Abstract
Objective
Spinal and bulbar muscular atrophy (SBMA) is caused by an abnormal expansion of the CAG repeat in the androgen receptor gene. This study aimed to systematically phenotype a German SBMA cohort (n = 80) based on laboratory markers for neuromuscular, metabolic, and endocrine status, and thus provide a basis for the selection of biomarkers for future therapeutic trials.
Methods
We assessed a panel of 28 laboratory parameters. The clinical course and blood biomarkers were correlated with disease duration and CAG repeat length. A subset of 11 patients was evaluated with body fat MRI.
Results
Almost all patients reported muscle weakness (99%), followed by dysphagia (77%), tremor (76%), and gynecomastia (75%) as major complaints. Creatine kinase was the most consistently elevated (94%) serum marker, which, however, did not relate with either the disease duration or the CAG repeat length. Paresis duration and CAG repeat length correlated with dehydroepiandrosterone sulfate after correction for body mass index and age. The androgen insensitivity index was elevated in nearly half of the participants (48%).
Conclusions
Metabolic alterations in glucose homeostasis (diabetes) and fat metabolism (combined hyperlipidemia), and sex hormone abnormalities (androgen insensitivity) could be observed among SBMA patients without association with the neuromuscular phenotype. Dehydroepiandrosterone sulfate was the only biomarker that correlated strongly with both weakness duration and the CAG repeat length after adjusting for age and BMI, indicating its potential as a biomarker for both disease severity and duration and, therefore, its possible use as a reliable outcome measure in future therapeutic studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinal and bulbar muscular atrophy (SBMA), also known as Kennedy’s disease, is an adult-onset lower motor neuron disorder with an X-linked inheritance pattern. SBMA is characterized by late-onset, slowly progressive weakness, atrophy and fasciculations of the bulbar and limb skeletal musculature. SBMA is caused by the abnormal expansion of an unstable CAG repeat in the coding region of the androgen receptor gene (AR) [1]; more than > 38 repeats produce the fully penetrant disease phenotype [2]. Clinical features, especially muscle strength, and testosterone levels show an association with disease severity [3]. Insulin resistance has also been postulated to serve as potential therapeutic target because of its association with disease severity [4]. Establishing the causality of the SBMA mutation and its molecular pathophysiology helped to identify a range of potential therapeutic targets (for reviews, see [5,6,7]). Encouraging results from animal trials based on androgen reduction led to independent clinical trials focused on hormonal interventions in SBMA [8, 9]. Katsuno and colleagues tested the therapeutic potential of leuprorelin, a gonadotropin-lowering drug that reduces testicular testosterone production [9]. Fernandes–Rhodes investigated the effect of the anti-androgen dutasteride [8]. While both trials failed to demonstrate a clear therapeutic benefit for androgen-lowering therapies, an urgent need for objective outcome measures became apparent [10].
The CAG repeat encodes a polyglutamine tract in the androgen receptor, and its size correlates with age of onset but not disease progression rate [11,12,13,14,15]. The effects of the mutation fall into two categories: loss of (androgen receptor) function causes androgen insensitivity with gynecomastia and decreased fertility, while (androgen-dependent) toxic gain of function is thought to causally underlie motor neuron degeneration [16]. Metabolic abnormalities are frequently reported, albeit without any current consensus on whether they rely on gain or loss of androgen receptor function. Hormonal and biochemical studies have reported creatine kinase (CK) elevation, dyslipidemia, glucose intolerance, and partial androgen insensitivity with increased testosterone and luteinizing hormone (LH) [17,18,19,20,21,22]. Partial androgen resistance is present in more than 80% of patients [15]. Hypertriglyceridemia may be related to mitochondrial disturbances [23] and androgen receptor insensitivity. CK elevation is considered to be due to myopathic disease secondary to motor neuron degeneration [21, 24, 25]. The present study aimed to characterize a large SBMA cohort with regard to laboratory markers for neuromuscular disease, metabolic and hormonal status, thereby providing a rational basis for the selection of potential biomarkers in future therapeutic trials.
Methods
Inclusion criteria were genetically confirmed SBMA and consent to the study; exclusion criteria were inability to provide detailed information on personal history, symptoms, and co-medication. Patients opting to participate in the imaging arm of the study had to be able to undergo MRI studies. Eighty genetically confirmed SBMA patients were recruited through the German neuromuscular referral centers in the Universities of Berlin, Bochum, Dresden, Halle, Hannover, Rostock, Ulm, and Würzburg. Blood samples and information about their disease history and characteristics, comorbidities, medication, neurological, metabolic, and endocrine symptoms were obtained in structured personal interviews. The patients completed a standardized questionnaire addressing the presentation of specific aspects: muscle weakness (onset), muscle cramps, body mass index (BMI), myalgia, family history, tremor, sensory deficits, comorbidities, dysphagia, dysarthria, gynecomastia, and respiratory symptoms. Laboratory parameters were divided into hormones and lipid and glucose metabolism markers. Parameters were considered “elevated” if they fell outside the established reference range. Disease onset was defined age at the first (any) symptom. Fasting blood samples were collected under standardized conditions between 8 and 10 AM and analyzed for glucose, HbA1c, insulin, C peptide, proinsulin, aspartate transaminase (AST), alanine transaminase (ALT), CK, cholesterol, triglycerides, HDL cholesterol, LDL cholesterol, 17-OH progesterone, androstendione, cortisol, dehydroepiandrosterone (DHEA), DHEA sulfate, follicle stimulating hormone (FSH), luteinizing hormone (LH), testosterone, estradiol, progesterone, prolactin, SHBG, plasminogen activator inhibitor (PAI), growth hormone, insulin like growth factor 1 (IGF-1), and insulin like growth factor 1 binding protein 3 (IGF1BP3).
Ethical approval of the Ulm University Hospital ethics board was obtained for all participants (protocol no. 73/10 and 92/10). Written informed consent was obtained from all participants.
A subgroup of 11 patients (58 ± 12 years, range 40–79 years) from the Ulm center received a total body fat MRI. For comparison, total body fat MRI data from a group of 29 male healthy controls (65 ± 12 years, range 53–81 years) were selected from our database.
Genetic testing was performed by PCR-based fragment analysis according to the standard procedures [1, 26]. CAG repeat length > 38 was considered diagnostic for SBMA.
MRI acquisitions
Adipose tissue volumes were quantified by MRI performed on a 1.5-T whole-body imager (Symphony, Siemens Medical, Erlangen, Germany), as described previously [27,28,29]. Briefly, measures of visceral (VFT) and subcutaneous (SFT) abdominal fat tissue were determined as the sum of VFT voxels from the top of the liver to the femoral heads inside the abdominal muscular wall, and as the sum of fat tissue voxels underneath the skin layer surrounding the abdomen from the top of the liver to the femur heads. VFT, SFT, and total fat tissue (TFT = VFT + SFT) volumes were expressed in dm3 and normalized to the body height.
Statistics
Statistical analyses were performed using GraphPad Prism 6 for Windows (GraphPad Software, Inc., La Jolla, CA, USA) and SAS, version 9.4 (SAS Institute, Chicago, IL, USA). Relations between CAG repeat length and age-at-onset of weakness as well as age-at-onset of any first symptom were analyzed using linear regression and Pearson’s correlation coefficient “r” and associated p values were calculated. The positively skewed homeostasis model assessment of insulin resistance (HOMA-IR) was log-transformed for analysis. A multiple linear regression analysis was conducted to adjust for age and BMI. Statistical significance was set at p < 0.05. Results from all tests were considered exploratory, in keeping with the study design, and therefore, no adjustment for multiple testing was done [30].
Results
Cohort characteristics
The reported mean age-at-onset (any symptom) was 39.1 ± 15.4 years (10.0–75.0 years). The mean disease duration at inclusion was 17.0 ± 11.6 years (range 2.0–47.0 years, age at inclusion 55.9 ± 10.5 years, range 25.0–80.0 years). The mean age-at-weakness-onset was 44.4 ± 12.0 years (25.0–75.0) and the mean length of the CAG expansion in AR was 46.2 ± 3.3 (range 39.0–55.0). The most common symptoms reported were muscle weakness (99%), followed by dysphagia (77%), tremor (76%), gynecomastia (75%), muscle cramps (71%), dysarthria (64%), sensory deficits/tingling (64%), myalgia (57%), and respiratory symptoms (34%). The mean BMI was 26.1 ± 4.4 kg/m2 (17.5–40.2). Dot plots of samples in relation with reference range for all biomarkers are summarized in Fig. 1.
CK was the laboratory value most consistently elevated above the reference range (mean 1053 ± 900 U/l, range 124–6140 U/l) and was elevated in 94% of participants. However, no correlations with CAG repeat length, disease duration, or onset of weakness were noted.
Relation with CAG repeat length and disease duration
Biomarker correlation with CAG repeat length
Given that polyglutamine diseases and SBMA in particular show dependence on CAG repeat length, we probed the correlation between repeat expansion length and laboratory parameters. The age-at-weakness-onset was inversely correlated with the CAG repeat expansion length (r = − 0.72; p < 0.0001) (Fig. 2a). The age-of-gynecomastia-onset (mean 30.0 ± 15.4 years, range 12.0–70.0) and the age-at-first-disease-symptom were also related to the CAG repeat length (r = − 0.59; p < 0.0001 in Fig. 2b; r = − 0.66; p < 0.0001 in Fig. 2c). No such correlation was observed for BMI (r = − 0.18; p = 0.1204).
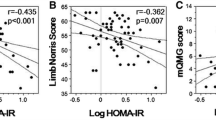
With regard to hormones, CAG repeat length correlated with androstendion (r = 0.27; p = 0.017), DHEA (r = 0.36; p = 0.005), DHEA sulfate (r = 0.49; p < 0.0001), and estradiol (r = 0.27; p = 0.017). HbA1c was inversely correlated with CAG repeat length but not with paresis or disease duration. IGF1BP3 also significantly correlated with CAG repeat length (r = 0.38; p = 0.0004). Figure 3 details the results for selected correlations.
After correction for age and BMI in a multiple linear regression model, only DHEA sulfate significantly correlated with CAG repeat length (r = 0.59; p = 0.0022); no significant correlations were observed for androstendion, DHEA, and estradiol. However, IGF1BP3 tended towards a significant correlation with CAG repeat length (r = 0.55; p = 0.066).
Correlation of biomarkers with disease duration
Significant correlations for all laboratory markers were tested with disease duration. A multiple linear regression model was used to rule out correlations that might manifest as a result of ageing, BMI or metabolic syndromes; subsequently, none of the tested laboratory values significantly correlated with disease duration (age-at-onset of any first symptom).
With respect to the duration from paresis onset, the following biomarkers were related significantly to duration of weakness: IGF1BP3 (r = 0.24; p = 0.03), FSH (r = 0.29; p = 0.01) and DHEA sulfate (r = 0.26; p = 0.02). In the multiple linear regression model, only DHEA sulfate (r = 0.3; p = 0.0478) related with duration after weakness-onset.
Endocrine parameters
We screened for a panel of endocrinological parameters that may be altered by SBMA-associated androgen insensitivity to test their potential as disease markers.
Gynecomastia was observed in 75% of participants. SHBG and androstendione were elevated in 48 and 38% of patients, respectively, while fasting morning cortisol level was elevated in 24%. The Androgen Sensitivity Index (ASI) (which reflects androgen resistance) was increased in 48% of patients (detailed in Table 1).
DHEA sulfate levels correlated significantly with duration of paresis in the multiple linear regression model with adjustment for age and BMI.
Lipid and glucose metabolism
Assessed lipid metabolism parameters revealed hypercholesterinemia, increased triglycerides, and increased LDL-cholesterol levels in 78, 56, and 66% respectively. Details are shown in Table 2.
An analysis of glucose metabolism-related parameters revealed increased C peptide, indicating the production of high levels of endogenous insulin with concomitant insulin resistance. Of the 42 patients with increased C peptide, only 4 showed increased HbA1c. A history of diabetes mellitus was reported in 9/80 patients (11.3%). Of these diabetic, six had elevated C peptide, four had increased insulin levels, and five patients had increased HbA1c. Eight of these nine diabetic patients took oral antidiabetics. With regard to the entire patient cohort, C peptide was increased in 53%, insulin levels in 11% and glucose in 29% of patients. A similar percentage of patients also had reduced fasting glucose levels (28%). HbA1c was increased without a history of diabetes in three patients. No correlation between HbA1c and weakness duration was observed; however, HbA1c was inversely correlated with CAG repeat length, even after correcting for age and BMI (Table 3). We calculated the insulin resistance index HOMA-IR, which was elevated in 35 patients of our cohort (44%). Log HOMA-IR did not correlate with disease duration and duration of weakness or CAG repeat length (r = − 0.19, p = 0.09). Log HOMA-IR was significantly related to other laboratory markers, i.e., triglycerides (r = 0.44, p < 0.01), HDL (r = − 0.45, p < 0.01), growth factor (r = 0.23, p = 0.04), IGF1 (r = 0.25, p = 0.02), estradiole (r = − 0.36, p < 0.01), testosterone (r = − 0.44, p < 0.01), SHBG (r = − 0.39, p < 0.01), C-peptide (r = 0.82, p < 0.01), insulin (r = 0.70, p < 0.01), proinsulin (r = 0.58, p < 0.01), and Hba1c (r = 0.27, p = 0.03). Log HOMA-IR also correlated with BMI (r = 0.48, p < 0.01). After correction for age and BMI in a multiple linear regression model, all laboratory markers with exception of growth factor still significantly correlated with HOMA-IR (Table 3).
Skeletal muscle
Although CK was elevated in 94% of the patients, it did not correlate with any of the aforementioned markers. AST and ALT were concomitantly elevated in 47% (mean 54.59 ± 27.09 U/l, range 20.00–202.00) and 68% (mean 61.82 ± 29.13 U/l, range 9.00–178.00) of cases, respectively. None of the patients displayed any elevation in either IGF1 or IGF1BP-3 values; values below normal are detailed in Table 2. IGF1BP3 significantly correlated with duration of weakness, but this correlation did not reach statistical significance after correcting for age and BMI (p = 0.16).
Body fat Imaging
Between-group comparisons of body fat composition
This cross-sectional MRI study included 11 SBMA patients and 29 appropriately matched controls. Body fat distribution was evaluated at the group level (Fig. 4); no significant differences were observed for either TFT (18.7 ± 7.9 l/m for SBMA vs. 18.3 ± 6.4 l/m for controls) or SFT (12.9 ± 6.0 l/m for SBMA vs. 15.2 ± 5.9 l/m for controls). However, patients had significantly higher VFT (5.8 ± 2.6 l/m for SBMA vs. 3.1 ± 1.7 l/m for controls, p < 0.007) (Fig. 4); SBMA patients had a significantly higher VFT/SFT ratio (0.51 ± 0.23 l/m for SBMA vs. 0.22 ± 0.1 l/m for controls, p < 0.001).
a Individual example of an MRI subset after post-processing. Sagittal, coronal, and axial slices. Visceral fat tissue volume (VFT): green; subcutaneous fat tissue volume (SFT): red. b Comparison of fat volumes between 11 SBMA patients and 29 matched controls. No significant between-group differences were observed for subcutaneous and total fat tissue volume but were observed for visceral fat tissue volume and the quotient between SFT and VFT volume
CAG repeat length positively correlated with the amount of subcutaneous fat. The proportion of subcutaneous fat relative to both visceral and whole-body fat increased with disease duration and progression rate. Of the assessed serum markers, body fat was associated with increased triglycerides, insulin, C peptide, HbA1c, plasminogen activator inhibitor (PAI), and low HDL-cholesterol. With respect to glucose metabolism markers (insulin, C peptide, HbA1c, PAI), the proportion of visceral fat increases in the entirely enlarged fat mass (Fig. 4).
Discussion
The recent negative results reported by SBMA clinical trials have highlighted the urgent need for rationally selected and objective outcome measures [10]. Given the multifaceted nature of the disease and clinical presentation that encompasses neuromuscular, metabolic, and endocrinological abnormalities, we attempted to fully characterize a large German cohort of genetically confirmed SBMA patients.
CK, a well-established indicator of muscle integrity, was by far the most consistently elevated disease marker, potentially indicating skeletal muscle involvement. Although not novel, this finding reaffirms and underscores skeletal muscle’s centrality as a site of SBMA disease pathology, thereby also emphasizing its significance as a potential therapeutic target [31,32,33]. Previous biopsy studies have reported a combination of denervation and myopathy [34, 35]. The elevation of CK also corroborated the self-reported clinical status of the patients, for whom weakness, cramping, and myalgia were the most common complaints. Surprisingly, no correlation of CK with either CAG repeat length or weakness duration was observed.
We must also point out the possibility of recollection bias within the clinical data reported, as there were collected via patient interviews. Another limitation of our study is the absence of an age-matched control group with either healthy subjects or patients with other muscular atrophies, as some of the laboratory values may be influenced by age and muscle mass. No longitudinal observation of the mentioned biomarkers is so far available which may be important for the validation of the correlations.
On one hand, we hypothesize that the mutated androgen receptor may correlate with the disease and/or paresis duration with a concomitant longitudinal worsening of symptoms. Indeed, DHEA sulfate, FSH, and IGF1BP3 positively correlated with the duration of muscle weakness, albeit with only the DHEA sulfate correlation reaching significance after correction for age and BMI. DHEA sulfate is an indicator of adrenal androgen production and its upregulation in our patients likely reflects an increased androgen insensitivity. The clinical signs of androgen insensitivity include gynecomastia, testicular atrophy, in addition to decreased fertility. Abdominal obesity is common [36]. Therefore, DHEA sulfate might reflect androgen insensitivity, which might become more pronounced during the progression of the disease. Conversely, no correlation of disease duration with the ASI (product of LH and testosterone) was observed.
This phenomenon has also been reported by previous studies, where ASI was elevated in 36% [17] of the cohort with testosterone, LH and FSH also elevated (10, 27, and 32%, respectively), but no correlations between testosterone/ASI values and CAG repeat length or age-at-onset were observed. A recent Chinese study with 155 patients reported similar laboratory values for testosterone but much higher estradiole levels [36] relative to our cohort. On the other hand, a correlation of disease symptoms or biomarkers may also correlate with CAG repeat length. Androstendion, DHEA, DHEA sulfate, estradiol, and IGF1BP3 were the only parameters positively correlating with CAG repeat length, but as before, only DHEA sulfate reached significance after correction for age and BMI. No correlation with CAG repeat length for either the ASI or testosterone values was observed.
Most notably, lipid markers (cholesterol and LDL cholesterol) were elevated in 78 and 66%, respectively, indicating dysregulated lipid metabolism in SBMA. Ni and colleagues reported similarly elevated triglycerides (66%), although elevated cholesterol was noted in only 22% of their Chinese cohort [22]. These discrepancies may be attributed to a variety of factors ranging from nutritional influences to ethnic background. Body fat MRI, which has not been reported elsewhere for SBMA patients, revealed higher visceral fat volumes compared to controls and a higher proportion of visceral fat compared to subcutaneous fat. This may reflect an effect of hyperlipidemia; curiously, this has also been reported in patients with amyotrophic lateral sclerosis, the most frequently occurring motor neuron disease [37].
The high percentage of C-peptide elevation points to a higher proportion of patients with insulin resistance, albeit without any manifestation of diabetes. HbA1c values and diabetes did not correlate with either symptom or weakness duration, but were inversely correlated with CAG repeat length. Since manifest diabetic patients were also included, reduced HbA1c with higher CAG repeats may reflect adequately managed diabetes treatment. Hypercholesterinemia and insulin resistance are core features of the metabolic syndrome, but in SBMA, these changes do not appear to be a function of disease duration. Log HOMA-IR is described to correlate with BMI, obesity-related indices, HDL, and testosterone [4]. We could reproduce these laboratory findings and expand to other insulin resistance associated biomarkers, namely, triglycerides, IGF1,
SHBG and C peptide as well as proinsulin. Any association of log HOMA-IR to CAG repeat length or disease/weakness duration was missing. The binding protein 3 of insulin like growth factor 1 (IGF1BP3) positively correlated with CAG repeat length, but did not reach significance when corrected for age and BMI. IGF1 has been reported to block toxicity of the androgen receptor at its binding position and to attenuate neuromuscular symptoms when it is overexpressed in a mouse model of SBMA [20, 31] In SBMA mouse models, muscle-specific overexpression of the anabolic hormone IGF-1 improves both functional outcomes and overall survival [20, 38]. IGF1 elevation may, therefore, be interpreted as an organism’s rescue mechanism and is reported to be increased with muscle exercise [39]. In our study, it was not identified as a biomarker for disease duration or polyglutamine expansion.
Inverse associations between CAG repeat length and age of onset, muscle strength, and testosterone levels have been previously reported in SBMA [2, 12]. Similar to other trinucleotide repeat diseases, the longer the CAG repeat, the earlier the onset and the more pronounced the disease severity are reported. Evidence for an association between several tested laboratory parameters and either disease duration or repeat length remains limited. It is possible that reported hormonal and metabolic disturbances may also be influenced by factors like physical activity and/or nutrition.
The present study identified DHEA sulfate as a potential biomarker, given that it correlated well with both CAG repeat length and paresis duration. We recommend the re-evaluation of IGF1BP3 within a larger cohort, given that it tended towards a positive albeit insignificant correlation with both repeat length and weakness duration.
Conclusions
Here, we report a range of laboratory parameters that are altered in SBMA patients. Most common were high CK values, followed by elevated AST and ALT, diabetic or pre-diabetic glucose metabolism and hyperlipidemia. Sex hormone levels were compatible with a picture of mild androgen insensitivity as shown by high levels of androgens and estradiol. Although many laboratory parameters were consistently elevated in this cohort, these did not correlate with any included clinical symptoms or phenotypical SBMA features (disease severity and duration). In a multiple linear regression analysis with correction for age and BMI, only DHEA sulfate correlated with the paresis duration and CAG repeat length. Therefore, DHEA sulfate may serve as an informative laboratory marker for disease severity.
References
La Spada AR, Wilson EM, Lubahn DB, Harding AE, Fischbeck KH (1991) Androgen receptor gene mutations in X-linked spinal and bulbar muscular atrophy. Nature 352(6330):77–79
Tanaka F, Reeves MF, Ito Y et al (1999) Tissue-specific somatic mosaicism in spinal and bulbar muscular atrophy is dependent on CAG-repeat length and androgen receptor–gene expression level. Am J Hum Genet 65(4):966–973
Rhodes LE, Freeman BK, Auh S et al (2009) Clinical features of spinal and bulbar muscular atrophy. Brain 132(Pt 12):3242–3251
Nakatsuji H, Araki A, Hashizume A, Hijikata Y, Yamada S, Inagaki T, Suzuki K, Banno H, Suga N, Okada Y, Ohyama M, Nakagawa T, Kishida K, Funahashi T, Shimomura I, Okano H, Katsuno M, Sobue G (2017) Correlation of insulin resistance and motor function in spinal and bulbar muscular atrophy. J Neurol 264(5):839–847
Katsuno M, Banno H, Suzuki K, Adachi H, Tanaka F, Sobue G (2012) Molecular pathophysiology and disease-modifying therapies for spinal and bulbar muscular atrophy. Arch Neurol 69:436–440
Rocchi A, Pennuto M (2013) New routes to therapy for spinal and bulbar muscular atrophy. J Mol Neurosci 50:514–523
Fischbeck KH (2012) Developing treatment for spinal and bulbar muscular atrophy. Prog Neurobiol 99(3):257–261
Fernández-Rhodes LE, Kokkinis AD, White MJ et al (2011) Efficacy and safety of dutasteride in patients with spinal and bulbar muscular atrophy: a randomised placebo-controlled trial. Lancet Neurol. 10(2):140–147
Katsuno M, Tanaka F, Adachi H et al (2012) Pathogenesis and therapy of spinal and bulbar muscular atrophy (SBMA). Prog Neurobiol 99(3):246–256
Weydt P, Sagnelli A, Rosenbohm A, Pradat P-F, Ludolph AC, Pareyson D (2015) Clinical trials in spinal and bulbar muscular atrophy-past, present, and future. J Mol Neurosci 58(3):379–387
Atsuta N, Watanabe H, Ito M et al (2006) Natural history of spinal and bulbar muscular atrophy (SBMA): a study of 223 Japanese patients. Brain 129(Pt 6):1446–1455
Igarashi S, Tanno Y, Onodera O et al (1992) Strong correlation between the number of CAG repeats in androgen receptor genes and the clinical onset of features of spinal and bulbar muscular atrophy. Neurology. 42(12):2300–2302
Lee J-H, Shin J-H, Park K-P et al (2005) Phenotypic variability in Kennedy’s disease: implication of the early diagnostic features. Acta Neurol Scand 112(1):57–63
Sperfeld AD, Karitzky J, Brummer D et al (2002) X-linked bulbospinal neuronopathy: Kennedy disease. Arch Neurol 59(12):1921–1926
Dejager S (2002) A comprehensive endocrine description of Kennedy’s disease revealing androgen insensitivity linked to cag repeat length. J Clin Endocrinol Metab 87(8):3893
Katsuno M, Adachi H, Kume A et al (2002) Testosterone reduction prevents phenotypic expression in a transgenic mouse model of spinal and bulbar muscular atrophy. Neuron 35(5):843–854
Querin G, Bertolin C, Da Re E et al (2015) Non-neural phenotype of spinal and bulbar muscular atrophy: results from a large cohort of Italian patients. J Neurol Neurosurg Psychiatr. 87(8):810–816
Pennuto M, Greensmith L, Pradat P-F et al (2015) 210th ENMC International Workshop: research and clinical management of patients with spinal and bulbar muscular atrophy, 27–29 March, 2015, Naarden, The Netherlands. Neuromuscul Disord 25:802–812
Grunseich C, Kats IR, Bott LC et al (2014) Early onset and novel features in a spinal and bulbar muscular atrophy patient with a 68 CAG repeat. Neuromuscul Disord 24(11):978–981
Palazzolo I, Stack C, Kong L et al (2009) Overexpression of IGF-1 in muscle attenuates disease in a mouse model of spinal and bulbar muscular atrophy. Neuron 63(3):316–328
Mariotti C, Castellotti B, Pareyson D et al (2000) Phenotypic manifestations associated with CAG-repeat expansion in the androgen receptor gene in male patients and heterozygous females: a clinical and molecular study of 30 families. Neuromuscul Disord 10(6):391–397
Ni W, Chen S, Qiao K, Wang N, Wu Z-Y (2015) Genotype-phenotype correlation in Chinese patients with spinal and bulbar muscular atrophy. PLoS One 10(3):e0122279
Ranganathan S, Harmison GG, Meyertholen K, Pennuto M, Burnett BG, Fischbeck KH (2008) Mitochondrial abnormalities in spinal and bulbar muscular atrophy. Hum Mol Genet 18(1):27–42
Harding AE, Thomas PK, Baraitser M, Bradbury PG, Morgan-Hughes JA, Ponsford JR (1982) X-linked recessive bulbospinal neuronopathy: a report of ten cases. Brain 45(11):1012–1019
Amato AA, Prior TW, Barohn RJ, Snyder P, Papp A, Mendell JR (1993) Kennedy’s disease: a clinicopathologic correlation with mutations in the androgen receptor gene. Neurology. 43(4):791–794
Doyu M, Sobue G, Mukai E et al (1992) Severity of X-linked recessive bulbospinal neuronopathy correlates with size of the tandem CAG repeat in androgen receptor gene. Ann Neurol 32:707–710
Müller H-P, Raudies F, Unrath A, Neumann H, Ludolph AC, Kassubek J (2010) Quantification of human body fat tissue percentage by MRI. NMR Biomed 24(1):17–24
Lindauer E, Dupuis L, Müller H-P, Neumann H, Ludolph AC, Kassubek J (2013) Adipose tissue distribution predicts survival in amyotrophic lateral sclerosis. PLoS One 8(6):e67783
Fischer K, Moewes D, Koch M et al (2015) MRI-determined total volumes of visceral and subcutaneous abdominal and trunk adipose tissue are differentially and sex-dependently associated with patterns of estimated usual nutrient intake in a northern German population. Am J Clin Nutr 101(4):794–807
Proschan MA, Waclawiw MA (2001) Practical guidelines for multiplicity adjustment in clinical trials. Control Clin Trials 21(6):527–539
Rinaldi C, Bott LC, Fischbeck KH (2014) Muscle matters in Kennedy’s disease. Neuron 82(2):251–253
Cortes CJ, Ling S-C, Guo LT et al (2014) Muscle expression of mutant androgen receptor accounts for systemic and motor neuron disease phenotypes in spinal and bulbar muscular atrophy. Neuron 82(2):295–307
Lieberman AP, Yu Z, Murray S et al (2014) Peripheral androgen receptor gene suppression rescues disease in mouse models of spinal and bulbar muscular atrophy. Cell Rep. 7(3):774–784
Sorarù G, Hashizume Y, Mukai E, Hirayama M, Mitsuma T, Takahashi A et al (1989) X-linked recessive bulbospinal neuronopathy. A clinicopathological study. Brain 112(1):209–232 (Pt 1)
Sorarù G, D’Ascenzo C, Polo A et al (2007) Spinal and bulbar muscular atrophy: skeletal muscle pathology in male patients and heterozygous females. J Neurol Sci 264(1–2):100–105
Sinclair R, Greenland KJ, van Egmond S, Hoedemaker C, Chapman A, Zajac JD (2007) Men with Kennedy disease have a reduced risk of androgenetic alopecia. Br J Dermatol 157(2):290–294
Lindauer E, Dupuis L, Hüller HP, Neumann H, Ludolph AC, Kassubek J (2013) Adipose tissue distribution predicts survival in amyotrophic lateral sclerosis. PLoS One 27(8):e67783. https://doi.org/10.1371/journal.pone.0067783
Papanikolaou T, Ellerby LM (2009) IGF-1: elixir for motor neuron diseases. Neuron 63(3):277–278
Fischbeck KH (2015) Spinal and bulbar muscular atrophy overview. J Mol Neurosci 58(3):317–320
Acknowledgements
We thank Nicola Laemmle for her excellent work as a study nurse and for her assistance with sample collection and Nayana Gaur for the critical reading of the manuscript.
Funding
This study was funded partly by the German Network of ALS (BMBF 01GM1103A).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical approval
All persons gave their informed consent prior to their inclusion in the study. The study was approved by the local ethics committee of the University of Ulm (73/10 and 92/10).
Rights and permissions
About this article
Cite this article
Rosenbohm, A., Hirsch, S., Volk, A.E. et al. The metabolic and endocrine characteristics in spinal and bulbar muscular atrophy. J Neurol 265, 1026–1036 (2018). https://doi.org/10.1007/s00415-018-8790-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-018-8790-2