Abstract
The K+ and hypoxanthine (Hx) concentrations of the vitreous humour (VH) rise gradually after death, providing a means of estimating the post-mortem interval (PMI). The correlation between these analytes and the PMI is good since the vitreous chamber is partially isolated from autolytic events occurring elsewhere; the [K +] and [Hx] recorded is thus the result of changes within the eye. The present work provides a systematic review, following PRISMA recommendations, of 36 articles (3 reviews and 33 retrospective cohort studies) discussing the many procedures and regression models that have been developed for improving PMI estimates involving VH analytes. The results of a descriptive study are also provided, highlighting the causes and distribution of mortality as registered in medico-legal autopsies performed in 2019 in Galicia (northwestern Spain), and revealing the use of these PMI estimation methods in real forensic practice. Great heterogeneity was detected in the collection of VH samples, the treatments to which they were subjected before examination, and in their conservation and analysis. A lack of reproducibility in the analytical methods employed to estimate [K +] and [Hx] was noted, as well as an absence of external validation for most of the regression formulae used to determine the PMI from analyte values. The use of methods based on high-performance liquid chromatography, focal electrophoresis, or thermogravimetric/chemometric procedures might solve the problems encountered with traditional analytical techniques, offering reliable results more quickly and effectively (even when samples are contaminated). This study recommends using flexible multiple regression models that combine physical and chemical variables, and that population databases be constructed so that models can be properly validated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Estimating the post-mortem interval (PMI) has long been an important procedure in forensic investigations. Estimates can be made using a variety of methods that can be classified by reliability according to the qualitative and quantitative evidence collected [1]. In descending order, these involve:
-
Collecting quantitative evidence via the use of precision tests and correcting factors; these tests are based on the cooling of the cadaver and the biochemistry of the vitreous humour (VH).
-
Relying on subjective measurements that require the use of quantifying scales and correcting factors.
-
Relying on subjective methods that involve the use of empirical estimates and correcting factors.
-
Relying on subjective measurements based on empirical conclusions.
-
Post-mortem changes dependent on environmental conditions.
Attempts have been made to develop methods that can be used with any type of cadaver, but to date, none has been entirely successful, a consequence of the many contextual and environmental variables to which a dead body is subject. In forensic investigations, the best PMI estimates are usually obtained by combining different methods [2], and further combining these with information provided by witnesses.
For some years, the biochemistry of the VH has received attention for estimating the PMI, with [K+] and [hypoxanthine {Hx}] the major variables of interest. After death, VH [K+] gradually increases [3], the result of simple diffusion across cell membranes, while VH [Hx] depends on both diffusion and the activity of the enzyme xanthine oxidase. The vitreous chamber provides protection from putrefaction for some time, offering a chance to study the post-mortem modifications it experiences independent of those affecting the external environment [4, 5].
The idea of using post-mortem changes in [K+] as a marker of time since death was introduced by Sturner in 1963 [3]. In 2001 [6], it was established that the best way to make a regression model was by using [K+] and/or [Hx] as the independent or predictive variable (IV). The environmental temperature is now taken into account in multi-variable models that also include rectal temperature, VH [urea], and age at or cause of death [7,8,9].
Several functions for estimating PMI have been proposed that reflect strong correlations between the former and VH analytes. However, most have not been properly validated. This leads to results appearing better than they may really be [10].
The use of quantitative tools is uncommon. In Galicia (northwestern Spain), the PMI is frequently estimated from circumstantial evidence and cadaveric phenomena—quick and easy, but not as accurate.
This paper presents literature discussing the accuracy and reliability of estimating the PMI via the biochemistry of the VH. To determine how often VH biochemistry is used in PMI estimates made in forensic investigations in Galicia, a retrospective study was performed to examine the methods used by the Galician Institute of Legal Medicine (IMELGA; the public institution responsible for investigating violent and suspicious deaths in the region) to estimate PMI throughout 2019.
Material and methods
Systematic review
A systematic search was made in PubMed for papers published between 01/01/1950 and10/11/2021 focusing on VH [K+] and/or [Hx], alone or with other variables, for estimating the PMI. This was done using MeSH terms, free terms, and combinations:
“Humor vítreo AND intervalo post mórtem” OR “Ciencias forenses AND humor vítreo AND potasio” OR “Humor vítreo AND PMI” OR “Humor vítreo AND (potasio OR hipoxantina) AND tiempo desde la muerte” OR “Cronodiagnóstico AND humor vítreo AND potasio” OR “Vitreous humor AND time since death” OR “Post-mortem biomarkers AND vitreous humour” OR “(Potassium OR hypoxanthine) AND vitreous humour AND time since death” OR “Thanatochemistry AND (potassium OR hypoxanthine)” OR “(Potassium OR hypoxanthine) AND vitreous humour AND regression model AND time since death” OR “Potassium AND linear correlation AND vitreous humour AND time since death” OR “PMI AND (potassium OR hypoxanthine) AND vitreous humour” OR “Vitreous potassium AND postmortem interval” OR “PMI AND thanatochemistry AND potassium AND vitreous humour” OR “Postmortem biomarkers AND (potassium OR hypoxanthine) AND vitreous humour” OR “Forensic pathology AND vitreous humour AND (potassium OR hypoxanthine)” OR “Estimation of postmortem interval AND vitreous humour” OR “Estimation of postmortem interval and K+”.
The filters applied were Full text, Classical Article, Clinical Study, Clinical Trial, Controlled Clinical Trial, Journal Article, Meta-Analysis, Observational Study, Pragmatic Clinical Trial, Preprint, Randomized Controlled Trial, Review, Systematic Review, Humans, English, Spanish, Preschool Child: 2–5 years, Child: 6–12 years, Adolescent: 13–18 years, Adult: 19 + years, Young Adult: 19–24 years, Adult: 19–44 years, Middle Aged + Aged: 45 + years, Middle Aged: 45–64 years, Aged: 65 + years, 80 and over: 80 + years, from 1950 – 2020/10/12.
Google Scholar was also used to detect further papers in Spanish, employing search terms such as “Humor vítreo, intervalo post mórtem, potasio, y/o, hipoxantina. The filters used were Desde 1950 hasta 2020, Buscar páginas solo en español.
The resulting documents underwent further filtering by inspection of the title, abstract, and keywords. Those finally included in the analysis had to:
-
Aim to determine/quantify the accuracy of PMI estimates made via VH [K+] and/or [Hx] analysis.
-
Examine correlations of the variables of interest or discuss germane adjusted regression models, providing correlation coefficients, goodness of fit, mean squared error, confidence intervals, or p values.
-
Be either observational or experimental, a systematic review, or a meta-analysis.
-
Involve a validated VH extraction technique.
-
Involve cadavers not in an advanced stage of putrefaction (≤ 210 h since death), showing no large hydro/electrolyte alterations, and with death being extra-hospital in nature and of medico-legal interest.
-
Involve transparent VH with no blood, and be from an intact eye of a non-decapitated cadaver.
-
Involve victims over 2 years of age.
-
Be written in English, Spanish, German, or French.
The references of the chosen papers were checked to detect any further works of interest missed in the above searches.
The following data were recorded from the chosen papers:
-
Name of first and last author, location where study was performed, date of publication, study design, aims.
-
Inclusion and exclusion criteria, sample size, extraction and treatment of VH samples, variables recorded (VH [K+] and [Hx], other analytes, bodyweight, age, rectal temperature [Tr], among other variables.
-
Results including linear determination coefficient (R), standard deviation, means squared error, prediction/correlation formulae, 95% confidence interval (95%CI) for PMI, and p value.
-
Biases, methodological quality.
The criteria of the Scottish Intercollegiate Guidelines Network (SIGN) [11] were used to assess the level of evidence and degree of recommendation of the analysed reviews. Clinical trials and meta-analyses are level 1, and score ++ for little risk of bias, + for moderate risk of bias, or – for high risk. Reviews of observational studies (case control and cohort studies) are level 2, with ++ if the probability of a causal relationship is high, + if moderate, or – if poor. Case reports are level 3, and expert opinions level 4. A recommendation level A was awarded if 1 ++ or 1 + studies were applicable to their target population; B was awarded to 2 ++ studies applicable to the target population but globally consistent; C to 2 + studies applicable to the target population but globally consistent; and D to the rest.
The methodological quality of each study was decided using CASP software [12]. Reviews were given overall scores summarizing the methodological quality of the works discussed; the answers given are yes, no, or can’t tell. Scores awarded for the results are either 1 or 0 depending on whether certain criteria are met. The review table (Table 1) constructed provides a final score for each paper of 0–10 (≥ 8 = high quality; 6–7 = moderate quality; ≤ 5 = low quality). This table also records the first and last authors, the date of publication, design, the IV and dependent variable (DV), sample characteristics, results, and observations.
Estimation of the PMI in Galicia
Information was obtained on all forensic autopsies performed in 2019 by the IMELGA centres in Galicia (those of A Coruña, Lugo, Santiago de Compostela, Ourense, Pontevedra, Ferrol, and Vigo). The data collected included age, sex, month of death, medico-legal aetiology, main cause of death, and the method used to estimate the PMI. Reports missing any of this information were excluded.
Results
Systematic review
Of the 288 articles that were initially located and processed, a final total of 36 studies were admitted for study. Figure 1 summarises the selection process.
Table 1 provides the details of the 36 studies analysed. Of these, 21 were performed in Europe, four each in the USA and India, and the remainder in Thailand, South Korea, China, Egypt, Peru, Canada, and Australia.
In cohort studies, the most frequently used analyte, alone or in combination, was VH [K+]. In 23 studies, [K+] or [Hx] were analysed alone or in combination with other analytes. Two studies reported the development of regression models involving VH [K+], VH [Hx], and Tr or ambient temperature (Ta), and eight involved [K+] and/or VH [Hx] plus VH [Na2+], [Ca2+], [Mg2+], and [Cl−], and the VH concentrations of urea, creatinine, albumin, uric acid, or glucose. A total of 28 studies reported only VH analytical results, one reported the same plus synovial fluid (SF) concentrations, and three examined the VH and CSF.
Two papers were narrative reviews—one a review plus a cohort study. Thirty-three studies were retrospective cohort studies. Twenty-four studies involved simple linear correlation, one involved Loess local regression, and eight involved advanced regression models, of which three combined simple and multiple linear regression.
Muñoz et al. [6] highlighted the need to swap the identity of the DV and IV. Since then, papers have identified PMI as the DV (excluding Zhou et al. [13] and Bortolotti et al. [14]). Before 2001, all papers were published with the PMI as the IV (excluding Lange et al. [15]). Most studies excluded contaminated VH, and that from cadavers belonging to people with a chronic disease, who suffered electrolyte alterations, took diuretics, were dehydrated, or had chronic kidney disease. In four studies, those who had died from drug overdoses were excluded, and in three, victims of drowning were excluded.
Different treatments of the VH samples were noted. Sclera puncture with slow but complete aspiration, followed by centrifugation, was the most common pre-analytical step taken. Three papers used VH microsamples, while one involved repeated sclera puncturing. Studies also used different sample preservation methods, including the storage temperature used. Finally, in 17 studies, VH [K+] was determined by direct or indirect electrode potentiometry, 12 used photometry, two used capillary electrography, one low-pressure ion chromatography, and one liquid chromatography and mass spectrometry (LC–MS/MS).
Correlations between analytes and PMI
Of the 36 studies examined, 24 involved the use of simple linear regression to correlate VH [K+] with the PMI (Table 2). Coe et al. [23] concluded that large variations existed in the error obtained (± 26 h), and that the Sturner et al. [3] model was the most accurate. In 1989, Madea et al. [24] obtained a 95%CI of ± 34 h with their model, improving to ± 22 h if samples with VH [urea] of > 100 mg/dL were excluded, and to ± 20 h if persons who suffered an agonal period of > 6 h were excluded. Later, in 1994, the same authors showed that VH [Hx] was no better than VH [K+] for determining PMI, and that the increase in CSF [Hx] was not linear [27].
In 2001, using [K+] as the IV, Muñoz et al. [6] obtained a better correlation between VH [K+] and PMI, changing the established paradigm in which the latter is determined [14]. In 2005, Madea et al. [2] also concluded that the relationship between VH [K+] and PMI is not entirely linear due to interindividual variation. They also noted that multiple regression analysis improved the accuracy of PMI estimation.
The window during which increases in VH [K+] with PMI were found to be linear differed between publications. Tatiya et al. [38] reported a linear increase until a PMI of 48 h. Zhou et al. [13], Bortolotti et al. [14], and Nermeen et al. [32] reported this linear relationship to be stronger in cadavers with a PMI of > 24 h.
In 2016, Ortmann et al. [36] concluded that in European climates the models of Madea et al. [29] and Muñoz et al. [6] provided the most accurate results, but that new formulae were needed for hotter climates. However, this conclusion does not take into account seasonal variations, sun exposure, shade, or indoor/outdoor conditions.
Devenaux et al. [19] concluded a positive significant linear correlation to exist between VH [K+] and PMI, and a negative correlation between PMI and both VH [Na+] and [Cl−]. Other studies also focused on whether there was a linear correlation between combinations of analytes and PMI. VH [K+] with [Na +] and [glucose] [25], and VH [K+] and [NH4+] [43], as well as VH [Hx] with [lactic acid] in cadavers grouped by season of the year and Ta, were all examined [40], but VH [K+] and [Hx] alone were found to be the most reliable. The reliability of VH and CSF analytes, and their combinations, was also examined; VH analytes alone were found to give the best results [42]. In these studies, VH [K+] and VH [Hx] were both found to show a linear relationship with PMI, although this was contradicted by Chandrakanth et al. in 2012 [30].
Among the studies that involved non-linear, multivariate analysis, Lange et al. [15] used the Loess regression and obtained a smaller standard error with lower VH [K +] values. However, Madea et al. [29] determined the latter model to overestimate the PMI. In 2016, Rognum et al. [35] used two separate multivariate algorithms with [K+] and [Hx]. In 2018, Srettabunyong et al. [39] correlated PMI with VH and synovial fluid [K+], [Na+], [glucose], [creatinine], [urea], [lactate], and [uric acid], and obtained good PMI results for both backgrounds. Other authors [14] worked with a multivariate model combining [Hx], [urea], and [K +], while Focardi [43], in 2020, developed a model combining [K +] and [albumin] or log[albumin] which had a very good fit. In 2018, Cordeiro et al. [7] concluded that generalized additive models were better for determining the PMI, and improved when physico-chemical variables were included. The model that combined Tr, Ta, and VH [K +], [Hx], [urea], and bodyweight gave the highest R value (0.786), while that which used Tr and VH [K +], [Hx], [urea], and bodyweight gave the lowest mean squared error.
Other factors that might modify the predictor variable-PMI relationship
In 2005, Madea et al. [2] reported that the slope correlating VH [K+] and PMI should be steeper as Ta increases. According to Coe [23], the regression slope may vary between 0.14 and 0.55 mEq/L/h. As the PMI becomes longer, the diffusion velocity of K+ becomes slower as equilibrium is approached. Muñoz et al. [6, 9] suggest that not properly stating which variable is the IV, and which is the DV, makes comparisons between studies difficult.
Many factors might affect the slope obtained: for example, the effects of electrolytic alterations before death on the predictor variable-PMI relationship, the duration of any disease, and the length of the agonal period. Many studies excluded cadavers with signs of eye trauma or chronic disease, with non-transparent VH, or that were victims of decapitation. Madea et al. [24] reported that knowing the urea concentration before death, and whether the agonal period was prolonged, significantly improved the accuracy of PMI estimates. Muñoz et al. [6] reported better accuracy in determining non-hospital death PMIs when the VH [urea] was > 30 mg/dL and [creatinine] ≤ 0.5 mg/dL (95%CI ± 17.55 h.
In some publications [21, 43], cadavers of people with sepsis or drug intoxication were excluded, and some involved only persons aged 18–65 years or with a PMI of 3–30 h. Tatiya et al. [38] and Cordeiro et al. [7] included cadavers with a PMI known to be within ± 15 min. The latter authors also excluded samples from people who died in a state of hypo-/hyperthermia but took data on any resuscitation manoeuvres used. Srettabunjong et al. [39] included very early samples (< 8 h) and excluded cadavers that had been submerged in water. Go et al. [40] classified cadavers with a PMI of < 103 h according to the season of the year in which death occurred. Garland et al. [42] ruled out cadavers from people who were murdered, those submerged in water, and the bodies of children. Finally, Palacio et al. [44] only examined cadavers of people aged 19–75 years and excluded those showing signs of opiate intoxication.
The sample sizes in each paper examined, how they were obtained, pre-treated, and analysed, may also have influenced PMI estimates (Table 1).
Finally, other variables of interest may be important. Stephens et al. [21] considered the cause of death to be a determining factor in PMI estimation. Lange et al. [15] affirmed that as VH [K+] increases, so too does this error. This was later corroborated by Ortmann et al. [36].
Coe et al. [23] reported that the differences between eyes were more evident when determined by indirect potentiometry than by flame emission spectrophotometry, and that VH [K+] was higher in children and in samples with VH [urea] > 100 mg/dL. They also recommended that as much VH be aspirated as possible so that the results were not affected by any difference in concentration between different parts of the vitreous chamber. Rognum et al. [25] showed the VH [Hx] to be elevated in children who had died from sudden infant death syndrome or infection. In contrast, in live patients undergoing vitrectomy, VH [Hx] was close to zero. It may thus be concluded that significant periods of hypoxia prior to death induce [Hx] elevation. It should be noted that [Hx] may be influenced by electrolyte alterations and alcoholism [35].
Gamero et al. [26] and Madea et al. [29] reported age to have a major influence on VH [K+]. They also concluded the variation in VH [Hx], but not in CSF [Hx], to be linear. Mild and moderate hypoxias were found to significantly affect VH [Hx], as did electrolyte alterations, alcoholism, and genetically related abnormalities in purine metabolism [35]. The formulae suggested by Rognum et al. [35]—with precautions and restraints—are available in an app (iTOD) available for free in app stores.
Muñoz et al. [6] indicated that cause of death and admission to hospital before death have a significant influence on PMI estimates. Age was also said to affect VH [K+] (with greater concentrations seen in children). The same authors, as well as Saldaña et al. [41], also concluded that VH [urea] could be used as a pre-death marker of electrolyte balance since it changed little with advancing PMI.
Schmidt et al. [22] reported no differences between the two eyes when sampled < 4 h or > 4 h apart. Madea et al. [2] reported a 10% difference between the eyes when samples were analysed using different techniques. Other authors saw no such differences [14, 22, 30,31,32].
Cordeiro et al. [7] found neither age, cause of death, resuscitation manoeuvres, nor sex to have any significant influence on PMI estimates. They did conclude, however, that the post-collection storage temperature should be < 10 °C, and that bodyweight did influence PMI estimates. Srettabunjong et al. [39] reported that [K+], [Na+], [Cl−], and [Mg2+] were higher in the VH than in the synovial fluid. Finally, Coe et al. [23] determined the gold standard for VH collection to be scleral puncture with slow aspiration of all the VH possible using an 18-20G needle, followed by centrifugation at 3000 rpm for 10 min (with the freezing of samples not immediately tested). This procedure was the most commonly used in the papers examined.
Table 2 shows the great variation in the formulae used to estimate the PMI. These variations are the result of differences in the sample sizes available, the collection and pre-treatment of samples, and the analytical technique used to determine the analyte concentrations.
Methodological quality of the examined studies and their limitations
The present work examined three reviews of cohort studies and 33 retrospective cohort studies. The reviews of Coe et al. [23], Lange et al. [15] and Madea et al. [2] discussed papers with SIGN classifications [9] of 2 + + B. The retrospective cohort studies of Chandrakanth et al. [30], Srettabunjong et al. [39], and Garland et al. [42] were classified as 2- D, while those of Adjutantis et al. [17], Aggarwal et al. [18], Gamero et al. [26], Mulla et al. [28], and Palacio et al. [44] had classifications of 2- C. The remaining 25 studies were classified as 2 + C. Tables 3 and 4 show the results of the CASP analysis of the reviews/cohort studies [12].
Both Coe et al. [23] and Madea et al. [2] (Table 3) examined the results of quality papers (scores 9 and 8 out of 10 respectively). Lange et al. [15] used the data in their review to determine a model for estimating PMI by local regression. Referring to Lange et al. [15], Madea et al. [2, 24] indicate that the variation in VH [K+] in six of the studies examined rendered results inapplicable to other populations. When Madea et al. [2] used the latter authors’ regression model with their own data, they noticed several overestimates.
The retrospective cohort studies (Table 4) had notable limitations. For example, in the study of Sturner et al. [3], the burnt or frozen cadavers studied had no control group, and the formula presented only works if the Ta is < 10 °C (2), and even then, it tends to overestimate the PMI [36].
Some papers, such as that of Adjutantis et al. [17], only involved cadavers with a short PMI.
The formula of Aggarwal et al. [18] underestimated the PMI, as shown by Gamero et al. [26], and their samples only included a few cadavers with a PMI of < 24 h. Stephen et al. [21] only included cadavers with a PMI of up to 35 h.
Madea et al. [24] proposed an arbitrary VH [urea] limit of > 100 mg/dL. They did not examine any other markers of pre-death electrolytic alteration.
Rognum et al. [25] used repeated extractions, but the trauma generated may have increased the VH [Hx]. According to Madea [24], the latter authors could not properly conclude that the slope for VH [K+] was steeper than that for [Hx].
To allow for comparisons between VH and synovial fluid analysts, Srettabunjong et al. [39] excluded cadavers of people with joint disease, and had no pre-death information for any cadaver, perhaps reducing the study’s external validity.
Mihailovic et al. [31] did not take into account the effect of Ta on VH [K+]. The repetitive sampling reduced the volume of the VH; this, plus the diffusion occurring, could have led to a further elevation of VH [K+].
Tumram et al. [33] studied cadavers with a PMI of up to 18 h, but the regression slope obtained is only applicable in hot climates.
Chandrakanth et al. [30] examined cadavers with a maximum PMI of 36 h, some of which were victims of poisoning, and the study group (n = 70) and control group (n = 30) numbers were unbalanced.
Cordeiro et al. [7] log-transformed their values to ensure the homoscedasticity of their models—an inconvenience (although easily resolved).
Go et al. [40] did not consider the influence of the cause of death since they had no pre-death information. This is also apparent in other publications [16, 19, 22].
Saldaña et al. [41] worked with a very small sample and indicated that the analytical equipment they used had limitations.
The work of Garland et al. [42] was exploratory and involved just 20 samples. The effects of sample storage, Ta, and pre-treatment were not analysed, and PMI was defined as the time between finding the body and the time of sample analysis.
Focardi et al. [43] included cadavers of PMI > 72 h but the effects of sex, age, and bodyweight were not studied.
Finally, Devenaux et al. [19], and Palacio et al. [44], had a small sample size, and the variation in the results and the standard error for cadavers with a PMI of < 60 h was large.
Estimating the PMI in Galicia
The IMELGA centres in Galicia examined 1913 cases. Those involving persons who had spent a prolonged period in hospital, and cases in which there was a question about the reliability of the information, were excluded, leaving a total of 1768 cases for study. The sample examined included 1256 men and 512 women. The mean number of deaths was 148.67/month (SD ± 17.8).
Forensic reports normally mention the major cause of death based on the International Classification [46], but this classification is insufficiently precise for a study of the present nature. The most common cause of death was cardiovascular (ischemic heart disease), followed by asphyxia (more specifically, hanging); see Fig. 2. The cause of death in 973 (55.03%) cases was natural, in 495 accidental, in 285 suicide, and in 15 (0.85%) homicide.
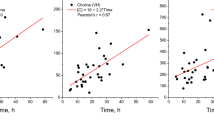
Table 5 shows the methods used. On very few occasions was PMI estimated using more than one method. Most often, it was estimated only from circumstantial evidence (54.75%). VH biochemistry was used on its own on 10 occasions, combined with cadaveric phenomena plus forensic entomology on three occasions, with cadaveric phenomena on two, and with temperature on another two. The formula most used was that of Muñoz et al. [4] (eight occasions), followed by that of Madea et al. [18] (four occasions). Figure 3 shows that quantitative methods were only used in the first 72 h after death; cadaveric phenomena were most commonly employed to determine the PMI (93.73%).
The Galician data show that circumstantial information (such as witness’ accounts) is commonly deemed sufficient to estimate the PMI. It is more easily obtained and more reliable when less time has elapsed since death. This is reflected in the low mean PMI value and small associated SD (Table 6). In cases with late cadaveric phenomena and signs of putrefaction, the method used to determine the PMI relied on these same phenomena; VH biochemistry would not be reliable in such cases, leaving any analytical results without value. In cases in which an intermediate interval had elapsed since death, biochemical methods and Tr were used to estimate the PMI. It is therefore uncertain whether taking just one sample for testing via only one method is good enough for estimating the PMI. In practice, two or more samples should be taken and more than one method used to estimate the PMI (although this is not always possible). Despite the impossibility of providing a statistical analysis, the present data doubtlessly open the debate on the need to use more than one method to estimate PMI.
Discussion
Numerous methods are available for correlating VH with the PMI. VH [K +] and the PMI are best related via the formulae of Madea et al. [24] or Muñoz et al. [6, 9]. Ta, which has been reported to strongly influence VH [K+] and [Hx] [35, 36], was omitted from many models. A correlation has also been recorded between the increase in VH [K+] and [Hx]. The values for VH [Hx] in the first 24 h after death are, in fact, less dispersed than those for VH [K+], but PMI estimates are less accurate if determined from VH [Hx] alone than from VH [K+] alone [2, 6, 24, 35].
PMI estimates are influenced by variables such as trauma, eye disease, and hydroelectrolytic disturbances [6, 24]. These factors were considered in most of the studies examined.
High values for VH [urea] and [creatinine] have been related to higher VH [K +] [6, 36], although few studies took this into account. Age, however, may not be important except when the cadaver is that of a very young child [7, 27]. Finally, deaths by carbonization, freezing, or drowning were excluded in most studies.
Despite the linear trend in VH [K+] and [Hx] regarding PMI, the slope was somewhat steeper in the first 6 h [23]. This trend was seen in most papers, although Chandrakanth et al. [30] found no correlation between [Na+], [K+], [Cl−], or [Na+]/[K+] and PMI. This contradiction might be explained in that the latter authors only included cadavers with a PMI of up to 36 h, death by poisoning was not excluded, and the study and control groups were of different sizes and PMI.
Lange et al. [15], using Loess local regression, indicated the increase in VH [K +] not to be linear. However, Madea et al. [2] report that the latter authors’ findings not to have been borne out in independent studies because they only used a Loess curve with a single 95%CI to explain the trends of six large studies covering a wide range of VH [K +]. When applying the same model to their own data, Madea et al. [2] reported it to return many overestimates.
Most papers showed strong correlations in linear regression. It might be thought that any formula might work. However, the same data cannot be used to construct a model and then used to test it [10], and many studies made this mistake. This leads to results that appear better than they really are. Independent datasets are needed to validate a model. However, a Monte Carlo–like analysis can be made. In the studies examined, Cordeiro et al. [7] were the only authors to do this. Generalized additive models carry more weight and improve the 95%CI [45, 47, 48]. The disadvantage is that, being additive, the influence of certain interactions might be lost, making it important to adjust the weight of each variable for Ki correction factors [47].
Discussion continues as to which is the best analytical technique. In 2012, Lendoiro et al. [49] affirmed that HPLC was the best for determining [Hx]. Any pre-treatment of the VH samples should be done when they are fresh; when not possible, samples should be frozen. Frozen samples should be thawed in a refrigerator and then brought to room temperature for analysis; exposure to light should be avoided [50].
The classic technique for measuring VH [K +] is flame emission spectrophotometry. Many studies have mentioned significant differences between the left and right eye when this analyte is measured by indirect or direct potentiometry [13, 23, 28, 51]. New techniques being investigated include capillary electrophoresis with microsamples, which does not have the latter limitations and appears promising [2, 43, 44]. Low-pressure ion chromatography is cheap and widely available and would also appear to be adequate, but further studies are needed [38].
Other analytical tools and sampling methods for VH have also been developed. Risoluti et al. [52] reported thermogravimetric and chemometric techniques to be very accurate when used with either clear or contaminated VH. In addition, they indicated their method, which is claimed requires only a few microlitres of VH and needs no sample pre-treatment, to be capable of predicting PMI to within an hour for recent cadavers. Following this line, they went on to develop a “two-way multiparametric platform” based on inductively coupled plasma–optical emission spectrometry (ICP–OES) and thermogravimetric analysis (TGA), and suggested the P, S, Mg, and the water contents of VH to predict PMI just as well as [K+]; they even reported the range over which estimates could be made as up to 15 days [53]. In another work, Aiello et al. used a matrix-assisted laser desorption mass spectrometry–based method, and an untargeted metabolomics method, to analyse the VH. Using two multivariate statistical strategies (principal component regression and partial least squares regression), they reported R2 = 0.95 for both methods, and a prediction error of 6 h for each when the PMI was < 24 h [54].
Although samples can be collected in different ways, this can lead to large biases and results that differ from what might be expected according to the literature [30]. Nevertheless, obtaining good VH samples becomes difficult when the PMI is more than 30–48 h.
Quantitative methods are rarely used in forensic cases in Galicia as information primarily comes from circumstantial data and cadaveric phenomena. Police and witness information was essential in most of the suspicious cases. PMI was either known or easily determined without the need to use analytical techniques. This might be due to the slow and complex nature of such techniques, a lack of experience in their use, or knowledge of their existence. In most cases, only one method was used to estimate PMI, but, in practical forensic casework, all collectable evidence should be included so that reliable conclusions can be drawn.
To increase the use of quantitative methods, it is necessary to train forensic experts, and systematize data collection. Predictive simple software tools are also needed if the use of quantitative methods is to be promoted.
Conclusions
VH [K +] and [Hx] are good markers for estimating PMI. The disparity in the results in the different papers examined, and the validity of the conclusions with respect to the estimation of PMI, is owed to:
-
1.
The effect of Ta, drugs, differences between the right and left eyes, age, and bodyweight.
-
2.
The use—or not—of gentle puncturing to prevent trauma during sample collection, of adequate pre-treatment, and whether samples were preserved by freezing if they could not be immediately tested.
-
3.
The use of different analytical techniques for the determination of VH [analytes].
-
4.
The non-uniform distribution of known PMIs, and the small number of samples for each PMI time range (especially those > 72 h).
-
5.
The use of different informative variables
VH biochemistry alongside other physical factors provides the best means of establishing a PMI with acceptable error. Advanced regression models provide the most reliable formulae. Cross-validation is, however, needed to validate any model. The search for the “ultimate” means of estimating the PMI continues; proteomics and chemometrics methods might allow a more accurate and faster analysis of VH samples in the future.
In Galicia, most deaths of medico-legal interest were determined to be of cardiovascular origin, followed by asphyxia and traumatic accidents. Quantitative methods were not frequently used to determine the PMI; in most cases, only circumstantial evidence was used, although cadaveric phenomena were often relied upon. If VH biochemistry is to be used in the estimation of PMI, trained personnel, better storage for biological samples, and simple software tools will all be needed. Finally, the present work suggests that the cause of death categories employed by the International Classification of Diseases are too wide to be of use in the forensic research setting.
Key points
This paper provides:
-
1.
A systematic review following PRISMA recommendations.
-
2.
A scientific review of the biochemistry of the vitreous humour and its relationship with the post-mortem interval (PMI).
-
3.
An assessment of the quality of the papers examined using the CASP tool.
-
4.
New perspectives on predictive models for estimating the PMI via VH analyte concentrations and other variables.
-
5.
Past and current analytical methods and regression models for estimating the PMI.
-
6.
A descriptive study on the use made of PMI estimation methods in real forensic practice in Galicia.
References
Madea B, Henssge C. General remarks on estimating the time since death. In: Madea B, editor. Estimation of the Time Since Death. 3rd ed. CRC Press; 2015. p. 1–6.
Madea B. Is there recent progress in the estimation of the postmortem interval by means of thanatochemistry? Forensic Sci Int. 2005;151(2–3):139–149. https://doi.org/10.1016/j.forsciint.2005.01.013.
Sturner WQ, Gantner GE. The postmortem interval. Am J Clin. Pathol. 1964;42:137–144.
Bévalot F, Cartiser N, Bottinelli C, et al. Vitreous humor analysis for the detection of xenobiotics in forensic toxicology: a review. Forensic Toxicol. 2016;34:12–40. https://doi.org/10.1007/s11419-015-0294-5º.
Zilg B, Alkass K, Kronstrand R, Berg S, Druid H. A rapid method for postmortem vitreous chemistry—deadside analysis. Biomolecules. 2022;12(1):32. https://doi.org/10.3390/biom12010032.
Munoz JI, Suarez-Penaranda JM, Otero XL, Rodriguez-Calvo MS, Costas E, Miguens X, Concheiro L. A new perspective in the estimation of postmortem interval (PMI) based on vitreous. J Forensic Sci. 2001;46(2):209–14 (PMID: 11714180).
Cordeiro C, Ordóñez-Mayán L, Lendoiro E, Febrero-Bande M, Vieira DN, Muñoz-Barús JI. A reliable method for estimating the postmortem interval from the biochemistry of the vitreous humor, temperature and body weight. Forensic SciInt. 2018;295:157–168. https://doi.org/10.1016/j.forsciint.2018.12.007.
Zilg B, Bernard S, Alkass K, Berg S, Druid H. A new model for the estimation of time of death from vitreous potassium levels corrected for age and temperature. Forensic Sci Int. 2015;254:158–166. https://doi.org/10.1016/j.forsciint.2015.07.020.
Muñoz Barus JI, Suarez-Penaranda J, Otero XL, Rodríguez-Calvo MS, Costas E, Miguens X, Concheiro L. Improved estimation of postmortem interval based on differential behaviour of vitreous potassium and hypoxanthine in death by hanging. Forensic Sci Int. 2002;125(1):67–74. https://doi.org/10.1016/s0379-0738(01)00616-8.
Rodríguez S, Muñoz Barús JI. La identificación médico legal: utilidad de los metatarsianos y las vértebras cervicales en la estimación del sexo y estatura [PhDThesis]. Universidade de Santiago de Compostela. 2015.
Manterola C, Asenjo-Lobos C, Otzen T. Jerarquización de la evidencia: Niveles de evidencia y grados de recomendación de uso actual. Rev chil infectol. 2014;31(6):705–18.
Critical Appraisal Skills Programme. https://casp-uk.net/casp-tools-checklists/. Accessed 24 Sept 2021.
Zhou B, Zhang L, Zhang G, Zhang X, Jiang X. The determination of potassium concentration in vitreous humor by low pressure ion chromatography and its application in the estimation of postmortem interval. J Chromatogr B. 2007;852(1–2):278–81. https://doi.org/10.1016/j.jchromb.2007.01.027.
Bortolotti F, Pascali JP, Davis GG, Smith FP, Brissie RM, Tagliaro F. Study of vitreous potassium correlation with time since death in the postmortem range from 2 to 110 hours using capillary ion analysis. Med Sci Law. 2011;51(1):S20–3. https://doi.org/10.1258/msl.2010.010063.
Lange N, Swearer S, Sturner WQ. Human postmortem interval estimation from vitreous potassium: an analysis of original data from six different studies. Forensic Sci Int. 1994;66:159–74. https://doi.org/10.1016/0379-0738(94)90341-7.
Krause D, Klein A, Meissner D, Roitzsch E, Herrmann W. Die Bedeutung der Kaliumkonzentrationim Glaskörpermenschlicher Augenfür die Todeszeitbestimmung. Zeitschrift fur Arztliche Fortbildung (Jena). 1971; LE22022300423 65(6):345–8. ISSN/ISBN: 0044–2178.
Adjutantis G, Coutselinis A. Estimation of the time of death by potassium levels in vitreous humor. Forensic Sci Int. 1972;1:55–60. https://doi.org/10.1016/0300-9432(72)90147-1.
Aggarwal RL, Gupta PC, Nagar CK. Determination of time of death by estimating potassium level in the cadaver vitreous humour. Indian J Ophthalmol. 1983;31(5):528–31 (PMID: 6671749).
Devenaux M, Desurmont M, Lenoir L, Muller PH. The measurement of biochemical parameters in the vitreous humor. Their relations. Acta medicinae legalis et socialis. 1985; 2022022300346 35(1):48–58. ISSN/ISBN: 0065–1397.
Madea B, Henssge C, Staak M. Postmortaler Kaliumanstieg in Glaskörperflüssigkeit. Welche Parameter sindals Indikator eneiner vitalen, agonalen Elektrolyt dysregulation geeignet? [Postmortem increase in potassium in the vitreous humor. Which parameters are suitable as indicators of antemortem agonal electrolyte imbalance?]. Z Rechtsmed. 1986;97(4):259–68. German. https://doi.org/10.1007/BF00200605.
Stephens RJ, Richards RG. Vitreous humor chemistry: the use of potassium concentration for the prediction of the postmortem interval. J Forensic Sci. 1987;32(2):503–9 (PMID: 3572343).
Schmidt V, Wischhusen F, Püschel K, Madea B, Henssge C, Hönig W. Kalium konzentration in Glaskörperflüssigkeit—zeitlich versetzte Probenentnahme zur Todeszeitbestimmung [Potassium concentration in the vitreous body--sample collection at different time intervals to determine time of death]. Beitr Gerichtl Med. 1988;46:423–6. German. PMID: 3178692.
Coe JL. Vitreous potassium as a measure of the postmortem interval: an historical review and critical evaluation. Forensic Sci Int. 1989;42(3): 201–213. https://doi.org/10.1016/0379-0738(89)90087-X.
Madea B, Henssge C, Hönig W, Gerbracht A. References for determining the time of death by potassium in vitreous humor. Forensic Sci Int. 1989;40(3):231–43. https://doi.org/10.1016/0379-0738(89)90181-3.
Rognum OT, Hauge S, Øyasaeter S, Saugstad OD. A new biochemical method for estimation of postmortem time. Forensic Sci Int. 1991;51(1): 139–146. https://doi.org/10.1016/0379-0738(91)90214-4.
Gamero JL, Romero JL, Ramos HM, Arufe MI, Vizcaya MA. Precision of estimating time of death by vitreous potassium, comparison of various equations. Forensic Sci Int. 1992;56(2):137–45. https://doi.org/10.1016/0379-0738(92)90171-R.
Madea B, Käferstein H, Hermann N, Sticht G. Hypoxanthine in vitreous humor and cerebrospinal fluid--a marker of postmortem interval and prolonged (vital) hypoxia? Remarks also on hypoxanthine in SIDS. Forensic Sci Int. 1994;65(1):19–31. https://doi.org/10.23907/2016.002.
Mulla A, Massey KL, Kalra J. Vitreous humor biochemical constituents: evaluation of between-eye differences. Am J Forensic Med Pathol. 2005;26(2):146–9 (PMID: 15894848).
Madea B, Rödig A. Time of death dependent criteria in vitreous humor: accuracy of estimating the time since death. Forensic Sci Int. 2005;164(2–3):87–92. https://doi.org/10.1016/j.forsciint.2005.12.002.
Chandrakanth VH, Kanchan T, Balaraj BM, Virupaksha HS, Chandrashekar TN. Postmortem vitreous chemistry–an evaluation of sodium, potassium and chloride levels in estimation of time since death (during the first 36 h after death). J Forensic Leg Med. 2013;20(4):211–6. https://doi.org/10.1016/j.jflm.2012.09.001.
Mihailovic Z, Atanasijevic T, Popovic V, Milosevic MB, Sperhake JP. Estimation of the postmortem interval by analyzing potassium in the vitreous humor: could repetitive sampling enhance accuracy? Am J Forensic Med Pathol. 2012;33(4):400–3. https://doi.org/10.1097/PAF.0b013e31826627d0.
Hassan NAM, El-Dakroory SA. A correlation study between postmortem interval estimation and vitreous potassium level. Mansoura J Forensic Med Clin Toxicol. 2013;21(2): 1–14. https://doi.org/10.21608/mjfmct.2013.47671.
Tumram N, Ambade V, Dongre A. Thanatochemistry: study of vitreous humor potassium. Alexandria Journal of Medicine. 2014;50(4):365–8. https://doi.org/10.1016/j.ajme.2013.12.002.
Swain R, Kumar A, Sahoo J, Lakshmy R, Gupta SK, Bhardwaj DN, Pandey RM. Estimation of post-mortem interval: a comparison between cerebrospinal fluid and vitreous humour chemistry. J Forensic Leg Med. 2015;36:144–8. https://doi.org/10.1016/j.jflm.2015.09.017.
Rognum TO, Holmen S, Musse MA, Dahlberg PS, Stray-Pedersen A, Saugstad OD, Opdal SH. Estimation of time since death by vitreous humor hypoxanthine, potassium, and ambient temperature. Forensic Sci Int. 2016;262:160–5. https://doi.org/10.1016/j.forsciint.2016.03.001.
Ortmann J, Markwerth P, Madea B. Precision of estimating the time since death by vitreous potassium-comparison of 5 different equations. Forensic Science Intrnational. 2016;269:1–7. https://doi.org/10.1016/j.forsciint.2016.10.005.
Jashnani KD, Kale SA, Rupani AB. Vitreous humor: biochemical constituents in estimation of postmortem interval. J Forensic Sci. 2010;55(6):1523–7. https://doi.org/10.1111/j.1556-4029.2010.01501.x.
Tatiya HS, Kulkarni DG, Punpale SB. Utility of vitreous potassium concentration to estimate time since death. Indian Journal of Basic and Applied Medical Research. 2016;6:567–75.
Srettabunjong S, Thongphap W, Chittamma A. Comparative and correlation studies of biochemical substances in vitreous humor and synovial fluid. J Forensic Sci. 2019. https://doi.org/10.1111/1556-4029.13966.
Go A, Shim G, Park J, Hwang J, Nam M, Jeong H, Chung H. Analysis of hypoxanthine and lactic acid levels in vitreous humor for the estimation of post-mortem interval (PMI) using LC-MS/MS. Forensic Sci Int. 2019;299:135–141. https://doi.org/10.1016/j.forsciint.2019.03.024.
Saldaña Sánchez ML, Amésquita Cárdenas ML, Hilario Vargas JS, Paredes Julca A. Concentraciones de Hipoxantina, Urea y Potasio del Humor Vítreo y su correlación con el intervalo post mórtem. [PhD Thesis]. Universidad Nacional de Trujillo. 2019.
Garland J, Olds K, Rousseau G, Palmiere C, Ondruschka B, Kesha k, Glenn C, Morrow P, Stables S, Tse R. Using vitreous humour and cerebrospinal fluid electrolytes in estimating post-mortem interval - an exploratory study. Aust J Forensic Sci. 2020;6(52):626–633. https://doi.org/10.1080/00450618.2019.1642956.
Focardi M, Lanzilao L, Bonari A, Lazzeretti M, Lorubbio M, Ognibene A, Gualco B, Fanelli A, Pinchi V. Improvement in estimation of time since death by albumin and potassium concentrations in vitreous humor. Forensic Sci Int. 2020;314: 110393. https://doi.org/10.1016/j.forsciint.2020.110393.
Palacio C, Gottardo R, Cirielli V, Musile G, Agard Y, Bortolotti F, Tagliaro F. Simultaneous analysis of potassium and ammonium ions in the vitreous humour by capillary electrophoresis and their integrated use to infer the post mórtem interval (PMI). Med Sci Law. 2020;61:96–104. https://doi.org/10.1177/0025802420934239.
Muñoz-Barús JI, Rodríguez-Calvo MS, Suárez-Peñaranda JM, Vieira DN, Cadarso-Suárez C, Febrero-Bande M. PMICALC: a R code-based software for estimating post-mortem interval (PMI) compatible with Windows, Mac and Linux operating systems. Forensic Sci Int. 2010;194(1–3):49–52. https://doi.org/10.1016/j.forsciint.2009.10.006.
O.M.S. CIE-10. Trastornos Mentales y del Comportamiento. Décima Revisión de la Clasificación Internacional de las Enfermedades. Descripciones Clínicas y pautas para el diagnóstico. Organización Mundial de la Salud, Ginebra. 1992. ISBN: 978–84–340–2438–0.
Gil C. Métodos de regresión no lineal. 2018. https://rpubs.com/Cristina_Gil/Regr_no_lineal. Accessed 24 Sept 2021.
Muñoz Barús JI, Febrero-Bande M, Cadarso-Suárez C. Flexible regression models for estimating postmortem interval (PMI) in forensic medicine. Stat Med. 2008;27(24):5026–38. https://doi.org/10.1002/sim.3319.
Lendoiro E, Cordeiro C, Rodríguez-Calvo MS, Vieira DN, Suárez-Peñaranda JM, López-Rivadulla M, Muñoz-Barus JI. Applications of tandem mass spectrometry (LC-MSMS) in estimating the post-mortem interval using the biochemistry of the vitreous humour. Forensic Sci Int. 2012;223(1–3):160–4. https://doi.org/10.1016/j.forsciint.2012.08.022.
Trincado-Ave M, Ordóñez-Mayán L, Camiña M, Febrero-Bande M, Muñoz-Barús JL. Estimation of the post-mortem interval: effect of storage conditions on the determination of vitreous humour [K+]. Sci Justice. 2021;61(5):597–602. https://doi.org/10.1016/j.scijus.2021.07.005.
Cutamora E, Parmisana A. Flame photometer and direct ion-selective electrode on serum sodium and potassium concentration. Asian J Health. 2015;5(10). ISSN: 2244–047X.
Risoluti R, Gullifa G, Fineschi V, Frati P, Materazzi S. Application of innovative TGA/chemometric approach for forensic purposes: the estimation of the time since 53 death in contaminated specimens. Diagnostics (Basel). 2021;14; 11(1):121. https://doi.org/10.3390/diagnostics11010121.
Risoluti R, Canepari S, Frati P, Fineschi V, Materazzi S. “2n analytical platform” to update procedures in thanatochemistry: estimation of post mortem interval in vitreous humor. Anal Chem. 2019;91(11):7025–31. https://doi.org/10.1021/acs.analchem.9b01443.
Aiello D, Lucà F, Siciliano C, Frati P, Fineschi V, Rongo R, Napoli A. Analytical strategy for MS-based thanatochemistry to estimate postmortem interval. J Proteome Res. 2021;20(5):2607–17. https://doi.org/10.1021/acs.jproteome.0c01038.
Funding
This study was supported by a grant from Xunta de Galicia – Spain [Proxectos Plan Galego IDT (ED431C 2021/35). The research by Manuel Febrero – Bande has been partially supported by the Spanish Grant PID2020-116587 GB-I00 funded by MCIN/AEI/10.13039/501100011033 through the European Regional Development Funds (ERDF).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the ethics committee of the University of Santiago de Compostela (USC-19/2020) and was carried out in compliance with the legal and ethical requirements (Spanish Acts 14/2007 and 3/2018).
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Da Cunha, E.C., Ordóñez-Mayán, L., Vázquez, M.L.R. et al. The biochemistry of the vitreous humour in estimating the post-mortem interval—a review of the literature, and use in forensic practice in Galicia (northwestern Spain). Forensic Sci Med Pathol 19, 236–265 (2023). https://doi.org/10.1007/s12024-022-00539-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12024-022-00539-5