Abstract
A fatality of an inpatient ingesting a disinfectant containing ethanol, propan-1-ol, and propan-2-ol is reported. The alleged survival time was about 1 h. Major findings at autopsy were an extended hemorrhagic lung edema, an edematous brain, and shock kidneys. Concentrations of alcohols and acetone, a major metabolite of propan-2-ol, were determined from body fluids (blood from the heart and the femoral vein, urine, gastric contents) and tissues (brain, muscle, liver, kidneys, lungs) by headspace/gas chromatography using 2-methylpropan-2-ol as the internal standard. All samples investigated were positive for propan-1-ol, propan-2-ol, ethanol, and acetone except stomach contents, where acetone was not detectable. The low concentration of acetone compared to propan-2-ol likely supports the short survival time. The concentration ratios estimated from the results are in accordance with the physico-chemical properties of the particular alcohols, their different affinities towards alcohol dehydrogenase as well as their interdependence during biotransformation. Autopsy did not reveal the cause of death. According to the few published data, blood concentrations of 1.44 and 1.70 mg/g of propan-2-ol and propan-1-ol, respectively, are considered sufficient to have caused the death. This case also points to the need to restrict access to antiseptic solutions containing alcohols in wards with patients at risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Consistent with the epidemiological evidence, alcohol is by far the most common drug seen in completed suicides and accidental deaths [1, 2]. However, life-threatening intoxications with long-chain alcohols have been reported very rarely. Dürwald and Degen [3] presented a death case caused by propan-1-ol in 1956; Wirth and Gloxhuber [4] published a fatality due to 2-methyl-butan-1-ol in 1994. A few cases involved poisoning with propan-2-ol [5, 6], and only three cases reported on a mixed intoxication with propan-2-ol and propan-1-ol [5, 7, 8].
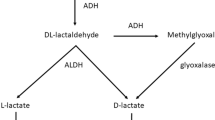
Propan-2-ol is a colorless, flammable liquid being used for industrial and pharmaceutical processes, in household and personal care products as well as in antiseptic formulations [7]. If swallowed, propan-2-ol is rapidly absorbed within 15 to 30 min and is metabolized via liver alcohol dehydrogenase (ADH) to form acetone by 80–90 % being detectable at about 30 min post-ingestion [9]. Exhalation via the lungs is a minor route of elimination compared to metabolism and excretion in urine. In humans, the half-life of propan-2-ol ranges between 2.5 and 8.0 h; that of acetone averages about 22 h [10]. Ethanol and propan-1-ol prolong the elimination of propan-2-ol due to their higher affinity towards ADH. Both acetone and propan-2-ol are assumed being liable for the toxic effects [8]. Although propan-2-ol is not considered as toxic as methanol, ingestion of about 150 to 240 mL may be life-threatening [10].
Propan-1-ol is a colorless, volatile, flammable liquid which is used for paints and as a cleaning and disinfection solution [5]. The unchanged alcohol is partly excreted via the lungs and the kidneys. In man, propan-1-ol is metabolized by the same enzyme activities as ethanol. Propanal is thus converted to propionic acid, which may enter the citric acid cycle as a coenzyme A conjugate [7]. A small amount of propan-1-yl glucuronide and sulfate may also be formed. Although data on the elimination half-life of propan-1-ol in man are not available, it was suggested to be lower than that of propan-2-ol [8]. While propan-1-ol is considered less toxic than ethanol, the reverse has been attributed to their aldehydes [11].
We present a case of a mixed propan-1-ol and propan-2-ol intoxication where death occurred within approximately 1 h after ingestion of about 1 L of an antiseptic solution. Concentrations of all three alcohols as well as of acetone have been determined from body fluids and, for the first time, in tissues.
Case report
The inpatient (21 years, female) suffered from a borderline personality disorder for many months. Her medical treatment comprised zolpidem in the evening as well as pipamperone and olanzapine. On the day of her death, she was seen alive last at lunchtime. About 1 h later, the nurse noticed that she was lifeless. Although being started immediately, attempts at resuscitation failed. In the bathroom of the patient, an empty bottle was detected, previously having contained 1 L of an antiseptic formulation consisting of 450 mg propan-1-ol, 250 mg propan-2-ol, and 47 mg ethanol per gram, respectively.
An autopsy was conducted 4 days later. The mucosa of the esophagus, the trachea, and the stomach were corroded, appearing like tanned leather. This appearance raised a first, yet strong suspicion that an irritant, denaturizing agent may have been swallowed. Further major findings were an extensive hemorrhagic lung edema with blood also covering the peripheral lung vessels, an edematous brain, and shock kidneys. Preexisting diseases of the internal organs that might have caused or contributed to death were absent.
Materials and methods
Materials
Acetone (≥99.8 %), propan-1-ol (≥99.5 %), propan-2-ol (≥99.9 %), and 2-methylpropan-2-ol (≥99.5 %) were from Roth (Karlsruhe, Germany). Ethanol standard solutions were supplied from Diasys Diagnostic Products (0.5, 1.0, 2.0, 3.0, and 4.0 mg/mL; Holzheim, Germany) and Medichem (0.2 mg/mL; Steinenbronn, Germany). Bi-distilled water was from Braun (Melsungen, Germany).
Samples analyzed for alcohols and acetone were blood from the femoral vein and the heart cavities, urine, stomach contents (30 mL in total), brain, lung, liver, kidney, and muscle. Aliquots of these samples were taken at autopsy, immediately transferred into headspace vials with Teflon-lined seals, and frozen at −20 °C.
Methods
A urine aliquot was screened for abused drugs such as amphetamine and derivates, benzodiazepine tranquilizers, cannabinoids, cocaine, opiates, and methadone (Cedia DAU®, Thermo Scientific, Passau, Germany; Olympus AU 400®, Beckman Coulter, Krefeld, Germany). General unknowns on basic, neutral, and acidic drugs following solid-phase extraction of urine and stomach contents were performed by gas chromatography/mass spectrometry (GC/MS). With regard to final results, hydrolysis of the urine sample or derivatization prior to analysis has not been performed. Confirmation and quantitation of identified drugs in blood taken from the femoral vein was by GC/MS (pipamperone, zolpidem) and by liquid chromatography/tandem mass spectrometry (olanzapine) using validated in-house procedures.
Propan-1-ol and propan-2-ol, ethanol, and acetone were determined by headspace/gas chromatography equipped with a flame ionization detector (Autosystem XL® gas chromatograph; Turbo Matrix® 100 headspace sampler; Perkin Elmer, Überlingen, Germany). Frozen body fluids and frozen tissues were chopped within the ice-cold vials and weighed into new ice-cold headspace vials (ca. 0.20 g for ethanol, and 1.00 g for propan-1-ol, propan-2-ol, acetone); bi-distilled water was added to samples (1:2 by mass) and stomach contents (1:9 by mass), as well as the internal standard (0.50 mg/g). Headspace vials were tightly capped again with Teflon-lined crimp seals within 60 s at the longest. Each specimen was measured twice. Following equilibration (12 min), samples were eluted from a packed wide-bore column isothermally at 95 °C (Carbowax 15 on Carbopack 60/80 mesh, 1.0 m · 3 mm; Grace, Worms, Germany). Data acquisition and analysis were performed using Totalchrom® workstation version V6.3.2 (Perkin Elmer, Überlingen, Germany).
A blank sample was inserted between each specimen to check for carryover. A four-point calibration curve was prepared at 0.25, 0.50, 0.75, and 1.00 mg of propan-1-ol, propan-2-ol, and acetone, respectively/gram blank blood or liver with alcohols being not detectable in these specimens. For determination of ethanol, the commercially available standards have been used. Quality control samples (QC) for propan-1-ol, propan-2-ol, ethanol, and acetone covered concentrations of 0.40 and 0.80 mg/g (QClow, QChigh, blood, and liver, respectively), respectively. A blank (matrices processed without internal standard) and a zero sample (matrices processed with internal standard) were also included.
Calibration curves were assessed for linearity by least square regression analysis; respective lower limits of detection and quantitation (LLOD, LLOQ) were derived from calibration lines according to DIN 32645 [12]. The assay was linear down to the estimated LLOQ for each analyte. If a concentration at or above the highest calibration standard was measured, the respective sample was re-analyzed using a smaller amount. Selectivity was examined by testing blank blood from six different sources for interference with the analytes and the internal standard. Intraday imprecision and interday imprecision were related to five measurements of each QC sample; accuracy has been determined from eight replicates of QClow and QChigh; data analysis was performed using software Valistat 2.0 [13].
Results
Testing urine by immunoassay for commonly abused drugs was negative; general unknown analyses identified zolpidem and pipamperone in gastric contents and urine, where olanzapine was detectable in addition. Confirmation in blood from the femoral vein revealed 22 ng zolpidem/mL, 252 ng pipamperone/mL, and 229 ng olanzapine/mL.
Ethanol, acetone, propan-2-ol, propan-1-ol, and 2-methylpropan-2-ol eluted at 0.36, 0.43, 0.56, 0.72, and 0.90 min, respectively, achieving baseline separation (Fig. 1). The total run time was 2 min. There was no carryover between samples. No interference with the analytes or the internal standard was present at respective retention times. Validation data for whole blood are summarized in Table 1; those for liver did not significantly differ (data not shown). Blank liver was used as a model tissue; interfering or additional peaks were not detectable from other tissue samples.
All samples investigated in the presented case were positive for propan-1-ol, propan-2-ol, ethanol, and acetone except stomach contents, where acetone could not be detected (Table 2).
Discussion
To our knowledge, this is the first case report of tissue concentrations following a mixed intoxication with propan-1-ol, propan-2-ol, and ethanol. The significantly higher concentrations in heart blood compared to femoral venous blood may suggest that absorption had not been complete at the time of death. Aspiration of the liquid and subsequent diffusion of the alcohols into the heart cavities might be a further potential explanation. The short survival time is also reflected by the small amount of acetone determined from the kidney and urine samples. The concentration of ethanol, propan-2-ol, and propan-1-ol measured in urine, kidney, and muscle tissue mirrors most widely the proportion of the three alcohols present in the antiseptic solution. Virtually the same concentration of propan-1-ol and propan-2-ol was present in liver tissue in accordance with the delayed metabolism of propan-2-ol if ethanol and propan-1-ol are present. The highest concentrations could be determined from the lungs. The proportion of the three alcohols determined from the lung specimen largely differs from that being present in the antiseptic solution. Although clearance of alcohols and acetone with the breathing air may vary depending on the particular vapor pressure of ethanol, propan-2-ol, and propan-1-ol [14], this minor route of elimination does not account for this difference. Results also suggest that the more lipophilic propan-1-ol enters the brain more readily compared to ethanol and propan-2-ol.
At present, only three cases involving a mixed intoxication with propanols and only one fatal case following ingestion of propan-1-ol have been published [3, 5–9]. This case is also one of few reporting autoptic findings [3]. Liquid cadaver blood, an extensive, hemorrhagic lung edema, and frothy, blood-stained fluid in the bronchia were the most important observations at autopsy. Although uncharacteristic, these findings are in line with those observed in the presented case. Propan-1-ol could be identified from intestinal contents following distillation and derivatization with 4-nitrobenzoic acid to form crystals of the propylester. Quantitation of the alcohol was not feasible; the amount ingested was estimated at 400–500 mL. The authors suggested propan-1-ol to be more effective than ethanol, causing loss of consciousness at a lower dose compared to ethanol.
The acceptable daily intake of propan-1-ol has been estimated to range from 3.0 to 14 mg/kg; after consumption of alcoholic beverages, its concentration does not exceed 2.0 μg/mL blood. The potency of aliphatic alcohols assumingly increases with their molecular mass, and propan-1-ol was estimated to be about three times as toxic as ethanol. However, this assumption, also called Richardson’s law, appears to be valid only to primary effects when formation of propanal and propionic acid is still insignificant [11].
Far more cases have been reported on propan-2-ol poisoning [8, 15, 16]. Propan-2-ol toxicity presented with drowsiness, confusion, slurred speech, hypotension, respiratory depression, and coma; formation of acetone results in ketosis and ketonuria [9]. Autoptic findings in a fatal case revealed hemorrhage due to erosion of the mucous membranes of the stomach and the small intestine, subepicardial bleeding, congestion of the internal organs, shock kidneys as well as edema of the lungs and the brain. Concentrations of propan-2-ol and acetone determined from a femoral venous blood specimen by headspace/gas chromatography were 3.15 and 0.47 mg/g, respectively. Survival time was grossly estimated at 2–3 h post-ingestion; the marked shock syndrome, however, suggested an agonal phase lasting for several hours [15]. Currently, there is conflicting evidence with regard to propan-2-ol’s toxicity. Megabarne and Villa [9] suggested propan-2-ol to be twice as toxic as ethanol with regard to central nervous depression. This assumption was based on animal studies as well as on the combined toxicity of propan-2-ol and acetone. Nevertheless, the toxicity of acetone remains controversial [17]. Clark [18] considered propan-2-ol to be two- to threefold more potent than ethanol without giving particulars. Slaughter et al. [10] suggested propan-2-ol not to be as toxic as ethanol or methanol for the following reason: unlike these two alcohols, propan-2-ol does not cause an anion gap acidosis; however, it produces an osmolal gap between calculated and measured osmolaties in serum. Generally, toxicity seems to decrease from primary to secondary alcohols [11].
In mixed intoxications with propanols, symptoms similar to those summarized above have been observed. The case report of Vujasinovic et al. [7] showed respiratory insufficiency and ataxia on admittance followed by unconsciousness and respiratory arrest. Investigations revealed an empty bottle of a hand disinfectant containing about 130 mL propan-1-ol and 300 mL propan-2-ol. The concentrations of propanols and acetone have not been determined from body fluids. During the first 12 h, the patient developed mixed acidosis; ketonuria appeared only after 12 h whereas after isolated propan-2-ol ingestion, peak serum concentrations of acetone were already observed within 4 h. Blanchet et al. [8] reported a case following ingestion of a hand disinfectant solution containing 80 g propan-2-ol and 54 g propan-1-ol, respectively, two times at an interval of about 24 h. The patient did not present with severe symptoms of poisoning. Plasma concentrations at 8 h after the second intake were 0.37 mg/mL propan-2-ol and 2.27 mg/mL acetone, whereas propan-1-ol was no longer detectable at a detection limit <0.1 mg/mL. The analytical finding reflects both the delayed metabolism of propan-2-ol and accumulation of acetone due to its longer half-life compared to propan-2-ol. A known alcoholic was admitted to the hospital as an emergency with propan-1-ol and propan-2-ol concentrations of 1.8 and 1.5 mg/mL, which rapidly dropped to <0.2 and 0.9 mg/mL, respectively, within 1 h following hemodialysis [5]. At present, immediate hemodialysis is the therapy of choice.
Concentrations above 1.25 mg propan-2-ol/g serum are considered to be associated with significant toxicity [5, 19]. On the assumption that propan-1-ol is not less toxic than propan-2-ol, the death in the presented case can be attributed to propan-1-ol and propan-2-ol poisoning. Acetone and ethanol findings can be assessed as ineffective which also applies to the zolpidem level. The pipamperone concentration was within the therapeutic range, whereas olanzapine was highly dosed. Therefore, it cannot be excluded that olanzapine may have contributed to a slight extent to the central nervous depression in addition to propan-1-ol and propan-2-ol.
There is no doubt that on-site availability of disinfecting agents largely improves hygiene compliance [20]. However, placing such bottles inside a patient’s room is associated with two risks: (a) disinfecting solutions are ignitable products and (b) they may be swallowed accidentally or in a suicide attempt in units or wards caring for children, patients with alcohol-related disorders, and demented or psychiatric patients. The possibilities to minimize such risks may include the use of small-sized or secured bottles or their placement outside the patient’s reach.
References
Darke S, Duflou J, Torok M, Prolov T (2013) Characteristics, circumstances and toxicology of sudden or unnatural deaths involving very high-range alcohol concentrations. Addiction 108:1411–1417
Below E, Lignitz E (2003) Cases of fatal poisoning in post-mortem examination at the Institute of Forensic Medicine in Greifswald—analysis of five decades of post-mortems. Forensic Sci Int 23:125–131
Dürwald W, Degen W (1956) Eine tödliche Vergiftung mit n-Propylalkohol. Arch Toxikol 16:84–88
Wirth W, Gloxhuber C (1994) Toxikologie, 4th edn. Thieme, Stuttgart
Koball S, Schipper J, Hinz M (2011) Mischintoxikationen mit Propanol und Ethanol. Intensivmed 48:439–442
Steinmann D, Faber T, Auwärter V, Heringhaus C (2009) Akute Intoxikation mit Isopropanol. Anaesthesist 58:149–152
Vujasinovic M, Kocar M, Kramer K, Bunc M, Brvar M (2007) Poisoning with 1-propanol and 2-propanol. Hum Exp Toxicol 26:975–978
Blanchet B, Charachon A, Lukat S, Huet E, Hulin A, Astier A (2007) A case of mixed intoxication with isopropyl alcohol and propan-1-ol after ingestion of a topical antiseptic solution. Clin Toxicol 45:701–704
Megabarne B, Villa A (2010) Poisoning with ethanol and 2-propanol-based hand rubs: give Caesar what belongs to Caesar! Neurocrit Care. doi:10.1007/s12028-010-9353-2
Slaughter RJ, Mason RW, Beasly DM, Vale VA, Schep LJ (2014) Isopropanol poisoning. Clin Toxicol 52:470–478
Lachenmeier DW, Haupt S, Schulz K (2008) Defining maximum levels of higher alcohols in alcoholic beverages and surrogate alcohol products. Regul Toxicol Pharmacol 50:313–321
Deutsches Institut für Normung. DIN 32645 (1999) Chemische Analytik – Nachweis-, Erfassungs- und Bestimmungsgrenze. Beuth, Berlin, Germany, pp 3–10
Schmitt G, Herbold M, Peters F (2011) Valistat—software for method validation in forensic toxicology. Toxichem Krimtech 78:392–395
Sunshine I (1969) Handbook of analytical toxicology. The Chemical Rubber, Cleveland
Petkovits T, Bohn G, Brinkmann B (1989) Rechtsmedizinische und toxikologische Aspekte bei Propanol-2-Intoxikationen. Z Rechtsmed 102:69–75
Baselt RC (2011) Disposition of toxic drugs and chemicals in man, 9th edn. Biomedical Publications, Seal Beach
Papa AJ (2005) Propanols. Ullmann’s encyclopedia of industrial chemistry. Wiley VCH, Weinheim
Clark JD (2010) Isopropyl alcohol intoxication. Pharm/Tox Corner. doi:10.1016/j.jen.2009.10.006
Schulz M, Schmoldt A (2003) Therapeutic and toxic blood concentrations of more than 800 drugs and other xenobiotics. Pharmazie 58:447–474
Tavolacci MP, Marini H, Vanheste S, Merle V, Coulon AM, Micaud G, Czernichow P (2007) A voluntary ingestion of alcohol-based hand rub. J Hosp Infect 66:86–87
Acknowledgments
The authors greatly acknowledge the technical assistance of Ms. B. Neureither.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Skopp, G., Gutmann, I., Schwarz, CS. et al. An unnatural death by propan-1-ol and propan-2-ol. Int J Legal Med 130, 975–980 (2016). https://doi.org/10.1007/s00414-015-1302-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-015-1302-3