Abstract
Pathobiological factors underlying phenotypic diversity in Alzheimer’s disease (AD) are incompletely understood. We used an extended cerebrospinal fluid (CSF) panel to explore differences between “typical” with “atypical” AD and between amnestic, posterior cortical atrophy, logopenic aphasia and frontal variants. We included 97 subjects fulfilling International Working Group-2 research criteria for AD of whom 61 had “typical” AD and 36 “atypical” syndromes, and 30 controls. CSF biomarkers included total tau (T-tau), phosphorylated tau (P-tau), amyloid β1-42, amyloid βX-38/40/42, YKL-40, neurofilament light (NFL), and amyloid precursor proteins α and β. The typical and atypical groups were matched for age, sex, severity and rate of cognitive decline and had similar biomarker profiles, with the exception of NFL which was higher in the atypical group (p = 0.03). Sub-classifying the atypical group into its constituent clinical syndromes, posterior cortical atrophy was associated with the lowest T-tau [604.4 (436.8–675.8) pg/mL], P-tau (79.8 ± 21.8 pg/L), T-tau/Aβ1-42 ratio [2.3 (1.4–2.6)], AβX-40/X-42 ratio (22.1 ± 5.8) and rate of cognitive decline [1.9 (0.75–4.25) MMSE points/year]. Conversely, the frontal variant group had the highest levels of T-tau [1185.4 (591.7–1329.3) pg/mL], P-tau (116.4 ± 45.4 pg/L), T-tau/Aβ1-42 ratio [5.2 (3.3–6.9)] and AβX-40/X-42 ratio (27.9 ± 7.5), and rate of cognitive decline. Whilst on a group level IWG-2 “typical” and “atypical” AD share similar CSF profiles, which are very different from controls, atypical AD is a heterogeneous entity with evidence for subtle differences in amyloid processing and neurodegeneration between different clinical syndromes. These findings also have practical implications for the interpretation of clinical CSF biomarker results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s disease (AD) is usually associated with early decline in episodic memory followed by progressive cognitive deficits reflecting a symmetrical, generalised loss of function of association cortices [1]. However, there is also considerable symptomatic heterogeneity, particularly in young onset cases [2]. Whilst previously only amnestic presentations were recognised in diagnostic criteria, newer criteria, including those from the International Working Group (IWG-2) combining biomarkers and clinical phenotypes, distinguish “typical”, i.e. memory-led AD, from “atypical” AD, the latter comprising visual/biparietal (posterior cortical atrophy, PCA [3–5]), logopenic[6] (language) and frontal (behavioural) variants [7]. Whilst these AD variants are underpinned by the same core pathology they appear to differ in distribution of tau pathology [8], neuronal cell loss [9, 10] and network disruption [11]. Atypical AD variants are over-represented in young onset cases [2], and there is evidence for different genetic risk in some atypical forms [12–14], but the biological factors responsible for this phenotypic diversity are largely not understood.
Cerebrospinal fluid (CSF) allows for assessment of different biological processes implicated in AD. The most established, and now in routine clinical practice, include amyloid beta 1-42 (Aβ1-42), “total” tau (T-tau), and tau phosphorylated at 181 (P-tau). Aβ1-42 is inversely correlated with amyloid load [15, 16]; T-tau is thought to reflect the intensity of neurodegeneration [17], and P-tau correlates with neurofibrillary tangle burden [18, 19]. Other available CSF biomarkers include YKL-40, a marker of neuroinflammation [20]; neurofilament light (NFL), a marker of the breakdown of large-calibre myelinated axons [21]; soluble amyloid precursor protein (APP) isoforms APPα and APPβ, reflecting non-amyloidogenic and amyloidogenic APP processing, respectively [22, 23]; and Aβ1-38 and Aβ1-40 which in combination with Aβ1-42 provide insights into γ-secretase-dependent APP processing generating C-terminally ragged Aβ species [24]. In this study, we used an extended CSF panel to assess differences between IWG-2 typical and atypical AD and then to investigate the CSF profiles of amnestic, PCA, logopenic and frontal variants of AD. We hypothesised that there would be differences in markers of neurodegeneration and amyloid processing between AD subtypes to reflect different distribution of tau deposition and neuronal disruption and considered that variations in neuroinflammation and large-calibre myelinated axon involvement might contribute to clinical heterogeneity.
Materials and methods
Ethics statement
The study was conducted in accordance with local clinical research regulations and was approved by the local Ethics Committee.
Subjects
We included 97 subjects with a diagnosis of AD assessed at the Specialist Cognitive Disorders Service at Queen Square between October 2008 and October 2012. All subjects had had a diagnostic CSF examination; had a CSF profile consistent with AD (Aβ1-42 <550 pg/mL and tau/Aβ1-42 ratio ≥0.5) [25] and fulfilled IWG-2 criteria for AD [7]. We included 30 age-matched controls who were spouses of affected individuals, did not have cognitive symptoms and had a CSF examination only for research.
We retrospectively classified individuals as having typical (amnestic) AD or atypical AD according to IWG-2 criteria (Fig. 1), further sub-classifying the IWG-2 atypical AD group into those fulfilling clinical criteria for PCA [26] or LPA [6]. In the absence of published criteria for frontal variant AD (fvAD), we examined the notes of all individuals with atypical AD not fulfilling PCA or LPA criteria, determining that all had early behavioural features (see supplementary Table 1), thus fulfilling IWG-2 criteria for fvAD [7]. We recorded the nearest mini-mental state examination (MMSE) score to the date of the lumbar puncture, and estimated disease duration from first symptom to LP, based on recorded information from patients/informants. We estimated rate of cognitive decline (MMSE/year) as (30-MMSE at time of LP)/disease duration.
A number of exclusion criteria apply. See Dubois et al. (2014), Lancet Neurology for full details; PSEN presenilin, App amyloid precursor protein
The majority of patients were seen in routine clinical practice and had not been assessed using a single standardised neuropsychology battery. A proportion (n = 22; 22.7 %) had been assessed on a research neuropsychology battery, details of which are included in supplementary material.
Cerebrospinal fluid collection and biomarker analysis
CSF was collected by lumbar puncture in polypropylene containers, spun at 4000 RPM for 10 min at 4 °C and frozen in aliquots at −80 °C within 60 min. Biomarker levels were measured using commercially available immunoassays according to manufacturers’ protocols (full details in supplementary material). Amyloidogenic APP processing was measured using two different kits: the INNOTEST® β-amyloid(1-42) assay (Fujirebio, Ghent, Belgium) in which N- and C-terminal antibodies are used to measure specifically the 42 amino acid long form of Aβ (Aβ1-42) and the MSD Aβ Triplex assay (Meso Scale Discovery, Rockville, MD, USA). The latter assay is a multiplexed method in which C-terminally specific antibodies are used to selectively capture Aβ forms ending at amino acids 38, 40 and 42, respectively, which are then quantified using the 6E10 detector antibody. This assay is thus not specific to the 1st amino acid of the Aβ peptides (the epitope of 6E10 lies within amino acids 3–8 in the Aβ sequence), and the measured Aβ isoforms are therefore called AβX-38, AβX-40 and AβX-42 in this paper. Board-certified laboratory technicians, blinded to clinical data, performed all analyses using one batch of reagents with intra-assay coefficients of variation of <10 %.
Statistical analysis
Demographics and CSF biomarker levels were compared between groups using t tests when there were no clear departures from a normal distribution and Wilcoxon rank-sum tests for skewed or truncated data. Demographics and CSF biomarkers were compared across individuals with PCA, LPA and fvAD using one-way ANOVA when the distribution was approximately normal and Kruskal–Wallis rank test for skewed or truncated data, or Chi-squared tests for categorical variables. Post hoc pairwise comparisons between pairs of groups were made when the initial test across all groups was statistically significant. Linear regression was used to explore the relationship between diagnosis and biomarker incorporating nuisance variables (age, sex, cognitive decline and MMSE) as covariates; non-normally distributed variables were log transformed for linear regression analysis. All statistical analyses used Stata Version 12.1 (Stata corporation, College Station, TX, USA).
Results
Asymptomatic controls and IWG2 typical and atypical Alzheimer’s disease
30 asymptomatic controls were recruited and 97 patients fulfilled IWG2 criteria for AD (Table 1). The groups were similar in terms of age (59.8 ± 9.9 vs. 62.5 ± 6.9) and sex, but there were significant differences in MMSE (29.7 ± 0.5 vs. 20 ± 6.8) and all other measured biomarkers except for APPα and APPβ.
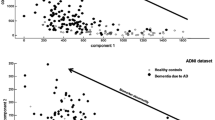
Of the 97 patients, 61 patients fulfilled criteria for typical AD and 36 for atypical AD (Table 1). The groups were similar in terms of age (62.5 ± 6.6 vs. 62.3 ± 7.4) and MMSE (20.6 ± 6.4 vs 19.1 ± 7.5) at the time of LP or estimated rates of cognitive decline (median = 2.5 vs 2.8 MMSE points/year); there was a non-significant trend for more women in the typical AD group (73.8 vs 55.6 %). The CSF biomarker profiles of typical and atypical Alzheimer’s disease are shown in Table 1. There were no significant differences for any biomarker except for NFL, which was significantly higher in the atypical Alzheimer’s disease group (p = 0.03). In a regression model incorporating age, sex, MMSE and rate of decline included in the model, this difference remained significant (p < 0.05).
Comparing atypical Alzheimer’s disease subtypes
Of the 36 patients with atypical AD, 17 patients fulfilled criteria for PCA and 11 for LPA, and the remaining eight were classified as having fvAD. Demographics and CSF results are shown in Table 2. There were no significant differences in age or MMSE, but there were significant differences between the estimated rates of cognitive decline between the groups, with the fvAD cases declining significantly faster (median 5.3 MMSE points/year) than either the LPA (3 points/year) or PCA groups (1.9 points/year). Rate of decline remained significantly higher in the fvAD group compared with typical AD even after adjusting for nuisance variables age, sex and MMSE (p = 0.01).
Comparing the CSF profiles between the three subgroups (Table 2), significant differences were seen in T-tau, P-tau, T-tau/Aβ1-42 ratio, AβX-42 (measured using the MSD Abeta Triplex method) and AβX-40/X-42 ratio. Both T-tau and P-tau were lowest in the PCA group, intermediate in the LPA group and highest in the fvAD group with significant differences between PCA and each of the other groups. T-tau/Aβ1-42 ratio was significantly higher in the fvAD group than the PCA and LPA groups. There was a non-significant trend for Aβ1-42 measured using the Innotest ELISA to be lower in the fvAD group, and this was significant for AβX-42 measured using the MSD Abeta Triplex assay (p < 0.05). AβX-42 was lowest in the frontal variant subgroup and highest in PCA. AβX-40/X-42 ratio was significantly higher in the fvAD group than the PCA group.
Comparing atypical Alzheimer’s disease subgroups to amnestic Alzheimer’s disease
Compared to typical AD, the fvAD group had significantly faster rates of MMSE decline (p = 0.01), and significantly higher T-tau/Aβ1-42 ratio (0.01), NFL (<0.048) and AβX-42 levels measured using the triplex assay (p = 0.02) and borderline lower AβX-40 levels (p = 0.08). The LPA group were significantly more likely to be male (p = 0.03), but there were no differences in any of the CSF profiles. The PCA group as whole had significantly lower levels of P-tau (p = 0.04) and borderline lower AβX-40/X-42 ratios (p = 0.06). Of the 22 individuals with detailed neuropsychology, 14, all previously classified as having IWG-2 typical AD, fulfilled criteria for n-tAD. Eight, all of whom fulfilled criteria for IWG-2 atypical AD and Tang-Wai criteria for PCA, also fulfilled criteria for n-PCA. Comparing these groups (Supplementary Table 2), the n-PCA group had lower T-tau (p = 0.048), lower P-tau (p = 0.048) and lower AβX-40/X-42 ratio (p = 0.01) than the n-tAD group. In a regression model including age, sex, MMSE and rate of cognitive decline as covariates, AβX-40/X-42 ratio remained significantly different between the groups.
Discussion
The key findings of this study are that the CSF profiles of IWG-2 typical and atypical AD are remarkably similar, bar elevation of NFL in the atypical group. However, when carefully sub-classified there are significant differences between the various AD subtypes. Notably, PCA emerges as the phenotype associated with lower concentrations of T-tau and P-tau and AβX-40/X-42 ratio, and with a more indolent course; and that we define a small AD subgroup (fvAD) with prominent behavioural features higher concentrations of the neurodegeneration markers T-tau, P-tau and NFL, lower concentrations of the amyloidogenic form of Aβ, Aβ1-42, and more aggressive disease.
The cohort had an average age at onset of 62 years, with 52 % fulfilling criteria for young onset AD (onset <65 years). Whilst atypical for AD per se, this reflects both the focus of our clinic, and that patients with younger onset disease are those more likely to be offered a CSF examination as part of the diagnostic work-up [27–29]. In keeping with previous studies [2] that have shown an over-representation of atypical presentations in younger onset cohorts, we found that a relatively high proportion (~40 %) had a non-amnestic presentation.
On a group level, we found, as expected, that patients fulfilling IWG-2 criteria for AD had significantly different biomarker levels than controls in all bar APPα and APPβ, as previously reported [30]. The typical and atypical AD groups were well matched for gender, age, severity and estimated rate of decline, which at ~2.5 MMSE points/year was as expected for individuals with mild–moderate disease [31]. On a group level, the CSF profiles were also similar. The only difference between the groups was a significant elevation of NFL in the atypical group. NFL, a marker of degeneration of large-calibre axons, has previously been shown to be elevated in vascular dementia, while only slightly elevated in frontotemporal dementia in AD compared to healthy controls [32, 33]. Possible explanations for our findings are either that elevated NFL might be a marker of atypical AD per se, or that the atypical AD group is heterogeneous, with some individuals having very elevated NFL levels. Subsequent analyses of the atypical group suggest the latter to be the most likely explanation, with the NFL increase in the atypical AD group being driven by those with fvAD.
Despite the broad similarities to typical AD on a group level, a more detailed assessment of the atypical AD group revealed further differences between its constituent subtypes. Although severity was not significantly different at the time of LP, the PCA group had the lowest levels of T-tau and P-tau, the lowest AβX-40/AβX-42 ratios and the slowest rates of estimated cognitive decline. There were significant differences seen in all of these levels between PCA and fvAD; in P-tau and AβX-40/AβX-42 ratio comparing all PCA cases with all those with typical AD and in T-tau, P-tau and AβX-40/X-42 ratio in the subgroup of individuals with more stringently neuropsychologically defined n-PCA and n-tAD. The existing literature examining CSF T-tau and P-tau levels in PCA has shown conflicting results. Several studies have reported levels to be similar between PCA and tAD [34–40] although a recent study of 12 PCA patients also found T-tau and P-tau to be reduced in PCA compared to patients with LPA and typical AD [41]. Whilst the biological significance of CSF T-tau and P-tau needs further study, both are thought to reflect ongoing neuronal degeneration [42]. High CSF T-tau is believed to reflect the intensity of neurodegeneration [17] and is not specific for AD; the highest levels are found in rapidly progressing disorders such as Creutzfeldt-Jakob disease, in encephalitis and after stroke [43]. By contrast, P-tau elevation is thought to be more specific to AD-related neurodegeneration [42], with prior studies suggesting that CSF P-tau correlates well with post-mortem cortical neurofibrillary tangle (NFT) burden [19, 44]. Imaging and pathological studies of PCA have consistently shown similar levels and distribution of amyloid pathology [36, 45, 46], but not differences in the distribution of cortical tau pathology [8, 26, 47–49] and pattern of atrophy [4, 9, 50]. The lower levels of both T-tau and P-tau in CSF with similar levels of Aβ may therefore reflect differences in the focality of neurodegeneration in this variant of AD. Another possible explanation might relate to the rate of neurodegeneration, given that as well as the reduced levels of T-tau and P-tau we found estimated rate of progression to be lower in the PCA group than in the other atypical phenotypes. This is however in contrast to another study Teng et al. [41] which found no differences in severity or disease duration in PCA compared to other subtypes. Whilst it is possible that some of the PCA patients had non-AD pathology, the similar levels of Aβ1-42 compared to the other phenotypes makes this unlikely.
Whilst Aβ1-42, the major component of the AD amyloid plaque, is reduced in CSF in AD, AβX-40 is thought to relate more to amyloid angiopathy and less to plaque pathology [51] and is relatively unchanged in AD [52, 53]. Elevated AβX-40/X-42 ratio is reported as improving diagnostic accuracy in early AD [54–56], and unlike Aβ42 level alone, to correlate with the extent of tau pathology [57]. The latter is consistent with our finding of both rather lower AβX-40/X-42 ratio and lower levels of P-tau in the PCA group.
In marked contrast to the PCA cases, the fvAD subjects had the highest rates of cognitive decline, together with high T-tau and P-tau levels, and AβX-40/AβX-42 ratio. Additionally, this group also had the highest levels of CSF NFL and T-tau/Aβ1-42 ratio, and the lowest levels of Aβ1-42. There were significant differences between rate of decline, T-tau, P-tau, T-tau/Aβ1-42 and AβX-40/X-42 ratios and AβX-42 (measured using the MSD platform) levels compared to PCA; and rate of cognitive decline, T-tau/Aβ42 ratio, AβX-42 and NFL levels compared to typical AD. We did not use an a priori classification to define fvAD; this group was composed of individuals who fulfilled CSF criteria for AD but did not fulfil criteria for the other AD variants, and who on review of the case notes were found to have early behavioural features. Prior studies have suggested that fvAD (or behavioural variant AD) is a rare phenotypic variant of AD that can be clinically indistinguishable from behavioural variant frontotemporal dementia [58–61] and is often but not always associated with young onset [2, 29]. In the few published pathological studies AD pathology preferentially affected the frontal lobes [62]. Our finding of higher levels of T-tau and P-tau, lower levels of AβX-40/X-42 and more aggressive decline in these cases is the opposite to what we observed in PCA, and consistent with a relationship between these different pathological processes and rate of progression. The marked differences in CSF profile between these two AD variants suggests that aside from having affecting different brain regions, there may well be fundamental differences in the underlying disease biology, reflected by alterations in amyloid processing and neurodegeneration. The increased NFL levels observed in these cases are likely to be a further reflection of the more aggressive disease course. Alternate explanations are that the elevated NFL level may be influenced by those cases with additional vascular changes on MRI.
Despite a number of biological differences between the various AD subtypes, we did not find any differences in YKL-40. There is growing evidence that neuroinflammation plays a role in AD pathogenesis [63], and with the caveat that the neuroinflammatory process is very complex and YKL-40 is only one of many potential biomarkers [64], we did not find evidence for differences in inflammatory process to be a major driver of phenotype.
This study has a number of strengths, including a relatively high proportion of well-matched atypical cases allowing for meaningful comparisons with typical AD. We used established criteria for defining PCA and LPA cases, and an unbiased approach for determining fvAD. Weaknesses include the relatively small number of cases in each of the atypical syndromic variants, although these numbers are favourable when compared to other studies and we employed statistical approaches appropriate for the samples of this size. The study was retrospective, and so samples were not always collected under ideal research conditions, limited prospective psychology was available and ApoE4 status is not available. Whilst we excluded patients with known mutations in genes causing AD, these were not tested systematically. Rates of cognitive decline were estimated, and based on the MMSE which, being heavily weighted towards the deficits associated with typical amnestic AD, may not accurately capture decline in the atypical phenotypes. As the typical AD cases were relatively young at onset, a study of older onset sporadic cases would be valuable to determine whether these findings are applicable to late onset AD. Finally, in the absence of pathology, we cannot be certain that all had underlying AD, or that individuals with AD did not have additional pathologies.
In summary, we have shown that whilst ostensibly similar to typical AD, IWG-2 defined atypical AD is not a homogeneous entity, with significant differences between PCA, LPA and fvAD; and between typical AD and both PCA and fvAD. These differences are mainly focussed on differential levels of tau and P-tau, and ratio of AβX-40/X-42 and likely rates of clinical progression, suggesting that subtle differences in amyloid processing and neurodegenerative mechanisms may underpin at least some of the phenotypic diversity in AD. As well as providing biological insights, these results have practical implications when it comes to interpreting CSF results in atypical variants of AD.
References
Blennow K, Wallin A, Gottfries CG (1991) Presence of parietotemporal symptomatology distinguishes early and late onset Alzheimers-disease. Int J Geriatr Psychiatry 6(3):147–154. doi:10.1002/gps.930060306
Koedam EL, Lauffer V, van der Vlies AE, van der Flier WM, Scheltens P, Pijnenburg YA (2010) Early-versus late-onset Alzheimer’s disease: more than age alone. J Alzheimer’s Dis 19(4):1401–1408. doi:10.3233/JAD-2010-1337
Benson DF, Davis RJ, Snyder BD (1988) Posterior cortical atrophy. Arch Neurol 45(7):789–793
Mendez MF, Ghajarania M, Perryman KM (2002) Posterior cortical atrophy: clinical characteristics and differences compared to Alzheimer’s disease. Dement Geriatr Cogn Disord 14(1):33–40. doi:10.1159/000058331
Crutch SJ, Lehmann M, Schott JM, Rabinovici GD, Rossor MN, Fox NC (2012) Posterior cortical atrophy. Lancet Neurol 11(2):170–178. doi:10.1016/S1474-4422(11)70289-7
Gorno-Tempini ML, Hillis AE, Weintraub S, Kertesz A, Mendez M, Cappa SF, Ogar JM, Rohrer JD, Black S, Boeve BF, Manes F, Dronkers NF, Vandenberghe R, Rascovsky K, Patterson K, Miller BL, Knopman DS, Hodges JR, Mesulam MM, Grossman M (2011) Classification of primary progressive aphasia and its variants. Neurology 76(11):1006–1014. doi:10.1212/WNL.0b013e31821103e6
Dubois B, Feldman HH, Jacova C, Hampel H, Molinuevo JL, Blennow K, DeKosky ST, Gauthier S, Selkoe D, Bateman R, Cappa S, Crutch S, Engelborghs S, Frisoni GB, Fox NC, Galasko D, Habert MO, Jicha GA, Nordberg A, Pasquier F, Rabinovici G, Robert P, Rowe C, Salloway S, Sarazin M, Epelbaum S, de Souza LC, Vellas B, Visser PJ, Schneider L, Stern Y, Scheltens P, Cummings JL (2014) Advancing research diagnostic criteria for Alzheimer’s disease: the IWG-2 criteria. Lancet Neurol 13(6):614–629. doi:10.1016/S1474-4422(14)70090-0
Ossenkoppele R, Schonhaut DR, Baker SL, O’Neil JP, Janabi M, Ghosh PM, Santos M, Miller ZA, Bettcher BM, Gorno-Tempini ML, Miller BL, Jagust WJ, Rabinovici GD (2015) Tau, amyloid, and hypometabolism in a patient with posterior cortical atrophy. Ann Neurol 77(2):338–342. doi:10.1002/ana.24321
Lehmann M, Crutch SJ, Ridgway GR, Ridha BH, Barnes J, Warrington EK, Rossor MN, Fox NC (2011) Cortical thickness and voxel-based morphometry in posterior cortical atrophy and typical Alzheimer’s disease. Neurobiol Aging 32(8):1466–1476. doi:10.1016/j.neurobiolaging.2009.08.017
Madhavan A, Whitwell JL, Weigand SD, Duffy JR, Strand EA, Machulda MM, Tosakulwong N, Senjem ML, Gunter JL, Lowe VJ, Petersen RC, Jack CR Jr, Josephs KA (2013) FDG PET and MRI in logopenic primary progressive aphasia versus dementia of the Alzheimer’s type. PLoS One 8(4):e62471. doi:10.1371/journal.pone.0062471
Lehmann M, Ghosh PM, Madison C, Laforce R Jr, Corbetta-Rastelli C, Weiner MW, Greicius MD, Seeley WW, Gorno-Tempini ML, Rosen HJ, Miller BL, Jagust WJ, Rabinovici GD (2013) Diverging patterns of amyloid deposition and hypometabolism in clinical variants of probable Alzheimer’s disease. Brain 136(Pt 3):844–858. doi:10.1093/brain/aws327
Schott JM, Ridha BH, Crutch SJ, Healy DG, Uphill JB, Warrington EK, Rossor MN, Fox NC (2006) Apolipoprotein e genotype modifies the phenotype of Alzheimer disease. Arch Neurol 63(1):155–156. doi:10.1001/archneur.63.1.155
Carrasquillo MM, Khan Q, Murray ME, Krishnan S, Aakre J, Pankratz VS, Nguyen T, Ma L, Bisceglio G, Petersen RC, Younkin SG, Dickson DW, Boeve BF, Graff-Radford NR, Ertekin-Taner N (2014) Late-onset Alzheimer disease genetic variants in posterior cortical atrophy and posterior AD. Neurology 82(16):1455–1462. doi:10.1212/WNL.0000000000000335
van der Flier WM, Schoonenboom SN, Pijnenburg YA, Fox NC, Scheltens P (2006) The effect of APOE genotype on clinical phenotype in Alzheimer disease. Neurology 67(3):526–527. doi:10.1212/01.wnl.0000228222.17111.2a
Strozyk D, Blennow K, White LR, Launer LJ (2003) CSF Abeta 42 levels correlate with amyloid-neuropathology in a population-based autopsy study. Neurology 60(4):652–656
Palmqvist S, Zetterberg H, Blennow K, Vestberg S, Andreasson U, Brooks DJ, Owenius R, Hagerstrom D, Wollmer P, Minthon L, Hansson O (2014) Accuracy of brain amyloid detection in clinical practice using cerebrospinal fluid beta-amyloid 42: a cross-validation study against amyloid positron emission tomography. JAMA Neurol 71(10):1282–1289. doi:10.1001/jamaneurol.2014.1358
Blennow K, Hampel H, Weiner M, Zetterberg H (2010) Cerebrospinal fluid and plasma biomarkers in Alzheimer disease. Nat Rev Neurol 6(3):131–144. doi:10.1038/nrneurol.2010.4
Hampel H, Burger K, Pruessner JC, Zinkowski R, DeBernardis J, Kerkman D, Leinsinger G, Evans AC, Davies P, Moller HJ, Teipel SJ (2005) Correlation of cerebrospinal fluid levels of tau protein phosphorylated at threonine 231 with rates of hippocampal atrophy in Alzheimer disease. Arch Neurol 62(5):770–773. doi:10.1001/archneur.62.5.770
Buerger K, Ewers M, Pirttila T, Zinkowski R, Alafuzoff I, Teipel SJ, DeBernardis J, Kerkman D, McCulloch C, Soininen H, Hampel H (2006) CSF phosphorylated tau protein correlates with neocortical neurofibrillary pathology in Alzheimer’s disease. Brain 129(Pt 11):3035–3041. doi:10.1093/brain/awl269
Craig-Schapiro R, Perrin RJ, Roe CM, Xiong C, Carter D, Cairns NJ, Mintun MA, Peskind ER, Li G, Galasko DR, Clark CM, Quinn JF, D’Angelo G, Malone JP, Townsend RR, Morris JC, Fagan AM, Holtzman DM (2010) YKL-40: a novel prognostic fluid biomarker for preclinical Alzheimer’s disease. Biol Psychiatry 68(10):903–912. doi:10.1016/j.biopsych.2010.08.025
Sjogren M, Rosengren L, Minthon L, Davidsson P, Blennow K, Wallin A (2000) Cytoskeleton proteins in CSF distinguish frontotemporal dementia from AD. Neurology 54(10):1960–1964
Lewczuk P, Kornhuber J, Vanmechelen E, Peters O, Heuser I, Maier W, Jessen F, Burger K, Hampel H, Frolich L, Henn F, Falkai P, Ruther E, Jahn H, Luckhaus C, Perneczky R, Schmidtke K, Schroder J, Kessler H, Pantel J, Gertz HJ, Vanderstichele H, de Meyer G, Shapiro F, Wolf S, Bibl M, Wiltfang J (2010) Amyloid beta peptides in plasma in early diagnosis of Alzheimer’s disease: a multicenter study with multiplexing. Exp Neurol 223(2):366–370. doi:10.1016/j.expneurol.2009.07.024
Brinkmalm G, Brinkmalm A, Bourgeois P, Persson R, Hansson O, Portelius E, Mercken M, Andreasson U, Parent S, Lipari F, Ohrfelt A, Bjerke M, Minthon L, Zetterberg H, Blennow K, Nutu M (2013) Soluble amyloid precursor protein alpha and beta in CSF in Alzheimer’s disease. Brain Res 1513:117–126. doi:10.1016/j.brainres.2013.03.019
Bibl M, Gallus M, Welge V, Esselmann H, Wiltfang J (2012) Aminoterminally truncated and oxidized amyloid-beta peptides in the cerebrospinal fluid of Alzheimer’s disease patients. J Alzheimer’s Dis 29(4):809–816. doi:10.3233/JAD-2012-111796
Duits FH, Teunissen CE, Bouwman FH, Visser PJ, Mattsson N, Zetterberg H, Blennow K, Hansson O, Minthon L, Andreasen N, Marcusson J, Wallin A, Rikkert MO, Tsolaki M, Parnetti L, Herukka SK, Hampel H, De Leon MJ, Schroder J, Aarsland D, Blankenstein MA, Scheltens P, van der Flier WM (2014) The cerebrospinal fluid “Alzheimer profile”: easily said, but what does it mean? Alzheimer’s Dement 10(6):713–723. doi:10.1016/j.jalz.2013.12.023
Tang-Wai DF, Graff-Radford NR, Boeve BF, Dickson DW, Parisi JE, Crook R, Caselli RJ, Knopman DS, Petersen RC (2004) Clinical, genetic, and neuropathologic characteristics of posterior cortical atrophy. Neurology 63(7):1168–1174
Waldemar G, Dubois B, Emre M, Scheltens P, Tariska P, Rossor M (2000) Diagnosis and management of Alzheimer’s disease and other disorders associated with dementia. The role of neurologists in Europe. European Federation of Neurological Societies. Eur J Neurol 7(2):133–144
Knopman DS, DeKosky ST, Cummings JL, Chui H, Corey-Bloom J, Relkin N, Small GW, Miller B, Stevens JC (2001) Practice parameter: diagnosis of dementia (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 56(9):1143–1153
Rossor MN, Fox NC, Mummery CJ, Schott JM, Warren JD (2010) The diagnosis of young-onset dementia. Lancet Neurol 9(8):793–806. doi:10.1016/s1474-4422(10)70159-9
Paterson RW, Toombs J, Slattery CF, Schott JM, Zetterberg H (2014) Biomarker modelling of early molecular changes in Alzheimer’s disease. Mol Diagn Ther 18(2):213–227. doi:10.1007/s40291-013-0069-9
Birks J (2006) Cholinesterase inhibitors for Alzheimer’s disease. Cochrane Database Syst Rev. doi:10.1002/14651858.CD005593
Skillback T, Farahmand B, Bartlett JW, Rosen C, Mattsson N, Nagga K, Kilander L, Religa D, Wimo A, Winblad B, Rosengren L, Schott JM, Blennow K, Eriksdotter M, Zetterberg H (2014) CSF neurofilament light differs in neurodegenerative diseases and predicts severity and survival. Neurology 83(21):1945–1953. doi:10.1212/WNL.0000000000001015
Scherling CS, Hall T, Berisha F, Klepac K, Karydas A, Coppola G, Kramer JH, Rabinovici G, Ahlijanian M, Miller BL, Seeley W, Grinberg LT, Rosen H, Meredith J Jr, Boxer AL (2014) Cerebrospinal fluid neurofilament concentration reflects disease severity in frontotemporal degeneration. Ann Neurol 75(1):116–126. doi:10.1002/ana.24052
Ossenkoppele R, Mattsson N, Teunissen CE, Barkhof F, Pijnenburg Y, Scheltens P, van der Flier WM, Rabinovici GD (2015) Cerebrospinal fluid biomarkers and cerebral atrophy in distinct clinical variants of probable Alzheimer’s disease. Neurobiol Aging. doi:10.1016/j.neurobiolaging.2015.04.011
Seguin J, Formaglio M, Perret-Liaudet A, Quadrio I, Tholance Y, Rouaud O, Thomas-Anterion C, Croisile B, Mollion H, Moreaud O, Salzmann M, Dorey A, Bataillard M, Coste MH, Vighetto A, Krolak-Salmon P (2011) CSF biomarkers in posterior cortical atrophy. Neurology 76(21):1782–1788. doi:10.1212/WNL.0b013e31821ccc98
de Souza LC, Corlier F, Habert MO, Uspenskaya O, Maroy R, Lamari F, Chupin M, Lehericy S, Colliot O, Hahn-Barma V, Samri D, Dubois B, Bottlaender M, Sarazin M (2011) Similar amyloid-beta burden in posterior cortical atrophy and Alzheimer’s disease. Brain 134(Pt 7):2036–2043. doi:10.1093/brain/awr130
Coppi E, Ferrari L, Santangelo R, Caso F, Pinto P, Passerini G, Comi G, Magnani G (2014) Further evidence about the crucial role of CSF biomarkers in diagnosis of posterior cortical atrophy. Neurological Sci 35(5):785–787. doi:10.1007/s10072-014-1644-5
Baumann TP, Duyar H, Sollberger M, Kuhle J, Regeniter A, Gomez-Mancilla B, Schmidtke K, Monsch AU (2010) CSF-tau and CSF-Abeta(1-42) in posterior cortical atrophy. Dement Geriatr Cogn Disord 29(6):530–533. doi:10.1159/000314679
Formaglio M, Costes N, Seguin J, Tholance Y, Le Bars D, Roullet-Solignac I, Mercier B, Krolak-Salmon P, Vighetto A (2011) In vivo demonstration of amyloid burden in posterior cortical atrophy: a case series with PET and CSF findings. J Neurol 258(10):1841–1851. doi:10.1007/s00415-011-6030-0
Beaufils E, Dufour-Rainfray D, Hommet C, Brault F, Cottier JP, Ribeiro MJ, Mondon K, Guilloteau D (2013) Confirmation of the amyloidogenic process in posterior cortical atrophy: value of the Abeta42/Abeta40 ratio. J Alzheimer’s Dis 33(3):775–780. doi:10.3233/JAD-2012-121267
Teng E, Yamasaki TR, Tran M, Hsiao JJ, Sultzer DL, Mendez MF (2014) Cerebrospinal fluid biomarkers in clinical subtypes of early-onset Alzheimer’s disease. Dement Geriatr Cogn Disord 37(5–6):307–314. doi:10.1159/000355555
Hampel H, Blennow K, Shaw LM, Hoessler YC, Zetterberg H, Trojanowski JQ (2010) Total and phosphorylated tau protein as biological markers of Alzheimer’s disease. Exp Gerontol 45(1):30–40. doi:10.1016/j.exger.2009.10.010
Riemenschneider M, Wagenpfeil S, Vanderstichele H, Otto M, Wiltfang J, Kretzschmar H, Vanmechelen E, Forstl H, Kurz A (2003) Phospho-tau/total tau ratio in cerebrospinal fluid discriminates Creutzfeldt-Jakob disease from other dementias. Mol Psychiatry 8(3):343–347. doi:10.1038/sj.mp.4001220
Tapiola T, Overmyer M, Lehtovirta M, Helisalmi S, Ramberg J, Alafuzoff I, Riekkinen P Sr, Soininen H (1997) The level of cerebrospinal fluid tau correlates with neurofibrillary tangles in Alzheimer’s disease. NeuroReport 8(18):3961–3963
Rosenbloom MH, Alkalay A, Agarwal N, Baker SL, O’Neil JP, Janabi M, Yen IV, Growdon M, Jang J, Madison C, Mormino EC, Rosen HJ, Gorno-Tempini ML, Weiner MW, Miller BL, Jagust WJ, Rabinovici GD (2011) Distinct clinical and metabolic deficits in PCA and AD are not related to amyloid distribution. Neurology 76(21):1789–1796. doi:10.1212/WNL.0b013e31821cccad
Leyton CE, Villemagne VL, Savage S, Pike KE, Ballard KJ, Piguet O, Burrell JR, Rowe CC, Hodges JR (2011) Subtypes of progressive aphasia: application of the International Consensus Criteria and validation using beta-amyloid imaging. Brain 134(Pt 10):3030–3043. doi:10.1093/brain/awr216
Levine DN, Lee JM, Fisher CM (1993) The visual variant of Alzheimer’s disease: a clinicopathologic case study. Neurology 43(2):305–313
Galton CJ, Patterson K, Xuereb JH, Hodges JR (2000) Atypical and typical presentations of Alzheimer’s disease: a clinical, neuropsychological, neuroimaging and pathological study of 13 cases. Brain 123(Pt 3):484–498
Kanne SM, Balota DA, Storandt M, McKeel DW Jr, Morris JC (1998) Relating anatomy to function in Alzheimer’s disease: neuropsychological profiles predict regional neuropathology 5 years later. Neurology 50(4):979–985
Whitwell JL, Petersen RC, Negash S, Weigand SD, Kantarci K, Ivnik RJ, Knopman DS, Boeve BF, Smith GE, Jack CR Jr (2007) Patterns of atrophy differ among specific subtypes of mild cognitive impairment. Arch Neurol 64(8):1130–1138. doi:10.1001/archneur.64.8.1130
Verbeek MM, Kremer BP, Rikkert MO, Van Domburg PH, Skehan ME, Greenberg SM (2009) Cerebrospinal fluid amyloid beta(40) is decreased in cerebral amyloid angiopathy. Ann Neurol 66(2):245–249. doi:10.1002/ana.21694
Wiltfang J, Esselmann H, Bibl M, Smirnov A, Otto M, Paul S, Schmidt B, Klafki HW, Maler M, Dyrks T, Bienert M, Beyermann M, Ruther E, Kornhuber J (2002) Highly conserved and disease-specific patterns of carboxyterminally truncated Abeta peptides 1-37/38/39 in addition to 1-40/42 in Alzheimer’s disease and in patients with chronic neuroinflammation. J Neurochem 81(3):481–496
Welge V, Fiege O, Lewczuk P, Mollenhauer B, Esselmann H, Klafki HW, Wolf S, Trenkwalder C, Otto M, Kornhuber J, Wiltfang J, Bibl M (2009) Combined CSF tau, p-tau181 and amyloid-beta 38/40/42 for diagnosing Alzheimer’s disease. J Neural Transm 116(2):203–212. doi:10.1007/s00702-008-0177-6
Hansson O, Buchhave P, Zetterberg H, Blennow K, Minthon L, Warkentin S (2009) Combined rCBF and CSF biomarkers predict progression from mild cognitive impairment to Alzheimer’s disease. Neurobiol Aging 30(2):165–173. doi:10.1016/j.neurobiolaging.2007.06.009
Struyfs H, Molinuevo JL, Martin JJ, De Deyn PP, Engelborghs S (2014) Validation of the AD-CSF-index in autopsy-confirmed Alzheimer’s disease patients and healthy controls. J Alzheimer’s Dis 41(3):903–909. doi:10.3233/JAD-131085
Fukuyama R, Mizuno T, Mori S, Nakajima K, Fushiki S, Yanagisawa K (2000) Age-dependent change in the levels of Abeta40 and Abeta42 in cerebrospinal fluid from control subjects, and a decrease in the ratio of Abeta42 to Abeta40 level in cerebrospinal fluid from Alzheimer’s disease patients. Eur Neurol 43(3):155–160. doi:10.1159/000008156
Wiltfang J, Esselmann H, Bibl M, Hull M, Hampel H, Kessler H, Frolich L, Schroder J, Peters O, Jessen F, Luckhaus C, Perneczky R, Jahn H, Fiszer M, Maler JM, Zimmermann R, Bruckmoser R, Kornhuber J, Lewczuk P (2007) Amyloid beta peptide ratio 42/40 but not A beta 42 correlates with phospho-Tau in patients with low- and high-CSF A beta 40 load. J Neurochem 101(4):1053–1059. doi:10.1111/j.1471-4159.2006.04404.x
Storey E, Slavin MJ, Kinsella GJ (2002) Patterns of cognitive impairment in Alzheimer’s disease: assessment and differential diagnosis. Front Biosci 7:e155–184
Aries MJ, Le Bastard N, Debruyne H, Van Buggenhout M, Nagels G, De Deyn PP, Engelborghs S (2010) Relation between frontal lobe symptoms and dementia severity within and across diagnostic dementia categories. Int J Geriatr Psychiatry 25(11):1186–1195. doi:10.1002/gps.2481
Taylor KI, Probst A, Miserez AR, Monsch AU, Tolnay M (2008) Clinical course of neuropathologically confirmed frontal-variant Alzheimer’s disease. Nat Clin Pract Neurol 4(4):226–232. doi:10.1038/ncpneuro0746
Woodward M, Jacova C, Black SE, Kertesz A, Mackenzie IR, Feldman H, group Ai (2010) Differentiating the frontal variant of Alzheimer’s disease. Int J Geriatr Psychiatry 25(7):732–738. doi:10.1002/gps.2415
Johnson JK, Head E, Kim R, Starr A, Cotman CW (1999) Clinical and pathological evidence for a frontal variant of Alzheimer disease. Arch Neurol 56(10):1233–1239
Schott JM, Revesz T (2013) Inflammation in Alzheimer’s disease: insights from immunotherapy. Brain 136(Pt 9):2654–2656. doi:10.1093/brain/awt231
Rosen C, Hansson O, Blennow K, Zetterberg H (2013) Fluid biomarkers in Alzheimer’s disease—current concepts. Mol Neurodegener 8:20. doi:10.1186/1750-1326-8-20
Acknowledgments
We gratefully acknowledge the support of our patients and their families, the Leonard Wolfson Experimental Neurology Centre, Alzheimer’s Research UK and Iceland Foods Ltd. This work was supported by the National Institute for Health Research Queen Square Dementia Biomedical Research Unit, University College London Hospitals Biomedical Research Centre and the Swedish Research Council. HZ is a Wallenberg Academy Fellow. SC is supported by an Alzheimer’s Research UK Senior Research Fellowship and ESRC/NIHR grant (ES/K006711/1). The authors have no conflicts of interest that are directly relevant to the content of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
H. Zetterberg and J. M. Schott are Joint Senior Authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Paterson, R.W., Toombs, J., Slattery, C.F. et al. Dissecting IWG-2 typical and atypical Alzheimer’s disease: insights from cerebrospinal fluid analysis. J Neurol 262, 2722–2730 (2015). https://doi.org/10.1007/s00415-015-7904-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-015-7904-3