Abstract
Introduction
Glymphatic fluid circulation may be considered the lymphatic system of the brain and the main role of such system seems to be played by aquaporins (AQPs), a family of proteins which regulates water exchange, in particular AQP4 and 1. Alterations of glymphatic fluid circulation through AQPs variations are now emerging as central elements in the pathophysiology of different brain conditions, like hydrocephalus. This systematic review provides an insight about the role of AQPs in hydrocephalus establishment and compensation, investigating their possible role as diagnostic tools or therapeutic targets.
Methods
PubMed database was screened searching for the relevant existing literature in English language published until February 29th 2020, according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement.
Results
A total of 40 articles met the inclusion criteria for our systematic analysis. AQP4 resulted the most studied water channel, followed by AQP1. The changes in cerebrospinal fluid (CSF), brain parenchyma and choroid plexus (CP) in different hydrocephalus type were analyzed. Moreover, important pharmacological interactions regarding AQP and molecules or conditions were discussed. A very interesting result is the general consensus on increase of AQP4 in hydrocephalic patients, unless in patients suffering from idiopathic normal pressure hydrocephalus, where AQP4 shows a tendency in reduction.
Conclusion
AQP seem to play a central role in the pathophysiology of hydrocephalus and in its compensation mechanisms. Further studies are required to definitively establish their precise roles and their quantitative changes to allow their utilization as diagnostic tools or therapeutic targets.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Brain parenchyma is devoid of lymphatic vessels for interstitial fluid (ISF) transport. Glymphatic fluid circulation can be considered the lymphatic system of the brain and it is emerging as a fundamental system for supporting brain metabolism and clearance of waste products [1, 2]. It is also emerging as an important player in some forms of dementia, where clearance of B-amyloid is impaired due to a reduction of expression of aquaporin (AQP) 4 channels [3,4,5].
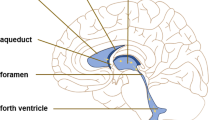
Cerebrospinal fluid (CSF) is a fluid contained in subarachnoid space and ventricles and it amounts for about 150 ml of which 125 are contained in basal cisterns [6]. After production, the amount of CSF derives from the net filtration and adsorption of water and solutes in the interstitial space [1, 7, 8]. In fact, CSF flows within the Virchow–Robin spaces in an arterial paravascular space, where it enters the brain and is then absorbed in the venous paravascular space, where it enters the venous flow [2, 4, 9]. This exchange of water is regulated by AQP channels that are a family of membrane proteins that passively allow the bidirectional transport of water according to hydrostatic and osmotic pressure [4, 7]. Any changes in AQPs expression may contribute to hydrocephalus due to an impairment of water reabsorption in the venous compartment [10,11,12].
Nowadays AQP4 is considered the most important element in the glymphatic system but other aquaporins, such as AQP1, have also been reported to play important roles [7, 10, 13]. AQP4 is predominantly expressed in the brain parenchyma, while other AQPs such as AQP1 are expressed in other regions like choroid plexus.
Hydrocephalus is a common disease that neurosurgeons are required to face during the everyday clinical practice. It can be related to an acute blockage of the CSF circulation as a result, for example, of an intracranial hemorrhage; or it may be a chronic condition, like idiopathic normal pressure hydrocephalus (iNPH) [6].
Nowadays, CSF diversions both in terms of ventriculoperitoneal shunts or endoscopic third ventriculostomies represent the only way to treat hydrocephalus. On one hand, they are simple surgical procedures but, on the other hand, they could have a poor clinical response [14, 15] or complications that might be dangerous and potentially fatal [6].
For this reason, neurosurgeons should treat only patients with a certain or a very probable diagnosis. This may not be so easy in communicating and chronic hydrocephalus, like iNPH [14, 16]. AQPs are, therefore, be good candidates as diagnostic tools [6, 14, 17], potentially dosing them in CSF samples taken during a tap test.
Further looking, understanding the role of AQPs in the development and maintenance of a hydrocephalus may lead to consider these water channels also as good candidates for targeted treatments [18,19,20], in a similar way as acetazolamide for idiopathic intracranial hypertension [21]. In other words, discovering their precise function could allow the realization of targeted medicaments to alternatively inhibit or activate them, to be administered intrathecally or orally.
Given the increasing knowledge about the involvement of glymphatic system and AQPs in hydrocephalus, we aim to provide a systematical review of the literature about the role of AQPs in hydrocephalus to enlighten possible future translational aspects of basic research studies on hydrocephalus.
Methods
We reviewed the existing literature on PubMed (Medline) until February 29th 2020, in English language, without restrictions about the paper publication status, according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement [22] (see also Supplementary Material for the PRISMA checklist). We conducted a research on PubMed with the sequential keywords “aquaporin AND hydrocephalus” and “aquaporin AND CSF”, then we reviewed the references of the relevant studies as additional source of eligible articles. We decided to include works specifically focused on hydrocephalus, without limitation about the species of the research, and to exclude pure reviews (without new cases) and editorials.
Afterwards, all titles and abstracts were screened to exclude not relevant studies: neurological conditions other than/causing other than hydrocephalus (brain edema, including infectious diseases and tumors causing it); studies about the role of AQPs in physiologic conditions; AQPs in spinal cord physiology and pathology. Some other studies could successively have been excluded after full-text article reading.
Data of the eligible works were obtained through careful analysis of full text by one author and checked by another.
Results
Through literature searching on PubMed, 87 articles were found using the words “aquaporin AND hydrocephalus”. Using as keywords “aquaporin AND CSF” we found 330 articles, 49 of which already included in the first search. In addition, 4 other articles were identified as eligible from the analysis of the references in the previous articles.
Therefore, a total of 372 papers were screened through analysis of title and abstract and 327 were excluded (articles considered not relevant, pure reviews and editorials, studies without at least the abstract in English language).
A number of 45 articles were analyzed through full text reading and other 5 were further excluded (3 because did not actually investigate the hydrocephalic condition, 1 because was in fact a review, 1 because was not about the hydrocephalus-AQP relationship).
Finally, 40 articles could be included in the qualitative synthesis (Fig. 1) [11, 12, 18,19,20, 23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57].
Flow diagram of the inclusion process based on the “PRISMA 2009 flow diagram” (see reference [22])
For each study, we extrapolated the AQP type(s) the authors addressed to, the hydrocephalus type(s) considered, the species involved, the material, wherein AQPs were studied, the effective number of cases, and the relevant results with possible direct pharmacological evidence (Tables 1, 2, studies in animals and human beings, respectively). For analysis purposes, we considered Tables 1, 2 as a whole.
Some general statements can be posed considering all the 40 articles, while others are based on the different hydrocephalus type.
General considerations
Considering the year of publication, it is evident that the interest about the role of AQPs in the pathophysiology has been discovered during the last 15 years, and that the last year was the most prolific one (Fig. 2).
Column chart representing the number of studies per year investigating the role of aquaporins in hydrocephalus. The article by Eide et al. officially published in 2020 (see reference [23]) has been included in the column “2019”, since it was available online before December 31st, 2019
It is also clear that the AQP the scientists are more interested in is AQP4 (Table 3). In 10 studies more than one channel was studied (two or three at once). They all included APQ1 and AQP4 (10/10); one also studied AQP5 (1/10) and another AQP9 (1/10). Looking at the 30 works focused on a single AQP, in 24/30 (80.0%) the main character was AQP4, while in the others 6/30 (20%) it was AQP1. Moreover, all articles but one in the last 3 years studied AQP4.
As long as it concerns the species involved in the investigations, only 4 studies included two species, while the others included only one. Human patients and controls underwent acquisition of CSF and/or specimens of brain parenchyma or of choroid plexus or underwent radiological evaluation for obtaining results in 19 works; in 1 work, human cells were cultured. In 15 and 6 experiments were involved rats and mice, respectively; dog, parrot and rabbit were used in one work each (Tables 1, 2, 4).
Another interesting consideration is about control groups: 33 out of the 40 (82.5%) studies included a control patient or group. The remaining 7 works are case reports or limited case series (4/7), a large series in which only encephalomegalic mice were considered (1/7) and papers in which specific number of cases as well as a possible control cohort are not mentioned (2/7).
AQP and hydrocephalus “type”
We gathered studies in which the same or similar hydrocephalus pathophysiology (simplifying, “type”) was involved.
Obstructive hydrocephalus
A number of 16 articles (16/40—40%) specifically studied obstructive hydrocephalus; 2 of these described the phenomenon in neuromyelitis optica (NMO) patients, while 1 was focused on the initial stage of non-communicating hydrocephalus development. The interest in obstructive hydrocephalus has been present since the first studies. This is the only type in which AQP5 and 9 were investigated (1/16 each—6.2%), although a greater interest was posed in AQP1 (6/16—3.7% studies) and even more on AQP4 (14/16—25%).
From the synthesis of the results, AQP4 in obstructive hydrocephalus has generally shown an altered distribution within cells when studied with immunohistochemical tools on biopsies and a generalized increase when studied in CSF. Some studies report that, although this, a difference in AQP4 concentration does not exist, while the majority of the studies described firstly a “normal” concentration of AQP4 at the initial stages of the developing of hydrocephalus and then a higher presence of this water channel in later stages. This is evident in particular when the patients/cases are studied at different time points.
Other two results underline the role of AQP4: hydrocephalus in NMO and AQP4 knockout mice. NMO is primarily an autoimmune disease directed against AQP4, and some of these patients may develop hydrocephalus. In such cases, the pathophysiology seems clearly relatable to this water channel and the absence of immunoreactivity for AQP4 can be found in obstructive hydrocephalic patients suffering from such pathology. On the other hand, in a subset of AQP4 knockout mice there was development of hydrocephalus and if another cause was superimposed the hydrocephalus worsened.
As far as it concerns AQP1, it equally shows in some studies only an altered polarity, whereas in other a decrease in the acute condition and then a slight increase later. Interesting the described down-regulation of AQP1 mRNA levels both at 24 and at 72 h, phenomenon anyway described also in controls.
Communicating hydrocephalus
In 6 works (6/40—15%) the authors studied communicating hydrocephalus, and in 2 out of 6 reported the possibility of communicating hydrocephalus in NMO.
Communicating hydrocephalus has been constantly investigated during the years too. The experiments were quite equally subdivided between AQP1 (3/6) and AQP4 (4/6).
AQP4 shows an increase and an altered polarization also in communicating hydrocephalus. If a dysfunction of this channel is figured out, this may predispose to such a type of hydrocephalus—this was observed in communicating hydrocephalic NMO patients.
AQP1 shows a general decrease: it can’t be detected in CSF and express an extremely low immunoreactivity even in case of hyperplasia of the choroid plexus.
NPH/age related hydrocephalus
Other 8 papers (8/40—20%) focused on either iNPH or “age-related” hydrocephalus. Authors considered these etiologies only since 2013 and interest increased during the last months of our review. In almost all AQP4 was the main character (7/8), but also AQP1 deserved a role (2/8).
NPH could have a distinct physiopathology with respect to other chronic hydrocephalus cases. In iNPH, AQP1 generally shows an increase, while AQP4 a decrease. On the other hand, in chronic and age-related cases in experimental models, AQP4 express an increase combined with less polarization.
Congenital or “multiple” hydrocephalus
A particular subgroup is constituted by the reports in which was studied “congenital” hydrocephalus independently from its origin, articles about one type evolving in the other type, or works without subgrouping for hydrocephalus type. This group includes 10 articles (10/40—25%) and was more investigated at the beginning of our considered period. As in the others anyway, AQP4 has always been the most studied (8/10) followed by AQP1 (4/10).
Very interestingly in one study many CSF biomarkers showed robust association with congenital hydrocephalus, but not with AQP4 [34]. In other studies, AQP4 shows a general increase in the CSF of hydrocephalic patients and this increase is greater in communicating than in obstructive and controls [42]. Moreover, the increase is higher at later stage (also when it is caused by another condition such as neurocysticercosis [27]) and is accompanied by the usual altered polarization.
AQP1 is characterized by a certain degree of decrease in choroid plexus and brain at initial stages, but a quite sure increase at the CSF-blood barrier and in the CSF (more in obstructive cases, with inverted polarization) [46]. AQP1 shows an increase in CSF hypersecretion conditions and a decrease when there is an obstruction of CSF circulation or when ventricular sizes are in range [20, 26, 46].
Pharmacological implications
Four studies out of 40 involving possible pharmacological considerations were found. Two dealt with obstructive hydrocephalus cases (olomoucine [19], erythropoietin or EPO [18]); one involved age-related hydrocephalus (hypoxia related) [31] and one involved congenital hydrocephalus (vinpocetine) [20].
In one study intraperitoneal olomoucine showed a capacity to attenuate the entity of hydrocephalus through inhibition of astrogliosis, which can be among the causes of later stages obstruction [19].
In another research intraperitoneal EPO further up-regulated AQP4 enhancing the natural mechanism which begins when hydrocephalus becomes clinically evident [18].
Hypoxia seems to have a key role in development of hydrocephalus. In fact, in a mice model it seems to act synergistically with aging to produce hydrocephalus [31].
Vinpocetine in a choroid plexus cell line of a congenital hydrocephalus demonstrated to up-regulate AQP1 and AQP4 in cultured choroid plexus cells [20].
Discussion
The brain parenchyma has no lymphatic system [1, 4]. This dogma of the human anatomy has fallen after recent studies suggesting that ISF is exchanged at the level of the so-called glymphatic system, which represent a form of lymphatic system of the brain. In this view, our knowledge about CSF formation and reabsorption has changed [1]. In fact, CSF derives from the net filtration and adsorption of water and solutes in the interstitial space. This exchange is regulated by several complex mechanisms that are mainly regulated by hydrostatic and oncotic pressure at the level of the paravascular system [1, 4, 5, 7]. Given the presence of a waterproof blood brain barrier, exchange of water in the glymphatic system is granted by the presence of a family of water channels proteins called aquaporins (AQPs) [7, 13]. Expression of these channels regulates the amount of water in the central nervous system. As consequence, hydrocephalus which means “accumulation of water in the brain” can be explained in some cases by an impairment of function of the glymphatic system at AQP level, especially in case of communicating hydrocephalus [7, 42, 58].
Different is the case of obstructive hydrocephalus in which a macroscopic blockage of the CSF circulation is at the base for a compartmentalization of CSF, like in case of triventricular or biventricular hydrocephalus due to tumors, or a microscopic blockage impairs adequate flow like in hemorrhages. Moreover, in case of hydrocephalus due to degenerative diseases the mechanism of development seems different from the previous two. So far, basic research studies are opening a new window on the knowledge about hydrocephalus formation and physiology that have the possibility to impact on clinical management and treatment [4, 8]. For example, on the apical membrane of choroid plexus epithelium AQP1 has been found, suggesting a role for it in CSF production [8]. Moreover, it has been proved that inhibition of CSF production in rodents by treatment with acetazolamide impairs CSF clearance [4]
This is why the scientific community has intensified the production of works about AQP in the last years. About the scientific production, it is possible to note some focal points: (1) AQP4 is the most studied aquaporin followed by AQP1, while other aquaporin are only matter of small reports; (2) the majority of study groups is trying to recreate an own internal reference system with a control group; (3) the number of studies involving animals is comparable to the number involving humans (24 vs. 20, Tables 1, 2 and 4); (4) up to now, a standard model of hydrocephalus is still lacking.
From this systematic review, we inferred some interesting results that allowed us many reflections about different hydrocephalus types.
-
Obstructive hydrocephalus
Obstructive hydrocephalus is the most studied hydrocephalus in our topic, firstly because this is the easiest to be recreated through animal models (with blood or kaolin). From a pathophysiological point of view, we found an interesting report showing how a deletion of AQP4 predispose to congenital aqueductal stenosis and hydrocephalus probably due to ependymal cells alterations [12]. This study suggests that AQP4 may have a role in maintaining the structural integrity of ependymal epithelium [12, 44].
As far as it concerns AQP4, it seems to have a concentration in range of normality in case of initial stages of obstructive hydrocephalus and it shows a higher presence in later stages, when hydrocephalus becomes relevant [28, 32, 45]. This is in line with experimental studies on kaolin-induced hydrocephalus in which serial CSF sampling demonstrates an up-regulation of AQP4 in later stage of hydrocephalus probably in response to obstruction of CSF circulation [42]. Such studies also suppose that AQP4 production might be regulated by a pressure sensitive mechanism. For AQP1 there is no unequivocal statement, since in some studies, only altered polarization is described, while in others, there’s a trend similar to AQP4 but less evident. However, interestingly in a study an increase in AQP1 and AQP4 was found in a model of rat subarachnoid hemorrhage with hydrocephalus, with also an increased ratio AQP1/AQP4 [28].
In this kind of hydrocephalus, where there is a mechanical obstruction to CSF circulation, pharmacological options seem to have a poor promising utility. However, in a study olomoucine showed a capacity to attenuate the entity of hydrocephalus through astrogliosis inhibition [19]. At later stages, obstruction due to aqueductal stenosis seems effectively to have among its causes also astrogliosis so olomoucine would be a very promising option in selected cases.
Furthermore, it is interesting to note that obstructive hydrocephalus seems to have two components involved in its physiopathology: (1) related to obstruction of CSF circulation; (2) related to an alteration of AQP recycle at later stage that it can be speculated to be a compensatory mechanism secondary to an engulfment of glymphatic system.
-
Communicating hydrocephalus
Considering communicating hydrocephalus in its inclusive meaning, the studies in humans principally concern iNPH and communicating hydrocephalus NMO-related, while other kinds of hydrocephalus are sporadically reported [43] and almost only in animal models [31, 36, 40, 49]. In a study, AQP4 demonstrated to be increased in communicating congenital hydrocephalus in comparison to controls [42]. The increase of AQP4 in communicating hydrocephalus might be a compensatory mechanism of the brain to try to react to an impairment of the reabsorption of CSF.
So far, reports from the literature suggest the existence of two distinct features relating hydrocephalus and AQPs: (1) AQP4 is generally increased in CSF or parenchyma of communicating hydrocephalus; (2) in iNPH, there is a global decrease of AQP4 in CSF in contrast with other kind of communicating hydrocephalus.
Considering the congenital hydrocephalus, AQP4 is again generally reported as increased, while AQP1 seems to increase when there is CSF hypersecretion. Some discordant results have been proposed in 2017 [34]: no association between AQP4 and congenital hydrocephalus. These controversial findings can be related with the model of hydrocephalus chosen (congenital hydrocephalus mainly due to aqueductal stenosis): firstly, CSF circulation is different in the early stages of life; secondly, the kind of hydrocephalus is mainly but not totally obstructive.
In 2013 a series of children with both communicating and obstructive hydrocephalus was studied [42]. A significant increase of AQP4 was evident in CSF of children with communicating hydrocephalus compared to normal controls and to children with obstructive hydrocephalus; these latter had a higher AQP4 concentration compared to controls, but not statistically significant. These results confirm our considerations being in line with the previous analyses.
This discrepancy between the two studies is of interest, since it shows how the kind of hydrocephalus can influence the expression of AQPs in humans.
-
Are normal pressure hydrocephalus and degenerative brain diseases linked pathologies?
Although iNPH is a type of communicating hydrocephalus, it has shown a distinct pattern of CSF concentration of AQPs. In fact, CSF or parenchymal concentrations of iNPH patients showed that AQP1 is generally increased. Interestingly, it was reported an increase in AQP1 both in patients with MCI and iNPH [38]. Concerning AQP4, it has been found generally decreased in patients with iNPH [23, 25, 29, 30, 33]. In another study a decreased concentration of AQP4 in CSF of patients with iNPH and with Alzheimer’s disease (AD) was reported [25]. Moreover, several studies reported an increase of amyloid-β (Aβ) in both patients with AD and iNPH, while hyperphosphorylated Tau is increased only in patients with AD [59,60,61]. Therefore, these results suggest a connection between AD and iNPH [25].
As consequence, from the few studies available on human also suggesting the reduced Aβ clearance by the gylmphatic systems due to a reduction in AQP4 [62, 63], AD and iNPH might be linked by an impairment of the glymphatic system. Such considerations could also explain why iNPH patients often show overlapping symptoms with other brain conditions such as AD, basal ganglia degeneration and Parkinson’s disease [14, 16].
Differently from other kind of hydrocephalus, AQP4 reduction in iNPH and AD is related to a progressive disruption of the paravascular unit involved in the water exchange [63]. In a purely speculative way, this fact can lead to an alternative model of hydrocephalus explaining both the normal intracranial pressure and the low concentration of AQP4. In fact, in communicating hypertensive hydrocephalus there may not be a loss of brain parenchyma but rather an accumulation of CSF due to the obstruction of paravascular spaces [36, 40]. This fact may lead to an up-regulation of AQP4 in response to increased intracranial pressure and, therefore, to an increased AQP4 concentration in parenchyma and subsequently in CSF [40, 42]. On the other hand, in case of iNPH there is a progressive accumulation of Aβ, loss of brain parenchyma and progressive impairment of glymphatic system without an increased intracranial pressure, probably due to brain atrophy. As consequence, due to a lack of mechanisms to up-regulate AQP4 expression and to a progressive loss of paravascular units it is possible to register low concentrations of AQP4 in CSF of patients with iNPH [23, 25, 29, 30, 33]. In a similar way, in AD patients, there is a progressive loss of brain parenchyma and paravascular units which relates with low AQP4 concentrations in CSF [3].
Less is known about the role of AQP1 in iNPH which generally shows a tendency to increase which is possibly related with the different expression of such protein in the brain [38].
These considerations may lead to further investigations aiming at improving knowledge about hydrocephalus and normal CSF circulation. Moreover, definitive findings may lead to the use of a panel of CSF biomarkers to better differentiate brain degenerative diseases from iNPH, reducing the number of misdiagnoses and increasing the response rate of patients after VP shunt placement.
A summary of the number of studies underlying which aquaporin is increased or decreased in which hydrocephalus type is provided in Table 5.
-
Future clinical aspects related to AQPs
From a clinical point of view, studies on AQPs show several translational aspects that may be at the base of the increased number of studies published in the last months: AQPs are candidate to become a possible CSF biomarker to diagnose hydrocephalus. Their role is probably going to develop from basic science to human clinical experience.
In fact, AQPs measured in CSF might help clinician in differentiating iNPH from other conditions, to diagnose some forms of chronic communicating hydrocephalus or to support the diagnosis of a shunt malfunction in difficult cases, like in patients with overdrainage or slit ventricles [64,65,66]. Considering our hypotheses, in overdrainage cases APQs levels should not be altered compared to controls, –as in the slit ventricle syndrome they would show variations in concentration. In case of obstructive hydrocephalus, AQPs would as well theoretically be useful in selected cases. They would be ideally suitable in some clinical scenarios like, for example, to differentiate between patients responding to third ventriculostomies or VP shunt.
Moreover, AQPs might be candidates as therapeutic targets for hydrocephalus. Unfortunately nowadays only few non-specific and toxic inhibitors or modulators that targets some AQPs are currently available, greatly limiting their therapeutic utility. The only substances or conditions with a proven effect in single studies (EPO, olomoucine and vinpocetine) neither have a validation yet, nor their mechanism of action is fully understood. EPO seems to have the ability to further up-regulate AQP4 expression, enhancing the mechanism which physiologically begins when hydrocephalus becomes significant. EPO is a well-known substance, already utilized in different diseases, whose use could be relatively easy to extend also to this condition if the data would be validated.
The study of pathophysiology of hydrocephalus in all its forms, the molecular study of AQPs and the possible future development of target therapies (monoclonal antibodies, microRNA) could be the keys to make AQPs a routine diagnostic test and also a therapeutic target of paramount importance in hydrocephalic cases. They would be another “weapon” in the neurologist’s and neurosurgeon’s armamentarium, together with other targets of contemporary hydrocephalus research, like Na–K-ATPase, mineralocorticoid receptors or precocious blood dissolution after subarachnoid hemorrhage [67].
Finally, studies on other AQPs also present in the brain (like AQP5 or 9) might help to better understand pathogenesis and physiopathology of hydrocephalus.
This review has some limitations. First of all, a uniform model of hydrocephalus is still lacking, and therefore, generalizations may be affected by the differences in the models. Secondly, although generally accepted the division between “obstructive” and “communicating” remains arbitrary; this may reflect into partially different results with `t to this review. Finally, other factors besides AQPs are likely to be involved in this complex system.
Conclusion
AQPs have been widely studied in the recent years and in particular their role in hydrocephalus has been investigated. AQP4 is considered the main player in the glymphatic system, followed by AQP1. Their proven implication in hydrocephalic mechanisms could inspire new research towards assessment of their role as diagnostic tools or as therapeutic targets. Moreover, in a speculative way, studying the variation of AQPs in CSF and brain parenchyma may lead in the future a possible reclassification of hydrocephalus that could be of help not only in understanding the pathophysiology of hydrocephalus but also in clinical decision making.
Availability of data and material
All data and materials support published claims and comply with field standards.
Code availability
Not applicable.
References
Iliff JJ, Goldman SA, Nedergaard M (2015) Implications of the discovery of brain lymphatic pathways. Lancet Neurol 14:977–979. https://doi.org/10.1016/S1474-4422(15)00221-5
Iliff JJ, Wang M, Liao Y et al (2012) A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid. Sci Transl Med 4:147111. https://doi.org/10.1126/scitranslmed.3003748
Zeppenfeld DM, Simon M, Haswell JD et al (2017) Association of perivascular localization of aquaporin-4 with cognition and Alzheimer disease in aging brains. JAMA Neurol 74:91. https://doi.org/10.1001/jamaneurol.2016.4370
Rasmussen MK, Mestre H, Nedergaard M (2018) The glymphatic pathway in neurological disorders. Lancet Neurol 17:1016–1024. https://doi.org/10.1016/S1474-4422(18)30318-1
Jessen NA, Munk ASF, Lundgaard I, Nedergaard M (2015) The glymphatic system: a beginner’s guide. Neurochem Res 40:2583–2599. https://doi.org/10.1007/s11064-015-1581-6
Farb R, Rovira À (2020) Hydrocephalus and CSF disorders. In: Hodler J, Kubik-Huch RA, von Schulthess GK (eds) Diseases of the brain, head and neck, spine 2020–2023: diagnostic imaging. Springer, Cham (CH)
Papadopoulos MC, Verkman AS (2013) Aquaporin water channels in the nervous system. Nat Rev Neurosci 14:265–277. https://doi.org/10.1038/nrn3468
Nakada T, Kwee IL (2019) Fluid dynamics inside the brain barrier: current concept of interstitial flow, glymphatic flow, and cerebrospinal fluid circulation in the brain. Neuroscientist 25:155–166. https://doi.org/10.1177/1073858418775027
Iliff JJ, Lee H, Yu M et al (2013) Brain-wide pathway for waste clearance captured by contrast-enhanced MRI. J Clin Invest 123:1299–1309. https://doi.org/10.1172/JCI67677
Mestre H, Hablitz LM, Xavier AL et al (2018) Aquaporin-4-dependent glymphatic solute transport in the rodent brain. eLife 7:e40070. https://doi.org/10.7554/eLife.40070
Guo J, Mi X, Zhan R et al (2018) Aquaporin 4 silencing aggravates hydrocephalus induced by injection of autologous blood in rats. Med Sci Monit 24:4204–4212. https://doi.org/10.12659/MSM.906936
Feng X, Papadopoulos MC, Liu J et al (2009) Sporadic obstructive hydrocephalus in Aqp4 null mice. J Neurosci Res 87:1150–1155. https://doi.org/10.1002/jnr.21927
Iliff J, Simon M (2019) CrossTalk proposal: The glymphatic system supports convective exchange of cerebrospinal fluid and brain interstitial fluid that is mediated by perivascular aquaporin-4. J Physiol (Lond) 597:4417–4419. https://doi.org/10.1113/JP277635
Raneri F, Zella MAS, Di Cristofori A et al (2017) Supplementary tests in idiopathic normal pressure hydrocephalus: a single-center experience with a combined lumbar infusion test and tap test. World Neurosurg 100:567–574. https://doi.org/10.1016/j.wneu.2017.01.003
Locatelli M, Draghi R, Cristofori ADI et al (2014) Third ventriculostomy in late-onset idiopathic aqueductal stenosis treatment: a focus on clinical presentation and radiological diagnosis. Neurol Med Chir (Tokyo) 54:1014–1021. https://doi.org/10.2176/nmc.oa.2013-0367
Wikkelso C, Hellstrom P, Klinge PM et al (2013) The European iNPH Multicentre Study on the predictive values of resistance to CSF outflow and the CSF Tap Test in patients with idiopathic normal pressure hydrocephalus. J Neurol Neurosurg Psychiatry 84:562–568. https://doi.org/10.1136/jnnp-2012-303314
Marmarou A, Bergsneider M, Klinge P et al (2005) The value of supplemental prognostic tests for the preoperative assessment of idiopathic normal-pressure hydrocephalus. Neurosurgery 57:S2-17–S2-28. https://doi.org/10.1227/01.NEU.0000168184.01002.60
Rizwan Siddiqui M, Attar F, Mohanty V et al (2018) Erythropoietin-mediated activation of aquaporin-4 channel for the treatment of experimental hydrocephalus. Childs Nerv Syst 34:2195–2202. https://doi.org/10.1007/s00381-018-3865-z
Ding Y, Zhang T, Wu G et al (2019) Astrogliosis inhibition attenuates hydrocephalus by increasing cerebrospinal fluid reabsorption through the glymphatic system after germinal matrix hemorrhage. Exp Neurol 320:113003. https://doi.org/10.1016/j.expneurol.2019.113003
Paul L, Madan M, Rammling M et al (2009) The altered expression of aquaporin 1 and 4 in choroid plexus of congenital hydrocephalus. Fluids Barriers CNS 6:S7. https://doi.org/10.1186/1743-8454-6-S1-S7
Supuran CT (2015) Acetazolamide for the treatment of idiopathic intracranial hypertension. Expert Rev Neurother 15:851–856. https://doi.org/10.1586/14737175.2015.1066675
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097. https://doi.org/10.1371/journal.pmed.1000097
Eide PK, Hansson H-A (2020) Blood-brain barrier leakage of blood proteins in idiopathic normal pressure hydrocephalus. Brain Res 1727:146547. https://doi.org/10.1016/j.brainres.2019.146547
Close LN, Zanaty M, Kirby P, Dlouhy BJ (2019) Acute hydrocephalus resulting from neuromyelitis optica: a case report and review of the literature. World Neurosurg 129:367–371. https://doi.org/10.1016/j.wneu.2019.05.177
Arighi A, Di Cristofori A, Fenoglio C et al (2019) Cerebrospinal fluid level of aquaporin4: a new window on glymphatic system involvement in neurodegenerative disease? JAD 69:663–669. https://doi.org/10.3233/JAD-190119
Castañeyra-Ruiz L, Hernández-Abad LG, Carmona-Calero EM et al (2019) AQP1 overexpression in the CSF of obstructive hydrocephalus and inversion of its polarity in the choroid plexus of a Chiari malformation type II case. J Neuropathol Exp Neurol 78:641–647. https://doi.org/10.1093/jnen/nlz033
Hamamoto Filho PT, Fogaroli MO, Oliveira MAC et al (2019) A rat model of neurocysticercosis-induced hydrocephalus: chronic progressive hydrocephalus with mild clinical impairment. World Neurosurg 132:e535–e544. https://doi.org/10.1016/j.wneu.2019.08.085
Long C-Y, Huang G-Q, Du Q et al (2019) The dynamic expression of aquaporins 1 and 4 in rats with hydrocephalus induced by subarachnoid haemorrhage. FN 57:182–195. https://doi.org/10.5114/fn.2019.86296
Hasan-Olive MM, Enger R, Hansson H-A et al (2019) Pathological mitochondria in neurons and perivascular astrocytic endfeet of idiopathic normal pressure hydrocephalus patients. Fluids Barriers CNS 16:39. https://doi.org/10.1186/s12987-019-0160-7
Hasan-Olive MM, Enger R, Hansson H-A et al (2019) Loss of perivascular aquaporin-4 in idiopathic normal pressure hydrocephalus. Glia 67:91–100. https://doi.org/10.1002/glia.23528
Trillo-Contreras JL, Ramírez-Lorca R, Hiraldo-González L et al (2018) Combined effects of aquaporin-4 and hypoxia produce age-related hydrocephalus. Biochimica et Biophysica Acta (BBA) Mol Basis Dis 1864:3515–3526. https://doi.org/10.1016/j.bbadis.2018.08.006
Jeon T, Park K-S, Park S-H et al (2017) Expression of aquaporin 1 and 4 in the choroid plexus and brain parenchyma of kaolin-induced hydrocephalic rats. Korean J Neurotrauma 13:68. https://doi.org/10.13004/kjnt.2017.13.2.68
Eide PK, Hansson H-A (2017) Astrogliosis and impaired aquaporin-4 and dystrophin systems in idiopathic normal pressure hydrocephalus. Neuropathol Appl Neurobiol 44:474–490. https://doi.org/10.1111/nan.12420
Limbrick DD, Baksh B, Morgan CD et al (2017) Cerebrospinal fluid biomarkers of infantile congenital hydrocephalus. PLoS ONE 12:e0172353. https://doi.org/10.1371/journal.pone.0172353
Guo Y, Weigand SD, Popescu BF et al (2017) Pathogenic implications of cerebrospinal fluid barrier pathology in neuromyelitis optica. Acta Neuropathol 133:597–612. https://doi.org/10.1007/s00401-017-1682-1
Schmidt MJ, Rummel C, Hauer J et al (2016) Increased CSF aquaporin-4, and interleukin-6 levels in dogs with idiopathic communicating internal hydrocephalus and a decrease after ventriculo-peritoneal shunting. Fluids Barriers CNS 13:12. https://doi.org/10.1186/s12987-016-0034-1
Gu W, Li F, Zhang PJ (2016) Expression and significance of aquaporin protein in Sprague–Dawley rats after experimental intraventricular hemorrhage. Cell Mol Biol 62:59–62. https://doi.org/10.14715/cmb/2016.62.4.11
Castañeyra-Ruiz L, González-Marrero I, Carmona-Calero EM et al (2016) Cerebrospinal fluid levels of tumor necrosis factor alpha and aquaporin 1 in patients with mild cognitive impairment and idiopathic normal pressure hydrocephalus. Clin Neurol Neurosurg 146:76–81. https://doi.org/10.1016/j.clineuro.2016.04.025
Ortega E, Muñoz RI, Luza N et al (2016) The value of early and comprehensive diagnoses in a human fetus with hydrocephalus and progressive obliteration of the aqueduct of Sylvius: case report. BMC Neurol 16:45. https://doi.org/10.1186/s12883-016-0566-7
Blasco E, Martorell J, De la Fuente C, Pumarola M (2014) Immunohistochemical study of aquaporins in an African Grey Parrot (Psittacus erithacus) with hydrocephalus. J Avian Med Surg 28:309–315. https://doi.org/10.1647/2013-059
Sveinsdottir S, Gram M, Cinthio M et al (2014) Altered expression of aquaporin 1 and 5 in the choroid plexus following preterm intraventricular hemorrhage. Dev Neurosci 36:542–551. https://doi.org/10.1159/000366058
Castañeyra-Ruiz L, González-Marrero I, González-Toledo JM et al (2013) Aquaporin-4 expression in the cerebrospinal fluid in congenital human hydrocephalus. Fluids Barriers CNS 10:18. https://doi.org/10.1186/2045-8118-10-18
Skjolding AD, Holst AV, Broholm H et al (2013) Differences in distribution and regulation of astrocytic aquaporin-4 in human and rat hydrocephalic brain: AQP4 in human and rat hydrocephalic brain. Neuropathol Appl Neurobiol 39:179–191. https://doi.org/10.1111/j.1365-2990.2012.01275.x
Roales-Buján R, Páez P, Guerra M et al (2012) Astrocytes acquire morphological and functional characteristics of ependymal cells following disruption of ependyma in hydrocephalus. Acta Neuropathol 124:531–546. https://doi.org/10.1007/s00401-012-0992-6
Aghayev K, Bal E, Rahimli T et al (2012) Aquaporin-4 expression is not elevated in mild hydrocephalus. Acta Neurochir 154:753–759. https://doi.org/10.1007/s00701-011-1241-9
Paul L, Madan M, Rammling M et al (2011) Expression of aquaporin 1 and 4 in a congenital hydrocephalus rat model. Neurosurgery 68:462–473. https://doi.org/10.1227/NEU.0b013e3182011860
Wang D, Nykanen M, Yang N et al (2011) Altered cellular localization of aquaporin-1 in experimental hydrocephalus in mice and reduced ventriculomegaly in aquaporin-1 deficiency. Mol Cell Neurosci 46:318–324. https://doi.org/10.1016/j.mcn.2010.10.003
Skjolding AD, Rowland IJ, Søgaard LV et al (2010) Hydrocephalus induces dynamic spatiotemporal regulation of aquaporin-4 expression in the rat brain. Fluids Barriers CNS 7:20. https://doi.org/10.1186/1743-8454-7-20
Tourdias T, Dragonu I, Fushimi Y et al (2009) Aquaporin 4 correlates with apparent diffusion coefficient and hydrocephalus severity in the rat brain: a combined MRI—histological study. NeuroImage 47:659–666. https://doi.org/10.1016/j.neuroimage.2009.04.070
Smith ZA, Moftakhar P, Malkasian D et al (2007) Choroid plexus hyperplasia: surgical treatment and immunohistochemical results: case report. J Neurosurg Pediatr 107:255–262. https://doi.org/10.3171/PED-07/09/255
Shen XQ, Miyajima M, Ogino I, Arai H (2006) Expression of the water-channel protein aquaporin 4 in the H-Tx rat: possible compensatory role in spontaneously arrested hydrocephalus. J Neurosurg Pediatr 105:459–464. https://doi.org/10.3171/ped.2006.105.6.459
Mao X, Enno TL, Del Bigio MR (2006) Aquaporin 4 changes in rat brain with severe hydrocephalus. Eur J Neurosci 23:2929–2936. https://doi.org/10.1111/j.1460-9568.2006.04829.x
Longatti P, Basaldella L, Orvieto E et al (2006) Aquaporin(s) expression in choroid plexus tumours. Pediatr Neurosurg 42:228–233. https://doi.org/10.1159/000092359
Bloch O, Auguste KI, Manley GT, Verkman A (2006) Accelerated progression of kaolin-induced hydrocephalus in aquaporin-4-deficient mice. J Cereb Blood Flow Metab 26:1527–1537. https://doi.org/10.1038/sj.jcbfm.9600306
Oshio K, Watanabe H, Song Y et al (2005) Reduced cerebrospinal fluid production and intracranial pressure in mice lacking choroid plexus water channel aquaporin-1. FASEB J 19:76–78. https://doi.org/10.1096/fj.04-1711fje
Clardy SL, Lucchinetti CF, Krecke KN et al (2014) Hydrocephalus in neuromyelitis optica. Neurology 82:1841–1843. https://doi.org/10.1212/WNL.0000000000000428
Gratton S, Mora C (2013) Unexplained hydrocephalus in a patient with neuromyelitis optica. In: Proceedings of the 2012 North American Neuro-Ophthalmology Society, San Antonio, TX, USA
Eide PK, Eidsvaag VA, Nagelhus EA, Hansson H-A (2016) Cortical astrogliosis and increased perivascular aquaporin-4 in idiopathic intracranial hypertension. Brain Res 1644:161–175. https://doi.org/10.1016/j.brainres.2016.05.024
Leinonen V, Koivisto AM, Savolainen S et al (2010) Amyloid and tau proteins in cortical brain biopsy and Alzheimer’s disease. Ann Neurol 68:446–453. https://doi.org/10.1002/ana.22100
Golomb J, Wisoff J, Miller DC et al (2000) Alzheimer’s disease comorbidity in normal pressure hydrocephalus: prevalence and shunt response. J Neurol Neurosurg Psychiatry 68:778–781. https://doi.org/10.1136/jnnp.68.6.778
Tarasoff-Conway JM, Carare RO, Osorio RS et al (2015) Clearance systems in the brain—implications for Alzheimer disease. Nat Rev Neurol 11:457–470. https://doi.org/10.1038/nrneurol.2015.119
Kress BT, Iliff JJ, Xia M et al (2014) Impairment of paravascular clearance pathways in the aging brain: paravascular clearance. Ann Neurol 76:845–861. https://doi.org/10.1002/ana.24271
Reeves BC, Karimy JK, Kundishora AJ et al (2020) Glymphatic system impairment in Alzheimer’s disease and idiopathic normal pressure hydrocephalus. Trends Mol Med 26:285–295. https://doi.org/10.1016/j.molmed.2019.11.008
Bateman GA (2013) Hypertensive slit ventricle syndrome: pseudotumor cerebri with a malfunctioning shunt? JNS 119:1503–1510. https://doi.org/10.3171/2013.7.JNS13390
Hamilton K, Koueik J, Maganti R, Iskandar B (2019) Slit ventricle syndrome leads to 10-year history of repetitive transient central herniation masquerading as seizures: hydrocephalus case report. World Neurosurg 126:134–138. https://doi.org/10.1016/j.wneu.2019.02.106
Sivaganesan A, Krishnamurthy R, Sahni D, Viswanathan C (2012) Neuroimaging of ventriculoperitoneal shunt complications in children. Pediatr Radiol 42:1029–1046. https://doi.org/10.1007/s00247-012-2410-6
Del Bigio MR, Di Curzio DL (2016) Nonsurgical therapy for hydrocephalus: a comprehensive and critical review. Fluids Barriers CNS. https://doi.org/10.1186/s12987-016-0025-2
Funding
The authors declare that they have no sources of funding.
Author information
Authors and Affiliations
Contributions
Concept of the article: AC, CL. Literature search and data analysis: CL, AC. Draft of the article: AC, CL, AA. Critically revision of the article: all authors.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest/competing interests.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Integrity of research and reporting
The manuscript does not contain clinical studies or patient data.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
de Laurentis, C., Cristaldi, P., Arighi, A. et al. Role of aquaporins in hydrocephalus: what do we know and where do we stand? A systematic review. J Neurol 268, 4078–4094 (2021). https://doi.org/10.1007/s00415-020-10122-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-020-10122-z