Abstract
A prognostic biomarker that can provide a good prediction of prognosis in patients with intracerebral hemorrhage (ICH) would be beneficial in guiding the initial management decisions in the setting of ICH. N-terminal pro-brain natriuretic peptide (NT-proBNP) is a biomarker of prognosis in patients with cardiovascular disease and ischemic stroke. However, the prognostic role of NT-proBNP in patients with spontaneous ICH is still a controversial issue. This study aimed to determine the prognostic value of NT-proBNP in patients with spontaneous ICH. A total of 132 patients from 571 ICH cases in inpatient settings were enrolled in this study. Blood samples from each subject were obtained and analyzed for NT-proBNP on admission and on days 4 and 7. The first end point was functional outcome at discharge, which was dichotomized into favorable or unfavorable; the secondary end point was mortality within 6 months after ICH. Compared with the baseline levels on admission after ICH, the NT-proBNP levels increased markedly on day 4 (P < 0.05). Multivariate logistic regression analysis indicated that the NT-proBNP level on day 4, the ICH score, and the APACHE II score were independent prognostic factors of functional outcome and 6-month mortality in ICH patients. A cutoff NT-proBNP level of 999.85 pg/ml predicted an unfavorable functional outcome (with 66.1% sensitivity and 98.7% specificity) and 6-month mortality (with 93.8% sensitivity and 92.0% specificity) in ICH patients. Thus, the NT-proBNP level on day 4 was found to be a powerful prognostic predictor of functional outcome and 6-month mortality in ICH patients, which would be beneficial to guiding the initial management decisions in the setting of ICH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite advances in medical technology, intracerebral hemorrhage (ICH) is still a common and devastating disease associated with high morbidity and mortality rates. Prognostic biomarkers that can provide a good prediction of prognosis in patients with ICH would be beneficial to guiding the initial management decisions in the setting of ICH.
Brain natriuretic peptide (BNP) and N-terminal pro-brain natriuretic peptide (NT-proBNP) have been identified as predictive biomarkers of cardiovascular disease, such as systolic and diastolic dysfunction, acute coronary syndrome, and left ventricular (LV) dysfunction [1,2,3]. NT-proBNP is a circulating precursor of BNP. It has a longer half-life, which makes it more sensitive in detecting early stage LV dysfunction [4]. Recent studies have shown that the serum NT-proBNP level is increased in patients hospitalized for acute cerebral lesions, such as traumatic brain injury (TBI), subarachnoid hemorrhage (SAH), and ischemic stroke [5,6,7,8,9].
In patients with acute ischemic stroke, NT-proBNP has been shown to be a strong predictor of in-hospital mortality [10]. However, studies on the association between serum NT-proBNP concentration and ICH are lacking, and the role of NT-proBNP in evaluating the prognosis of patients with ICH remains a controversial issue. The present research was designed to determine the prognostic value of NT-proBNP in patients with ICH, in terms of functional outcome at discharge and mortality within 6 months.
Methods
Patients
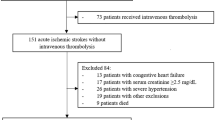
This prospective, observational, multicenter cohort study was carried out in four hospitals in the People’s Republic of China. A total of 571 ICH patients were recruited from August 2015 to July 2016. No additional interventions were done in the treatment of the recruited subjects. The criteria for inclusion in the research were: isolated ICH confirmed by computed tomography scanning, 18 years old or above, admitted within 8 h of ICH onset, and surviving for at least 7 days after admission. The patients excluded from the study were those with a history of endocrine disease, renal insufficiency, heart disease (such as congestive heart failure and coronary ischemia), and multiple organ dysfunction and those with neurologic symptomatology caused by TBI, brain tumors, cerebrovascular malformation, SAH, and ischemic stroke. According to the above-mentioned inclusion and exclusion criteria, 132 patients from 571 ICH cases in inpatient settings were enrolled. Treatment of ICH was done according to the Guidelines for Spontaneous ICH published in 2015 [11].
Date collection and measurement
The baseline characteristics of the patients were collected from their hospital records. These included: gender, hematoma location, hematoma volume, ICH score, age, ICH volume, intraventricular involvement, supratentorial versus infratentorial origin, Glasgow Coma Scale (GCS) score, Acute Physiology and Chronic Health Evaluation (APACHE) II score (age, history of severe organ insufficiency or being immunocompromised, GCS score, rectal temperature, heart rate, respiratory rate, oxygenation, mean arterial pressure, arterial pH, leukocyte count, hematocrit, serum sodium, potassium, and creatinine), the average length of hospital stay before discharge and other parameters. Similarly to previous researches [12,13,14], the ICH, GCS, and APACHE II scores were assessed on the day of admission. Blood samples from each subject were obtained and analyzed for NT-proBNP. To decrease the bias caused by daytime variation, the serum NT-proBNP was measured at the time of enrollment and at 6 a.m. on days 4 and 7 after admission. NT-proBNP was detected with the use of an electrochemiluminescence immunoassay (Roche Diagnostics GmbH, Sandhofer Strasse 116, D-68305 Mannheim, Germany). According to the information provided by the manufacturer, the measurement range was 5–35,000 pg/ml, and the reference range for ages 50–75 years was 0–900 pg/ml. To minimize any non-blinded outcome assessment bias, the medical laboratory technologists were blinded to the information on all patients.
End points
The first end point was functional outcome at discharge, which was dichotomized into favorable or unfavorable based on the Glasgow Outcome Score (GOS). A favorable outcome was defined as a GOS score of 4 or 5, whereas an unfavorable outcome was defined as a GOS score of 1–3. The secondary end point was mortality within 6 months after ICH. Follow-up data were collected monthly through telephone interviews with the patients or their next of kin.
Statistical analysis
Normally distributed continuous variables were expressed as mean ± standard deviation (\( \bar{x} \) ± SD), and non-normally distributed variables as medians and confidence intervals. Categorical variables were expressed as percentages. For normally distributed continuous variables, an independent samples t test was used to compare the differences between the two groups, and a Chi-square test was applied to analyze enumeration data. Data with skewed distributions were analyzed by using the Mann–Whitney U test or the Kruskal–Wallis test. Univariate and multivariate logistic regression analyses were carried out to identify the prognostic factors predicting outcomes. In the multivariate logistic regression analysis, the clinical variables, such as the ICH score, APACHE II score, and NT-proBNP level, were entered as number scores. The “method” chosen was “Enter”. A receiver operating characteristic (ROC) analysis was applied to determine the cutoff NT-proBNP level (with the highest sum of specificity and sensitivity) for the prognosis of ICH. Statistical significance was defined as P < 0.05. All statistical analyses were done by using SPSS version 20.0 for Windows (SPSS Inc, Chicago, IL).
Results
Patient characteristics
This study included 132 cases from 571 ICH patients: 62 men and 70 women, with ages ranging from 50 to 74 years. None of the patients suffered cardiac infarction or heart failure during the study, and no patient was lost to follow-up. 56 cases had an unfavorable functional outcome at discharge, and 32 patients died within 6 months. Table 1 shows the clinical characteristics of the patients, including gender, hematoma location/volume, ICH score, APACHE II score, and average length of hospital stay before discharge.
Temporal development of serum NT-proBNP levels
The NT-proBNP levels showed a marked increase after ICH. Compared with the measurements on the two other days, the mean NT-proBNP level on day 1 was significantly lower (426.50 ± 224.10 pg/ml; 95% CI 387.92–465.09; P < 0.001 and P = 0.017, respectively). The mean plasma NT-proBNP level was 745.95 ± 428.89 pg/ml on day 4 (95% CI 672.10–819.80), which was significantly higher than the average levels of 426.50 ± 224.10 pg/ml (95% CI 387.92–465.09; P < 0.001) and 522.93 ± 292.08 pg/ml (95% CI 387.92–465.09; P < 0.001) on days 1 and 7, respectively (Fig. 1).
NT-proBNP levels and functional outcome
The serum NT-proBNP levels on days 1, 4, and 7 in patients with favorable functional outcomes (GOS 4 or 5) were significantly lower than those in patients with unfavorable functional outcomes (GOS 1–3): 302.09 ± 81.37 versus 595.35 ± 245.29 pg/ml (95% CI of the difference, 233.65–352.88; P < 0.001), 503.51 ± 126.75 pg/ml versus 1074.98 ± 474.10 pg/ml (95% CI of the difference, 458.92–684.03; P < 0.001), and 366.17 ± 85.03 pg/ml versus 735.68 ± 336.58 pg/m (95% CI of the difference, 289.98–449.03; P < 0.001), respectively (Fig. 2a). The univariate logistic regression analysis showed that the serum NT-proBNP levels on days 1, 4, and 7, the ICH score, and the APACHE II score were prognostic indicators of functional outcome. The multivariate logistic regression analysis indicated that the serum NT-proBNP level on day 4, the ICH score, and the APACHE II score were independent prognostic factors of functional outcome (Table 2). The ROC curve analysis showed that the area under the curve (AUC) for the NT-proBNP level on day 4 was 0.838 (95% CI 0.762–0.915; P < 0.001). By applying the cutoff NT-proBNP level (999.85 pg/ml), the sensitivity and specificity of the NT-proBNP levels in predicting the functional outcome were obtained as 66.1 and 98.7%, respectively (Fig. 2b).
a Serum NT-proBNP levels and functional outcomes of ICH patients. b The receiver operating characteristics curve was constructed to determine the cutoff level of NT-proBNP for an unfavorable functional outcome. The cutoff level of 999.85 pg/ml showed a sensitivity of 66.1% and a specificity of 98.7%. The area under the curve was 0.838
NT-proBNP levels and mortality
Compared with those in survivors, the NT-proBNP levels in non-survivors on days 1, 4, and 7 were significantly higher: 719.08 ± 178.45 versus 332.88 ± 141.28 pg/ml (95% CI of the difference, 325.54–446.86; P < 0.001), 1366.24 ± 344.78 versus 547.46 ± 204.99 pg/ml (95% CI of the difference, 720.07–917.49; P < 0.001), and 910.60 ± 280.50 versus 398.88 ± 155.32 pg/m (95% CI of the difference, 434.29–589.15; P < 0.001), respectively (Fig. 3a). In the univariate logistic regression analysis, the prognostic indicators of 6-month mortality after ICH included the serum NT-proBNP levels on days 1, 4, and 7, the ICH score, and the APACHE II score. In the multivariate logistic regression analysis, however, only the NT-proBNP level on day 4, the ICH score, and the APACHE II score were independently associated with 6-month mortality after ICH (Table 2). The AUC for the NT-proBNP level on day 4 was 0.958 (95% CI 0.907–1.000; P < 0.001) (Fig. 3b); the sensitivity of the NT-proBNP cutoff level of 999.85 pg/ml was 93.8%, with a specificity of 92.0%.
a Serum NT-proBNP levels and 6-month mortality of ICH patients. b The receiver operating characteristics curve was constructed to determine the cutoff level of NT-proBNP for 6-month mortality. The cutoff level of 999.85 pg/ml showed a sensitivity of 93.8% and a specificity of 92.0%. The area under the curve was 0.958
Discussion
To our knowledge, this is the first prospective study specifically designed to evaluate the prognostic value of NT-proBNP in patients with ICH. As shown in the results, the plasma concentrations of NT-proBNP increased markedly after ICH, and the increases in serum NT-proBNP levels were more common in patients who had an unfavorable functional outcome at discharge and who died within 6 months after ICH. The multivariate logistic regression analysis indicated that the NT-proBNP level on day 4 was an independent predictor of functional outcome and 6-month mortality in patients with ICH.
In the early stage of ICH, various hormones, such as natriuretic peptide, are involved in the pathophysiologic process of neurologic injury [15]. In a previous study, the median level of plasma BNP was shown to be significantly higher in non-survivors than in survivors, and a plasma BNP of >60.0 pg/ml was found to be independently associated with mortality within 1 month after ICH [16]. Because of its longer half-life and stable biological characteristics, NT-proBNP, which is secreted in equivalent proportion to BNP, seems to be more convenient for clinical detection. Previous works have indicated that increased NT-proBNP levels in patients with acute coronary syndrome or LV dysfunction were associated with poor prognosis [1,2,3]. On the other hand, several cohort studies have shown that NT-proBNP levels were increased early and markedly after acute brain injury, such as ischemic stroke, as well as SAH, and were associated with poor short-term prognosis for these patients [10, 17].
However, there are few studies on the prognostic role of NT-proBNP in patients with ICH. In the present work, patients with other diseases leading to increased NT-proBNP levels were excluded; the serum NT-proBNP levels were found to increase markedly after ICH, which was consistent with the results of Nyberg et al. [17]. Further, a significant increase in serum NT-proBNP concentrations was found in patients who had an unfavorable functional outcome at discharge and who died within 6 months after ICH; this finding was in accordance with previous studies, which showed that NT-proBNP was correlated with the severity and prognosis of neurologic injury [10].
In the current study, the plasma NT-proBNP levels were measured on days 1, 4, and 7 because our previous work showed that the plasma NT-proBNP levels increased progressively and markedly at least in the first 4 days after ICH, reached a peak level on the fourth day, and then decreased gradually [18]. The univariate logistic regression analysis indicated that the serum NT-proBNP levels on days 1, 4, and 7 were prognostic indicators of clinical outcome. However, the multivariate logistic regression analysis indicated that, compared with the measurements on the other days, only the serum NT-proBNP concentration on day 4 was a powerful independent prognostic factor of functional outcome and mortality in ICH patients. A possible explanation for this finding is that the serum NT-proBNP levels in the acute stage of ICH are closely correlated to the severity of neurologic injury [5, 10]; the secondary brain edema after ICH, which peaks at around day 3 and decreases by day 7, is well known to be the major cause of deterioration of neurologic function.
In this research, the AUC was used to determine the diagnostic value of the NT-proBNP level on day 4 in patients with ICH. In predicting the 6-month mortality after ICH, the AUC for the NT-proBNP on day 4 was greater than 0.9, with high sensitivity (93.8%) and specificity (92.0%); in the prediction of neurologic function, the AUC was slightly less than 0.9 (0.838), suggesting that the NT-proBNP concentration on day 4 after ICH is a powerful prognostic biomarker of clinical outcome, including 6-month mortality, in patients with ICH.
The present work has several limitations that need to be considered. First, the small sample size limits the generalizability of the findings to all ICH patients. Second, selection bias exists in that the biomarker was measured in patients surviving at least 7 days after admission rather than in all patients, including those who died within 3 days after ICH. In addition, other factors that might account for the increased serum NT-proBNP levels during the study could not be completely excluded, which might have caused bias in the results. Finally, the first end point of this study was functional outcome at discharge rather than after rehabilitation at home; the latter would have allowed for the possibility of more patients ultimately obtaining favorable functional outcomes after rehabilitation. Mortality data on long-term follow-up of the patients are needed in future studies.
Conclusion
The present study clearly showed that the serum NT-proBNP concentrations increased markedly and progressively after ICH. The increase in serum NT-proBNP levels was more common in patients with poor clinical outcomes. The NT-proBNP level on day 4 was shown to be a powerful prognostic predictor of functional outcome and 6-month mortality in patients with ICH.
References
McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, Falk V, Filippatos G, Fonseca C, Gomez-Sanchez MA, Jaarsma T, Køber L, Lip GY, Maggioni AP, Parkhomenko A, Pieske BM, Popescu BA, Rønnevik PK, Rutten FH, Schwitter J, Seferovic P, Stepinska J, Trindade PT, Voors AA, Zannad F, Zeiher A, Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology, Bax JJ, Baumgartner H, Ceconi C, Dean V, Deaton C, Fagard R, Funck-Brentano C, Hasdai D, Hoes A, Kirchhof P, Knuuti J, Kolh P, McDonagh T, Moulin C, Popescu BA, Reiner Z, Sechtem U, Sirnes PA, Tendera M, Torbicki A, Vahanian A, Windecker S, McDonagh T, Sechtem U, Bonet LA, Avraamides P, Ben Lamin HA, Brignole M, Coca A, Cowburn P, Dargie H, Elliott P, Flachskampf FA, Guida GF, Hardman S, Iung B, Merkely B, Mueller C, Nanas JN, Nielsen OW, Orn S, Parissis JT, Ponikowski P, ESC Committee for Practice Guidelines (2012) ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 14:803–869
Morrow DA, Cannon CP, Jesse RL, Newby LK, Ravkilde J, Storrow AB, Wu AH, Christenson RH, National Academy of Clinical Biochemistry Laboratory Medicine Practice Guidelines (2007) National Academy of Clinical Biochemistry Laboratory Medicine Practice Guidelines: clinical characteristics and utilization of biochemical markers in acute coronary syndromes. Circulation 115:e356–e375
Lorgis L, Zeller M, Dentan G, Sicard P, Buffet P, L’Huillier I, Beer JC, Vincent-Martin M, Makki H, Gambert P, Cottin Y, RICO Survey Working Group (2009) Prognostic value of N-terminal pro-brain natriuretic peptide in elderly people with acute myocardial infarction: prospective observational study. BMJ 338:b1605
Hunt PJ, Yandle TG, Nicholls MG, Richards AM, Espiner EA (1995) The amino-terminal portion of pro-brain natriuretic peptide (Pro-BNP) circulates in human plasma. Biochem Biophys Res Commun 214:1175–1183
Xing Wu, Sha Hongying, Sun Yirui, Gao Liang, Liu Hua, Yuan Qiang, Zhang Tao, Zhu Jianhong, Zhou Liangfu, Jin Hu (2011) N-terminal Pro-B-type natriuretic peptide in patients with isolated traumatic brain injury: a prospective Cohort study. J Trauma 71:820–825
Tykocki T, Kostyra K, Bojanowski K, Kostkiewicz B (2014) Analysis of the serum components in acute period after subarachnoid hemorrhage. Turk Neurosurg 24:672–678
Chang L, Yan H, Li H, Song Z, Gui Y, Yan Z, Li T, Duan D (2014) N-terminal probrain natriuretic peptide levels as a predictor of functional outcomes in patients with ischemic stroke. NeuroReport 25:985–990
Naveen V, Vengamma B, Mohan A, Vanajakshamma V (2015) N-terminal pro-brain natriuretic peptide levels and short term prognosis in acute ischemic stroke. Ann Indian Acad Neurol 18:435–440
Jensen JK, Mickley H, Bak S, Korsholm L, Kristensen SR (2006) Serial measurements of N-terminal pro-brain natriuretic peptide after acute ischemic stroke. Cerebrovasc Dis 22:439–444
Hajdinjak E, Klemen P, Grmec S (2012) Prognostic value of a single prehospital measurement of N-terminal pro-brain natriuretic peptide and troponin T after acute ischaemic stroke. J Int Med Res 40:768–776
Hemphill JC 3rd, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, Fung GL, Goldstein JN, Macdonald RL, Mitchell PH, Scott PA, Selim MH, Woo D, American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology (2015) Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 46:2032–2060
Lei C, Wu B, Liu M, Tan G, Zeng Q (2016) Pathogenesis and subtype of intracerebral hemorrhage (ICH) and ICH score determines prognosis. Curr Neurovasc Res 13:244–248
Kwon WK, Park DH, Park KJ, Kang SH, Lee JH, Cho TH, Chung YG (2014) Prognostic factors of clinical outcome after neuronavigation-assisted hematoma drainage in patients with spontaneous intracerebral hemorrhage. Clin Neurol Neurosurg 123:83–89
Huang Y, Chen J, Zhong S, Yuan J (2016) Role of APACHE II scoring system in the prediction of severity and outcome of acute intracerebral hemorrhage. Int J Neurosci 126:1020–1024
Levin ER, Gardner DG, Samson WK (1998) Natriuretic peptides. N Engl J Med 339:321–328
Goya Y, Shibazaki K, Sakai K, Aoki J, Uemura J, Saji N, Isa K, Ohya Y, Kimura K (2014) Brain natriuretic peptide upon admission as a biological marker of short-term mortality after intracerebral hemorrhage. Eur Neurol 71:203–207
Nyberg Christoffer, Karlsson Torbjörn, Ronne-Engsrtöm Elisabeth (2014) Predictors of increased cumulative serum levels of the N-terminal prohormone of brain natriuretic peptide 4 days after acute spontaneous subarachnoid hemorrhage. J Neurosurg 120:599–604
Li F, Chen QX, Xiang SG, Yuan SZ, Xu XZ (2017) N-terminal pro-brain natriuretic peptide concentrations after hypertensive intracerebral hemorrhage. J Intensive Care Med. doi:10.1177/0885066616683677
Acknowledgements
We gratefully acknowledge the help of all members of the Department of Neurosurgery, Renmin Hospital of Wuhan University, as well as the patients and their families who participated in the study; their participation and contributions made this study possible.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics statement
This study was conducted in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The research protocol was approved by the Medical Ethics Board of the Renmin Hospital of Wuhan University. Informed consent was obtained from all patients or their next of kin.
Conflicts of interest
The authors confirm that there is no conflict of interest.
Funding
None.
Rights and permissions
About this article
Cite this article
Li, F., Chen, QX., Xiang, SG. et al. The role of N-terminal pro-brain natriuretic peptide in evaluating the prognosis of patients with intracerebral hemorrhage. J Neurol 264, 2081–2087 (2017). https://doi.org/10.1007/s00415-017-8602-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-017-8602-0