Abstract
Objective and design
Whether combining intravenous thrombolysis (IVT) and mechanical thrombectomy (MT) is superior to mechanical thrombectomy alone for large vessel occlusion acute ischemic stroke is still uncertain. Our aim was to compare the safety and the efficacy of these two therapeutic strategies.
Materials
Patients with acute ischemic stroke secondary to anterior circulation large vessel occlusion.
Methods
A retrospective analysis was conducted. IVT was performed with full dose recombinant tissue plasminogen activator. MT alone was performed only if intravenous thrombolysis was contraindicated. Primary outcomes were successful reperfusion, 3-month functional independence, symptomatic intracranial hemorrhage (sICH), and 3-month mortality.
Results
325 patients were analyzed: 193 treated with combined IVT and MT, 132 with MT alone. The combined treatment group showed higher systolic blood pressure (140 [80–230] vs 150 [90–220]; p = 0.036), rate of good collaterals (55.9% vs 67%; p = 0.03), use of aspiration devices (68.2% vs 79.3%; p = 0.003) and shorter onset-to-reperfusion time (300 [90–845] vs 288 [141–435]; p = 0.008). No differences were found in the efficacy and safety outcomes except for mortality which was lower in the combined treatment group (36.4% vs 25.4%; p = 0.02). However, after multivariable analysis combined treatment was not associated with lower mortality (OR 1.47; 95% CI 0.73–2.96; p = 0.3).
Conclusions
Our study suggests that mechanical thrombectomy alone is effective and safe in patients with contraindications to intravenous thrombolysis. Preceding use of IVT in eligible patients was not associated with increased harm or benefit. Randomized controlled trials are needed to clarify whether intravenous thrombolysis before mechanical thrombectomy is associated with additional benefit.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Randomized endovascular stroke trials have clearly shown the efficacy of mechanical thrombectomy (MT) combined to intravenous thrombolysis (IVT) compared to IVT alone for the treatment of acute ischemic stroke (AIS) secondary to large vessel occlusion (LVO) [1,2,3,4,5]. These trials have opened new perspectives of AIS management in the next future. A recent meta-analysis showed that the number needed to treat with MT to reduce disability by at least one level on modified Rankin scale (mRS) is 2.6 and that the effect size favoring MT over control persists also in patients ineligible for IVT [6]. In line with these findings, a recent randomized controlled trial, the diffusion-weighted imaging or computerized tomography perfusion assessment with clinical mismatch in the triage of wake up and late presenting strokes undergoing neurointervention with Trevo (DAWN) trial, demonstrated the efficacy and safety of MT between 6 and 24 h after stroke onset [7]. Whether treatment with IVT before MT is necessary in LVO stroke is highly controversial. We compared the safety and efficacy outcomes between patients treated with IVT and MT (IVMT) and those treated with MT alone (MT).
Materials and methods
A retrospective analysis of patients with anterior circulation AIS consecutively collected from our prospective endovascular stroke registry (August 2009–June 2017) was performed. Patients were selected based on following current treatment guidelines criteria: (1) proximal occlusion of MCA or anterior cerebral artery (ACA) or terminal ICA (tICA), or proximal ICA in combination to an intracranial vessel on CT-angiography (CTA) confirmed on conventional angiography; (2) groin puncture within 6 h from symptom onset or Alberta Stroke Program Early CT score (ASPECTS) ≥ 6; (3) pre-stroke modified Rankin Scale (mRS) ≤ 2; (4) available 3-month follow-up [8,9,10]. IVT was administered within 4.5 h after stroke onset at a full dose (recombinant tissue plasminogen activator 0.9 mg/kg, 10% as a bolus and the remaining in 1-h infusion) without delay in the beginning of endovascular procedure [8,9,10]. MT alone was employed only if IVT was contraindicated, as listed in Table 1. Patients treated with pharmacological intra-arterial thrombolysis used in addition to mechanical thrombectomy were included in the analysis. Via transfemoral access, intracranial thrombectomy was performed with a coaxial system. An intermediate aspiration catheter was then advanced till the target vessel and aspiration was performed manually or with dedicated aspiration pump. The choice of device (stentriever or aspiration) was at discretion of the neurointerventionalist.
Baseline characteristics including age, sex, NIHSS, vascular risk factors, type of intracranial occlusion, procedural details, ASPECTS on non-contrast CT [11], collaterals on pre-treatment CTA. Collaterals were independently assessed by two investigators (E.P. and S.F.) using a scale from 0 to 3 derived from the prolyse in Acute Cerebral Thromboembolism (PROACT) II trial (0: no collaterals; 1: collaterals to the periphery of ischemia; 2: collaterals filling 50%-100% of ischemic area; 3: collaterals filling 100% of ischemic area) [12], blinded to the treatment arm and clinical outcome. Thereafter, collateral score was dichotomized in poor (0–1) and good (2–3). The validity of this dichotomization has been already shown [13]. Successful reperfusion was defined as TICI ≥ 2b [14] and complete reperfusion as TICI 3, according to the thrombolysis in cerebral infarction (TICI) grading. Hemorrhagic complications were defined according to the European Cooperative Acute Stroke Study criteria (no hemorrhage, hemorrhagic infarction-1, hemorrhagic infarction-2, parenchymal hematoma-1, parenchymal hematoma-2) [15] and symptomatic ICH (sICH) as a hemorrhage associated with an increase of at least 4 points in the NIHSS. HT on follow-up NCCT was assessed independently and retrospectively by two investigators (G. K. and F. A.) blinded to the treatment arm and clinical outcome. Other outcome measures included 24-h clinical improvement defined as a reduction of at least 4 points in the NIHSS or an NIHSS of 0, 3-month functional independence defined as mRS ≤ 2 and 3-month mortality. The study was approved by the local ethics committee. Informed consent was obtained from all patients or their relatives for treatment and for the study.
Statistical analysis
All data were initially entered into an EXCEL database (Microsoft, Redmond, Washington, USA) and the analysis was performed using the Stata/IC version 13 (StataCorp 2013, College Station, TX, USA). Descriptive statistics consisted of means ± standard deviation (SD) or medians with range for parameters with Gaussian distributions (after confirmation with histograms and the Kolmogorov–Smirnov test) or frequencies (%) as appropriate. Comparison of continuous variables was performed by means of Student’s t test or Mann–Whitney U test. Comparison of categorical variables was performed by means of Fisher’s exact test. Variables with a p value < 0.2 in univariate analysis were further tested in a multivariable analysis using logistic regression analysis. A p value of < 0.05 was considered statistically significant.
Results
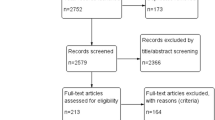
Among 414 patients with LVO ischemic stroke, 89 were excluded and 325 patients were included in our analysis (Fig. 1). Of those, 193 were treated with IVMT and 132 were treated with MT. Supplementary table 1 shows the distribution of treated patients over the study period. Baseline and demographic characteristics are shown in Table 2. The two groups differed for lower rate of diabetes (21.5% vs 11.5%; p = 0.01), higher systolic blood pressure (140 [80–230] vs 150 [90–220]; p = 0.036) and higher rate of good collaterals (55.9% vs 67%; p = 0.03) in the IVMT group. Table 3 summarizes the procedural characteristics. The two groups differed for the higher use of thromboaspiration devices (68.2 vs 79.3; p = 0.003) and shorter onset-to-reperfusion time (300 [90–845] vs 288 [141–435]; p = 0.008) in the IVMT group. 1 patient in the IVMT and 5 patients in the MT group were treated beyond 6 h after symptom onset because of favorable imaging (ASPECTS ≥ 6).
The analysis of safety and efficacy outcomes revealed no significant difference in the rate of successful reperfusion, sICH and 3-month functional independence. Mortality at 3 months was lower in the IVMT group (36.4% vs 25.4%; p = 0.02) (Table 4). Complete reperfusion was higher in the IVMT group (44% vs 56%; p = 0.02). After logistic regression analysis adjusted for age and NIHSS, IVMT remained associated with lower mortality (OR 2, 95% 1.1–3.4, p = 0.009). However, this association did not remain significant when we included collateral status and successful reperfusion in the multivariable model (p = 0.07). When we included all variables with a p value < 0.2 in univariate analysis, age (OR 1.00; 95% CI 092-0.98; p = 0.001), successful reperfusion (OR 0.38; 95% CI 0.19–0.77; p = 0.007), 24-h clinical improvement (OR 0.31; 95% CI 0.15–0.65; p = 0.002), sICH (OR 5.0; 95% CI 2.0–12.7; p = 0.001), atrial fibrillation (OR 2.18; 95% CI 1.11–4.29; p = 0.024), collateral status (OR 0.39; 95% CI 0.20–0.75; p = 0.005) and baseline glycemia (OR 1.0; 95% CI 0.98–1.0; p = 0.018) were associated with higher mortality, whereas, treatment strategy (OR 0.76; 95% CI 0.4–1.48; p = 0.4) was not.
Discussion
In this retrospective analysis of a large prospective registry of LVO ischemic stroke, the safety and efficacy of MT were not significantly different in patients treated with MT alone or combined IVT and MT. Mechanical thrombectomy alone appeared to be a valid option for AIS patients ineligible for IVT. The apparent safer profile with lower mortality found in the IVMT group was not confirmed after adjustment for confounding factors. However, our data showed that combining IVT to MT did not result in an increased risk of sICH. Recent studies comparing MT and IVMT have shown contrasting results in terms of safety and efficacy [16,17,18]. In a recent metanalysis showing better safety and efficacy outcomes for combined treatment, IVMT represented 60% of all treatments [18]. The lower use of MT alone in randomized and non-randomized studies could be explained as a result of the current 6-h time window with the first 4.5 h for IVMT and the last 1.5 h for direct MT [8,9,10]. This proportion is likely going to change after the results of the DAWN and DEFUSE 3 trials [7, 19]. Of note, our results are in line with those from the study by Coutinho et al. which is the only based on randomized controlled data to date [16]. Differently from this study, we found shorter onset-to-reperfusion time in the IVMT group. This finding was not affected by the site of the occlusion since no differences were found between groups, including in the rate of tandem occlusions which are known to an independent predictor of poor outcome [20, 21]. Despite shorter reperfusion time (12 min earlier) and higher rate of complete reperfusion (absolute difference = 12%) in the IVMT group, this did not translate in different outcomes. Our data revealed a higher use of aspiration catheters compared to stent-retrievers. This could be explained by the availability of different devices throughout the study period and by the cost-effectiveness of aspiration catheters.
Although we cannot exclude that the higher mortality rate found in the MT group may be related to the pre-existing IVT contraindications with possible severe comorbidities and poorer prognosis [22], our results also suggested an association with the higher rate of recanalization and good collaterals in the IVMT group.
The unanswered question of whether IVT prior to endovascular clot retrieval is beneficial for LVO stroke is currently of high interest in clinical practice. The reasons are numerous: (1) IVT increases the risk of ICH and systemic bleeding without definite increase chances of recanalization; (2) IVT might limit the use of antiplatelets or anticoagulants, especially in the hyperacute phase; MT without IVT has no contraindications when delivered in the appropriate time window for LVO stroke.
Our “real-world” results suggest that combining IVT with MT for AIS is not harmful and that MT alone for AIS patients with contraindication to IVT is effective and safe. In addition, if early post-treatment antithrombotic prevention is required, MT alone could be a safe and effective alternative option.
Our study has several limitations. First, its retrospective design and relatively small sample size. Second, assignment to MT group was based on contraindications to IVT which might have affected our results. These contraindications included: late presentation, use of oral anticoagulants, recent major surgery and recent gastrointestinal bleeding, which could have made patients more fragile. In a recent study comparing bridging thrombolysis and direct MT in eligible-IVT patients, the final decision on treatment approach was individualized on a case-by-case basis at the discretion of the team of neurologists and neuroradiologists [23]. This approach may lead to significant delays in pre-treatment workflow and biased assignment group with a likely increase in cohort heterogeneity. Third, this was a single-center study, and therefore, generalizability of results should be cautious. Nonetheless, our analyses are not affected by treatment protocol heterogeneity deriving from multicenter experience. Fourth, the two groups differed for lower rate of diabetes, higher SBP and rate of good collaterals in the IVMT group. However, admission glycemia, which has been shown to be a strong predictive factor of outcome [24], was not different between groups. Furthermore, a recent post hoc analysis from the Multicenter Randomized Clinical Trial of Endovascular Treatment of Acute Ischemic Stroke in the Netherlands (MR CLEAN) showed that blood pressure did not affect the benefit or safety of MT in AIS patients [25]. Concerning collaterals, it is of note that such a favorable condition in the IVMT group did not translate into a better clinical outcome. Fifth, as shown in Fig. 1, 44 patients were excluded from our analysis because of missing 3-month follow-up data. This could have affected our results. One of the strengths of our study is that all patients in the combined group were treated with full dose recombinant tissue plasminogen activator and thus results were unlikely affected by IVT dose. There are several ongoing randomized controlled clinical trials which are aiming to compare combined IVT and MT vs MT alone (MR CLEAN-NO IV, DIRECT-SAFE and SWIFT-DIRECT) in patients eligible for intravenous thrombolysis. Pending these results, our findings demonstrated that MT alone is effective and safe in patients with contraindications to intravenous thrombolysis. Preceding use of IVT in eligible patients was not associated with increased harm or benefit.
In conclusions, we found no differences in 3-month functional independence and rate of any or symptomatic ICH between combined IVT and MT and MT alone in patients with LVO anterior circulation ischemic stroke. Quicker reperfusion time observed in the combined treatment group needs further research. Results from the ongoing clinical trials may clarify whether IVT is associated with an additional benefit in MT patients eligible for intravenous thrombolysis.
References
Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ et al (2015) A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 372:11–20. https://doi.org/10.1056/NEJMoa1411587
Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N et al (2015) Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 372:1009–1018. https://doi.org/10.1056/NEJMoa1414792
Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J et al (2015) Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 372:1019–1030. https://doi.org/10.1056/NEJMoa1414905
Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM et al (2015) Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 372:2285–2295. https://doi.org/10.1056/NEJMoa1415061
Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A et al (2015) Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 372:2296–2306. https://doi.org/10.1056/NEJMoa1503780
Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM et al (2016) Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 387:1723–1731. https://doi.org/10.1016/S0140-6736(16)00163-X
Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P et al (2018) Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med 378:11–21. https://doi.org/10.1056/NEJMoa1706442
Powers WJ, Derdeyn JP, Biller J, Coffey CS, Hoh BL, Jauch EC et al (2015) 2015 American Heart Association/American Stroke Association Focused Update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment. Stroke 46:3020–3035
Demaerschalk BM, Kleindorfer DO, Adeoye OM, Demchuk AM, Fugate JE, Grotta JC et al (2016) Scientific rationale for the inclusion and exclusion criteria for intravenous alteplase in acute ischemic stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 47:581–641. https://doi.org/10.1161/STR.0000000000000086
Wahlgren N, Moreira T, Michel P, Steiner T, Jansen O, Cognard C et al (2016) Mechanical thrombectomy in acute ischemic stroke: consensus-statement by Eso-Karolinska Stroke Update 2014/2015, supported by ESO/ESMINT, ESNR and EAN. Int J Stroke 11:134–147
Barber PA, Demchuk AM, Zhang J, Buchan AM (2000) Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS Study Group. Alberta Stroke Programme Early CT Score. Lancet 355:1670–1674
Tan JC, Dillon WP, Liu S, Adler F, Smith WS, Wintermark M (2007) Systematic comparison of perfusion-CT and CT-angiography in acute stroke patients. Ann Neurol 61:533–543. https://doi.org/10.1002/ana.21130
Sallustio F, Motta C, Pizzuto S, Diomedi M, Giordano A, D’Agostino VC et al (2017) CT angiography-based collateral flow and time to reperfusion are strong predictors of outcome in endovascular treatment of patients with stroke. J Neurointerv Surg 9:940–943. https://doi.org/10.1136/neurintsurg-2016-012628
Zaidat OO, Yoo AJ, Khatri P, Tomsick TA, von Kummer R, Saver JL et al (2013) Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke 44:2650–2663. https://doi.org/10.1161/STROKEAHA.113.001972
Hacke W, Kaste M, Fieschi C, Toni D, Lesaffre E, von Kummer R et al (1995) Intravenous thrombolysis with recombinant tissue plasminogen activator for acute hemispheric stroke. The European Cooperative Acute Stroke Study (ECASS). JAMA 274:1017–1025
Coutinho JM, Liebeskind DS, Slater LA, Nogueira RG, Clark W, Dávalos A et al (2017) Combined intravenous thrombolysis and thrombectomy vs thrombectomy alone for acute ischemic stroke: a pooled analysis of the SWIFT and STAR studies. JAMA Neurol 74:268–274. https://doi.org/10.1001/jamaneurol.2016.5374
Abilleira S, Ribera A, Cardona P, Rubiera M, López-Cancio E, Amaro S et al (2017) Outcomes after direct thrombectomy or combined intravenous and endovascular treatment are not different. Stroke 48:375–378. https://doi.org/10.1161/STROKEAHA.116.015857
Mistry EA, Mistry AM, Nakawah MO, Chitale RV, James RF, Volpi JJ et al (2017) Mechanical thrombectomy outcomes with and without intravenous thrombolysis in stroke patients: a meta-analysis. Stroke 48:2450–2456. https://doi.org/10.1161/STOKEAHA.117.017320
Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S et al (2018) Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. New Engl J Med 378:708–718. https://doi.org/10.1056/NEJMoa1713973
Sallustio F, Motta C, Koch G, Pizzuto S, Campbell BC, Diomedi M et al (2017) Endovascular stroke treatment of acute tandem occlusion: a single-center experience. J Vasc Interv Radiol 28:543–549. https://doi.org/10.1016/j.jvir.2017.01.007
Rubiera M, Ribo M, Delgado-Mederos R, Santamarina E, Delgado P, Montaner J et al (2006) Tandem internal carotid artery/middle cerebral artery occlusion: an independent predictor of poor outcome after systemic thrombolysis. Stroke 37:2301–2305. https://doi.org/10.1161/01.STR.0000237070.80133.1d
Szymanski FM, Lip GY, Filipiak KJ, Platek AE, Hrynkiewicz-Szymanska A, Opolski G (2015) Stroke risk factors beyond the CHA2DS2-VASc score: can we improve our identification of “high stroke risk” patients with atrial fibrillation? Am J Cardiol 116:1781–1788. https://doi.org/10.1016/j.amjcard.2015.08.049
Broeg-Morvay A, Mordasini P, Bernasconi C, Bühlmann M, Pult F, Arnold M et al (2016) Direct mechanical intervention versus combined intravenous and mechanical intervention in large artery anterior circulation stroke: a matched-pairs analysis. Stroke 47:1037–1044. https://doi.org/10.1161/STROKEAHA.115.011134
Flint AC, Xiang B, Gupta R, Nogueira RG, Lutsep HR, Jovin TG et al (2013) THRIVE score predicts outcomes with a third-generation endovascular stroke treatment device in the TREVO-2 trial. Stroke 44:3370–3375. https://doi.org/10.1161/STROKE.AHA.113.002796
Mulder MJHL, Ergezen S, Lingsma HF, Berkhemer OA, Fransen PSS, Beumer D et al (2017) Baseline blood pressure effect on the benefit and safety of intra-arterial treatment in MR CLEAN (multicenter randomized clinical trial of endovascular treatment of acute ischemic stroke in The Netherlands). Stroke 48:1869–1876. https://doi.org/10.1161/STOKEAHA.116.01625
Acknowledgements
This work was supported by the Italian Ministry of Health (RF-2013-02358679). We are grateful to Caterina Motta MD, Francesco Mori MD, Simone Napolitano, Domenico Samà MD, Barbara Rizzato MD, Vittoria Carla D’Agostino MD, Angela Giordano MD, Marta Panella MD, Alessandro Davoli MD for collection of data.
Funding
None in study design, collection, analysis and interpretation of data, writing and decision to submit the article for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None of the authors has conflict of interest to declare.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sallustio, F., Koch, G., Alemseged, F. et al. Effect of mechanical thrombectomy alone or in combination with intravenous thrombolysis for acute ischemic stroke. J Neurol 265, 2875–2880 (2018). https://doi.org/10.1007/s00415-018-9073-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-018-9073-7