Abstract
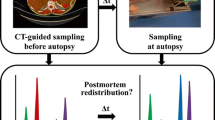
Interpretation of postmortem morphine concentrations in forensic toxicology provides several pitfalls such as missing information on tolerance, analyte stability, or postmortem redistribution (PMR). Recently, it had been shown that computed tomography (CT)-guided collection of biopsies using a robotic arm (virtobot) provides a valuable strategy for systematic studies on time-dependent PMR. Using this technique, time-dependent PMR of morphine and its metabolites was investigated in 12 cases. At admission to the institute (t1), femoral and heart blood (right ventricle) as well as biopsies from the right lung, the right kidney, liver, spleen, and muscle tissue were collected. At autopsy approximately 24 h later (t2), samples from the same body regions were collected again. Additionally, gastric contents, urine, brain tissue, and heart blood from the left ventricle was collected. Morphine, normorphine, hydromorphone, morphine-3-glucuronide, morphine-6-glucuronide, and morphine-sulfate were quantified with LC-MS/MS. In femoral blood, significant increase of morphine concentrations was observed, although ultimately not relevant for forensic interpretation. In the alternative matrices, increases as well as decreases were observed without a clear trend. The morphine metabolites did not exhibit relevant concentration changes. Investigation of underlying redistribution mechanisms indicated that concentration change (i.e., increase) of morphine in femoral blood rather resulted from diffusion processes than from release of morphine from its conjugates. Concentration changes in heart blood might have been caused by redistribution from lung tissue or gastric content. This study also proved that CT-guided collection of biopsies using a virtobot arm is an invaluable tool for future studies on PMR redistribution of other substance groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Interpretation of postmortem morphine concentrations in forensic toxicology provides several pitfalls. Besides antemortem factors such as missing information on opiate tolerance or duration of an agonal phase, postmortem factors such as analyte stability or postmortem redistribution (PMR) have to be considered. If available, hair analysis may be useful to gather information on drug history. PMR of morphine might be caused by diffusion processes along concentration gradients, instability, or bacterial conversion of morphine-conjugates to morphine [1, 2]. To date, several in vitro experiments on analyte stability and vascular permeation of morphine were performed to clarify its redistribution mechanisms [1, 3–5]. Unfortunately, only few studies on analyte stability were performed in postmortem specimen. Moriya et al. found morphine and its conjugates to be stable in postmortem blood at 37 °C for 10 days [1], whereas Carrol et al. found conversion of morphine-3-glucuronide (M3G) to morphine at 37 °C in postmortem blood within 2 weeks [3]. However, a temperature of 37 °C might not reflect environmental temperature for most cases in the postmortem interval. Skopp et al. showed that morphine concentrations in postmortem blood increased within 124 days at 20 °C, and the morphine-glucuronide concentrations decreased correspondingly [6]. In addition, the morphine glucuronide stability seemed to be dependent on environmental temperature and the degradation was accelerated by light exposure. Considering the described studies, morphine conjugate stability might differ from case to case as contributing factors such as microbiological load, environmental temperature, or light exposure may differ interindividually. Vascular permeation of morphine and its glucuronides was shown to start after a lag time and to be dependent on the disintegration of the vascular wall, the temperature, and the concentration gradient [5]. Consequently, analyte instability as well as diffusion processes might be involved in postmortem morphine concentration changes. In vivo investigation of time-dependent PMR of morphine and its metabolites was performed on animal models and in human case studies. Studies in rat, rabbit, and pig model revealed relevant concentration increases of free morphine in blood and other matrices within minutes to days after death [7–10]. In contrast, time-dependent PMR studies on human cases indicate that morphine and its metabolites do not undergo significant postmortem concentration changes in peripheral blood [11–14]. However, the investigated time intervals mostly did not include the first few hours after death, where high concentration changes are believed to occur. Tolliver et al. compared antemortem to postmortem morphine concentrations and found increased postmortem concentrations in five of seven cases mostly in central blood specimen [15]. In conclusion, it remains unclear whether postmortem morphine blood concentrations can be assumed to represent antemortem concentrations, especially as concentration changes within the first minutes and hours after death were not investigated in human cases so far. Next, to the lack of information on PMR in the postmortem interval (PMI) few hours after death, concentration changes in alternative matrices such as organs and tissues have not been investigated in humans to date. In rabbit liver, lung, or kidney tissue, postmortem increases as well as decreases were observed for morphine and M3G [10]. The aim of our study was to further clarify time-dependent PMR and its mechanisms of morphine including its metabolites not only in blood but also in alternative matrices such as the muscle, liver, kidney, lung, spleen, and adipose tissue in humans. Especially, the application of CT-guided biopsy sampling hours before conventional autopsy should provide valuable information on drug concentration changes in alternative matrices [16].
Materials and methods
Chemicals and reagents
Methanolic solutions of morphine, M3G, morphine-6-glucuronide (M6G), normorphine, hydromorphone, and 6-monoacetylmorphine (MAM) (1 mg/mL) and the deuterated internal standards (IS) morphine-d3, M3G-d3, M6G-d3, and MAM-d3 (0.1 mg/mL) were obtained from Cerilliant (delivered by Sigma-Aldrich, Buchs, Switzerland). Water was purified with a Purelab Ultra millipore filtration unit (Labtech, Villmergen, Switzerland), and acetonitrile of HPLC grade was obtained from Fluka (Buchs, Switzerland). All other chemicals used were from Merck (Zug, Switzerland) and of the highest grade available.
Postmortem samples
Blood and alternative matrices were collected at two time points t1 and t2 after death within the routine toxicological investigation according to Staeheli et al. [16]. After the routine postmortem CT imaging procedure (t1) on a 128-slice scanner (Somatom Definition Flash, Siemens Medical Solutions, Forchheim, Germany), introducer needles were placed into the right heart ventricle, the right lung, the right lobe of the liver, the right kidney, the spleen, subcutaneous adipose tissue of the waist, muscle tissue at the upper left thigh, and the right femoral vein using the virtobot system [16, 17]. After placement of the introducer needles, another CT scan was performed to verify needle positions. From the right heart ventricle and the femoral vein, 1 mL blood was collected each. Biopsies were collected in triplicate from all mentioned matrices. Directly after sample collection, the biopsies were weighed into 2-mL Metal Bead Lysing Matrix tubes (MP Biomedicals, Illkirch, France). The body fluids were aliquoted into 2-mL Eppendorf Safe Lock Tubes (Schoenenbuch, Switzerland) in triplicate of 20 μL for morphine quantitation and into duplicates of 100 μL for morphine metabolite quantitation. The following day at autopsy (t2), samples from the same locations were collected where biopsies had been taken at t1. Additionally, heart blood from the left ventricle, urine, gastric content, and cerebellum were collected. After autopsy, the solid matrices were aliquoted into triplicate of approx. 20 mg and body fluids into triplicate of 20 μL for morphine quantitation. The blood samples additionally were aliquoted into duplicate of 100 μL for morphine metabolite quantitation. All samples were stored at −20 °C until analysis.
Quantitation of morphine
All samples belonging to the same case were extracted and analyzed on the same day. Sample preparation and analysis of morphine was performed according to Staeheli et al. [18]. Briefly, tissue samples were homogenized and two liquid-liquid extractions (LLE) with butyl acetate/ethyl acetate (1:1, v/v) were performed, one at pH 7.4 and one at pH 13.5. The extracts were combined and analyzed by an LC-MS/MS method, which was previously validated in postmortem femoral blood (pB), heart blood (HB), muscle, liver, kidney, spleen, lung, brain, and adipose tissue [18].
Quantitation of morphine metabolites
The morphine metabolites M3G, M6G, normorphine (NM), hydromorphone (HM), morphine-3-sulfate (M3S), and morphine-6-sulfate (M6S) were quantified in pB and HB samples. Blood samples were extracted by solid-phase extraction (SPE) adapted from [19]. Briefly, 100 μL blood were fortified with an IS mixture containing morphine-d3 75 ng/mL, MAM-d3 50 ng/mL, M3G-d3 400 ng/mL, and M6G-d3 500 ng/mL and diluted with 1 mL 0.5 M carbonate buffer pH 9.3. The sample was loaded onto a preconditioned (2 mL methanol, 2 mL H2O, 1 mL 5 mM carbonate buffer pH 9.3) BakerBond C18 200 mg 3 mL SPE column (Avantor Performance Materials, Deventer, Netherlands). The column was washed with 1 mL 5 mM carbonate buffer pH 9.3, dried for 1 min under vacuum, and elution was performed with 1.5 mL MeOH. The eluate was evaporated to dryness under a gentle stream of nitrogen at 40 °C and reconstituted in 50 μL of a mixture of eluents A and B (5:95 v/v). The analysis was performed using the same LC-MS/MS instrument mentioned in the previous chapter. The LC settings were as follows: Merck (Darmstadt, Germany) SeQuant® ZIC®-HILIC column (150 × 2.1 mm, 3.5 μm), gradient elution with eluents A and B, start conditions 95 % B for 0.5 min with a flow rate of 0.5 mL/min, 1–7 min concave downward to 10 % B, hold at 10 % B for 0.5 min and reequilibrating to 95 % B for 1.5 min. Injection volume was 10 μL. The MS was operated in the MRM mode using three transitions for each analyte. MRM 3 corresponded to the 13C isotope of MRM 1 to extend the dynamic range of the method in case of high concentrations [18]. The MS settings for each analyte are given in Table 1. Calibrator and quality control (QC) samples were prepared using blank postmortem pB samples spiked with 20 μL calibration spiking solution and 25 μL IS spiking mix. Calibration range was 4–4000 ng/mL for M3G, 10–1600 ng/mL for M6G, 1–300 for NM, and 0.5–300 for HM. QC concentration was defined 20 % above lowest calibrator for QC low, 20 % below highest calibrator for QC high, and 80 % below highest calibrator for QC med. The regressions were calculated using a simple linear model with 1/X weighting. All metabolites were quantified using MRM 1. Morphine-sulfate identity was confirmed with a high-resolution mass spectrum using the described chromatographic method and a Sciex 6600 QTOF system. Additionally, reversed-phase chromatography was performed and elution order of M3S resp. M6S was compared to Andersson et al. [20].
Data analysis
PMR of morphine and its metabolites
Distribution of morphine at t1 was evaluated as concentration ratio of each matrix to pB. Percent concentration differences between t1 and t2 were calculated for morphine, M3G, M6G, M3S, and NM defining mean concentration at t1 as 100 %. For statistical evaluation, a nonparametric Wilcoxon matched-pairs signed ranks test (p < 0.05) was applied between t1 and t2 using GraphPad Prism 6.0 (GraphPad Software, La Jolla, CA, USA).
PMR mechanisms: diffusion processes
The percentage concentration change per hour relative to the concentration at t1 (mc) was calculated for pB, HB, and spleen according to
ct1 = mean morphine concentration at t1 [ng/mL]; ct2 = mean morphine concentration at t2 [ng/mL]; dt = time interval between t1 and t2 [h].
The lung-to-HB (right ventricle) concentration ratio at t1 as well as the gastric content-to-HB (right ventricle) concentration ratio at t2 were compared with the percentage concentration change in HB (right ventricle) (mc HB). Additionally, the lung-to-HB (right ventricle) concentration ratio at t1 was compared with the concentration ratio between HB from the left ventricle and HB from the right ventricle at t2. The muscle-to-pB as well as the HB-to-pB concentration ratio (i.e., central to peripheral ratio; C/P-ratio) at t1 was compared to the percentage concentration change in pB (mc pB). The concentration ratio between stomach content (t2) and spleen (t1) was compared to the percentage concentration change in spleen (mc spleen). Nonparametric Spearman correlation coefficients were calculated using GraphPad Prism 6.
PMR mechanisms: conjugate stability
The molar concentration change of M3G was compared to the molar concentration change of morphine in pB and HB. The percentage change of the area ratio of M3S was compared with the percentage concentration change of morphine in pB and HB. Nonparametric Spearman correlation coefficients were calculated using GraphPad Prism 6.
Results and discussion
Time-dependent PMR and distribution of morphine and its metabolites was investigated in blood and alternative matrices of 12 cases within a PMI of 6 to 88 h (Table 2). CT-guided biopsy sampling was applied before actual autopsy to provide two time points for investigation of PMR. PMI until first sampling time point ranged from 6 to 63 h and the time interval between first and second sampling ranged from 18 to 29 h. In seven cases, morphine resulted from a heroin application and in the other cases most probably from a morphine intake or application. In most cases, cause of death was of toxicological nature, except for case 6 who died of an acute cardiac infarction.
Concentrations and redistribution of morphine
Morphine concentrations in all matrices are displayed as concentration ratio to pB, where concentrations ranged from not detectable to 2500 ng/mL (Fig. 1). In case 6, morphine was below LOQ in all samples except for muscle, liver, and lung at t1. Distribution of morphine was rather inhomogeneous with highest concentrations in the lung, liver, kidney, and gastric content. These findings are in line with previous publications [21, 22]. In muscle tissue, concentrations were 1.2 to 3.9 times higher compared to pB and thus closest to pB within the alternative matrices. Due to the relatively narrow range of morphine concentration ratio to pB, muscle from the upper thigh might therefore be a recommendable alternative to pB in cases where pB is not available.
Distribution of morphine displayed as concentration ratio to femoral blood, each dot representing one case and the line representing the median ratio. In cases where concentration at t1 was not available, concentration at t2 was displayed. The dotted line indicates equal concentration to femoral blood
Time-dependent redistribution of morphine was investigated comparing concentration at t1 with t2 (Fig. 2). In pB, a morphine concentration increase was observed in all cases (range 0.4–240 %, mean 65 %, median 44 %). Morphine concentration change in pB was significant (p < 0.05) in contrast to previous studies [11–14]. However, in none of the cases, the toxicological interpretation had to be altered regarding morphine concentration at t1. Therefore, the concentration increases were considered as not relevant for case interpretation. In general, statistical significance of the observed concentration changes should be interpreted with caution, as interindividual differences in postmortem cases are usually great.
PMR of morphine in femoral blood, heart blood (right ventricle), muscle, liver, lung, and spleen displayed as concentration vs. the postmortem interval (PMI). Each dot represents one sample of the triplicate measurements. The mean concentration at the sampling time points t1 and t2 were connected with a line in each case
In all other matrices, concentration increases as well as decreases were observed with ranges of −5 to 680 % (median 37 %) in HB, −100 to 160 % (median −3.1 %) in liver, −59 to 170 % (median −20 %) in kidney, −100 to 26 % (median −24 %) in muscle, −10 to 155 % (median 9.5 %) in spleen, and −100 to 300 % (median −8.6 %) in lung tissue (Fig. 2). In adipose tissue, concentration ranges of t1 and t2 were overlapping in the majority of the cases, and therefore, changes in concentration could not be assumed. PMR in kidney was not displayed as concentrations within the time points varied widely. Further experiments showed that drug concentrations in the kidney medulla and cortex differed (data not shown). As it was not possible to distinguish between cortex and medulla during sampling, this might have been the reason for the variations. In case 1, highest concentration changes were observed in the majority of matrices compared to the other cases. As case 1 reported the shortest PMI compared to the other cases, this study might support the theory of PMR mainly occurring in the first few hours after death. However, Hargrove et al. who reported even shorter intervals before first sampling did not observe significant concentration changes [11].
Concentrations and redistribution of morphine metabolites
The morphine metabolites were quantitated with a separate LC-MS/MS method because the recovery of the morphine-conjugates was insufficient with the LLE used for the quantitation of morphine in all matrices. Chromatography of the LC-MS/MS method for the morphine metabolites is displayed in Fig. 3. Although quantitation of MAM was not aimed for, it was included into the method to prove chromatographic separation. As the morphine-sulfate metabolites were not commercially available, identity was confirmed by high-resolution mass spectrum and comparison of the M3S and M6S elution order in authentic cases with published work from Andersson et al. [20].The high-resolution mass spectrum of M3S ([M + H] 366.1013 Da, mass error 1.9 ppm) included the [M + H] fragments 286.1459, 268.1332, 201.0915, 185.0594, and 165.0717 Da, thus proving morphine-sulfate identity. M3S was shown to occur in higher concentrations than M6S, leading to the assumption that the first eluting peak represents M3S [20]. Additional experiments with reversed-phased chromatography showed that M3S and M6S eluted in the same order as in the HILIC chromatography. Comparison of the morphine-sulfates elution order with published work from Andersson et al. further confirmed assignment of M3S and M6S [20]. However, as M6S was not detectable in many cases and signal to noise ratios were generally low, only results for M3S are discussed. As also HM concentrations were below LOD in most cases, they were not discussed either. As primarily concentration changes and therefore relative concentrations were of importance for the presented work, metabolite quantitation without full method validation was considered acceptable. Additionally, the use of deuterated internal standards and the comparison of concentration in matrices from the same individuals should further reduce a possible lack of precision or accuracy.
LC-MS/MS chromatogram of the morphine metabolites quantitation method including 6-monoacetylmorphine (MAM, 328 → 165), hydromorphone (HM, 286 → 185), morphine, morphine-3-sulfate (M3S, 366 → 286), normorphine (NM, 272 → 152), morphine-6-sulfate (M6S, 366 → 286), morphine-6-glucuronide (M6G, 462 → 286), and morphine-3-glucuronide (M3G, 462 → 286). Quantitation of morphine was performed according to Staeheli et al. [18]
Morphine metabolite percentage concentration changes in pB were minor in most cases. However, concentration increases as well as decreases were observed (Fig. 4). Concentration changes ranged from −66 to 49 % (median −12 %) for M3G, −15 to 86 % (median 5.3 %) for M6G, −12 to 280 % (median 3.1 %) for NM and −43 to 180 % (median 4.3 %) for M3S in pB. In HB, concentration changes of the metabolites were greater compared to those in pB (Fig. 4). Median changes were 15 % for M3G, −1.2 % for M6G, 1.2 % for NM, and 70 % for M3S. Especially for the morphine conjugates, no significant decrease could be observed. This leads to the conclusion that conjugate instability was not a major problem in the selected cases. However, storage of the bodies at 5 °C between the sampling time points did not reflect natural environment and might have supported analyte stability.
PMR of a morphine-3-glucuronide (M3G), b morphine-6-glucuronie (M6G), and c) normorphine (NM) in femoral and heart blood (right ventricle) displayed as concentration vs. the postmortem interval (PMI). Each dot represents one sample of the triplicate measurements. The mean concentration at the sampling time points t1 and t2 were connected with a line in each case
Redistribution mechanisms
As significant morphine concentration changes were observed in this study, possible redistribution mechanisms were evaluated, especially diffusion processes and release from conjugate metabolites. Diffusion processes were already shown to contribute to postmortem concentration changes for other drugs [23]. Therefore, morphine concentration changes were correlated to concentration ratios to adjacent tissues. In addition, the role of the C/P-ratio as a marker for PMR was evaluated. To compensate for interindividual differences in PMI, the concentration change was divided by the PMI, although linearity of concentration changes could not be assumed.
High C/P ratios were stated to be a marker for PMR processes [24]. However, Spearman correlation of the C/P-ratio of morphine to concentration change in pB (mc pB) was only weak (Fig. 5a). Therefore, a high C/P ratio might not be a valuable indicator for postmortem concentration changes in case of morphine. Concentration increases in pB might have been caused by diffusion from adjacent muscle tissue, as a concentration gradient was observed in all cases (Fig. 1). Therefore, the concentration ratio of morphine in muscle from the upper thigh to pB was compared to mc pB and a moderate positive correlation was observed (Fig. 5b). Skopp et al. showed that vascular permeation can occur for morphine and its metabolites [5]. Although permeation was found to be mainly dependent on the disintegration of the vascular wall and the PMI, it was stated that permeation might even occur at early postmortem stages. Consequently, morphine diffusion from muscle to pB seems to be likely, especially in cases with high concentration ratios between muscle and pB. However, diffusion along the blood vessels cannot be excluded as concentrations distal or proximal to the sampling point were not investigated.
Evaluation of redistribution mechanisms of morphine in femoral blood (pB), displayed as the muscle-to-pB concentration ratio (a) and the C/P-ratio (b) compared to the morphine concentration increase in pB (mc pB). Evaluation of redistribution mechanisms in heart blood (HB) displayed as the lung-to-HB concentration ratio (c) as well as the gastric content-to-HB ratio (d) compared to the morphine concentration increase in HB (mc HB). Additionally, the lung-to-HB concentration ratio was compared to the HB concentration ratio between left and right ventricle (e). Gastric content-to-spleen concentration ratio was compared to the concentration increase in spleen (mc spleen) (f). Spearman correlation coefficient r is shown (r* with exclusion of cases exceeding the calibration range)
In cases where no pB and appropriate alternatives are available, HB is sometimes used for drug quantitation. However, interpretation of concentrations in HB provides several pitfalls. Concentrations are often higher compared to pB, and several redistribution mechanisms are discussed, such as diffusion from gastric content, heart muscle or lung tissue [2]. Although concentration changes generally were not statistically significant in HB in our study, individual cases exhibited relatively great concentration changes. Therefore, concentration changes in HB (mc HB) were compared to the concentration ratios between lung and HB (Fig. 5c) and to the ratio between gastric content and HB (Fig. 5d). Morphine concentration in HB of case 1 and in gastric content of cases 7 and 9 exceeded the calibration range at t2. Therefore, Spearman coefficient r* was calculated with exclusion of these cases. Weak to moderate positive correlation was found in both comparisons; thus, redistribution from gastric content and lung to HB appears to be possible. Furthermore, correlation of ratio between lung and HB was compared to the concentration ratio between HB from the left and the right ventricle (Fig. 5e). It showed moderate to strong positive correlation. These findings strongly support the theory of redistribution from the lung to the left heart via the pulmonary veins. Unfortunately, concentrations in heart muscle were not determined, and therefore, redistribution from heart muscle cannot be excluded.
Postmortem morphine concentration changes in spleen might not be relevant in the majority of the forensic cases. Nevertheless, diffusion processes from gastric content was investigated as the spatial proximity to spleen let it seem plausible (Fig. 5f). The observed moderate to strong positive correlation supported this theory.
Besides diffusion processes, conjugate instability is discussed as cause for potential postmortem concentration changes, as morphine is released from its conjugates. Therefore, M3G and M3S concentration changes were correlated with the morphine concentration change in pB and HB (Fig. 6). In case of morphine conjugate instability, negative correlation between concentration change of the conjugates and morphine would be expected. In our study, no correlation was observed in pB and even strong positive correlation in HB. Consequently, it can be stated that conjugate instability did not lead to morphine increase in pB or HB. Moreover, M3G and M3S in HB rather seemed to be redistributed with comparable mechanisms like morphine itself. Carrupt et al. showed that the morphine glucuronides are only slightly less lipophilic compared to morphine, which might be a factor contributing to the similar postmortem behavior of M3G and morphine [25].
Evaluation of redistribution of morphine in femoral (pB) and heart blood (HB) due to conjugate instability: molar concentration change of morphine compared to molar concentration change of M3G in pB (a) and HB (c) and percentage concentration change of morphine compared to the percentage concentration change of morphine-sulfate in pB (b) and HB (d). Spearman correlation coefficient r is shown (r* with exclusion of cases exceeding the calibration range)
Conclusions
Significant morphine concentration increase was observed in pB; however, the concentration changes were not relevant regarding interpretation of the forensic cases. In the alternative matrices, increases as well as decreases were observed without a clear trend. Metabolites did not undergo extensive PMR. Especially, the conjugates were shown to be rather stable, thus not contributing to morphine concentration increase in pB. The latter might rather have been caused by diffusion processes from, e.g., surrounding muscle tissue. Investigation of HB and lung resp. gastric content supported the theory of redistribution along pulmonary veins to the left heart ventricle or from stomach to the heart. Moreover, CT-guided biopsy sampling proved to be a valuable tool for investigation of PMR mechanisms.
References
Moriya F, Hashimoto Y (1997) Distribution of free and conjugated morphine in body fluids and tissues in a fatal heroin overdose: is conjugated morphine stable in postmortem specimens? J Forensic Sci 42(4):736–740
Pelissier-Alicot AL, Gaulier JM, Champsaur P, Marquet P (2003) Mechanisms underlying postmortem redistribution of drugs: a review. J Anal Toxicol 27(8):533–544
Carroll FT, Marraccini JV, Lewis S, Wright W (2000) Morphine-3-D glucuronide stability in postmortem specimens exposed to bacterial enzymatic hydrolysis. Am J Forensic Med Pathol 21(4):323–329
Skopp G, Potsch L, Klingmann A, Mattern R (2001) Stability of morphine, morphine-3-glucuronide, and morphine-6-glucuronide in fresh blood and plasma and postmortem blood samples. J Anal Toxicol 25(1):2–7
Skopp G, Lutz R, Potsch L, Ganssmann B, Klinder K, Schmidt A, Aderjan R, Mattern R (1997) An in vitro experiment for postmortem vascular permeation. The passage of morphine and morphine glucuronides across a vascular wall. J Forensic Sci 42(3):486–491
Skopp G, Lutz R, Ganssmann B, Mattern R, Aderjan R (1996) Postmortem distribution pattern of morphine and morphine glucuronides in heroin overdose. Int J Legal Med 109(3):118–124
Sawyer WR, Forney RB (1988) Postmortem disposition of morphine in rats. Forensic Sci Int 38(3–4):259–273
Koren G, Klein J (1992) Postmortem redistribution of morphine in rats. Ther Drug Monit 14(6):461–463
Crandall CS, Kerrigan S, Aguero RL, Lavalley J, McKinney PE (2006) The influence of collection site and methods on postmortem morphine concentrations in a porcine model. J Anal Toxicol 30(9):651–658
Maskell PD, Albeishy M, De Paoli G, Wilson NE, Seetohul LN (2015) Postmortem redistribution of the heroin metabolites morphine and morphine-3-glucuronide in rabbits over 24 h. Int J Legal Med 130(2):519–531
Hargrove VM, Molina DK (2014) Peripheral postmortem redistribution of morphine. Am J Forensic Med Pathol 35(2):106–108
Gerostamoulos J, Drummer OH (2000) Postmortem redistribution of morphine and its metabolites. J Forensic Sci 45(4):843–845
Gerostamoulos D, Beyer J, Staikos V, Tayler P, Woodford N, Drummer OH (2012) The effect of the postmortem interval on the redistribution of drugs: a comparison of mortuary admission and autopsy blood specimens. Forensic Sci Med Pathol 8(4):373–379
Logan BK, Smirnow D (1996) Postmortem distribution and redistribution of morphine in man. J Forensic Sci 41(2):221–229
Tolliver SS, Hearn WL, Furton KG (2010) Evaluating the relationship between postmortem and antemortem morphine and codeine concentrations in whole blood. J Anal Toxicol 34(8):491–497
Staeheli SN, Gascho D, Fornaro J, Laberke P, Ebert LC, Martinez RM, Thali MJ, Kraemer T, Steuer AE (2016) Development of CT-guided biopsy sampling for time-dependent postmortem redistribution investigations in blood and alternative matrices-proof of concept and application on two cases. Anal Bioanal Chem 408(4):1249–1258
Ebert LC, Ptacek W, Breitbeck R, Furst M, Kronreif G, Martinez RM, Thali M, Flach PM (2014) Virtobot 2.0: the future of automated surface documentation and CT-guided needle placement in forensic medicine. Forensic Sci Med Pathol 10(2):179–186
Staeheli SN, Poetzsch M, Kraemer T, Steuer AE (2015) Development and validation of a dynamic range-extended LC-MS/MS multi-analyte method for 11 different postmortem matrices for redistribution studies applying solvent calibration and additional (13)C isotope monitoring. Anal Bioanal Chem 407(29):8681–8712
Taylor K, Elliott S (2009) A validated hybrid quadrupole linear ion-trap LC-MS method for the analysis of morphine and morphine glucuronides applied to opiate deaths. Forensic Sci Int 187(1–3):34–41
Andersson M, Bjorkhem-Bergman L, Ekstrom L, Bergqvist L, Lagercrantz H, Rane A, Beck O (2014) Detection of morphine-3-sulfate and morphine-6-sulfate in human urine and plasma, and formation in liver cytosol. Pharmacol Res Perspect 2(6):e00071
Wyman J, Bultman S (2004) Postmortem distribution of heroin metabolites in femoral blood, liver, cerebrospinal fluid, and vitreous humor. J Anal Toxicol 28(4):260–263
Baselt RC (2008) Disposition of toxic drugs and chemicals in man, 8th edn. Chemical Toxicology Institute, Foster City
Pounder DJ, Smith DR (1995) Postmortem diffusion of alcohol from the stomach. Am J Forensic Med Pathol 16(2):89–96
Han E, Kim E, Hong H, Jeong S, Kim J, In S, Chung H, Lee S (2012) Evaluation of postmortem redistribution phenomena for commonly encountered drugs. Forensic Sci Int 219(1–3):265–271
Carrupt PA, Testa B, Bechalany A, el Tayar N, Descas P, Perrissoud D (1991) Morphine 6-glucuronide and morphine 3-glucuronide as molecular chameleons with unexpected lipophilicity. J Med Chem 34(4):1272–1275
Acknowledgments
This work was supported by the Swiss National Science Foundation (grant no. 310030_165875). The authors would like to thank the group from the Department of Forensic Medicine and Imaging, ZIFM, for their assistance and Prof. B. Seifert and the scientists from the Department of Forensic Pharmacology and Toxicology, ZIFM, for helpful discussions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Declaration of no objection for ethical approval was obtained by the cantonal ethics committee of Zurich, Switzerland (number 42.2005).
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Staeheli, S.N., Gascho, D., Ebert, L.C. et al. Time-dependent postmortem redistribution of morphine and its metabolites in blood and alternative matrices—application of CT-guided biopsy sampling. Int J Legal Med 131, 379–389 (2017). https://doi.org/10.1007/s00414-016-1485-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-016-1485-2