Gertz MA, Gillmore JD, Hawkins PN, Lousada I, Suhr OB, Merlini G (2021) Expert consensus recommendations to improve diagnosis of ATTR amyloidosis with polyneuropathy. J Neurol 268(6):2109–2122. https://doi.org/10.1007/s00415-019-09688-0
Schmidt HH, Waddington-Cruz M, Botteman MF, Carter JA, Chopra AS, Hopps M, Stewart M, Fallet S, Amass L (2018) Estimating the global prevalence of transthyretin familial amyloid polyneuropathy. Muscle Nerve 57(5):829–837. https://doi.org/10.1002/mus.26034
Conceição I, González-Duarte A, Obici L, Schmidt HH, Simoneau D, Ong ML, Amass L (2016) “Red-flag” symptom clusters in transthyretin familial amyloid polyneuropathy. J Peripher Nerv Syst 21(1):5–9. https://doi.org/10.1111/jns.12153
Planté-Bordeneuve V, Kerschen P (2013) Transthyretin familial amyloid polyneuropathy. Handb Clin Neurol 115:643–658. https://doi.org/10.1016/b978-0-444-52902-2.00038-2
Jang SC, Nam JH, Lee SA, An D, Kim HL, Kwon SH, Lee EK (2022) Clinical manifestation, economic burden, and mortality in patients with transthyretin cardiac amyloidosis. Orphanet J Rare Dis 17(1):262. https://doi.org/10.1186/s13023-022-02425-3
Berk JL, Suhr OB, Obici L, Sekijima Y, Zeldenrust SR, Yamashita T, Heneghan MA, Gorevic PD, Litchy WJ, Wiesman JF, Nordh E, Corato M, Lozza A, Cortese A, Robinson-Papp J, Colton T, Rybin DV, Bisbee AB, Ando Y, Ikeda S, Seldin DC, Merlini G, Skinner M, Kelly JW, Dyck PJ (2013) Repurposing diflunisal for familial amyloid polyneuropathy: a randomized clinical trial. JAMA 310(24):2658–2667. https://doi.org/10.1001/jama.2013.283815
Coelho T, Maia LF, Martins da Silva A, Waddington Cruz M, Planté-Bordeneuve V, Lozeron P, Suhr OB, Campistol JM, Conceição IM, Schmidt HH, Trigo P, Kelly JW, Labaudinière R, Chan J, Packman J, Wilson A, Grogan DR (2012) Tafamidis for transthyretin familial amyloid polyneuropathy: a randomized, controlled trial. Neurology 79(8):785–792. https://doi.org/10.1212/WNL.0b013e3182661eb1
Patirisan PI. Prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/210922s012lbl.pdf. Accessed 9 May 2024
Inotersen PI. Prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2024/211172s014lbl.pdf. Accessed 9 May 2024
Vutrisiran PI. Prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/215515s002lbl.pdf. Accessed 9 May 2024
Coelho T, Ando Y, Benson MD, Berk JL, Waddington-Cruz M, Dyck PJ, Gillmore JD, Khella SL, Litchy WJ, Obici L, Monteiro C, Tai LJ, Viney NJ, Buchele G, Brambatti M, Jung SW, St L, O’Dea L, Tsimikas S, Schneider E, Geary RS, Monia BP, Gertz M (2021) Design and rationale of the global phase 3 NEURO-TTRansform study of antisense oligonucleotide AKCEA-TTR-LRx (ION-682884-CS3) in hereditary transthyretin-mediated amyloid polyneuropathy. Neurol Ther 10(1):375–389. https://doi.org/10.1007/s40120-021-00235-6
Viney NJ, Guo S, Tai LJ, Baker BF, Aghajan M, Jung SW, Yu RZ, Booten S, Murray H, Machemer T, Burel S, Murray S, Buchele G, Tsimikas S, Schneider E, Geary RS, Benson MD, Monia BP (2021) Ligand conjugated antisense oligonucleotide for the treatment of transthyretin amyloidosis: preclinical and phase 1 data. ESC Heart Fail 8(1):652–661. https://doi.org/10.1002/ehf2.13154
Wang Y, Yu RZ, Henry S, Geary RS (2019) Pharmacokinetics and clinical pharmacology considerations of GalNAc(3)-conjugated antisense oligonucleotides. Expert Opin Drug Metab Toxicol 15(6):475–485. https://doi.org/10.1080/17425255.2019.1621838
Brannagan TH 3rd, Berk JL, Gillmore JD, Maurer MS, Waddington-Cruz M, Fontana M, Masri A, Obici L, Brambatti M, Baker BF, Hannan LA, Buchele G, Viney NJ, Coelho T, Nativi-Nicolau J (2022) Liver-directed drugs for transthyretin-mediated amyloidosis. J Peripher Nerv Syst 27(4):228–237. https://doi.org/10.1111/jns.12519
Coelho T, Marques W Jr, Dasgupta NR, Chao CC, Parman Y, França MC Jr, Guo YC, Wixner J, Ro LS, Calandra CR, Kowacs PA, Berk JL, Obici L, Barroso FA, Weiler M, Conceição I, Jung SW, Buchele G, Brambatti M, Chen J, Hughes SG, Schneider E, Viney NJ, Masri A, Gertz MR, Ando Y, Gillmore JD, Khella S, Dyck PJB, Waddington Cruz M, NEURO-TTRansform Investigators (2023) Eplontersen for Hereditary Transthyretin Amyloidosis With Polyneuropathy. JAMA 330(15):1448–1458. https://doi.org/10.1001/jama.2023.18688
Benson MD, Waddington-Cruz M, Berk JL, Polydefkis M, Dyck PJ, Wang AK, Plante-Bordeneuve V, Barroso FA, Merlini G, Obici L, Scheinberg M, Brannagan TH 3rd, Litchy WJ, Whelan C, Drachman BM, Adams D, Heitner SB, Conceicao I, Schmidt HH, Vita G, Campistol JM, Gamez J, Gorevic PD, Gane E, Shah AM, Solomon SD, Monia BP, Hughes SG, Kwoh TJ, McEvoy BW, Jung SW, Baker BF, Ackermann EJ, Gertz MA, Coelho T (2018) Inotersen treatment for patients with hereditary transthyretin amyloidosis. N Engl J Med 379(1):22–31. https://doi.org/10.1056/NEJMoa1716793
Coelho T, Waddington Cruz M, Chao CC, Parman Y, Wixner J, Weiler M, Barroso FA, Dasgupta NR, Jung SW, Schneider E, Viney NJ, Dyck PJB, Ando Y, Gillmore JD, Khella S, Gertz MA, Obici L, Berk JL (2023) Characteristics of patients with hereditary transthyretin amyloidosis-polyneuropathy (ATTRv-PN) in NEURO-TTRansform, an open-label phase 3 study of eplontersen. Neurol Ther 12(1):267–287. https://doi.org/10.1007/s40120-022-00414-z
Dyck PJB, Gonzalez-Duarte A, Obici L, Polydefkis M, Wiesman JF, Antonino I, Litchy WJ, Dyck PJ (2019) Development of measures of polyneuropathy impairment in hATTR amyloidosis: from NIS to mNIS + 7. J Neurol Sci 405:116424. https://doi.org/10.1016/j.jns.2019.116424
Suhr O, Danielsson A, Holmgren G, Steen L (1994) Malnutrition and gastrointestinal dysfunction as prognostic factors for survival in familial amyloidotic polyneuropathy. J Intern Med 235(5):479–485. https://doi.org/10.1111/j.1365-2796.1994.tb01106.x
Baker BF, Xia S, Partridge W, Kwoh TJ, Tsimikas S, Bhanot S, Geary RS (2023) Integrated assessment of phase 2 data on GalNAc(3)-conjugated 2’-O-methoxyethyl-modified antisense oligonucleotides. Nucleic Acid Ther 33(1):72–80. https://doi.org/10.1089/nat.2022.0044
Narayanan P, Curtis BR, Shen L, Schneider E, Tami JA, Paz S, Burel SA, Tai LJ, Machemer T, Kwoh TJ, Xia S, Shattil SJ, Witztum JL, Engelhardt JA, Henry SP, Monia BP, Hughes SG (2020) Underlying immune disorder may predispose some transthyretin amyloidosis subjects to inotersen-mediated thrombocytopenia. Nucleic Acid Ther 30(2):94–103. https://doi.org/10.1089/nat.2019.0829
Acknowledgements
The authors would like to thank the patients, their families, caregivers, and all investigators involved in the NEURO-TTRansform trial, Ionis Pharmaceuticals, Inc., and AstraZeneca for their participation and/or contribution.
This study was sponsored by Ionis Pharmaceuticals, Inc., Carlsbad, CA, USA. The sponsor was involved in the study design and collection, analysis, and interpretation of data, as well as data checking of information provided in the manuscript. Ultimate responsibility for opinions, conclusions, and data interpretation lies with the authors. Medical writing support was provided by Carl V. Felton, PhD, CMPP with editorial support from Jess Galbraith, BSc of Core (a division of Prime, London, UK), supported by AstraZeneca according to Good Publication Practice guidelines (Link).
Funding
This study was sponsored by Ionis Pharmaceuticals, Inc., Carlsbad, CA, USA.
Author information
Authors and Affiliations
Contributions
M.W., S.W.J., N.V., A.M. were involved in the design and conceptualization of the study. J.B., M.W., P.A.K., N.D., S.K., C–C.C., S.A., R.Z.Y., A.M., T.C. contributed to data acquisition. T.J.K., S.W.J., N.J.V., R.Z.Y., M.G. and T.C. analyzed and interpreted the data. All authors provided critical review and revision, and final approval of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
I.C. has received financial support as primary investigator, and is a consultant to Alnylam Pharmaceuticals, AstraZeneca, Ionis Pharmaceuticals Inc., and Pfizer Inc. J.L.B. has participated in an Ionis Pharmaceuticals Inc., ad hoc advisory committee. M.W. is a consultant to Akcea Therapeutics, Alnylam Pharmaceuticals, Biogen, Hoffmann-La Roche, Novo Nordisk, Pfizer, and Sobi; and has received speaker fees from Akcea Therapeutics, Alnylam Pharmaceuticals, and Biogen, and financial support for conference attendance from Akcea Therapeutics, Alnylam Pharmaceuticals, Ionis Pharmaceuticals Inc., and Pfizer Inc. P.A.K. is currently participating in the ION trial. N.R.D. is a consultant to Alnylam, Eidos, and Intellia; and has lectured for Alnylam. S.K. is a consultant to Alnylum and Ionis Pharmaceuticals Inc. C-C.C. reports no conflicts of interest. S.A. has provided consultancy for Alnylam Pharmaceuticals, AstraZeneca, and Pfizer Inc. T.J.K., S.W.J., N.J.V., and R.Z.Y. are employees of, and shareholders in Ionis Pharmaceuticals Inc. J.C. is an employee of, and shareholder in AstraZeneca. M.G. has been a consultant to Ionis Pharmaceuticals Inc./Akcea, Prothena, Sanofi, Janssen, Aptitude Health, Juno, Physicians Education Resource, AbbVie, Johnson & Johnson, Celgene, Research to Practice, and Sorrento; has received research funding from Ashfield; and has received fees for development of educational materials from i3 Health. A.M. has received research grants from Attralus, Cytokinetics, Ionis Pharmaceuticals Inc., Pfizer, Ultromics, and the Wheeler Foundation; and personal funding from Alnylam, Attralus, Bristol-Myers Squibb, Cytokinetics, Eidos, Haya, Ionis Pharmaceuticals Inc., Pfizer Inc., and Tenaya. M.W.C. is a principal investigator for the NEURO-TTRansform trial and is a consultant for Ionis Pharmaceuticals Inc. T.C. is a principal investigator for the NEURO-TTRansform trial (paid to institution) and has received financial support from Ionis Pharmaceuticals Inc., and Akcea to attend scientific meetings.
Ethics approval
The study protocol was approved by the institutional review board at each participating center, or by an independent ethics committee.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Conceição, I., Berk, J.L., Weiler, M. et al. Switching from inotersen to eplontersen in patients with hereditary transthyretin-mediated amyloidosis with polyneuropathy: analysis from NEURO-TTRansform. J Neurol (2024). https://doi.org/10.1007/s00415-024-12616-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00415-024-12616-6