Abstract
Objective
To report routine practice of “perimortem” CT-scan imaging to determine the causes of death in children dying from severe accidental injuries within the first hours following hospital admission.
Settings
Trauma center of a University Pediatric Hospital.
Methods
A retrospective study was conducted in children (0 to 15 years old) referred for severe trauma (GCS ≤ 8) to a regional pediatric trauma center, presenting with at least spontaneous cardiac rhythm and dying within the first 12 h after admission. “Perimortem” CT-scan consisted in high-resolution, contrast-enhanced, full-body CT-scan imaging, performed whatever child’s clinical status. Lethal and associated lesions found were analyzed and classified according to validated scales. The comparison between clinical and radiological examinations and CT-scan findings evaluated the accuracy of clinical examination to predict lethal lesions.
Results
CT-scan performed in 73 children detected 132 potentially lethal lesions, at least 2 lesions in 63%, and 1 in 37% of the cases. More frequent lethal lesions were brain (43%), and chest injuries (33%), followed by abdominal (12%), and cervical spine injuries (12%). Clinical and minimal radiological examinations were poorly predictive for identifying abdominal/chest lesions. Clinical and imaging data provided to the medical examiner were considered sufficient to identify the cause of death, and to deliver early burial certificates in 70 children. Only three legal autopsies were commanded.
Conclusions
Perimortem CT imaging could provide an insight into the causes of death in traumatized children. Performed on an emergency basis near death, it eliminates the difficulties encountered in forensic radiology. It could be a possible alternative to full-scale forensic examination, at least regarding elucidation of the potential, or highly probable causes of death.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In France, the incidence of accidental deaths varies from 9.4/100,000 in 5–14-year-old, to 18.2/100,000 in 1–4-year-old children, falls from heights and traffic accidents being the most frequent accidental mechanisms. As in many European countries, it represents 30% of the registered deaths occurring in 1–15-year-old boys, 22% in girls, and traumatic deaths are the first cause of death in children [1, 2].
Determining the cause of death in severely injured children could have four major implications. The first one is to answer to parent’s questioning about the process resulting in their child’s death occurring after an abrupt traumatic event, by identifying lesions that could directly result in unavoidable death. The second one is, especially in cases of unwitnessed falls and home accidents, to eliminate suspected associated assault or violence. The third one is to contribute to acute care quality assessment by establishing a definite correlation between traumatic lesions and unavoidable deaths. The last one could be to provide valuable information about the associated lesions contributing or causing death by themselves in most current accidents, and to contribute to improvement in child’s safety by proposing specific protective measures.
Despite recent European Union (EU) recommendations, legal autopsies remain rarely performed in French practice after accidental death. State prosecutors could command legal autopsies in less than 50% of adult accidental deaths. In children, affirmative death certificates that correlate with an adequately described accidental mechanism could be frequently considered sufficient for authorities and prevent any further attempts to determine the precise lesions causing death. Autopsies are therefore even less commanded in children dying from accidental trauma than in adults. An additional common concern to waive the need for legal autopsy is to avoid additional burden of heavy procedural constraints to abruptly bereaved parents. This concern could contribute to limit the practice of legal autopsies in children accidental deaths. For all these reasons, the recorded cause of accidental death could be, in many pediatric cases, derived only from physicians’ assumptions, clinical observations, and basic radiological examinations [3, 4]. However, full-scale forensic examinations are not limited to description of injuries and deduction of the cause of death and should obviously include data from precise analysis of scene, circumstances, mechanisms of the accident, and verification of concordance between impacts, soft tissue lesions, vehicle deformations, and other forensic and/or criminological data analysis.
High-resolution CT-scan has emerged as the gold standard for severe head and multiple trauma exploration, with a high capability of detecting silent or ignored lesions in most body areas. It has also gained recent interest in post-mortem evaluation, and it is considered as a very valuable and efficient adjunct to forensic examinations [5,6,7]. However, performed in unventilated and, not perfused subjects, several days after death, it could be significantly artifacted by post-mortem physiological and anatomical processes. Moreover, limited access to equipment in many forensic departments, related to technical, radiation protection, and maintenance constraints, limit its routine use in a few highly specialized units in Europe.
High-resolution CT-scan imaging is, in trauma centers, a routine practice available on a first-priority emergency basis, 24 h a day, for all severely traumatized children. We sought that extending indications to non-survivors could be a valuable routine practice. “Perimortem” CT-scan examination could depict lesions that could not be efficiently detected by physical examination and basic radiological examinations only [8]. Performed within the first instants preceding or following death, with preserved minimal perfusion and adapted alveolar ventilation, it obviates usual artifacts resulting from post-mortem processes. It could provide medical examiners with valuable objective arguments to waive the need for further legal autopsy and avoid thereby a major additional source of psychological burden in parents [6, 7]. We herein report our routine practice of perimortem total body CT-scan examination in children with severe trauma and discuss its value-added adjunct in forensic medical practice and its possible further developments.
Material and methods
As previously described [9], our center is the only pediatric trauma center serving the great Paris area with an approximately 12 million inhabitant population. All children (1 to 15 years old) referred from the accident scene to our center with a severe trauma (defined as a scene GCS of 8 or less, or a severe hemodynamic distress requiring active resuscitation) were prospectively enrolled in the study. All children were resuscitated, intubated, and mechanically ventilated at the scene by a medical team of the SAMU and referred directly to our emergency ward after at least transient successful scene resuscitation. Upon arrival, a dedicated trauma team was in charge of continuing resuscitation. Standard cervical spine and chest X-ray examination were performed immediately upon admission. As soon as possible after minimal hemodynamic and respiratory stabilization, systematic high-resolution spiral multi-slice CT-scan examination was routinely performed including head, cervical spine, and contrast-enhanced chest and abdominal explorations.
Before extending the practice of emergency CT-scan examination to predictable non-survivors (bilateral fixed dilated pupils with undetectable peripheral arterial pulse, intractable extreme hemodynamic instability, or no maintainable spontaneous cardiac rhythm despite active resuscitation), critical care and pediatric radiological department members reached a consensus to structure this practice. All involved personnel were informed about the extension of routine emergency CT-scan examinations to all children whatever their clinical status. Before transferring patients to the radiology ward, information about their moribund condition was always provided to the radiological team members. Hemodynamic resuscitation, monitoring, and mechanical ventilation were continued unchanged under close supervision of the trauma team until completion of CT-scan. A specific protocol with increased flow rate and volume of media infusion was designed, and to guarantee homogenous quality of CT-scan examination, children dead upon arrival who did not benefit from continuing mechanical ventilation during CT-scan examination were excluded from the present analysis, CT-scan examination being there considered as post-mortem examination.
CT-scan examinations from the vertex to the symphysis pubis were performed with a 64-detector high-speed HD Lightspeed VCT system (GE Healthcare® Barrington; Ill. USA). A first spiral acquisition from the vertex to the cervical dorsal junction was performed without IV contrast injection (0,625 /0,625 mm slices, 100 Kv voltage for 0–6 years old, 120 Kv for 6–15 years, 250 mA set auto modulation, for noise index 7). A second acquisition, from the superior orbital plan to the symphysis pubis (0,625 / 0,625 mm slices, 250 mA set auto modulation for noise index 23, 80 Kv for 0–18 months, 120 Kv for 18 months–6 years, and 120 Kv, 300 mA set auto modulation for noise index 25, for 6–15 years), was initiated 50 ms after completion of IV injection of 20 ml/kg bolus contrast (Iomeron® Bracco Imaging France), via a Nemoto automated injector (Medicor® Int. Rotselaar; Belgium), at a rate of 2 ml/s. Late acquisitions completed the examination. Multi-plan axial, coronal, and sagittal reformats were then created. All radiological examinations were analyzed online by a pediatric radiologist aware of clinical status and reviewed retrospectively by a senior pediatric radiologist, a pediatric critical care physician, and a surgeon, blinded from clinical data.
Since total body CT-scan represents a routine emergency practice in all children with severe trauma at our institution, our local institutional review boards waived the need for prior parents’ inform consent for radiological exploration. However, parents were systematically informed about the risks for imminent death, the on-going resuscitation process, and scheduled radiological explorations.
After CT-scan completion, information was provided to family members by a senior pediatric anesthesiologist in charge of hospital resuscitation, in the presence of a specialized trauma-trained psychologist. Non-survivors with persistent GCS 3, fixed dilated pupils, asystole, or pulseless extreme bradycardia were further disconnected from the ventilator, extubated, and pronounced dead. The trauma team leader completed a death certificate, including a precise description of all lesions. As required by French law and regulations, it was transmitted to a registered medical examiner under the authority of the state prosecutor. Prosecutor finally determined the need or waive for further forensic investigations before the burial certificate could be delivered to the family.
Data collection used a specially designed form including:
Mechanism and circumstances of injury
Initial scene GCS, cardiac and respiratory rates, blood pressure, and SpO2
Scene resuscitation summary and clinical evolution
Clinical status upon arrival
Summary of clinically suspected lesions by body area, and suspected dominant lesion (isolated brain injury, multiple trauma, associated spine, chest, or abdominal lesions) at the scene and after hospital admission
This form was completed both online upon arrival by physicians in charge of field resuscitation and by the trauma team leader in charge of in-hospital resuscitation.
CT-scan analysis used a standardized protocol. All radiological lesions were classified by body regions and assigned an AIS-95 score used for calculation of global injury severity score (ISS) [10, 11]. Abdominal lesions were classified according to AAST organ injury scaling (OIS) and brain injury description used Marshall’s classification [12, 13]. Diagnosis of brain death, when applicable, was based upon CT-scan criteria defined by Dupas et al. [14]. AIS ≥ 4 and AIS 3 lesions identified on CT-scan were considered respectively potentially lethal and serious associated lesions.
In an attempt to determine the accuracy of physical and minimal radiological evaluation to predict identified lethal lesions at CT-scan examination, clinically diagnosed lesions and their suspected level of severity (potentially lethal or not) were matched with the CT-scan findings. A complete concordance was considered when both affected body areas and type of lesions potentially causing death were identified before CT-scan examination. A partial concordance was considered when at least one lethal lesion located in the adequate body region, but not all potentially lethal lesions were diagnosed before CT-scan. No correlation was retained when both body area and type of lesions causing death were missed by physical and minimal radiological examinations, or when physical examination data were insufficient.
Statistical analysis first included a descriptive analysis of clinical and CT-scan findings in non-survivors. Results are presented as means for continuous variable and median as appropriate. Fisher’s exact test or Student‘s T test for comparison of means was used as appropriate with a p < .05, considered statistically significant. Positive and negative predictive values for physical and minimal radiological examinations were calculated for each body region with regard to the estimated severity of clinically suspected lesions.
Results
In a total of 556 comatose, younger than 15-year-old patients admitted to our trauma center during the 10-year study period (January 2006 o December 2015), 100 children (18%) died within the first 24 h after hospital admission. Among them, 13 (2%) did not benefit from continuing mechanical ventilation and were therefore considered dead upon arrival, and 10 had incomplete data recording. Finally, 73 children (13% of trauma population), constituting the analyzed non-survival group, died within the first 12 h following admission, and had CT-scan examination within the first 2 h after admission.
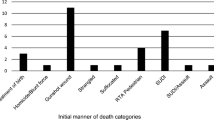
Mean age was 6.2 ± 4.7 years, pre-school children representing 52% of the population (Fig. 1). Among them, 50 were boys (68.5%) and 23 girls (31.5%), giving a male ratio of 3/1. Falls represented 32% of the mechanisms of accidents (70% in less than 6 years old children p < .005) and road traffic accidents 63%, with a predominance of pedestrian/moving vehicle accidents (MVA). This distribution of mechanisms of accidents, ages, and sex ratio were similar to that encountered in our general population [9]. Even though 46/73 children (63%) experienced at least one episode of extreme hypotension with impalpable peripheral pulse, or cardiac arrest in the pre-hospital settings, all of them had a spontaneous cardiac rhythm upon admission. All the children had a critical presentation, with only 25% having measurable arterial blood pressure, and 38% experiencing a recurrent episode of cardiac arrest requiring transient external chest compression in the emergency ward (Table 1). After aggressive initial resuscitation, GCS 3 without sedation was noted in all children, fixed dilated pupils in 65, and severe hemodynamic instability in 50 (Table 1).
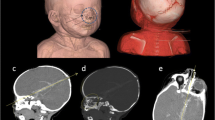
A serious lesion (classified AIS 3 or more after CT-scan) was clinically diagnosed in the pre-hospital settings, or after completion of hospital evaluation in the head (90% / 95%), chest (26% /38%), abdominal (40%/20%), or spinal area (10%/21%). None of these lesions could be considered resulting only from resuscitation maneuvers. It was considered as potentially causing death alone, after complete evaluation in the ward, in 50% for the head, 28% for the chest, 14% for abdominal lesions, and 8% for cervical spine lesions. All children had severe hypotension, hyperglycemia, severe coagulation disorders, acidosis, hypothermia, and hypoxemia upon presentation indicating a high risk of early mortality. CT-scan examination with high-quality IV contrast-enhanced slices could be completed in 58/73 children (80%). In the 15 children without detectable cardiac activity at the moment of IV injection, contrast, although notably diluted and delayed in appearance, could be visualized in abdominal solid organs in all cases. Brain death, diffuse absent cortical-subcortical differentiation, and/or axial hindbrain herniation, with or without identified traumatic brain lesions, was noted on CT-scan in all but one child.
CT-scan examination found a total of 132 potentially lethal injuries resulting in AIS ≥ 4 in at least one body area (Fig. 2) and 87 associated lesions (AIS ≤ 3); the most frequent were abdominal and chest lesions (Fig. 3). Brain injuries (43%) and chest injuries (33%) were the most frequent potentially lethal injuries identified. This tendency was noted in all ages, and in all mechanisms of injuries. Potentially lethal spinal injuries were all localized in the cervical segment and represented 12% of the lethal lesions. A single AIS ≥ 4 injury was found in 27/73 patients (37%) and at least 2 AIS ≥ 4 injuries in 46/73 (63%). In less than 6-year-old children, a unique cause of death, mostly brain injury, was found in 52% of the cases (vs. 20% in older children, p < 0.01). Severe traumatic brain injuries, resulting in head AIS ≥ 3 were found in 68/73 children (93%). Lesions classified as Marshall’s III (diffuse brain injuries without midline shift) represented 50% of these lesions (Fig. 4) and AIS ≥ 4 lesions 80%. Regarding the abdominal lesions, 26/45 were found in solid organs, mainly the liver, and 14 could be considered as potentially lethal (Fig. 5). A chest lesion was found in 70/73 patients (96%) and could be considered as potentially lethal in 21 (28%). ISS could be calculated in 71 patients (2 patients excluded with unclassifiable AIS-9 lesions). Median ISS was 75 (25–75), with 22% of the patients having at least one AIS-6 lesion resulting in ISS 75. Age and accidental mechanisms (motor vehicle accidents vs. falls) did not influence the distribution of ISS.
In 23% of the cases, physical examination data were insufficient to diagnose lethal lesions. A global complete concordance between CT-scan identified lesions, and physical and minimal radiological evaluation, was noted in only 14% of the patients. A partial concordance missing at least one lesion was noted in 47%, and no correlation was noted in 16% of the cases (Fig. 6). Brain lesions were the most frequently clinically diagnosed lesions (90%), causing death, alone or in association with other potentially lethal lesions, in 80% of the cases. The negative predictive value of physical examination for identifying potentially lethal traumatic brain lesions was 92% with a positive predictive value of 83% (Table 2). Chest and abdominal lesions were the most frequently clinically missed lesions with a positive predictive value for physical examination of 65% for chest lesions and only 22% for abdominal lesions. However, a better positive predictive value was found when considering only potentially lethal lesions in both body areas.
All patients of this series were pronounced dead less than 12 h after completion of CT-scan, and the death certificate mentioned a legal obstacle to immediate burial. A post-mortem evaluation was always performed by a registered medical examiner aware of physical and radiological findings recorded in the death certificate and medical files. To our knowledge, after data analysis, and physical examination, by the medical examiner, only three patients could have legal autopsies commanded by a state prosecutor before burial permit could be finally delivered. Autopsy findings were in accordance with CT-scan findings in all these three cases.
Discussion
To our knowledge, this is the first series reporting systematic practice of full-body CT-scan imaging to determine the causes of death in children dying from trauma immediately after their hospital admission. Even though identifying the cause of death could be a major concern for abruptly bereaved parents, the additional burden of post-mortem forensic examinations could be considered an addition to their grief and could be useless in helping them to live with their loss [7]. As previously mentioned, this concern could significantly contribute to the decreasing use, in Europe, of legal autopsies after traumatic death in children [4, 6, 8, 15,16,17]. In many cases, the causes of traumatic death could therefore only be determined with physical and minimal radiological examinations, consistent with the mechanism of accidents. This could, however, not reflect accurately the reality of the facts in most cases and should be considered an inadequate practice. Full-body CT-scan imaging adds mandatory objective arguments and could be considered a minimal prerequisite for medical examiner conclusions, before waiving the need of other examinations. It could also be of benefit to parent awareness of their child’s unavoidable death. In our experience, perimortem CT-scan was always well accepted, and considered, by all parents, as a valuable routine practice for trauma emergency management.
In forensic medicine, radiological explorations have gained an important place and are considered a valuable adjunct to medical autopsies. Among them, full-body CT-scan, called virtual autopsy, or Virtopsy© by their promoters of Bern University [18, 19], has gained an important place in the forensic armamentarium [20]. It provides high-quality images of all body regions, and in the absence of operative or forensic autopsy findings, it is mandatory in order to precisely analyze and classify lesions according to validated severity scales. Despite its important strengths, the practice of post-mortem CT-scan encounters difficulties in promoting its widespread use in forensic medicine departments. The first difficulties are technical constraints with radiation protection, the availability of trained radiological personnel, maintenance requirements, and equipment cost. These constraints result in limited accessibility to CT-scan equipment, on a 24/24 h 7/7 days basis, for many forensic medicine departments. Due to these constraints, most post-mortem CT-examinations are performed several days after death when hypostasis and pathophysiological and anatomical putrefactive changes related to death are in progress. Results should be interpreted cautiously, namely when diagnosing free gas collections [21, 22]. A maximum delay of 56 h post-mortem has been reported to be optimal for chest exploration in the literature [23]. The last, but not the least, it is difficult to perform and interpret a CT-scan in a cadaver with no effective alveolar ventilation and circulation. Because of these limits, namely for the diagnosis of pulmonary and vascular lesions, alternative techniques have been proposed for post-mortem CT-scan. The first one is palliative alveolar ventilation by the means of positive airway pressure application, with the risk of induced barotrauma with pressures over 40 mBar [21, 23, 24]. The second one is high-pressure vascular injection of mixed poly-ethylene-glycol and contrast for visualizing traumatic vascular disruption [25]. Dedicated devices and contrast media have been developed to improve the quality of post-mortem angiography [26]. All these techniques require technical high skills, and short delays in performing post-mortem CT-scan, which could be unavailable in many departments routine practice.
For children with severe multiple trauma, full-body CT-scan examination represents the first-line gold standard examination to identify adequately injuries in all the body area at a time [27]. It is therefore available on a first-priority emergency basis, 24/24 h a day, in every trauma center. However, its use remained restraint in children with no vital signs or severe hemodynamic distress, who could be considered predictable non-survivors within the first hours following hospital admission. Most of them were so pronounced dead upon arrival and disconnected from mechanical ventilation before full-body contrast-enhanced CT-scan could be performed. We thought logical to extend full-body CT examination practice to non-survivors that could represent 13% of the trauma population admitted with vital signs at our institution. Before generalizing the practice, all personnel participating in emergency management of multiple trauma children were previously informed and consulted. Despite the additional burden of performing radiological explorations in near-dying or dead children, everybody agreed to perform these explorations as long as they could be previously informed of the moribund status of the child.
The primary goal of this study was to identify, in children dying within the first few hours following hospital admission, a potentially lethal lesion that could be considered, alone or in association with other lesions, a cause of death (Fig. 7). CT-scan could be considered there a valuable tool since it depicted at least one potential lethal lesion in all children and a total of 132 potentially lethal lesions in 73 patients. Classifying all lesions with previously described scales and grading systems such as AIS, Marshall’s classification, and OIS, allowed us to define precisely these potentially lethal lesions, to calculate ISS, and to eliminate, in these severely injured children, avoidable causes of death. Distribution of age and mechanisms of accidents did not differ from the one reported in pediatric trauma center-based populations [9]. As previously described, severe brain injuries were the first causes of death, whatever age and accident mechanisms. They represent 50% of CT-scan lesions, and 43% of potentially lethal lesions. More surprisingly, a chest lesion was found in 96% of patients and was considered lethal in 33%, preceding abdominal lesions with a global incidence of 62%, but a 42% rate of lethal lesions. The fact that CT-scan could be performed with high-resolution equipment, in children with continuous effective alveolar ventilation, and with IV contrast injection in almost physiological conditions, could explain the very high incidence of chest and abdominal lesions that could be identified by perimortem CT-scan (Figs. 8, 9, and 10). It highlights the advantages of performing CT-scan before or very early after death, eliminating death processes that could artifact post-mortem examinations and technical difficulties for restoring minimal alveolar ventilation and circulation in cadavers [21, 23, 24].
The second goal was to evaluate the accuracy of physical and minimal radiological examination, performed by physicians trained in emergency care management of multiple trauma children, in determining a precise cause of death. This analysis tends to prove that data from clinical and minimal radiological examination alone failed to determine accurately the existing lesions. A complete concordance was found in only 14% of the cases, and partial in 47%, leaving 39% of situations where physical and minimal radiological examination did not match with CT-scan findings. Accuracy of clinical diagnosis for identifying chest and abdominal lesions could be especially questioned, with a sensitivity of clinical examination of respectively 66% and 22%, for all identified lesions, and of 57% and 92% for AIS ≥ 4 lesions. The predominant deleterious role of concomitant chest lesions, encountered in 84% of the children with severe brain injury benefiting from full-body CT-scan evaluation, has been underlined [28, 29], and identifying severe chest lesions is critical. Clinical diagnosis could be especially subtle in children where parietal lesions, namely costal fractures, are rare, even in high-velocity blunt torso impacts. High-resolution CT-scan has also gained a first-line role for the emergency diagnosis of aortic and other major thoracic vascular lesions and is nowadays considered of the gold standard [25, 30]. In our series, chest CT-scan could detect two heart ruptures, and two thoracic aortic disruptions causing death. These lesions were not diagnosed with physical examinations and could clearly be related to reported high-kinetic accidents. CT-scan remains the most useful imaging tool, superior to ultrasonography, with an excellent sensitivity both in alive but comatose and dead subjects, for detecting severe abdominal lesions [31]. Even though missed minor organ injuries have been reported with non-contrast-enhanced post-mortem CT imaging, it could not miss potentially lethal lesions that really matters in determining the cause of death in forensic medicine. These findings could be valuable arguments to recommend further explorations, namely CT-scan and/or legal autopsy, in all children dying from trauma, even when the presumed cause of death, identified in clinical files, matches with the mechanism of accident.
To our knowledge, only 3 out 73 children from these series had legal autopsies with results matching the CT-scan findings. This underlines the very restricted practice of legal autopsies in pediatric deaths in Europe [3, 4, 17, 32]. We therefore postulated that, except in case of unwitnessed accidents and suspected associated assault or violence, a precise description of the mechanism of the accident, and a CT-scan identification of at least one potentially lethal lesion could be considered sufficient, for trained medical examiners, to waive the need for further forensic investigations. This practice could be argued since a full-scale forensic examination could not be limited to identification of the cause of death and should include a precise analysis of the lethal lesions with regard to mechanism of accidents, identification of resulting impacts, soft tissue marks and lesions, and toxicological investigations. Full-body CT-scan should be considered a corner stone of a more complex process, and performing systematically emergency contrast-enhanced CT-scan, before death, in moribund children could add a valuable insight in this process.
Our study has some strengths. CT-scan imaging found at least one potentially lethal lesion in all patients. Perimortem contrast-enhanced CT-scan imaging was always performed on a routine emergency basis, within minutes preceding, or following, death in moribund but ventilated patients. It was included in daily practice for all children with severe trauma referred to our center whatever their clinical status. This clinical practice eliminates therefore the usually encountered difficulties in forensic radiological practice related to availability of equipment and artifacts related to rapidly developing post-mortem processes.
It has also significant limitations. The first one is that the lack of comparison between CT-scan and legal autopsy findings, due to the very low rate of legal autopsies. This precludes the formal conclusion that perimortem CT-scan could be considered a valuable alternative to autopsy. The second one is that a relatively small number of patients have been included in this monocentric observational study, precluding a complete and reliable statistical analysis. We therefore recommend that further multi-center studies could be designed to validate these preliminary findings.
Conclusion
Perimortem CT-scan is a valuable insight into the causes of death in children dying from trauma. It could be performed on a routine emergency basis in most trauma centers provided that all involved personnel could be previously informed of its interest and are aware of the moribund status of the child when performing examination. It provides high-quality imaging of potentially lethal and associated lesions in all areas of the body, without the usual artifacts related to post-mortem processes encountered in delayed post-mortem radiological imaging.
Included in a routine clinical practice, it could limit in bereaved parents the additional burden of heavy procedural constraints related to delayed forensic investigations. Included in the complex process of forensic investigation and provided that this practice could be validated by larger prospective series matching CT-scan imaging and autopsy findings, it could be the most valuable cost and time-effective way of determining early and efficiently the highly probable causes of death.
References
Aouba A, Eb M, Rey G, Pavillon G, Jougla E (2011) Données sur la mortalité en France: principales causes de décès en 2008, et evolution depuis 2000. Bulletin épidémiologique hebdomadaire; 22. Institut National de Veille Sanitaire
Sidebotham P, Fraser J, Covington T, Freemantle J, Petrou S, Pulikottil – Jacob R, Cuttler T, Ellis C (2014) Understanding why children die in high income countries. Lancet 384(9986):915–927
Malicier D (2001) Les indications de l’autopsie médico-légale en France. Bull Acad Natl Med 185(5):839–848
Brinkmann B (1999) Harmonisation of medico-legal autopsy rules. Int J Legal Med 113:1–14
Le Blanc-Louvry I, Thureau S, Duval C, Papin-Lefebvre F, Thiebot J, Dacher J, Gricourt C, Touré E, Proust B (2013) Post-mortem computed tomography compared to forensic autopsy findings : a French experience. Eur Radiol 23:1829–1835
McDermott M (2003) Obtaining consent for autopsy. Br Med J 327:804–806
Sullivan J, Monagle P (2011) Bereaved parent’s perceptions of the autopsy examination of their child. Pediatrics 127:1013
Bolliger S, Thali M, Ross S, Buck U, Naether S, Vock P (2008) Virtual autopsy using imaging : bridging radiologic and forensic sciences. A review of the Virtopsy and similar projects. Eur Radiol 18:273–282
Ducrocq S, Meyer P, Orliaguet G, Blanot S, Laurent-Vannier A, Renier D, Carli P (2006) Epidemiology and early predictive factors of mortality and outcome in children with traumatic severe brain injury: experience of a French pediatric trauma center. Pediatr Crit Care Med 7:461–467
Baker S, O'Neill B, Haddon W Jr, Long W (1974) The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 14:187–196
Champion H, Sacco W, Copes W, Gann D, Gennarelli TA, Flanagan M (1989) A revision of the trauma score. J Trauma 29:623–629
Moore E, Shackford S, Pachter H, McAninch J, Browner B, Champion HR, Flint L, Gennarelli T, Malangoni M, Ramenofsky M et al (1989) Organ injury scaling: spleen, liver and kidney. J Trauma 29:1664–1666
Marshall L, Bowers Marshall S, Klauber M, van Berkum Clark M, Eisenberg H, Jane J, Luerssen T, Marmarou A, Foulkes M (1991) A new classification of head injury based on computerized tomography. J Neuro-Oncol 75:S14–S20
Dupas B et al (2009) Diagnosis of brain death using two-phase spiral CT. Am J Neuroradiol 30:1566–1570
Pasquier B (2005) L’autopsie scientifique en 2005: luxe ou nécessité ? Rev Med Interne 26:611–614
Chatelain D, Sevestre H (2008) Requiem pour l’autopsie. Rev Med Interne 29:77–79
Gosselin B, Gaillard D, Rambaud C (1999) Les autopsies à l’aube de l’an 2000. Ann Pathol 19:S56–S63
Dirnhofer R, Jackowski C, Vock P, Potter K, Thali M (2006) VIRTOPSY : minimally invasive imaging-guided virtual autopsy. RadioGraphics 26:1305–1333
Thali M, Jackowski C, Oesterhelweg RS, Dirnhofer R (2007) VIRTOPSY- the Swiss virtual autopsy approach. Legal Med 9:100–104
O’Donnell C, Woodford N (2008) Post-mortem radiology – a new sub-specialty ? Clin Radiol 63:1189–1194
Christe A, Flach P, Ross S, Spendlove D, Bolliger S, Vock P, Thali M (2010) Clinical radiology and postmortem imaging (Virtopsy) are not the same : specific and unspecific postmortem signs. Legal Med 12:215–222
Gebhart F, Brogdon B, Zech W, Thali M, Germerott T (2012) Gas at postmortem computed tomography – an evaluation of 73 non-putrefied trauma and non trauma cases. Forensic Sci Int 222:162–169
Germerott T, Flach P, Preiss U, Ross S, Thali M (2012) Postmortem ventilation : a new method for improved detection of pulmonary pathologies in forensic imaging. Legal Med 14:223–228
Germerott T, Preiss U, Ebert L, Ruder T, Ross S, Flach P, Ampanozi G, Filograna L, Thali M (2010) A new approach in virtopsy : postmortem ventilation in multi-slice computed tomography. Legal Med 12:276–279
Grabherr S, Doenz F, Steger B, Dirnhofer R, Domínguez A, Sollberger B, Gygax E, Rizzo E, Chevalier C, Meuli R, Mangin P (2011) Multi-phase post mortem CT angiography: development of a standarized protocol. Int J Legal Med 125:791–802
Grabherr S, Grimm J, Domínguez A, Vanhaebost J, Mangin P (2014) Advances in post-mortem CT- angiography. Br J Radiol 87:20130488
Orliaguet G, Meyer P, Baugnon T (2008) Management of critically ill children with traumatic brain injury. Paediatr Anaesth 1:455–461
Orliaguet G, Rakotoniaina S, Meyer P, Blanot S, Carli P (2000) Effect of a lung contusion on the prognosis of severe head injury in the child. Ann Fr Anesth Reanim 19:164–170
Stewart TC, Alharfi IM, Fraser DD (2013) The role of serious concomitant injuries in the treatment and outcome of paediatric severe traumatic TBI. J Trauma Acute Care Surg 75:836–842
Ruder T, Hatch G, Thali M, Fischer N (2011) One small scan for radiology, one giant leap for forensic medicine – post-mortem imaging replaces forensic autopsy in a case of traumatic aortic laceration. Legal Med 13:41–43
De la Morandière K (2015) Towards evidence-based emergency medicine: best BETs from the Manchester royal infirmary. BET: is CT thorax necessary to exclude significant injury in paediatric patients with blunt chest trauma? Emerg Med J 32:660–662
Chariot P, Witt K, Pautot V, Porcher R, Thomas G, Zafrani E, Lemaire F (2000) Declining autopsy rate in a french hospital. Physician’s attitudes to the autopsy and use of autopsy material in research publications. Arch Pathol Lab Med 124:739–745
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Antúnez, S., Grevent, D., Boddaert, N. et al. “Perimortem” total body CT-scan examination in severely injured children: an informative insight into the causes of death. Int J Legal Med 134, 625–635 (2020). https://doi.org/10.1007/s00414-019-02058-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-019-02058-5