Abstract
In decomposed or skeletonized bodies, conventional matrices used in forensic toxicology may no longer be available for analysis. The aim of this paper was to test the survival and detection of toxicological substances in dry bone samples with over 23 years of post-mortem interval. In this perspective, bone samples from the cranium, ribs, and vertebrae of seven skeletons from the CAL Milano Cemetery Skeletal Collection, buried for over 23 years, fully decomposed and altered by taphonomic factors were selected based on their ante-mortem data, which included verified or suspected drug addictions or overdose. Qualitative and quantitative analyses were performed with Dionex™ ASE™ 350 Accelerated Solvent Extractor and Q-Exactive Orbitrap–mass spectrometry with a HPLC system. Positive results were obtained in six of the seven cases, and different psychoactive drugs (and in some cases their active metabolites) were detected, including analgesic (two opioids: methadone and buprenorphine) and anxiolytic drugs (benzodiazepines, in particular delorazepam, diazepam, nordiazepam, and lorazepam), a cannabinoid metabolite (THCCOOH) as well as metabolites of stimulants (benzoylecgonine and MDA). Consequently, this research shows that toxicological substances may be found in bone tissue after over 23 years of post-mortem interval.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Forensic toxicology consists in the search for exogenous compounds in different matrices and tissues in order to provide additional information in a medicolegal setting [1,2,3]. Conventional specimens used in forensic toxicology analysis include blood and urine [4,5,6,7]. However, when a human body is extremely decomposed, or even skeletonized, these specimens may not be available due to their degradation during decomposition or their contamination [4,5,6]. Thus, alternative matrices are necessary to perform toxicological analysis [4,5,6,7]. To be suitable for toxicological analyses, these alternative matrices must remain well-preserved for a long time after death to allow the detection of drugs [5, 8, 9]. The bone tissue can constitute such an alternative matrix, especially given that it is the only remaining sample material which can be used for toxicological analysis after decomposition and long PMIs (post-mortem intervals) [6, 10,11,12], along with teeth [13].
Studies have shown that the bone tissue may be used as an alternative matrix to perform analyses of drugs: in particular in human models [6, 8, 9, 11, 14,15,16,17,18,19,20,21,22,23,24], demonstrating the use of bone marrow [6, 9, 14, 16, 18, 24, 25] and bone tissue [6, 11, 15, 19,20,21,22,23] for the detection of drugs. Nonetheless, in most studies, the samples are taken immediately during the autopsy and analyzed [6, 9, 11, 17, 19,20,21,22,23] or buried for3 weeks [15] or 1 year [11], with findings including amphetamines, antidepressants, antipsychotic drugs, anticholinergics, anticonvulsants, benzodiazepines, cocaine, cannabinoids, opioids, and bromisovalum (a hypnotic sedative drug). The lack of studies on human models with a longer PMI limits our understanding of the possibility to detect drugs in bone with a PMI over a year. In fact, to the best of our knowledge, Grellner and Glenewinkel [18] performed the only study with a PMI over 1 year (a hyoid bone after 7.5 years of burial) but no details were provided on the methodology used or on the results obtained. This demonstrates the importance of this pilot study, despite the lack of some antemortem data and the limited number of samples, as it is the first one to test dry bone with a PMI of over 20 years for toxicological analyses.
In this paper, different dry bone samples from skeletal remains with a PMI of over 23 years and antemortem data relating to their condition during life were processed using accelerated solvent extraction (ASE) demonstrating that toxicological substances may be found in bone tissue even after a very long PMI.
Materials and methods
Bone samples and preparation for analysis
Seven cemeterial skeletons from the CAL (Collezione Antropologica LABANOF) Milano Cemetery Skeletal Collection [26] with verified or suspected drug addictions, intoxication, or overdose in their associated antemortem and perimortem documentation were selected for toxicological study. The CAL Milano Cemetery Skeletal Collection is constituted of 2127 unclaimed skeletons, housed in the LABANOF (Laboratorio di Antropologia e Odontologia Forense) in the Department of Biomedical Sciences for Health in the University of Milan, in accordance with article 43 of the Italian National Police Mortuary Regulation (10 September 1990, no. 285) [26]. The individuals selected included two females and five males; all were inhumed for about 20 years in a cemetery of Milan and based on the dates of death, the post-mortem intervals ranged between 23 and 29 years (Table 1).
All samples can be considered specimens of completely skeletonized individuals, in other words, dry bones. The skeletons were preserved in appropriately sized boxes in rooms with a dry environment and protected from light to prevent bone deterioration. Unfortunately, the autopsy reports were not available and so exact drugs taken in these cases could not be specified.
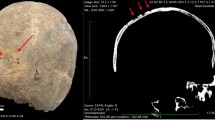
For each individual involved in this study, three bone samples were selected, including one from the cranial vault, one from a rib, and one from a body of lumbar vertebra. These bones were chosen in an effort to be representative of the material available in real scenarios, as they have a high potential of recovery in forensic or archaeological contexts, even if fragmented.
In addition, middle ribs and lumbar vertebral bodies constitute ideal bone samples for toxicological analyses, as they are heavily perfused with blood.
Bone samples of about 5 g were cut with a hand saw. In the cranium, when an autopsy had been performed, the sample was taken from the parietal or occipital bone using one of the cutting marks realized during the autopsy to limit bone damage. Alternatively, in the absence of autopsy cut marks, the sampling was performed from the foramen magnum in order to avoid extensive destruction of the cranium.
The quantification of drugs deposits was performed to understand whether the deposits were present in detectable quantities or only in traces and was not subjected to further interpretation. Indeed, the quantifications reported refer to the deposits and can in no way reflect the original drug intake by the individual. After the sampling, bone samples were pulverized using a ball mill until complete reduction to powder, before being submitted to accelerated solvent extraction (ASE) and HPLC-MS (high-performance liquid chromatography-mass spectrometry) analysis.
Chemicals and reagents
All reference standards involved in this study were purchased from Merck Life Science (diazepam 1.0 mg/mL in MeOH; methadone 1.0 mg/mL in MeOH; lorazepam 1.0 mg/mL in MeOH; MDA (3,4-methylenedioxymphetamine) 1.0 mg/mL in ACN; nordiazepam 1.0 mg/mL in MeOH; buprenorphine 1.0 mg/mL in MeOH; benzoylecgonine 1.0 mg/mL in MeOH; delorazepam 100 μg/mL in MeOH; and THCCOOH (11-nor-9-carboxy-Δ9-tetrahydrocannabinol) 1.0 mg/mL in MeOH. Solvents used in the extractive processes were purchased by VWR International (Radnor, PA, USA) (methanol 100%; chloroform 99.2%; ethyl acetate 99.9%; dichloromethane 100%; isopropanol ≥ 99.9 %, LC-MS grade; n-hexane 98%) and Merck (hydrochloric acid 37–38%; acetone ≥ 99.8%). Buffer solution pH 6.88 was purchased from PanReac AppliChem GmbH (Darmstadt, DE).
ASE: accelerated solvent extraction
The ASE is an alternative automatized procedure for the extraction and purification of xenobiotics from biological matrices. Usually, the ASE is used in the botanical field and animal subjects, but for the purpose of this research, it was applied to toxicological analyses [27,28,29].
The ASE instrument utilized was an ASE 350 Accelerated Solvent Extractor (Thermo-Fisher Scientific, Waltham, MA, USA). For the ASE, 100 ng of internal standard SKF 525-A (Proadifen hydrochloride, in powder form, purchased from Sigma-Aldrich, Darmstadt, DE) were added to the 0.5 g of every matrix sampled. Then, the material was poured in 5-ml stainless-steel cells, provided with glass fiber 20-mm filters (Restek Corporation, Bellefonte, PA, USA), and filled with Thermo Scientific ASE™ Prep DE. The cells, tightly sealed, were placed on an ASE 350 Accelerated Solvent Extraction. The elution solution used was composed by n-hexane and acetone with a volume ratio 4:1.
The conditions for the extraction protocol of the Dionex™ ASE™ 350 Accelerated Solvent Extractor included a 60 °C temperature with a pressure of 1500 psi, a Heat-up Time and Static Time of 5 min, a flush volume of 60%, a purge time of 100 s, a static cycle of 1, a total extraction time of 12 min per sample, and a total solvent use of 30 mL per sample.
The eluates were collected in glass vials and dried in a vacuum rotary evaporator. Then, the samples were restored with 10 μL of methanol. Two microliters of these final solutions were analyzed using the GC-MS TSQ 9000 Triple Quad and the Q-Exactive Orbitrap–mass spectrometry with a HPLC system.
HPLC-MS: high performance liquid chromatography-mass spectrometry analysis
Q-Exactive Orbitrap–mass spectrometry with a HPLC system (Thermo Fisher Scientific, San Jose, CA, USA) constituted by a Surveyor MS quaternary pump with degasser, Surveyor AS auto-sampler, oven with Rheodyne valve with a 20-μL loop. For chromatographic separation, we used a HPLC column with reverse phase Synergi Hydro-RP (150 × 2.0 mm, particle dimension of 4 μm) and a C-18 pre-column (4 × 3.00 mm) (Phenomenex, Torrance, CA, USA). Solvent A was used for analysis (20 mM ammonium formate in water; powder ≥ 99.995%) while solvent B (formic acid 0.1% in MeOH) represented the mobile phase utilized for the gradient. At time 00 s, solvents A and B were dosed at 10% and 90%, respectively. Solvent A was increased to 95% at 13.00 min until 20.00 min and then decreased to 10% at 22.00 min until 28.00 min. The detector used was a Thermo Q-Exactive Orbitrap (Thermo Scientific, San Jose, CA, USA) equipped with a Heated Electrospray Ionization Source (HESI). Capillary and vaporization temperatures were set at 330 °C and 280 °C while electrospray voltage was fixed at 3.50 kV with a positive mode. Complete scanning acquisition was combined with an independent data acquisition (IDA) mode providing MS2 spectrum for confirmation response according to an inclusion list. Resolution power of the full size (FS) was positioned at 70,000 full width at half maximum (FWMH). A scanning interval between 50 and 650 m/z was selected. Automatic gain control (AGC) was set at 1 × 10−6 and maximum injection time was fixed at 200 ms. The DIA segment operated with positive mode at 35,000 FWHM and the AGC target was set at 5 × 10−4 with a maximum injection time of 100 ms. The quadrupole filtered precursor ions with an isolation range of 2 m/z. Fragmentation of the precursors was optimized with a normalized collision energy in 3 steps (NCE) (10-40-60 eV).
All data obtained were then analyzed with the XcaliburTM software, and exact masses were studied using M/z Cloud Library.
GC-MS: gas chromatography–mass spectrometry analysis
A 5890 Agilent Technologies Gas Chromatograph with a Mass Selective Detector 5975 was used for this study. The instrument was equipped with a Chromopack CP-SIL 8 CB column (length 15 m, internal diameter 0.25 mm, and coating of 0.25 μm).
The processing method was set with the following characteristics: oven temperature at 100 °C for the first 2 min, increasing of the temperature to 160 °C with an increment of 40 °C/min and increasing from 160 to 290°C with an increment if 8 °C/min with a steady temperature for 1 min.
Injection temperature was at 270 °C and interface temperature was at 250 °C. Splitless: 45 s. Mass selected detector (MSD) scanning was from 40 to 650 m/z.
Both techniques were used for screening: GC-MS was performed to complement HPLC-MS analyses in order to detect the substances that are not easily ionizable with a standard HPLC-MS technique. For instance, HPLC-MS is less sensitive to the detection of barbiturates whereas GC-MS detects them more easily. However, no substance was found, for which gas chromatography resulted to be more suitable.
Method validation
Evaluation of method performance including limit of detection (LOD), lower limit of quantification (LLOQ), linearity, accuracy, precision, extraction recovery, and carryover was performed according to the Scientific Working Group for Forensic Toxicology [30].
Standard samples for all the analytes involved at three different concentrations and prepared in duplicates were used for evaluating linearity in calibration curves. The LLOQ was considered as the lowest concentration that gives a reproducible instrument response with a coefficient variation (CV%) < 10% and a signal-to-noise (S/N) ratio ≥ 10. The LOD was evaluated as the lowest concentration that gives a reproducible instrument response with a ratio S/N ≥ 3.
Calibration curves for the validation of the study were prepared for each substance with 4 calibration points performed twice per compound: diazepam (0.5–1–2–5 ng/ml; 10–20–50–100 ng/ml); delorazepam (2–5–10–20 ng/ml); nordiazepam, MDA, and benzoylecgonine (5–10–20–50 ng/ml); lorazepam and buprenorphine (2.5–5–10–5 ng/ml); THCCOOH (10–25–50–100 ng/ml); methadone (5–10–25–50 ng/ml; 100–250–500–1000 ng/ml). However, a variation lower than 9% was maintained throughout the preparation. Stability tests of the utilized standards were not performed because the standard solutions, preserved following the indications provided by the producer, do not degrade, considering that the expiration date had not been reached.
Results
Toxicological substances could be found in six of the seven (86%) individuals of the study sample. The different drugs and concentrations obtained per bone sample are reported in Table 2. As a result, different drugs, and their metabolites, were detected and identified, including analgesic opioids (methadone and buprenorphine), benzodiazepines (in particular delorazepam, diazepam, nordiazepam, and lorazepam), a metabolite cannabinoid (THCCOOH), and metabolites of stimulants (benzoylecgonine and MDA).
Discussion
Ribs and cranial bones (as used in this study) have superficial and deep arteries. Superficial arteries are born in the periosteal network and go into the bone diffusing mostly in the peripheral layer of the compact bone. Deep arteries pass through nutritive foramina toward the spongy bone tissue, where they terminate between the bone trabeculae and the bone marrow [31]. In the vertebrae, arteries perfuse the spongy tissue of the vertebral body and spinal process [32].
After the blood vessels enter in bones, it is believed that the mechanisms of incorporation into bones of stable isotopes and trace elements can be applied to drugs. The bone tissue is composed of organic matrix, inorganic matrix, and water. The water part is present in three forms: bulk water, hydrated layer, and deep lattice water. The interaction of bone water with the blood stream is an essential step in xenobiotic absorption [12]. Thus, drugs enter the body and pass through the blood stream into the bones. Indeed, Rubin [12] explained that drugs are incorporated in the bone matrix as part of primary or secondary mineralization through the remodeling. Moreover, as the trabecular structure possesses a higher remodeling rate, drug ions may be entrapped more easily in this part of the bone [12]. Furthermore, the bone tissue can store exogenous substances in a detoxification effort to remove them from the bloodstream and reduce their effects on the other tissues [33,34,35]; the substances are then degraded as they are gradually excreted from the bone matrix into the bloodstream [33, 34]. This means that a fraction of these substances remains trapped inside the bone matrix, largely inorganic due to the decomposition, and can be detected after the death of the individual.
All the drugs detected in this study, had already been reported in literature [6, 22, 23]. Moreover, studies on animal models [36, 37] have compared single and repeated administration of drugs (ketamine and norketamine) on rats [37] and detected acute administration of chemical weapon nerve agents on pigs [38] and a mix of drugs (amitriptyline, citalopram, diazepam, and morphine) in a minipig [36], demonstrating the possibility to detect acute or chronic drugs intake. However, the results should be interpreted with care as they were performed on animal (and thus not human) models and in conditions much different than those of the present study. Nonetheless, no study has ever reported these findings in individuals with a 23 to 29 years of PMI.
Indeed, the positive toxicological results obtained in the present study demonstrate that drugs can be found in dry bones after 23 years of burial and confirmed the suitability of the bone tissue as an alternative matrix for toxicological analyses, even years after death. Specifically, different psychoactive drugs and their metabolites were detected and identified, including: benzoylecgonine, buprenorphine, delorazepam, diazepam, nordiazepam and lorazepam, MDA, methadone, and THCCOOH.
Furthermore, the antemortem data can be reassociated to the drugs detected, although no interpretation regarding acute or chronic drug assumption can be formulated. For example, “drug addiction”, mentioned in cases 3 and 7, may be confirmed as methadone was detected in both cases and THCCOOH in case 7. Indeed, methadone is used to treat opioid addiction and THCCOOH is the metabolite of THC, another drug of abuse. In case 2, the associated documentation “benzodiazepine overdose” may be specified: diazepam, a benzodiazepine, was detected in cranial and costal samples. Moreover, when no specific drugs were mentioned in the antemortem data “overdose with psychoactive drugs” (cases 1 and 6) or “suspected drug overdose” (case 4), toxicological analysis permitted to name specific drugs (e.g., diazepam, MDA, and benzoylecgonine).
Case 5 did not provide positive results in any of the samples. One possible explanation is that during the sampling, the bone sample selected may not have contained any stored deposits of toxicological substances. However, it should be noted that this result does not mean that no toxicological substances were taken during the life of the individual or at the time of death.
In some cases, deposits of different drugs were found in different bone samples of the same individual. These results were expected considering that the mechanisms of drugs incorporation are not clearly understood. It is possible that the deposits were or were not collected during the sampling process, thus explaining why different samples of the same bone may provide different results.
Quantification of drug deposits was performed with the aim to determine whether drugs were found in bones in quantifiable concentrations or only in traces, but no further interpretation was performed as the quantification of drugs referred to the deposits and not to the quantity of drug intake by an individual during life. As a result, we found high quantities of drugs after more than 23 years of burial, thus providing far more significant results than if they had been found only in traces, which could have rendered them disputable. Thus, and despite the differences in the quantification of drugs deposits noted in the samples, no area of the skeleton appeared more susceptible to the accumulation of drugs compared to the others. This is why it is recommended in a forensic case to perform toxicological analyses on different specimens whenever possible, to avoid the potential bias caused by the sampling site.
Conclusion
In this study, bone samples of skeletons with very long PMIs (between 23 and 29 years after death) were analyzed to determine whether toxicological substances could be found in such dry bone forensic scenarios, that is, when bone marrow is no longer suitable for toxicological analysis and the corpse has been subjected to decomposition process and environmental contamination. Consequently, positive results were obtained in 6 of the 7 skeletons of the study sample and permitted the detection of psychoactive drugs and their metabolites, adding further information to the biological profile of the deceased which may orient the search among a missing persons list in forensic identification scenarios.
References
Dinis-Oliveira RJ, Carvalho F, Duarte JA, Remião F, Marques A, Santos A, Magalhães T (2010) Collection of biological samples in forensic toxicology. Toxicol Mech Methods 20:363–414. https://doi.org/10.3109/15376516.2010.497976
Mbughuni MM, Jannetto PJ, Langman LJ (2016) Mass spectrometry applications for toxicology. EJIFCC 27:263–357
Caplan YH (2008) Foreword. In: Jenkins AJ (ed) Drug testing in alternate biological specimens. Forensic Science and Medicine, pp ix–xi
Bévalot F, Cartiser N, Bottinelli C, Guitton J, Fanton L (2016) State of the art in bile analysis in forensic toxicology. Forensic Sci Int 259:133–154. https://doi.org/10.1016/j.forsciint.2015.10.034
Guillot E, de Mazancourt P, Durigon M, Alvarez JC (2007) Morphine and 6-acetylmorphine concentrations in blood, brain, spinal cord, bone marrow and bone after lethal acute or chronic diacetylmorphine administration to mice. Forensic Sci Int 166:139–144. https://doi.org/10.1016/j.forsciint.2006.03.029
Orfanidis A, Gika H, Mastrogianni O, Krokos A, Theodoridis G, Zaggelidou E, Raikos N (2018) Determination of drugs of abuse and pharmaceuticals in skeletal tissue by UHPLC–MS/MS. Forensic Sci Int 290:137–145. https://doi.org/10.1016/j.forsciint.2018.07.004
Watterson J (2006) Challenges in forensic toxicology of skeletonised human remains. Analyst 131:961–965. https://doi.org/10.1039/b609130j
Tattoli L, Tsokos M, Sautter J, Anagnostopoulos J, Maselli E, Ingravallo G, Delia M, Solarino B (2013) Postmortem bone marrow analysis in forensic science: Study of 73 cases and review of the literature. Forensic Sci Int 234:72–78. https://doi.org/10.1016/j.forsciint.2013.10.040
Wietecha-Posłuszny R, Lendor S, Garnysz M, Zawadzki M, Kościelniak P (2017) Human bone marrow as a tissue in post-mortem identification and determination of psychoactive substances—screening methodology. J Chromatogr B Anal Technol Biomed Life Sci 1061–1062:459–467. https://doi.org/10.1016/j.jchromb.2017.08.006
Drummer OH (2008) Drugs in bone and bone marrow. In: Jenkins AJ (ed) Drug Testing in Alternate Biological Specimens. Forensic Science and Medicine, pp 131–136
Raikos N, Tsoukali H, Njau SN (2001) Determination of opiates in postmortem bone and bone marrow. Forensic Sci Int 123:140–141. https://doi.org/10.1016/S0379-0738(01)00529-1
Rubin KM (2018) The current state and future directions of skeletal toxicology: forensic and humanitarian implications of a proposed model for the in vivo incorporation of drugs into the human skeleton. Forensic Sci Int 289:419–428. https://doi.org/10.1016/j.forsciint.2018.06.024
Cattaneo C, Gigli F, Lodi F, Grandi M (2003) The detection of morphine and codeine in human teeth: an aid in the identification and study of human skeletal remains. J Forensic Odontostomatol 21:1–5
Maeda H, Oritani S, Nagai K, Tanaka N (1997) Detection of bromisovalum from the bone marrow of skeletonized human remains: a case report with a comparison between gas chromatography/mass spectrometry (GC/MS) and high-performance liquid chromatography/mass spectrometry (LC/MS). Med Sci Law 37:248–253. https://doi.org/10.1177/002580249703700310
Gorczynski LY, Melbye FJ (2001) Detection of benzodiazepines in different tissues, including bone, using a quantitative ELISA assay. J Forensic Sci 46:916–918. https://doi.org/10.1520/jfs15069j
Schloegl H, Rost T, Schmidt W, Wurst FM, Weinmann W (2006) Distribution of ethyl glucuronide in rib bone marrow, other tissues and body liquids as proof of alcohol consumption before death. Forensic Sci Int 156:213–218. https://doi.org/10.1016/J.FORSCIINT.2005.03.024
Cartiser N, Bévalot F, Fanton L, Gaillard Y, Guitton J (2011) State-of-the-art of bone marrow analysis in forensic toxicology: a review. Int J Legal Med 125:181–198. https://doi.org/10.1007/s00414-010-0525-6
Grellner W, Glenewinkel F (1997) Exhumations: synopsis of morphological and toxicological findings in relation to the postmortem interval: survey on a 20-year period and review of the literature. Forensic Sci Int 90:139–159. https://doi.org/10.1016/S0379-0738(97)00154-0
McIntyre IM, King CV, Boratto M, Drummer OH (2000) Post-mortem drug analyses in bone and bone marrow. Ther Drug Monit 22:79–83
Horak EL, Jenkins AJ (2005) Postmortem tissue distribution of olanzapine and citalopram in a drug intoxication. J Forensic Sci 50:1–3. https://doi.org/10.1520/jfs2004067
Fernandez-Lopez L, Luna-Maldonado A, Falcon M, Mastrobattista L, Navarro-Zaragoza J, Mancini R (2019) Development and validation of a gas chromatography–mass spectrometry method for opiates and cocaine in human bone. J Pharm Biomed Anal 164:636–641. https://doi.org/10.1016/j.jpba.2018.11.015
McGrath KK, Jenkins AJ (2009) Detection of drugs of forensic importance in postmortem bone. Am J Forensic Med Pathol 30:40–44. https://doi.org/10.1097/PAF.0b013e31818738c9
Vardakou I, Athanaselis S, Pistos C, Papadodima S, Spiliopoulou C, Moraitis K (2014) The clavicle bone as an alternative matrix in forensic toxicological analysis. J Forensic Leg Med 22:7–9. https://doi.org/10.1016/j.jflm.2013.11.012
Kojima T, Okamoto I, Miyazaki T, Chikasue F, Yashiki M, Nakamura K (1986) Detection of methamphetamine and amphetamine in a skeletonized body buried for 5 years. Forensic Sci Int 31:93–102. https://doi.org/10.1016/0379-0738(86)90193-3
Kudo K, Sugie H, Syoui N, Kurihara K, Jitsufuchi N, Imamura T, Ikeda N (1997) Detection of triazolam in skeletal remains buried for 4 years. Int J Legal Med 110:281–283. https://doi.org/10.1007/s004140050086
Cattaneo C, Mazzarelli D, Cappella A, Castoldi E, Mattia M, Poppa P, de Angelis D, Vitello A, Biehler-Gomez L (2018) A modern documented Italian identified skeletal collection of 2127 skeletons: the CAL Milano Cemetery Skeletal Collection. Forensic Sci Int 287:219e1–219e5. https://doi.org/10.1016/j.forsciint.2018.03.041
Labella GF, Bousova K, Hollosi L, Arioli F (2016) Comparison between accelerated solvent extraction (ASE) with clean up in-line and quick, easy, cheap, effective, rugged, and safe (QuEChERS) extraction in honey. Int J Heal Anim Sci Food Saf 3(3927):10.13130/2283–10.13927/7018
Richter BE, Jones BA, Ezzell JL, Porter NL, Avdalovic N, Pohl C (1996) Accelerated solvent extraction: a technique for sample preparation. Anal Chem 68:1033–1039. https://doi.org/10.1021/ac9508199
Mottaleb MA, Sarker SD (2012) Accelerated solvent extraction for natural products isolation. Nat Prod Isol 864:1–25. https://doi.org/10.1007/978-1-61779-624-1
Group SW (2013) Scientific working group for forensic toxicology (SWGTOX) standard practices for method validation in forensic toxicology. J Anal Toxicol 37:452–474. https://doi.org/10.1093/jat/bkt054
Anastasi G (2012) Trattato di anatomia umana, 4th ed
Netter FH (2014) NETTER - Atlante Di Anatomia Umana, 5th edn. Elsevier Inc., Phuladelphia PA, USA
Premkumar S (2011) Biology of bone and cartilage. In: Textbook of craniofacial growth, 1st ed. Jaypee Brothers Medical Publisher (P) Ltd, New Delhi, pp 1–4
Saladin S (2018) Bone tissue. In: Anatomy & physiology: the unity of form and function, 8th ed. McGraw-Hill, pp 218–219
Kini U, Nandeesh BN (2012) Physiology of bone formation, remodeling, and metabolism. In: Radionuclide and hybrid bone imaging. Springer-Verlag, Berlin Heidelberg, pp 29–57
Watterson JH, Desrosiers NA, Betit CC, Dean D, Wyman JF (2010) Relative distribution of drugs in decomposed skeletal tissue. J Anal Toxicol 34:510–515. https://doi.org/10.1093/jat/34.8.510
Watterson JH, Donohue JP, Betit CC (2012) Comparison of relative distribution of ketamine and norketamine in decomposed skeletal tissues following single and repeated exposures. J Anal Toxicol 36:429–433. https://doi.org/10.1093/jat/bks045
Rubin KM, Rubin KM, Goldberger BA, Garrett TJ (2020) Detection of chemical weapon nerve agents in bone by liquid chromatography-mass spectrometry. J Anal Toxicol 44:391–401. https://doi.org/10.1093/jat/bkz118
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with animals performed by any of the authors. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Gaia Giordano and Lucie Biehler-Gomez are co-first authors
Rights and permissions
About this article
Cite this article
Giordano, G., Biehler-Gomez, L., Seneci, P. et al. Detecting drugs in dry bone: a pilot study of skeletal remains with a post-mortem interval over 23 years. Int J Legal Med 135, 457–463 (2021). https://doi.org/10.1007/s00414-020-02494-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-020-02494-8