Abstract
Background
Previous studies demonstrated an association between motor and cognitive performance in multiple sclerosis (MS). However, disease-related brain damage might represent a common substrate to both phenomena, which was not considered before.
Objective
Aim of this study is to investigate whether the association between cognition and motor function is beyond structural damage in patients with MS.
Methods
Eighty-one healthy controls and 106 relapsing–remitting (RR) MS patients underwent a 3.0 T MRI with quantification of T2-lesion volumes, T1-lesion volumes and normalized brain volumes. A functional examination [Nine-Hole Peg Test (9-HPT), Timed 25-Foot Walk test (T25FW) and Expanded Disability Status Scale] and a neuropsychological evaluation (Brief Repeatable Battery of Neuropsychological Tests) were also administered. Association between demographic, clinical, cognitive, MRI and functional measures were analysed with univariate analyses and hierarchical linear regression.
Results
In RRMS patients, Spatial Recall Test and Symbol Digit Modalities Test were positively correlated with 9-HPT (p < 0.001) and T25FW (p ≤ 0.035); Paced Auditory Serial Addition Test (PASAT) correlated with 9-HPT (p ≤ 0.009). 9-HPT and T25FW were significantly associated with normalized brain volumes (p ≤ 0.016), T2- and T1-lesion volumes (p ≤ 0.009). Hierarchical regression models selected age and normalized deep gray matter volume as predictors of T25FW (adjusted-R2 = 0.109). Younger age, female sex, higher normalized gray matter volume and higher PASAT 2″ scores predicted higher 9-HPT scores (adjusted-R2 = 0.337).
Conclusions
In RRMS patients, deficit in information processing speed and executive function may contribute to hand motor dysfunction beyond the effect of structural disease-related burden, supporting the integration of motor and cognitive assessment in clinical settings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple sclerosis (MS) is a chronic, inflammatory and neurodegenerative disease of the CNS characterized by inflammation, demyelination and neurodegeneration [1]. Motor dysfunction, deficits in gait and balance, and cognitive impairment are clinical hallmarks of MS that impact daily life activities [2]. Cognitive impairment affects 43–70% of MS patients. The most frequently involved cognitive domains are information processing speed, executive functions, attention, working memory and episodic memory [3].
Cognitive and motor symptoms often occur simultaneously and their relationship is well known in numerous neurological disorders [4,5,6,7,8]. In Alzheimer’s disease, impaired executive functions can lead to a significant increase of stride time and stride time variability during walking [4]. Gait deficits in patients with Parkinson's disease are exacerbated while performing simultaneous cognitive or motor tasks, with reduction in walking speed, left and right steps coordination and stride length [7]. In elderly individuals, the coexistence of cognitive deficits and mobility impairment (i.e., slow gait speed) is associated with elevated risk of progression to dementia [9, 10]. There is a growing recognition that mobility and cognitive impairments should be considered interrelated to develop new risk assessment procedures in clinical and research settings [11]. Since the likelihood of cognitive impairment increases in subjects with slower walking speed, gait speed assessment was proposed to detect prodromal dementia [11].
The simultaneous performance of cognitive tasks while walking, termed dual tasking, has been suggested as an useful tool to detect the impact of motor–cognitive impairment in patients suffering from MS [12, 13]. Several existing studies demonstrated that dual task generates cognitive–motor interference causing loss of efficacy in one or both tasks [14]. In MS patients, cognitive-motor interference intensifies functional impairments by reducing gait speed [15] and increasing fall risk [16]. Alterations in motor performance under dual-task condition are often explained within the context of the “limited-capacity model of attention”, according to which both the motor and cognitive tasks compete for finite attentional resources [16]. More recently, Plummer and Eskes [17] proposed the “task prioritization model” suggesting that the magnitude and direction of dual-task interference is also influenced by the way in which individuals spontaneously prioritize their attention.
In MS, deficits in executive functions and information processing speed have been reported to be correlated with slower gait speed measured with Timed 25-Foot Walk test (T25FW) [6, 18,19,20,21], poorer walking endurance assessed with the 6-min walk test [18, 20, 21] and lower functional mobility [18]. Moreover, cognitive dysfunction is associated with higher step length variability and increased fall frequency [22, 23]. One possible explanation is that slower information processing speed prevents a prompt response to postural threats, resulting in increased gait variability and risk of falling [22, 23]
In physiological normal conditions, walking is mainly automatic and rhythmic; however, moving across a complex environment requires higher-order cognitive functions to plan movements and avoid obstacles [5]. Gait control involves both the direct and indirect motor pathways, the former including the primary motor cortex, cerebellum, and spinal cord, and the latter involving the basal ganglia, premotor area and prefrontal cortex [5]. Existing studies of neurological patients and older adults [4, 7, 8] have mainly focused on associations between cognitive dysfunction and gait impairment, while the link between cognitive performance and hand motor function has received little attention. A few investigations demonstrated an association between hand dexterity and cognitive tests measuring information processing speed and executive functions in older adults [24] and MS patients [6]. Yet, the pathological mechanisms underpinning motor and cognitive dysfunctions remain unclear.
In one study [6], 211 MS patients underwent extensive functional and neuropsychological evaluation to assess the influence of cognitive impairment on motor dysfunction. Information processing speed and executive function tests predicted variability in gait speed and hand dexterity. However, the possible role of structural brain damage has not been explored. Gray matter atrophy and white matter abnormalities are known to correlate with both motor and cognitive dysfunction [25, 26], which can therefore develop in parallel, and not necessarily directly influencing each other. The detected association between motor and cognitive performance may be due to the tendency of MS patients with preserved mobility to perform better on neuropsychological tests than those with motor impairment.
Aim of this work is to investigate the association between cognitive function, motor performance and brain structural damage (i.e., WM lesions and atrophy) in patients with MS. To gain additional insights into the mechanisms underlying the different aspects of motor deficits in these patients and their interplay with cognitive dysfunction, we also assessed the effect of demographic, clinical, cognitive, and brain structural measures on gait speed measured with the T25FW and hand dexterity evaluated with the nine-hole peg test (9-HPT).
Methods
Ethics committee approval. The local ethical standards committee on human experimentation approved this study. Written informed consent was obtained from all participants.
Participants. We recruited 106 relapsing–remitting MS patients (RRMS) and 81 sex- and age-matched healthy controls (HC). To mitigate a potential bias due to the exhaustion of functional compensatory mechanisms and the severity of structural damage, which could mask any effects of cognition on motor performance [27], we excluded patients with the progressive phenotypes of the disease. Inclusion criteria were: age ≥ 18 years, right handedness (Edinburgh Handedness Inventory pre-MS condition ≥ 50) [28], Italian native language, no previous history of neurological disorders (other than MS for patients), and no psychiatric disorders. RRMS patients were steroid-free for at least one month, and treatment-stable for at least three months.
Clinical and functional assessment. Within 48 h from the MRI acquisition, all participants underwent a neurological and functional assessment. The neurological evaluation included the Expanded Disability Status Scale (EDSS) [29], right- and left 9-HPT, and T25FW. All functional tests were repeated twice and results were averaged.
Neuropsychological assessment. Patients also underwent cognitive assessment. Experienced neuropsychologists conducted the neuropsychological assessment on the day of MRI, using the Brief Repeatable Battery of Neuropsychological Tests (BRB-N), which assesses verbal memory (Selective Reminding Test [SRT]), visuospatial memory (10/36 Spatial Recall Test [SPART] and delayed-recall), attention and information processing speed (Symbol Digit Modalities Test [SDMT], Paced Auditory Serial Addition Test [PASAT] 3″ and 2″) and verbal fluency (Word List Generation [WLG]) [30]. Corrected scores for age, sex, and education according to normative values [30] were derived based on normative data, obtaining z-scores for each cognitive test.
MRI acquisition. Using a Philips Intera 3.0 T scanner, the following sequences of the brain were acquired from all subjects: (1) dual-echo turbo spin echo (DE-TSE) (TR/TE = 2599/16–80 ms; flip angle 90°; FOV 240 mm2; matrix 256 × 256; ETL 6; 44 contiguous, 3-mm-thick axial slices) and (2) 3D T1-weighted fast field echo (TR/TE = 25/4.6 ms, flip angle 30°, FOV 230 mm2, matrix 256 × 256, slice thickness 1 mm, 220 contiguous axial slices, in-plane resolution 0.89 × 0.89 mm2).
MRI Analysis. T2-hyperintense and T1-hypointense lesion volumes (LV) were measured on DE-TSE and 3D T1-weighted images, using a local thresholding segmentation technique (Jim 7.0, Xinapse Systems Ltd, Colchester, UK). After T1-hypointense lesion refilling [31], normalized volumes of the whole brain (NBV), GM (NGMV) and WM (NWMV) were measured using the SIENAx software [32]. Normalized deep GM volume (NDGMV), corresponding to the sum of the normalized volumes of bilateral thalamus, caudate, putamen, pallidum, amygdala and accumbens, measured with the FIRST tool [33], was also calculated.
Statistical analysis. The statistical analysis was performed using R-4.0.3 and SPSS software, version 22.0. Between-group comparisons of demographic and brain MRI measures were assessed with the chi-square test, Mann–Whitney U test, or two-sample t test (according to normality assumption).
The inverse of 9-HPT and T25FW scores were converted to z-scores using HC’s mean and standard deviation. The significance of z-scores deviation from the HC population was tested with a one-sample t test.
T2-LV and T1-LV underwent a logarithmic transformation before statistical analysis. Right and left 9-HPT z-scores were averaged to reduce the number of variables.
Univariate analyses (Pearson’s correlations) were used to assess the association between MRI measures, cognitive scores and motor performance (z-scores of T25FW and 9-HPT). We investigated the differences of correlation between the two considered functional scores by Steiger’s z-test [34]. Hierarchical regression analysis was performed to select the independent predictors of motor performance. We used a within-block stepwise approach: block 1 included demographic and clinical variables (age, sex, disease duration and education); block 2 comprised all MRI measures (NBV, NGMV, NWMV, NDGMV, T2-LV and T1-LV) and block 3 contained BRB-N tests z-scores (SRT, SPART, SDMT, PASAT 3″, PASAT 2″ and WLG). Since the EDSS score is not an independent variable explaining disability, but a measure of disability itself, it was not included among the demographic and clinical variables of the models. For all analyses, statistical significance was set at p < 0.05.
Results
Demographic, clinical, functional, neuropsychological and MRI features. Table 1 summarizes the main demographic, clinical, functional, neuropsychological and MRI findings in MS patients and HC. Compared to HC, RRMS patients showed significant motor impairment measured with 9-HPT (mean z-score = − 1.0 ± 0.8; p < 0.001) and T25FW (mean z-score = − 0.5 ± 0.8; p = 0.001).
RRMS patients performed below the normative values in all neuropsychological tests (mean z-score ≤ -0.3) except for SPART (mean z-score = 0.0 ± 0.9) and SPART recall (mean z-score = 0.0 ± 0.9).
Compared to HC, RRMS patients had lower NBV (p = 0.02), NGMV (p = 0.01) and NDGMV (p < 0.001).
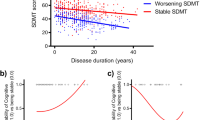
Correlations between cognitive, MRI and motor performance. Table 2 shows the univariate associations between functional measures (z-scores) and neuropsychological tests (z-scores) as well as between functional measures (z-scores) and MRI measures in RRMS patients. Linear relationship between motor and cognitive performance is presented in Figs. 1 and 2.
Scatterplots for significant positive correlations between 9-HPT and cognitive performance tests. Linear relationship between 9-HPT and SPART (r = 0.359; p < 0.001), SPART recall (r = 0.297; p = 0.002), SDMT (r = 0.388; p < 0.001) and PASAT 2″ (r = 0.294; p = 0.002). 9-HPT nine-hole peg test, PASAT paced auditory serial addition test, SDMT symbol digit modalities test, SPART 10/36 spatial recall test
Visuospatial memory assessed with SPART was associated with 9-HPT (r = 0.359; p < 0.001) and T25FW (r = 0.236; p = 0.015). Reduced information processing speed measured with SDMT, PASAT 3″ and PASAT 2″ was related to poorer performance on 9-HPT (r ≥ 0.254; p ≤ 0.009). SDMT z-scores resulted also significantly associated with T25FW (r = 0.205; p = 0.035). Verbal fluency significantly correlated with hand dexterity assessed with 9-HPT (r = 0.226; p = 0.020).
All functional measures were significantly associated with NBV (r ≥ 0.346; p < 0.001), NGMV (r ≥ 0.340; p < 0.001), NWMV (r ≥ 0.234; p ≤ 0.016) and NDGMV (r ≥ 0.317; p ≤ 0.001). Higher T2-LV and T1-LV were correlated with worse performance at 9-HPT (r ≤ -0.430; p < 0.001) and slower walking speed (r ≤ -0.254; p ≤ 0.009).
Applying Steiger’s z-test to assess differences between correlations, 9-HPT showed stronger association with PASAT 3″ (p = 0.018), PASAT 2″ (p = 0.021) and NGMV (p = 0.035) than T25FW.
Predictors of motor performance. Table 3 summarizes the results of the hierarchical regressions analysis.
Older age (p = 0.001; ΔR2 = 0.103), male sex (p = 0.042; ΔR2 = 0.035), lower NGMV (p < 0.001; ΔR2 = 0.187) and lower scores at PASAT 2″ (p = 0.017; ΔR2 = 0.037) predicted worse performance at 9-HPT (adjusted R2 = 0.337). Older age (p = 0.013; ΔR2 = 0.058) and lower NDGMV (p = 0.005; ΔR2 = 0.068) predicted slower gait speed measured with the T25FW (adjusted R2 = 0.109).
Discussion
In this study, we assessed the correlation between functional measures of upper and lower limbs, cognitive performance, and structural brain damage in RRMS patients. We subsequently identified the predictors of hand motor dexterity and walking speed among a set of demographic, clinical, MRI and cognitive variables using hierarchical regression analysis.
Better performance at tests measuring visuospatial memory and information processing speed correlated with higher degree of hand dexterity and faster walking speed. Motor performance resulted also associated with all MRI measures analysed (T2-LV, T1-LV, NBV, NGMV, NWMV and NDGMV).
As a second step, we searched for the predictors of motor impairment. Younger age, female sex, higher NGMV and higher PASAT 2″ scores predicted better hand motor performance assessed with 9-HPT, while younger age and higher NDGMV were selected as significant predictors of faster walking speed.
Our results confirm the positive correlation between motor and cognitive performance in MS [6, 19, 22, 35]. However, our work differs from available literature as we assessed the influence of potential confounding variables such as brain atrophy and focal WM lesions on the association between motor and cognitive dysfunction. It could therefore be hypothesized that information processing speed and executive function deficit contribute to explain hand motor dysfunction. Complex movements require cognitive planning and monitoring, especially in subjects with motor impairment [5, 7, 19] and a high order cognitive control dysfunction can affect the performance at complex motor tasks independently from physical disabilty and structural brain damage.
Significantly higher correlation coefficients were found between 9-HPT and PASAT 3″ and PASAT 2″ than T25FW. Our results are in line with those of previous studies which observed stronger correlations between SDMT [6, 35], PASAT [6, 35], the Brief Visuospatial Memory Test-Revised [6] and hand dexterity compared to walking speed. We hypothesize that eye-hand coordination needed to execute timely and skilful movements requires more cognitive resources than movement coordination and integration of sensory feedback necessary for walking forward [5, 36]. The greater level of cognitive complexity assumed for hand dexterity tasks compared to gait speed measures can thus explain why correlations with cognitive performance were more often statistically significant and higher for 9-HPT than T25FW.
Hand motor functioning and gait speed resulted significantly correlated with all measures of structural brain damage, as consistently demonstrated by previous studies [37]. In particular, 9-HPT scores resulted more closely associated with NGMV than walking ability. Such aspect might be due to the higher functional demand required for upper limb function, which could make it more influenced by brain damage accumulation. On the other hand, it is well-known that involvement of CNS areas, such as the spinal cord, may be more clinically relevant to explain locomotor dysfunction [38].
Univariate analysis results confirmed significant relationships between neuropsychological and motor outcomes [6, 18,19,20,21]. However, in our study, lower correlation coefficients were found compared with previous works [18, 21]. This can be explained by the fact that our sample was younger and less heterogeneous in terms of clinical phenotypes than the samples included in earlier studies [18, 21].
Applying hierarchical regression analysis, we identified the predictors of hand motor function and gait speed. Age was selected as significant predictor of motor dysfunction, confirming that slower ambulation and poorer hand dexterity are associated with advancing age in MS [39, 40]. The regression models also indicated that NDGMV is associated with T25FW. Our results align with previous works demonstrating the involvement of thalamic and basal ganglia structures in motor control [41, 42].
For the 9-HPT, predictors of performance were age, sex, NGMV and PASAT performance. The effect of sex on hand motor function is in agreement with previous studies showing that men need more time to complete the task than women [43]. A previous study in a large cohort of RRMS patients showed that NGMV was one of the main predictors of upper limb motor performance [44]. As reported by the literature, atrophy of cerebellum, basal ganglia and fronto-parietal regions may play a critical role in eye-hand coordination [25, 36].
Nine-HPT was confirmed significantly associated with PASAT 2″ even after controlling for demographic variables, clinical features and structural brain damage. PASAT has been developed to measure the rate of information processing [45]; however, numerous studies pointed out that PASAT is also related to other cognitive functions such as working memory and sustained attention [45]. Sherman and colleagues [46] tested PASAT construct validity and observed that, despite mathematical ability and attention accounted for a substantial amount of variance, verbal ability and even complex motor skills were also moderately correlated with its performance. The amount of variance shared between PASAT and complex motor skills such as manual dexterity is thought to be due to attentional/executive functioning deficits.
Evidence supports high-order cognitive functions involvement in complex movements. Our study confirmed the 9-HPT as a complex task requiring the interaction between motor- and cognitive abilities beyond the effect of disease progression and structural brain damage.
This study has a few limitations. First, our protocol did not include a spinal cord MRI acquisition that could have improved the ability of the final models to predict motor impairment. Second, we did not consider fatigue, depression and anxiety symptoms, which may influence cognitive performance in MS patients [3]. Third, it is cross-sectional, thus not allowing evaluating whether the observed predictors are related to motor worsening. Finally, the selected demographical, clinical, neuropsychological and MRI variables were able to explain only 34% and 11% of variance in the 9-HPT and T25FW, respectively. The inclusion of other MRI measures, such as those of structural and functional connectivity, could have increased the proportion of variance accounted.
Overall, this study provides evidence for an additional contribution of high order cognitive control dysfunction to motor hand dexterity impairment in MS, beyond the effect of structural brain damage.
Future studies should investigate the longitudinal evolution of cognitive and motor dysfunction in MS and clarify eventual common pathological mechanisms.
Our results support the idea that a multidimensional approach should be implemented in the clinical setting to improve the assessment of functional and cognitive deficits and enhance rehabilitation programs [11]. Also, this study provides further evidence for using composite scores for MS evaluation, including both motor and cognitive outcomes [35].
Availability of data and materials
The anonymized dataset used and analysed during the current study is available from the corresponding author on reasonable request.
References
Filippi M, Bar-Or A, Piehl F, Preziosa P, Solari A, Vukusic S, Rocca MA (2018) Multiple sclerosis. Nat Rev Dis Prim 4:43. https://doi.org/10.1038/s41572-018-0041-4
Buzaid A, Dodge MP, Handmacher L, Kiltz PJ (2013) Activities of daily living: evaluation and treatment in persons with multiple sclerosis. Phys Med Rehabil Clin N Am 24:629–638. https://doi.org/10.1016/j.pmr.2013.06.008
Rocca MA, Amato MP, De Stefano N, Enzinger C, Geurts JJ, Penner IK, Rovira A, Sumowski JF, Valsasina P, Filippi M, Group MS (2015) Clinical and imaging assessment of cognitive dysfunction in multiple sclerosis. Lancet Neurol 14:302–317. https://doi.org/10.1016/S1474-4422(14)70250-9
Allali G, Assal F, Kressig RW, Dubost V, Herrmann FR, Beauchet O (2008) Impact of impaired executive function on gait stability. Dement Geriatr Cogn Disord 26:364–369. https://doi.org/10.1159/000162358
Bayot M, Dujardin K, Tard C, Defebvre L, Bonnet CT, Allart E, Delval A (2018) The interaction between cognition and motor control: a theoretical framework for dual-task interference effects on posture, gait initiation, gait and turning. Neurophysiol Clin 48:361–375. https://doi.org/10.1016/j.neucli.2018.10.003
Benedict RH, Holtzer R, Motl RW, Foley FW, Kaur S, Hojnacki D, Weinstock-Guttman B (2011) Upper and lower extremity motor function and cognitive impairment in multiple sclerosis. J Int Neuropsychol Soc 17:643–653. https://doi.org/10.1017/S1355617711000403
Kelly VE, Eusterbrock AJ, Shumway-Cook A (2012) A review of dual-task walking deficits in people with Parkinson’s disease: motor and cognitive contributions, mechanisms, and clinical implications. Parkinsons Dis 2012:918719. https://doi.org/10.1155/2012/918719
Salvadori E, Galmozzi F, Uda F, Barbato C, Camilleri E, Cesari F, Chiti S, Diciotti S, Donnini S, Formelli B, Galora S, Giusti B, Gori AM, Marzi C, Melone A, Mistri D, Pescini F, Pracucci G, Rinnoci V, Sarti C, Fainardi E, Marcucci R, Poggesi A (2020) Association between motor and cognitive performances in elderly with atrial fibrillation: Strat-AF study. Front Neurol 11:571978. https://doi.org/10.3389/fneur.2020.571978
Grande G, Rizzuto D, Vetrano DL, Marseglia A, Vanacore N, Laukka EJ, Welmer AK, Fratiglioni L (2020) Cognitive and physical markers of prodromal dementia: a 12-year-long population study. Alzheimers Dement 16:153–161. https://doi.org/10.1002/alz.12002
Peel NM, Alapatt LJ, Jones LV, Hubbard RE (2019) The association between gait speed and cognitive status in community-dwelling older people: a systematic review and meta-analysis. J Gerontol A Biol Sci Med Sci 74:943–948. https://doi.org/10.1093/gerona/gly140
Grande G, Triolo F, Nuara A, Welmer AK, Fratiglioni L, Vetrano DL (2019) Measuring gait speed to better identify prodromal dementia. Exp Gerontol 124:110625. https://doi.org/10.1016/j.exger.2019.05.014
Argento O, Spano B, Pisani V, Incerti CC, Bozzali M, Foti C, Caltagirone C, Nocentini U (2021) Dual-task performance in multiple sclerosis’ patients: cerebellum matters? Arch Clin Neuropsychol 36:517–526. https://doi.org/10.1093/arclin/acaa089
Fritz NE, Kloos AD, Kegelmeyer DA, Kaur P, Nichols-Larsen DS (2019) Supplementary motor area connectivity and dual-task walking variability in multiple sclerosis. J Neurol Sci 396:159–164. https://doi.org/10.1016/j.jns.2018.11.015
Wajda DA, Sosnoff JJ (2015) Cognitive-motor interference in multiple sclerosis: a systematic review of evidence, correlates, and consequences. Biomed Res Int 2015:720856. https://doi.org/10.1155/2015/720856
Motl RW, Sosnoff JJ, Dlugonski D, Pilutti LA, Klaren R, Sandroff BM (2014) Walking and cognition, but not symptoms, correlate with dual task cost of walking in multiple sclerosis. Gait Posture 39:870–874. https://doi.org/10.1016/j.gaitpost.2013.11.023
Wajda DA, Motl RW, Sosnoff JJ (2013) Dual task cost of walking is related to fall risk in persons with multiple sclerosis. J Neurol Sci 335:160–163. https://doi.org/10.1016/j.jns.2013.09.021
Plummer P, Eskes G (2015) Measuring treatment effects on dual-task performance: a framework for research and clinical practice. Front Hum Neurosci 9:225. https://doi.org/10.3389/Fnhum.2015.00225
Bollaert RE, Sandroff BM, Stine-Morrow E, Sutton BP, Motl RW (2019) The intersection of cognitive performance, physical function, aging, and multiple sclerosis: a cross-sectional comparative study. Med Sci Sport Exer 51:986–986. https://doi.org/10.1249/01.mss.0000563456.84857.0d
D’Orio VL, Foley FW, Armentano F, Picone MA, Kim S, Holtzer R (2012) Cognitive and motor functioning in patients with multiple sclerosis: neuropsychological predictors of walking speed and falls. J Neurol Sci 316:42–46. https://doi.org/10.1016/j.jns.2012.02.003
Motl RW, Cadavid D, Sandroff BM, Pilutti LA, Pula JH, Benedict RHB (2013) Cognitive processing speed has minimal influence on the construct validity of Multiple Sclerosis Walking Scale-12 scores. J Neurol Sci 335:169–173. https://doi.org/10.1016/j.jns.2013.09.024
Motl RW, Sandroff BM, Benedict RHB, Hubbard EM, Pilutti LA, Sutton BP (2021) Do subcortical gray matter volumes and aerobic capacity account for cognitive-motor coupling in multiple sclerosis? Mult Scler J 27:401–409. https://doi.org/10.1177/1352458520914822
Hsieh KL, Sun R, Sosnoff JJ (2017) Cognition is associated with gait variability in individuals with multiple sclerosis. J Neural Transm (Vienna) 124:1503–1508. https://doi.org/10.1007/s00702-017-1801-0
Sosnoff JJ, Balantrapu S, Pilutti LA, Sandroff BM, Morrison S, Motl RW (2013) Cognitive processing speed is related to fall frequency in older adults with multiple sclerosis. Arch Phys Med Rehabil 94:1567–1572. https://doi.org/10.1016/j.apmr.2013.02.009
Kobayashi-Cuya KE, Sakurai R, Suzuki H, Ogawa S, Takebayashi T, Fujiwara Y (2018) Observational evidence of the association between handgrip strength, hand dexterity, and cognitive performance in community-dwelling older adults: a systematic review. J Epidemiol 28:373–381. https://doi.org/10.2188/jea.JE20170041
Cordani C, Meani A, Esposito F, Valsasina P, Colombo B, Pagani E, Preziosa P, Comi G, Filippi M, Rocca MA (2020) Imaging correlates of hand motor performance in multiple sclerosis: a multiparametric structural and functional MRI study. Mult Scler 26:233–244. https://doi.org/10.1177/1352458518822145
Riccitelli GC, Pagani E, Meani A, Valsasina P, Preziosa P, Filippi M, Rocca MA (2020) Cognitive impairment in benign multiple sclerosis: a multiparametric structural and functional MRI study. J Neurol 267:3508–3517. https://doi.org/10.1007/s00415-020-10025-z
Rocca MA, Colombo B, Falini A, Ghezzi A, Martinelli V, Scotti G, Comi G, Filippi M (2005) Cortical adaptation in patients with MS: a cross-sectional functional MRI study of disease phenotypes. Lancet Neurol 4:618–626. https://doi.org/10.1016/S1474-4422(05)70171-X
Oldfield RC (1971) The assessment and analysis of handedness: the Edinburgh inventory. Neuropsychologia 9:97–113. https://doi.org/10.1016/0028-3932(71)90067-4
Kurtzke JF (1983) Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology 33:1444–1452. https://doi.org/10.1212/wnl.33.11.1444
Amato MP, Portaccio E, Goretti B, Zipoli V, Ricchiuti L, De Caro MF, Patti F, Vecchio R, Sorbi S, Trojano M (2006) The Rao’s Brief Repeatable Battery and Stroop Test: normative values with age, education and gender corrections in an Italian population. Mult Scler 12:787–793. https://doi.org/10.1177/1352458506070933
Chard DT, Jackson JS, Miller DH, Wheeler-Kingshott CA (2010) Reducing the impact of white matter lesions on automated measures of brain gray and white matter volumes. J Magn Reson Imaging 32:223–228. https://doi.org/10.1002/jmri.22214
Smith SM, Zhang Y, Jenkinson M, Chen J, Matthews PM, Federico A, De Stefano N (2002) Accurate, robust, and automated longitudinal and cross-sectional brain change analysis. Neuroimage 17:479–489. https://doi.org/10.1006/nimg.2002.1040
Patenaude B, Smith SM, Kennedy DN, Jenkinson M (2011) A Bayesian model of shape and appearance for subcortical brain segmentation. Neuroimage 56:907–922. https://doi.org/10.1016/j.neuroimage.2011.02.046
Steiger JH (1980) Tests for comparing elements of a correlation matrix. Psychol Bull 87:245–251. https://doi.org/10.1037/0033-2909.87.2.245
Drake AS, Weinstock-Guttman B, Morrow SA, Hojnacki D, Munschauer FE, Benedict RH (2010) Psychometrics and normative data for the multiple sclerosis functional composite: replacing the PASAT with the Symbol Digit Modalities Test. Mult Scler 16:228–237. https://doi.org/10.1177/1352458509354552
Rizzo JR, Beheshti M, Naeimi T, Feiz F, Fatterpekar G, Balcer LJ, Galetta SL, Shaikh AG, Rucker JC, Hudson TE (2020) The complexity of eye-hand coordination: a perspective on cortico-cerebellar cooperation. Cerebellum Ataxias 7:14. https://doi.org/10.1186/s40673-020-00123-z
Peterson DS, Fling BW (2018) How changes in brain activity and connectivity are associated with motor performance in people with MS. NeuroImage Clin 17:153–162. https://doi.org/10.1016/j.nicl.2017.09.019
Rocca MA, Valsasina P, Meani A, Gobbi C, Zecca C, Rovira A, Montalban X, Kearney H, Ciccarelli O, Matthews L, Palace J, Gallo A, Bisecco A, Gass A, Eisele P, Lukas C, Bellenberg B, Barkhof F, Vrenken H, Preziosa P, Comi G, Filippi M, Group MS (2019) Clinically relevant cranio-caudal patterns of cervical cord atrophy evolution in MS. Neurology 93:e1852–e1866. https://doi.org/10.1212/WNL.0000000000008466
Kalinowski A, Cutter G, Bozinov N, Hinman JA, Hittle M, Motl R, Odden M, Nelson LM (2022) The timed 25-foot walk in a large cohort of multiple sclerosis patients. Mult Scler 28:289–299. https://doi.org/10.1177/13524585211017013
Oxford Grice K, Vogel KA, Le V, Mitchell A, Muniz S, Vollmer MA (2003) Adult norms for a commercially available Nine Hole Peg Test for finger dexterity. Am J Occup Ther 57:570–573. https://doi.org/10.5014/ajot.57.5.570
Motl RW, Hubbard EA, Sreekumar N, Wetter NC, Sutton BP, Pilutti LA, Sosnoff JJ, Benedict RH (2015) Pallidal and caudate volumes correlate with walking function in multiple sclerosis. J Neurol Sci 354:33–36. https://doi.org/10.1016/j.jns.2015.04.041
Motl RW, Zivadinov R, Bergsland N, Benedict RH (2016) Thalamus volume and ambulation in multiple sclerosis: a cross-sectional study. Neurodegener Dis Manag 6:23–29. https://doi.org/10.2217/nmt.15.71
Solaro C, Cattaneo D, Brichetto G, Castelli L, Tacchino A, Gervasoni E, Prosperini L (2019) Clinical correlates of 9-hole peg test in a large population of people with multiple sclerosis. Mult Scler Relat Disord 30:1–8. https://doi.org/10.1016/j.msard.2019.01.043
Cordani C, Hidalgo de la Cruz M, Meani A, Valsasina P, Esposito F, Pagani E, Filippi M, Rocca MA (2021) MRI correlates of clinical disability and hand-motor performance in multiple sclerosis phenotypes. Mult Scler 27:1205–1221. https://doi.org/10.1177/1352458520958356
Tombaugh TN (2006) A comprehensive review of the Paced Auditory Serial Addition Test (PASAT). Arch Clin Neuropsychol 21:53–76. https://doi.org/10.1016/j.acn.2005.07.006
Sherman EMS, Strauss E, Spellacy F (1997) Validity of the paced auditory serial addition test (pasat) in adults referred for neuropsychological assessment after head injury. Clin Neuropsychol 11:34–45. https://doi.org/10.1080/13854049708407027
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
Damiano Mistri, Laura Cacciaguerra, Claudio Cordani, Massimo Filippi and Maria A. Rocca contributed to the study conception and design. Data analysis was performed by Damiano Mistri, Laura Cacciaguerra, Alessandro Meani and Loredana Storelli. The first draft of the manuscript was written by Damiano Mistri, Laura Cacciaguerra, Claudio Cordani, Massimo Filippi and Maria A. Rocca and all authors commented on previous version of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
D. Mistri has no relevant financial or non-financial interest to disclose; L. Cacciaguerra received speaker and consultant honoraria from ACCMED, Roche, BMS Celgene, and Sanofi; L. Storelli has no relevant financial or non-financial interest to disclose; A. Meani received speaker honoraria from Biogen Idec; C. Cordani has no relevant financial or non-financial interest to disclose; M.A. Rocca received speaker honoraria from Bayer, Biogen, Bristol Myers Squibb, Celgene, Genzyme, Merck Serono, Novartis, Roche, and Teva, and receives research support from the MS Society of Canada and Fondazione Italiana Sclerosi Multipla; M. Filippi is Editor-in-Chief of the Journal of Neurology, Associate Editor of Human Brain Mapping, Associate Editor of Radiology, and Associate Editor of Neurological Sciences, received compensation for consulting services and/or speaking activities from Alexion, Almirall, Bayer, Biogen, Celgene, Eli Lilly, Genzyme, Merck-Serono, Novartis, Roche, Sanofi, Takeda, and Teva Pharmaceutical Industries, and receives research support from Biogen Idec, Merck-Serono, Novartis, Roche, Teva Pharmaceutical Industries, Italian Ministry of Health, Fondazione Italiana Sclerosi Multipla, and ARiSLA (Fondazione Italiana di Ricerca per la SLA).
Ethical approval
The local ethical standards committee on human experimentation approved this study.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Mistri, D., Cacciaguerra, L., Storelli, L. et al. The association between cognition and motor performance is beyond structural damage in relapsing–remitting multiple sclerosis. J Neurol 269, 4213–4221 (2022). https://doi.org/10.1007/s00415-022-11044-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-022-11044-8