Abstract
Parkinson’s disease is now considered a complex systemic disease also characterized by the occurrence of a variety of non-motor symptoms. Among them, a chemosensory impairment defined as a deficient olfactory performance is now acknowledged to be one of the prevalent symptoms since the early stages of the disease. Less clear are the incidence, extent and pathophysiology of taste function. The purpose of the present review is to summarize the state of the art in taste literature. To provide a better understanding of the available results, we will also discuss the different methods for taste evaluation and the other potential confounders to be addressed by future research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The gustatory system detects the food components, giving us information about the nature of the food ingested. Thus, we are informed about the pleasantness or unpleasantness of the food but we are also protected by distinguishing between edible and inedible food. In cooperation with the olfactory system, taste plays an important role in our interaction with the environment, influencing our behavior and memory processes [1]. Olfactory and taste disorders can have important effects on the quality of life, however, we can realize their importance only when they are lost [2].
The anatomy of taste is complex but its knowledge is important to reach a more clear clinical picture of its dysfunctions [1, 3]. Various nerves carry the taste sensation, each from a particular area (Fig. 1). Moreover, also the somatosensory information (e.g. pain, temperature, touch) carried by the trigeminal and glossopharyngeal nerves is important to produce, together with retronasal olfaction, a complete experience of flavor. Therefore, for a correct assessment of taste it is crucial to test the somatic sensory system and—more importantly—both olfaction and taste separately [4].
Diagram of the anatomy of taste from the periphery to the cortex (see text for details). Different cranial nerves carry the taste sensation: chorda tympani (VII) from the anterior tongue, the greater superficial petrosal nerve (VII) from the palate, glossopharyngeal nerve (IX) from the posterior tongue, and vagus nerve (X) from the throat
Although Parkinson’s disease (PD) is well characterized by the motor symptoms, the associated non-motor symptoms have received growing attention in recent years [5]. Among them, olfactory deficit is widely recognized as a very early biomarker of the disease, with a prevalence of about 90 % in sporadic PD patients [6]. Therefore, in case of idiopathic olfactory deficit, especially if associated with REM sleep behavior disorders or depression, PD should be considered as a potential underlying condition [7]. Indeed, there are increasing efforts to find biomarkers in PD to obtain an earlier and more accurate diagnosis [5].
Taste performance in PD has not fully clarified so far. Here we addressed the current knowledge in this field. A literature search was performed for English, German, French and Italian language publications by accessing PubMed database with no date restrictions and using the following keywords: ‘taste’ AND ‘Parkinson’s disease’. In addition, supplementation with the reference list from the articles was used as necessary. To date, there are seven studies carried out with a variable sample size and different assessment methods [8–14]. Prior to discuss these works, which are summarized in Table 1, we will briefly describe the most used methods to investigate the gustatory function, to guide readers in the understanding of limits and strengths of available literature.
Taste evaluation: methods
Taste evaluation can be performed in different ways, depending on a number of factors (e.g. geographic differences in available methods). In addition, test results can also be interpreted differently. As a consequence, the data on taste disorders exhibit great variation [15].
In general, taste performance can be assessed in the whole oral cavity (whole mouth test) or in particular tongue regions (regional test). The latter modality allows the assessment of single gustatory nerve afferents. All these methods rely on subjective responses and need patient’s collaboration.
A popular method to measure the taste threshold is the “three drop test” [16]. In this test, three drops (one containing a taste stimulus and the other two being pure water) are presented to the patient’s tongue. When the patient identifies the taste three times in a row the threshold is defined at a given concentration [2]. This method has not been established in clinical routine because it is time consuming, requires a trained staff and the solutions have to be prepared just prior to the test. Moreover, due to the immediate dissolving and dilution of the taste solution on the tongue’s surface, it is difficult to detect localized losses of taste perception [17].
Another method, mainly used in Japan, involves the use of filter paper discs (FPD), which are discs of 5 mm in diameter placed on the tongue with tweezers. This test can measure the recognition threshold for the four basic tastes sweet, salty, sour and bitter [19]. The umami taste (glutamate) can be also administrated, although this it is not regularly assessed [20].
In 2000 Ahne et al. [21] developed a whole mouth gustatory test based on tasting tablets. Patients receive 28 tablets containing sweet, sour, salty and bitter tastes in six concentrations plus four empty tablets. This test is easy to administer (e.g. after middle ear surgery when it is possible to damage the chorda tympani nerve), has a long shelf life but it does not allow testing of regional taste in different tongue’s parts.
Hummel et al. [22] also developed a taste test consisting of thin edible wavers. These wavers made of flour and water contain supra-threshold concentrations of tastants. Tasteless wavers are also used. Their shelf life is 2–3 years. They can be used both for regional or whole mouth testing but this test is not designed for the quantitative assessment of gustatory function [17].
Another test is the “Whole Mouth Test” (WMT), which consists of four supra-threshold taste solutions in 10 g of water (sucrose 10 % for sweet, citric acid 5 % for sour, sodium chloride 7.5 % for salty and quinine 0.05 % for bitter) sprayed into the oral cavity. Patient’s mouth is rinsed well with water in between the exposures to the tastants. This is a rapid screening test for the four basic taste qualities.
In 2003 Kobal designed the “Taste Strips Test” (TST), a technique based on strips made from filter paper, soaked with different taste solutions and dried [17, 18]. Each taste quality is tested with different concentrations (sweet: 0.4, 0.2, 0.1, 0.05 g/ml sucrose; sour: 0.3, 0.165, 0.09, 0.05 g/ml citric acid; salty: 0.25, 0.1, 0.04, 0.016 g/ml sodium chloride; bitter: 0.006, 0.0024, 0.0009, 0.0004 g/ml quinine hydrochloride). Umami was not included because it is not a familiar taste for most Europeans. TST is a validated test method for ascertaining tasting performance of the whole mouth. Strips are placed on the tongue and the patient is asked to move it with the mouth closed. Regional test can be also performed by placing the strip only on specific parts of the tongue, with patient’s mouth open until a response is provided.
In addition to techniques based on administration of chemicals on the tongue, electrogustometry (EGM) can be used. EGM uses electric current (generally delivered over 1.5s) as the stimulus and, as the other methods mentioned above, it relies on patient’s subjective responses. EGM has already been described in the 50s, but its use is quite limited [23]. Nevertheless, EGM (along with the filter paper disc method) is very popular in Japan and it has been introduced as routine procedures in almost all otorhinolaryngological institutions [24]. In 1974 Tomita began to develop EGM for the assessment of taste disorders [25]. At present, a TR-06 electrogustometer (Rion Company, Tokyo, Japan) is generally used. It delivers a low intensity current of 3–400 microampere (µA) through a stainless steel 5-mm circular electrode applied to the upper tongue surface and referenced to a neck band (indifferent electrode). The stimulus current is increased using a single staircase approach until the subject recognizes a taste sensation. This gives a taste recognition threshold measurement, expressed in decibel (dB). The signal can be varied from −6 to −34 dB and it is perceived variously as metallic, sour, salty or bitter. The patient can signal any taste sensation on the tongue with the aid of a response button connected to a small buzzer [10]. This technique is generally regarded as a sensitive and rapid measure of taste threshold that facilitates regional testing. A strong association between raised EGM threshold and chorda tympani lesions or the number of fungiform papillae have been described [26, 27] as well as a correlation with the taste performance of 114 healthy controls [28]. By contrast, the value of EGM has been questioned in a study of 32 patients because of a poor correlation with the WMT [29]. A theoretical disadvantage of EGM is that the patient may inadvertently report sensation via the trigeminal nerve. Yet, the sensory threshold for lingual trigeminal receptors is higher than that for taste [11]. In conclusion, EGM seems to complement chemical taste tests rather than substitute for them [28]. The good correlation between the EGM and FPD method found in another study reassures that EGM actually measures taste [23].
Gustatory evoked potentials can also be used for objective examination of taste perception [30] but, to our knowledge, there are no studies adopting this investigation method in PD.
PD and taste assessment: state of the art (Table 1)
Sienkiewicz-Jarosz et al. “Taste responses in patients with Parkinson’s disease” (2005)
This is the first taste investigation reported in PD patients. Taste responses (rated intensity, pleasantness, identification) were evaluated in 30 PD patients and 33 healthy controls aged 44–75 years. Only non-demented subjects were included to the study. The authors evaluated the self-reported smell/taste impairment. More than one-third of the patients reported subjective smell impairment whereas taste problems were indicated by four PD and two controls; only one PD patient reported isolated taste impairment.
Intensity and pleasantness were tested by customized method consisting of 13 different FPD of 1.3 cm in diameter and containing sucrose (sweet), quinine (bitter), citric acid (sour) or sodium chloride (salty). Each participant received and rated 13 different FPD. The subjects were also exposed to 100 ml samples of chocolate and vanilla milk. This method was used instead of tastant solutions to avoid olfactory stimulation via the so-called retronasal route, which could be a confounding factor, given the well-known olfactory dysfunction of PD patients. EGM was also used to obtain taste thresholds.
Perceived pleasantness of the sweet samples (sucrose, chocolate milk and vanilla milk) did not differ between the PD and control group. Moreover, ratings of the other samples (bitter, sour and salty) were also similar in the PD patients and controls. Therefore, the PD group did not show any major sensory deficit as assessed by intensity rating and identification of the gustatory samples; the authors also concluded that the dopaminergic dysfunction did not lead to any obvious alteration in more hedonic aspects of taste, i.e. perceived pleasantness of gustatory stimuli. In fact, the PD patients rated the filter papers soaked in the lowest quinine concentration as more intense, compared with the control group. This finding mirrored the lower EGM thresholds observed in the patients group compared with the controls.
Lang et al. “Taste in dementing diseases and Parkinsonism” (2006)
This study examined taste in 52 patients with various type of dementia (Alzheimer type in 24). Out of the 28 patients with non-Alzheimer type of dementia, 6 had PD-dementia (PDD). A control group of 52 subjects was also enrolled. Taste was assessed using the WMT and TST. Olfaction was evaluated using the Sniffin’ Sticks Test (SST), 12-stick version [31].
Globally, the TST results in demented patients were significantly different than controls (P = .036, Mann–Whitney U test), as were those for the WMT and SST (P = .000). As regards different taste qualities, sweet was recognized best in both taste tests (Friedman ANOVA, P = .029 for the WMT and .000 for the TST) whereas sour was recognized with the greatest difficulty. Finally the authors found that patients with Parkinsonism persistently scored with lower values than other patients and controls in all types of smell and taste tests. The main differences were on WMT sour and on TST salty taste qualities.
Shah et al. “Abnormality of taste and smell in Parkinson’s disease” (2009)
The authors investigated 75 non-demented PD patients and 74 controls. Taste threshold was measured by means of EGM, with electrodes separately applied to the right and left side of the tongue (on either side of the tip and the most lateral circumvallate papilla). They also evaluated olfaction by the University of Pennsylvania Smell Identification Test (UPSIT) in which 40 different odors are used and a forced choice is made from four possible answers.
Impaired taste appreciation was found in about 27 % of patients, particularly for fungiform papillae and vallate papilla, where the mean taste threshold was higher than controls. There was no significant effect of age, disease severity or smell sense, although the UPSIT score in PD patients was markedly lower than controls. Because of the overlap between patients and controls the authors argued that the taste test threshold could not be used alone as a diagnostic tool. The sensitivity of UPSIT was greater than EGM-based taste measurement, but the combination of abnormalities on both smell and taste, in their opinion, would support a diagnosis of PD. Interestingly, separate assessment of patients who were receiving levodopa preparations, compared to those who were not, showed no difference in mean taste thresholds. This study concluded that the independent abnormalities of smell and taste in PD most plausibly relate to their separate anatomical pathways.
Deeb et al. “A basic smell test is as sensitive as dopamine transporter scan: comparison of olfaction, taste and DaTSCAN in the diagnosis of Parkinson’s disease” (2010)
These authors evaluated 73 patients with early Parkinsonism by means of Unified PD Rating Scale (UPDRS), DAT-SPECT imaging, EGM and UPSIT. The anterior and posterior areas of the tongue were tested bilaterally. Olfactory event-related potentials (OERPs) were also performed in 49 patients. Subjects were also asked to subjectively rate their taste and olfactory abilities on a 6-point scale from absent (1) to excellent (6). Patients were followed up for an average period of 15.3 months and finally a clinical diagnosis of idiopathic PD or non-PD was made. Fifty patients were diagnosed as PD (age range 33–80 years) and 23 non-PD (age range 40–78; mean age 63; M:F = 14:9). Patients were not on anti-parkinsonian medications or received treatment for <3 months prior to enrolment. Different subsets of controls were enrolled: 311 for UPSIT, 74 for OERPs, 75 for EGM and 15 for DAT-SPECT.
EGM thresholds were impaired in 22 % of the PD group, the same percentage of patients was aware of some taste impairment. By contrast 86 % of PD patients were found to have an olfactory dysfunction but only 39 % of them were aware of it. The authors concluded that patients with early PD have a frequent and severe olfactory deficit that correlates with disease severity, symptom duration and DAT-SPECT but not with taste performance.
Kim et al. “Taste function in patients with Parkinson disease” (2011)
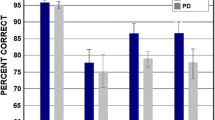
In this study, taste function of 31 PD patients and 29 controls (11 men and 14 women) was assessed quantitatively using TST (Burghart, Wedel, Germany). Olfactory function was assessed using the 12-item Cross-Cultural Brief Smell Identification Test (CC-SIT). The results of this study showed the mean TST score was significantly lower in PD patients as a group, however, the taste function was impaired in female patients only, while it did not differ significantly between patients and controls in men. This finding was likely to be attributable to the lower Mini Mental State Examination (MMSE) score found in female PD patients. However, in PD patients TST scores did not correlate with MMSE or Montreal Cognitive Assessment (MoCA) scores. Likewise, no correlation with age, olfactory function, severity or duration of disease was found.
Sienkiewicz-Jarosz et al. “Sweet liking in patients with Parkinson’s disease” (2013)
This is the second study of Sienkiewicz-Jarosz and collaborators. As primary aim, the authors intended to compare pleasantness rating of sucrose solutions and sweet liking/disliking condition in PD patients and healthy controls. They also evaluated gustatory function by EGM technique and olfactory function by means of SST (16-stick version, Burghart, Wedel, Germany). 20 PD patients (55 % women) and 20 healthy controls (70 % women) were examined. Only patients with stages I-III according to Hoehn and Yahr scale and with a MMSE score higher than 24 were recruited. Intensity and pleasantness of tastant were addressed by administrating sucrose solutions at different concentrations, in two repetitions. For neutral stimulus they used deionized water. Rated intensity and pleasantness of higher sucrose concentrations did not differ between PD patients and healthy controls. As in their previous study [8], EGM was performed with the Rion TR-06 electrogustometer (TR-06; Rion Co., Ltd., Tokyo, Japan). Here they found that EGM thresholds did not differed between PD patients and controls. By contrast, PD patients showed a significant impairment of olfactory identification ability as compared to control subjects.
Cecchini et al. “Taste performance in Parkinson’s disease” (2014)
Taste performance was investigated in 61 PD patients (range 48–85 years) and 66 controls (range 43–91 years) using the WMT and TST. Olfactory function was also assessed by means of SST 16-stick version (Burghart, Wedel, Germany). Taste and smell were also subjectively investigated by asking a question regarding the personal rating of smell and taste abilities. Exclusion criteria for both patients and controls were cognitive decline, otolaryngology disorders, major systemic diseases or any condition or drug interfering with taste or smell, history of middle ear surgery, Bell’s palsy, cranial trauma or stroke.
TST score was significantly lower in patients than controls, while WMT showed no differences. The authors explained this discrepancy as the results of the different methodology of the two tests, since WMT uses substances at supra-threshold concentration typical of the daily life, meaning that it is not able to capture slight impairment of taste function. This notion is also in keeping with the lack of correlation between objective and subjective measures of taste performance. Finally, the olfactory evaluation confirmed the results extensively reported in the literature as there was a significant reduction of the SST score in patients than controls. The authors partly attributed the taste decrease to a chemosensory interaction with olfaction and disease progression with cortical involvement.
The aforementioned studies are summarized in Table 1.
Discussion and future directions
As reviewed above, different taste tests are commonly applied worldwide and some of them were also used in PD patients. An impairment of taste has been described by all researcher groups but one [8, 13]. Although reported with highly variable prevalence, it is now evident that taste can be affected in PD although much less frequently than smell. An interesting source of speculation is the neuronal underpinning of such dysfunction. At present, the topographical significance of taste impairment in PD is unclear but given the sparing of the first and second gustatory neurons (Fig. 1), it most likely relies on the involvement of the frontal operculum or orbitofrontal cortex [10, 11, 14]. Therefore, taste dysfunction can be linked to the advanced phases of the disease [11] and might probably represent a hallmark of pathologically advanced disease (Braak stage 5), possibly being a risk factor for dementia. Not surprisingly, studies enrolling patients in the early phase only detected a taste dysfunction in a subgroup of patients while the only study performed in PDD disclosed a marked impairment, even worse than other dementia patients [9]. This is in contrast with smell dysfunction, which is almost invariably found in almost all PD patients and represent an early marker of the disease [11]. In keeping with this line of reasoning, smell and taste dysfunction were not found to correlate (Table 1) and only one study [14] found a marginal significance, likely due to the well-known impact of olfaction on taste experience.
These concepts would also help the diagnostic workout of PD, as Deeb and coworkers have proposed that taste testing alone could not be used diagnostically, but given the high sensitivity of UPSIT in PD, abnormality of both smell and taste would support a diagnosis of PD; conversely, a normal UPSIT and taste threshold in suspected PD would call for a diagnostic review. However, since the smell impairment starts gradually, patients are less likely to be aware of the problem and simply asking patients about their sense of smell has no usefulness; validated assessment of smell seems to have an accuracy comparable to the more sophisticated and expensive DAT-SPECT [11]. Notwithstanding, in our opinion it is still too early to draw conclusions about the clinical value of the taste impairment generally reported by PD studies. In fact, as broad effects of chemosensory interaction could be also considered [33], the decreased gustatory function might not reflect a direct impairment due to PD.
In addition, none of the studies performed so far investigated taste performance in a longitudinal fashion. Indeed, to really explore the causes of PD taste impairment, and to know how consistent and severe the taste disorder is, future prospective investigations are needed. This could help in understanding if the gustatory deficit is in relationship with a disease progression with cortical involvement, as suggested by some works reported. Certainly, the employment of validated tests will be of particular importance as well as the exclusion of concomitant pathologies that may influence smell/taste performance (i.e. otolaryngology disorders, history of middle ear surgery, smoking/alcohol habits, diabetes mellitus, thyroid dysfunction, cranial trauma or stroke, just to mention few of them). Other confounders should be addressed by future studies. Even if one study did not find any influence on taste exerted by levodopa [10], drug effects and changes in salivary constitution could not be excluded completely as about 5 % patients report change in taste when receiving this drug, probably due to excretion in saliva [32]. Moreover, on the basis of the strong correlation between taste and olfaction, it would be always recommended to evaluate in parallel also the olfactory performance. In conclusion, while a waiting for future longitudinal studies and in spite of a fair number of still unsolved issues, a gustatory deficit should be listed among the possible non-motor manifestations of PD.
References
Huart C, Collet S, Rombaux P (2009) Chemosensory pathways: from periphery to cortex. B-ENT 5:3–9
Hummel T, Landis BN, Hüttenbrink KB (2011) Smell and taste disorders. GMS Curr Top Otorhinolaryngol Head Neck Surg 10:1–15
Hummel T, Welge-Lüssen A (2006) Taste and smell. An update. In: Advances in oto-rhino-laryngology, Basel, Karger, vol. 63, pp 152–190
Fark T, Hummel C, Hähner A et al (2013) Characteristics of taste disorders. Eur Arch Otorhinolaryngol 270:1855–1860
Breen KC, Drutyte G (2013) Non-motor symptoms of Parkinson’s disease: the patient’s perspective. J Neural Transm 120:531–535
Doty RL (2012) Olfactory dysfunction in Parkinson disease. Nature Rev Neurol 8:329–339
Hüttenbrink KB, Hummel T, Berg D et al (2013) Olfactory dysfunction: common in later life and early warning of neurodegenerative disease. Dtsch Arztebl Int 110:1–7
Sienkiewicz-Jarosz H, Scinska A, Kuran W et al (2005) Taste responses in patients with Parkinson’s disease. J Neurol Neurosurg Psychiatry 76:40–46
Lang CJG, Leuschner T, Ulrich K et al (2006) Taste in dementing diseases and parkinsonism. J Neurol Sci 248:177–184
Shah M, Deeb J, Fernando M et al (2009) Abnormality of taste and smell in Parkinson’s disease. Parkinsonism Relat Disord 15:232–237
Deeb J, Shah M, Muhammed N et al (2010) A basic smell test is a sensitive as dopamine transporter scan: comparison of olfaction, taste and DaTSCAN in the diagnosis of Parkinson’s disease. QJMed 103:941–952
Kim H-J, Jeon BS, Lee J-Y et al (2011) Taste function in patients with Parkinson’s disease. J Neurol 258:1076–1079
Sienkiewicz-Jarosz H, Scinska A, Swiecicki L et al (2013) Sweet liking in patients with Parkinson’s disease. J Neurol Sci 329:17–22
Cecchini MP, Osculati F, Ottaviani S et al (2014) Taste performance in Parkinson’s disease. J Neural Transm 121:119–122
Welge-Lüssen A, Dörig P, Wolfensberger M et al (2011) A study about the frequency of taste disorders. J Neurol 258:386–392
Henkin RI, Gill JR, Bartter FC (1963) Studies on taste thresholds in normal men and in patients with adrenal cortical insufficiency: the role of adrenal cortical steroids and serum sodium concentration. J Clin Invest 42:727–735
Mueller C, Kallert S, Renner B et al (2003) Quantitative assessment of gustatory function in a clinical context using impregnated “taste strips”. Rhinology 41:2–6
Landis BN, Welge-Lüssen A, Brämerson A et al (2009) Taste strips—a rapid, lateralized, gustatory bedside identification test based on impregnated filter papers. J Neurol 256:242–248
Tomita H, Ikeda M, Okuda Y (1986) Basis and practice of clinical taste examinations. Auris Nasus Larynx 13:S1–S15
Kuriwada SS, Kawai M, Noriakishoji, et al (2012) Assessment of Umami taste sensitivity. J Nutr Food Sci S10:003. doi:10.4172/2155-9600.S10-003
Ahne G, Erras A, Hummel T et al (2000) Assessment of gustatory function by means of tasting tablets. Laryngoscope 110:1396–1401
Hummel T, Erras A, Kobal G (1997) A test for the screening of taste function. Rhinology 35:146–148
Berling K, Knutsson J, Rosenblad A et al (2011) Evaluation of electrogustometry and the filter paper disc method for taste assessment. Acta Otolaryngol 131:488–493
Ikeda M, Aiba T, Ikui A et al (2005) Taste disorders: a survey of the examination methods and treatments used in Japan. Acta Otolaryngol 125:1203–1210
Tomita H, Ikeda M (2002) Clinical use of electrogustometry: strengths and limitations. Acta Otolaryngol 546:27–38
Groves J, Gibson WP (1974) Significance of taste and electrogustometry in assessing the prognosis of Bell’s (idiopathic) facial palsy. J Laryngol Otol 88:855–861
Miller SL, Mirza N, Doty RL (2002) Electrogustometric thresholds: relationship to anterior tongue locus, area of stimulation, and number of fungiform papillae. Physiol Behav 75:753–757
Ellegård EK, Hay KD, Morton RP (2007) Is electrogustometry useful for screening abnormalities of taste? J of Laryngol Otol 121:1161–1164
Murphy C, Quiñonez C, Nordin S (1995) Reliability and validity of electrogustometry and its application to young and elderly persons. Chem Senses 20:499–503
Hummel T, Genow A, Landis BN (2010) Clinical assessment of human gustatory function using event related potentials. J Neurol Neurosurg Psychiatry 81:459–464
Daum RF, Sekinger B, Kobal G et al (2000) Riechprüfung mit “sniffin sticks” zur klinischen Diagnostik des Morbus Parkinson. Nervenartzt 71:643–650
Siegfried J, Zumstein H (1971) Changes in taste under L-DOPA therapy. Z Neurol 200:345–348
Landis BN, Scheibe M, Weber C et al (2010) Chemosensory interaction: acquired olfactory impairment is associated with decreased taste function. J Neurol 257:1303–1308
Acknowledgments
AF received speaker’s fees or honoraria from Abbvie, UCB pharma, Medtronic, Boston Scientific, TEVA; he is in one of the advisory boards for Abbvie and TEVA.
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cecchini, M.P., Fasano, A., Boschi, F. et al. Taste in Parkinson’s disease. J Neurol 262, 806–813 (2015). https://doi.org/10.1007/s00415-014-7518-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-014-7518-1