Abstract
The aim of this study was to measure catecholamines and their O-methylated metabolites in urine and vitreous humor collected in cardiac deaths and noncardiac control cases that underwent medicolegal investigations. Our first goal was to assess whether cardiac events of different types are characterized by different catecholamine/metanephrine urine and/or vitreous profiles. Our second goal was to determine whether noncardiac causes of death with different survival intervals are characterized by different catecholamine/metanephrine urine and/or vitreous profiles. Two study groups were prospectively and retrospectively formed, a cardiac death group (including three subgroups, according to the cause of death) and a noncardiac death group (including two subgroups, according to the length of the agonal period). Postmortem angiography, autopsy, histology, toxicology, and biochemistry were performed in all cases. First results seem to indicate that absolute values measured in urine and vitreous for each of the analyzed markers display no significant differences relating to each of the tested cardiac death subgroups. In the control group, absolute concentrations measured in urine and vitreous for each of the analyzed parameters failed to show significant differences relating to the length of agonal period. Our preliminary findings do not seem to confirm the conclusions of former studies and fail to corroborate the usefulness of urine catecholamine and metanephrine analysis to characterize stress response intensity or length of the dying process in the postmortem setting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Reactions to stressful situations such as trauma, surgery, various medical conditions, and cold/heat exposure are characterized by enhanced secretion of a number of hormones, including glucocorticoids and catecholamines. Activation of the pituitary-adrenal axis is a prominent neuroendocrine response to stress. Stimulation of this axis is associated with adrenaline (epinephrine) and noradrenaline (norepinephrine) release, which then leads to increased blood glucose levels, cardiac output, and skeletal muscle blood flow [1, 2].
In the realm of forensic pathology, catecholamine concentrations may be determined in postmortem serum obtained from blood collected at different sampling sites as well as pericardial and cerebrospinal fluids sampled during medicolegal autopsies. These concentrations have been indicated as useful in investigating stress responses during the death process in individual cases. This is especially true when assessed along with other biochemical and immunohistochemical analysis [3].
Urinary catecholamine levels have been reported to significantly increase in hypothermia fatalities. Measurement of these levels may thus be recommended in forensic pathology routine for the diagnosis of cold-related stress and death. More recently, urine adrenaline and its metabolite metanephrine have proven to be useful markers of stress responses related to cold exposure. Increases in these levels may thus help support the hypothesis of hypothermia-related death [4, 5].
Apart from these observations, data pertaining to catecholamine levels in urine collected during medicolegal autopsies are mainly limited to adrenaline and noradrenaline values in situations of suspected prolonged exposure to cold and subsequent death. Results concerning urinary concentrations of catecholamines and their metabolites in situations other than death by hypothermia are scarce indeed [3, 6, 7].
Strong sympathoadrenal activation is a hallmark of acute critical illness. Acute myocardial ischemia and other cardiac events immediately activate the sympathoadrenal axis, resulting in increases in circulating levels of adrenaline and noradrenaline [8].
In the study herein described, concentrations of catecholamines (adrenaline, noradrenaline, and dopamine) and their O-methylated metabolites (metanephrine, normetanephrine, and 3-methoxytyramine) were measured in urine and vitreous humor samples collected at autopsy in a series of cardiac deaths and noncardiac control cases that underwent medicolegal investigations. Our first aim was to determine whether cardiac events of different types (acute coronary thrombosis without myocardial infarction, acute coronary thrombosis with myocardial infarction, and arrhythmic cardiac death without acute coronary thrombosis) are characterized by different catecholamine/metanephrine urine and/or vitreous profiles. Our second aim was to assess whether noncardiac causes of death with different survival intervals/lengths of agonal period are characterized by different catecholamine/metanephrine urine and/or vitreous profiles.
Materials and methods
Study design and study populations
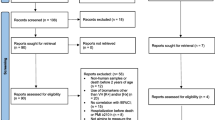
The present study was performed in 2014–2015. A total of 128 cases (94 males and 34 females) with a mean age of 46.4 years (range 18–71 years) were selected. Two study groups were formed, the first consisting of 72 cases of cardiac causes of death and the second consisting of 56 cases of noncardiac causes of death.
Medicolegal cases with cardiac causes of death were both prospectively and retrospectively selected and included:
-
Twenty-four cases of death involving individuals who had suddenly died in the presence of witnesses. All subjects underwent cardiopulmonary resuscitation. Catecholamine administration during cardiopulmonary resuscitation was not documented in any of these cases. Postmortem angiography performed prior to autopsy failed to show complete interruption of coronary artery opacification. Autopsies mainly revealed various degrees of coronary artery atherosclerosis with no evidence of significant luminal narrowing. Some cases were characterized by foci of interstitial fibrosis within the myocardium while none had acute coronary thrombosis or myocardial infarction. Immunohistochemistry did not reveal diffuse myocyte necrosis or necrosis involving groups of myocytes. Toxicology and biochemistry failed to provide evidence suggesting death following drug intoxication or metabolic disturbances. Postmortem biochemical investigations did not show significant increases in troponin T levels. Based on the results of all investigations, the cause of death was attributed to cardiac arrhythmia and cardiac arrest.
-
Twenty-four cases of death involving individuals with coronary artery atherosclerosis and acute coronary thrombosis, without acute myocardial infarction at autopsy. All subjects died without cardiopulmonary resuscitation, admission to hospital, or catecholamine administration. Postmortem angiography revealed complete interruption of coronary artery opacification at various locations. Macroscopy and microscopy confirmed the presence of acute thrombosis in the coronary arteries. Based on the results of all investigations, the cause of death was attributed to cardiac arrhythmia following acute coronary artery thrombosis.
-
Twenty-four cases of death involving individuals with coronary artery atherosclerosis, acute coronary thrombosis, and acute myocardial infarction at autopsy. All subjects died without cardiopulmonary resuscitation, hospital admission, or catecholamine administration. Postmortem angiography revealed complete interruption of coronary artery opacification at various locations. Macroscopy and microscopy confirmed the presence of acute thrombosis in the coronary arteries and myocardial infarction. Based on the results of all investigations, the cause of death was determined to be myocardial infarction in the presence of acute coronary artery thrombosis.
Case inclusion criteria consisted of postmortem interval (not exceeding 48 h) as well as urine and vitreous humor availability during autopsy. None of the selected cases had medical treatment that included beta-agonist or beta-blockers. Death and medicolegal autopsy intervals ranged between 6 and 48 h. All cases originated from forensic practice and underwent medicolegal autopsies as requested by local inquiring authorities. Postmortem biochemical analyses, including catecholamines and determination of their metabolites, were performed as part of the medicolegal investigations.
Noncardiac causes of death (control cases) were retrospectively selected and included:
-
Thirty-two cases of death characterized by short agony. This was defined as a period of a few seconds up to a few (five) minutes (eight cases of hanging, eight cases of thoracic gunshot wounds, eight cases of high falls, and eight cases of drowning). All these cases died without cardiopulmonary resuscitation, hospital admission, or catecholamine administration.
-
Twenty-four cases of death characterized by long agony. This was defined as a period lasting from several (above five) minutes up to hours (8 cases of thoracic and/or abdominal stab wounds and 16 cases of drug intoxication). All these cases died without cardiopulmonary resuscitation, hospital admission, or catecholamine administration.
Regarding the first group, all cases originated from forensic practice and underwent medicolegal autopsies as requested by local inquiring authorities. None had medical treatments that included beta-agonist or beta-blockers. Postmortem biochemical analyses, including catecholamines and determination of their metabolites, were performed as part of the medicolegal investigations. Death and medicolegal autopsy intervals ranged between 12 and 48 h. Case inclusion criteria consisted of postmortem interval (not exceeding 48 h) as well as urine and vitreous humor availability at autopsy.
Postmortem investigations and sample collection
Unenhanced computed tomography (CT) scans were performed before any manipulation of the corpses in all cases included in the study. Postmortem CT angiographies were systematically carried out after CT scans and prior to autopsies, according to the protocol previously described [9]. Complete, conventional medicolegal autopsies, histology, toxicology, and biochemical investigations were performed in all cases. Autopsies were jointly performed by two forensic pathologists (at least one board-certified) as in accordance with both local standards and international guidelines for medicolegal cases. Conventional histology included hematoxylin-eosin (HE) stains of brain, heart, lung, liver, and kidney samples. Immunohistochemical investigations using antibodies against fibronectin and C5b-9 of both cardiac ventricles were also performed in some selected cases of cardiac death.
Peripheral blood from the femoral veins, vitreous humor, and urine were systematically collected for toxicology and postmortem biochemistry as soon as possible upon arrival of the bodies at the morgue, prior to autopsy and prior to angiography.
Undiluted vitreous humor samples (between 1 and 3 ml) were obtained by aspiration using a sterile needle and syringe. Right and left vitreous samples were collected through a scleral puncture at the lateral canthus, aspirated from the center of each eye, pooled in the same syringe, and mixed together. After collection, vitreous samples were immediately centrifuged at 3000g for 15 min to remove debris. The separated supernatant was collected and stored in preservative-free tubes. No specimens were excluded due to insufficient sample volume. All samples were immediately frozen at −20 °C after collection.
Urine samples (between 5 and 10 ml) were collected by bladder aspiration using a sterile needle and syringe. After collection, specimens were centrifuged at 3000g for 15 min to remove debris. The separated supernatant was collected and stored in preservative-free tubes. Based on the results of former investigations, urine was collected in preservative-free tubes without acidification. All samples were frozen at −20 °C immediately after collection [5]. No specimens were excluded due to insufficient sample volume.
Laboratory assays
Catecholamines (adrenaline, noradrenaline, and dopamine), metanephrines (metanephrine and normetanephrine), and 3-methoxytyramine were analyzed in urine and vitreous humor using high-performance liquid chromatography (HPLC) with amperometric detection, as previously described [10].
The measured values in urine were related to creatinine concentrations in urine. Measured values in urine were expressed in nanomol per millimol creatinine. Measured concentrations in vitreous humor were expressed in nanomol per liter. Creatinine levels in urine were expressed in millimol per liter. The clinical reference intervals concerning fractionated metanephrines and catecholamines in urine were obtained from the clinical literature [11, 12]. Urine creatinine was determined (Jaffé method, rate-blanked, and compensated) by Roche standard methods on the Roche Modular P system (Roche Diagnostics GmbH, Mannheim, Germany).
Results
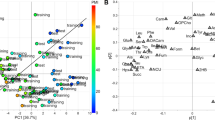
Data were analyzed by using the Stata statistical software package (Stata Corporation, College Station, TX, USA). Catecholamine, metanephrine, and 3-methoxytyramine concentrations in urine and vitreous humor in cardiac deaths and control cases (as well as within cardiac deaths and control cases) were compared using nonparametric tests. Statistical significance was set at p < 0.05. The relationship between catecholamine, metanephrine, and 3-methoxytyramine concentrations in urine and vitreous in cardiac deaths and control cases was also explored.
Tables 1 and 2 summarize the main results obtained in all studied groups in all tested samples.
In the cardiac death group, absolute values measured in urine for each of the analyzed markers displayed no significant differences relating to each of the tested subgroups. Analogously, in the control group, absolute values measured in urine for each of the analyzed markers failed to show significant differences relating to the cause of death and survival interval/length of agonal period. There were no statistically significant differences concerning catecholamine, metanephrine, and 3-methoxytyramine concentrations in urine in cardiac deaths compared to noncardiac cases.
Analysis of the results obtained from catecholamine, metanephrine, and 3-methoxytyramine measurements in vitreous humor revealed similar results. No statistically significant differences were observed in either cardiac deaths or control cases in relation to cause of death and length of agonal period. Analogously, no statistically significant differences were noticed in vitreous catecholamine, metanephrine, and 3-methoxytyramine levels between cardiac and noncardiac deaths.
Lastly, no correlation was observed between catecholamine, metanephrine, and 3-methoxytyramine concentrations in urine and vitreous humor in either of the studied groups.
Globally considered, these results tend to suggest that, contrary to what is observed in situations of prolonged exposure to cold and subsequent death, levels of urine and vitreous catecholamines, metanephrines, and 3-methoxytyramine measured after death in individual cases cannot be used to indicate the length of the dying process, irrespective of the cause of death.
Discussion
One of the current challenges for forensic pathologists in diagnosing the cause of death in cases of sudden, unexpected death depends on the fact that macroscopic and/or microscopic morphological correlates may be limited or completely absent due to the rapid dying process. This is especially true when death follows a functional disorder (for instance arrhythmia) or occurs in an initial stage of a disease. In these situations, morphological findings at autopsy may be scarce or missing. In such cases, ancillary techniques, including postmortem biochemistry, may help investigate the systemic pathophysiological changes involved in the dying process and formulate hypothesis pertaining to the cause of death [13–17].
Stress situations result in a massive release of catecholamines, which can be investigated after death by adrenaline and noradrenaline measurements in postmortem serum, vitreous humor, and urine as well as in pericardial and cerebrospinal fluids [3–7, 18, 19]. Increased serum concentrations of both adrenaline and noradrenaline have been reported in myocardial infarction deaths [4]. It has been speculated that catecholamine determination in different biological fluids collected at autopsy may help semi-quantify stress intensity and its role as a mechanism of death. Moreover, it has been postulated that high noradrenaline concentrations in cerebrospinal fluid or vitreous humor are especially indicative of protracted stress [15].
Prolonged exposure to cold leading to death is the most typical situation of forensic interest characterized by intense stress and subsequent sympatico-adrenal activation, which causes a rise in blood adrenaline and noradrenaline concentrations and their consequent increases in urine [4, 5, 15, 20]. In a recent study, not only increased values of urinary catecholamines but also those of their O-methylated metabolites may support the hypothesis of antemortem cold exposure, intense stress, and hypothermia-related deaths. However, adrenaline and metanephrine individually considered appeared to provide better diagnostic performance and discriminative values than other tested parameters and metabolites (noradrenaline, dopamine, normetanephrine, and 3-methoxytyramine) [5].
The reliability of urinary catecholamine determination in assessing antemortem stress intensity is based on their supposed stability in urine, irrespective of the time elapsed between death and sampling. Adrenaline and noradrenaline are considered to be biochemically stable in urine after death, with no significant changes in their concentrations with regard to the postmortem period [4, 5]. Ishikawa et al. [3] found that urinary catecholamine levels were virtually stable even 10 days after death, independent of the age or gender of the studied populations.
Catecholamine and metanephrine stability is crucial in ensuring the accuracy of their measurements (and the reliability of the measured values) in both the clinical and forensic setting. Indeed, both catecholamines and metanephrines are prone to oxidation. In the clinical setting, various authors have reported stability studies of catecholamines and metanephrines in biological fluids under different storage conditions, temperatures, and sample pHs. It was observed that free catecholamines and metanephrines are stable for at least 3 weeks in unpreserved samples stored at −80 °C. Some authors have observed that special requirements (such as acidification to pH 4) to stabilize catecholamines during urine collection and storage at room temperature do not appear to be necessary for fractionated metanephrines if samples were assayed or frozen within 1 week. Conversely, other research teams concluded that, in order to avoid issues with analyte instability, urine should be collected into acid (or acidified if collected fresh) and then frozen at −18 °C prior to analysis. This was recommended by some authors even though free metanephrines appear to be stable longer than free catecholamines for short periods of time at storage temperatures between 4 °C and −18 °C [21–24].
Determination of catecholamines in biological fluids collected at autopsy in causes of death other than hypothermia has been occasionally performed in the postmortem setting, with results often diverging. In a study performed on 119 medicolegal autopsies, Hausdörfer et al. [25] found that serum levels of catecholamines in instantaneous deaths were similar to the resting levels in the living, whereas serum levels in cases of prolonged death corresponded to those measured following maximal stress. Tormey et al. [6] obtained significantly different results measuring catecholamine concentrations in urine obtained from 30 unselected autopsies that included various subcategories of natural and traumatic deaths. These authors found overlapping urine catecholamine concentrations in cardiac and noncardiac causes of death, irrespective of the duration of the agonal period. Based on their results, they concluded that raised urine catecholamine levels are a common finding at the point of death and that urine catecholamine values in individual cases are useless to help indicate the length of the dying process.
Similar conclusions were drawn by Wilke et al. [7] based on the results obtained from a study involving 98 medicolegal cases with various causes of death and agonal durations. These authors found that urine catecholamine concentrations did not allow any hypothesis pertaining to the type of death or length of the dying process to be formulated. Concerning the measured values in vitreous, they observed that catecholamine levels only allowed the cases who had cardiopulmonary resuscitation with documented administration of adrenaline to be distinctively identified from the other investigated cases. A more recent study involving 83 hypothermia-related deaths and 144 forensic autopsy cases with diverse traumatic, violent, and natural causes of death confirmed the conclusions of Wilke et al. [7] by showing comparable urinary adrenaline and noradrenaline concentrations irrespective of the cause of death (traumatic death, drug intoxication, coronary thrombosis, or suicide by hanging) or duration of the agonal phase [5].
Contrasting conclusions were reached by Pakanen at al. [4], who found increased urinary noradrenaline concentrations (and low adrenaline levels) in a series of medicolegal autopsies including 103 cardiovascular deaths that had no signs of cold exposure. In recent years, Ishikawa et al. [3] performed a comprehensive study focusing on adrenaline, noradrenaline, and dopamine determination in postmortem serum from right heart blood and urine obtained from 199 consecutive forensic autopsy cases with various causes of death, survival times, and postmortem intervals. These authors found significant differences pertaining to catecholamine fraction profiles in urine compared to postmortem serum in different causes of death. They also observed that urinary adrenaline levels were increased in both hypothermia- and hyperthermia-related deaths (which also showed increased urine noradrenaline concentrations) and low in mechanical asphyxiation and acute cardiac deaths (which also had decreased urinary values of noradrenaline). Lastly, the authors failed to observe significant differences between urine adrenaline and noradrenaline concentrations in hypothermia- (and hyperthermia-) related cases compared to prolonged natural deaths. They attributed these findings to the diverse intensity and duration of stress responses in acute and prolonged deaths. They therefore concluded that the postmortem profiles of urinary catecholamine fractions might be useful in differentiating sudden, acute cardiac deaths from those characterized by more intense, prolonged stress responses such as cold exposure- (and heat stroke-) related fatalities.
Concerning metanephrine and 3-methoxytyramine determination in urine samples collected after death, forensic literature in this field is quite limited at present. The only study performed on this topic appears to suggest that no significant differences pertaining to urinary metanephrine and 3-methoxytyramine concentrations may be found in different types of traumatic death [5].
The results of the study presented herein tend to be in agreement with those reported by Tormey et al. [6] and Wilke et al. [7] and suggest that catecholamine and metanephrine profiles determined in urine samples collected after death do not allow any differentiation among cardiac events or violent deaths of different types to be made nor any hypotheses pertaining to the duration of the agonal period to be formulated. This same conclusion can be generalized for catecholamine and metanephrine profiles in vitreous humor, contrary to what former authors have postulated.
Our findings do not seem to confirm the conclusions of studies performed by Pakanen at al. [4] and Ishikawa et al. [3]. Hence, they fail to corroborate the usefulness of urine catecholamine and metanephrine analysis to characterize stress response intensity or length of the dying process in the postmortem setting. Based on our results, we might speculate that the diagnosis of suspected antemortem cold exposure- and hypothermia-related death is the only situation of forensic interest for which catecholamine and metanephrine measurement in urine specimens collected at autopsy is unquestionably helpful.
The limitations of our study must be acknowledged. The most important is the relatively small number of studied cases, which may limit the accuracy of our research. However, precise selection criteria were applied during the recruitment process in all studied groups and subgroups in order to minimize heterogeneity in the study populations. Prospective investigations including a greater number of subjects are therefore needed to confirm or invalidate our findings.
To conclude, though further studies are required to confirm these preliminary observations, our results suggest that postmortem urine (and vitreous) catecholamine and metanephrine profiles are of limited value in quantifying antemortem stress reactions in both violent and cardiac deaths, except in cases of hypothermia fatalities. The combination of biochemical investigations performed simultaneously in several biological fluids (and potentially involving several different biomarkers) could be a topic of interest and future research. A study of this nature might help to better understand the activation of the pituitary-adrenal axis as well as the systemic pathophysiological changes involved in the dying process in individual cases.
References
Zouhal H, Jacob C, Delamarche P, Gratas-Delamarche A (2008) Catecholamines and the effects of exercise, training and gender. Sports Med 38:401–423
Ranabir S, Reetu K (2011) Stress and hormones. Indian J Endocrinol Metab 15:18–22
Ishikawa T, Inamori-Kawamoto O, Quan L, Michiue T, Chen JH, Wang Q, Zhu BL, Maeda H (2014) Postmortem urinary catecholamine levels with regard to the cause of death. Legal Med 16:344–349
Pakanen L, Kortelainen ML, Särkioja T, Porvari K (2011) Increased adrenaline to noradrenaline ratio is a superior indicator of antemortem hypothermia compared with separate catecholamine concentrations. J Forensic Sci 56:1213–1218
Palmiere C, Teresiński G, Hejna P, Mangin P, Grouzmann E (2014) Diagnostic performance of urinary metanephrines for the postmortem diagnosis of hypothermia. Forensic Sci Med Pathol 10:518–525
Tormey WP, Carney M, FitzGerald RJ (1999) Catecholamines in urine after death. Forensic Sci Int 103:67–71
Wilke N, Janssen H, Fahrenhorst C, Hecker H, Manns MP, Brabant EG, Tröger HD, Breitmeier D (2007) Postmortem determination of concentrations of stress hormones in various body fluids—is there a dependency between adrenaline/noradrenaline quotient, cause of death and agony time? Int J Legal Med 121:385–394
Ostrowski SR, Pedersen SH, Jensen JS, Mogelvang R, Johansson PI (2013) Acute myocardial infarction is associated with endothelial glycocalyx and cell damage and a parallel increase in circulating catecholamines. Crit Care 17:R32
Grabherr S, Doenz F, Steger B, Dirnhofer R, Dominguez A, Sollberger B, Gygax E, Rizzo E, Chevallier C, Meuli R, Mangin P (2011) Multi-phase post-mortem CT angiography: development of a standardized protocol. Int J Legal Med 125:791–802
Grouzmann E, Fathi M, Gillet M, de Torrenté A, Cavadas C, Brunner H, Buclin T (2001) Disappearance rate of catecholamines, total metanephrines, and neuropeptide Y from the plasma of patients after resection of pheochromocytoma. Clin Chem 47:1075–1082
Grouzmann E, Drouard-Troalen L, Baudin E, Plouin PF, Muller B, Grand D, Buclin T (2010) Diagnostic accuracy of free and total metanephrines in plasma and fractionated metanephrines in urine of patients with pheochromocytoma. Eur J Endocrinol 162:951–960
Pussard E, Neveux M, Guigueno N (2009) Reference intervals for urinary catecholamines and metabolites from birth to adulthood. Clin Biochem 42:536–539
Madea B (2009) Sudden death, especially in infancy—improvement of diagnoses by biochemistry, immunohistochemistry and molecular pathology. Legal Med 11(Suppl 1):S36–S42
Madea H, Zhu BL, Ishikawa T, Quan L, Michiue T (2009) Significance of postmortem biochemistry in determining the cause of death. Legal Med 11(Suppl 1):S46–S49
Kernbach-Wighton G (2009) Diagnostic problems with functional cause of death: analytical approaches and procedures. Legal Med 11(Suppl 1):S31–S35
Maeda H, Zhu BL, Ishikawa T, Michiue T (2010) Forensic molecular pathology of violent deaths. Forensic Sci Int 203:83–92
Luna A (2009) Is postmortem biochemistry really useful? Why is it not widely used in forensic pathology? Legal Med 11(Suppl 1):S27–S30
Zhu BL, Ishikawa T, Michiue T, Li DR, Zhao D, Quan L, Oritani S, Bessho Y, Maeda H (2007) Postmortem serum catecholamine levels in relation to the cause of death. Forensic Sci Int 173:122–129
Ishikawa T, Quan L, Michiue T, Kawamoto O, Wang Q, Chen JH, Zhu BL, Maeda H (2013) Postmortem catecholamine levels in pericardial and cerebrospinal fluids with regard to the cause of death in medicolegal autopsy. Forensic Sci Int 228:52–60
Palmiere C, Bardy D, Letovanec I, Mangin P, Augsburger M, Ventura F, Iglesias K, Werner D (2013) Biochemical markers of fatal hypothermia. Forensic Sci Int 226:54–61
Chan EC, Wee PY, Ho PC (2000) Evaluation of degradation of urinary catecholamines and metanephrines and deconjugation of their sulfoconjugates using stability-indicating reversed-phase ion-pair HPLC with electrochemical detection. J Pharm Biomed Anal 22:515–526
Willemsen JJ, Ross HA, Lenders JW, Sweep FC (2007) Stability of urinary fractionated metanephrines and catecholamines during collection, shipment, and storage of samples. Clin Chem 53:268–272
Roberts NB, Higgins G, Sargazi M (2010) A study on the stability of urinary free catecholamines and free methyl-derivatives at different pH, temperature and time of storage. Clin Chem Lab Med 48:81–87
Peitzsch M, Pelzel D, Lattke P, Siegert G, Eisenhofer G (2015) Preservation of urine free catecholamines and their free O-methylated metabolites with citric acid as an alternative to hydrochloric acid for LC-MS/MS-based analyses. Clin Chem Lab Med. doi:10.1515/cclm-2015-0044
Hausdörfer C, Pedal I, Zimmer G, Remppis A, Strobel G (1999) Catecholamines, myofibrillary degeneration of the heart muscle and cardiac troponin T in various types of agony. Arch Kriminol 196:46–57
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Ethics approval
All relevant ethical issues were identified and discussed with the local ethical committee. No ethical approval was necessary to perform biochemical analyses in the collected cases.
Rights and permissions
About this article
Cite this article
Hervet, T., Grouzmann, E., Grabherr, S. et al. Determination of urinary catecholamines and metanephrines in cardiac deaths. Int J Legal Med 130, 995–1001 (2016). https://doi.org/10.1007/s00414-015-1303-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-015-1303-2