Abstract
Objectives
Ventilated postmortem computed tomography (vPMCT) is associated with improved pulmonary imaging compared to standard PMCT in adults. We aimed to evaluate the feasibility of performing ventilated PMCT in children.
Methods
Postmortem thoracic CT was performed before (PMCT) and after ventilation (vPMCT). We used a range of mouthpieces, including endotracheal tubes, bag and mask and laryngeal mask airway (LMA). Hounsfield units of the lungs at PMCT were measured for normal and abnormal lung areas, before and after ventilation. All patients underwent full conventional autopsy and histology.
Results
Twelve patients underwent ventilated PMCT, median age 52 days (range 3–304 days). Ventilated PMCT provided diagnostic lung images in all 12 cases, compared to only three unventilated PMCT examinations (p < 0.005). In all cases, ventilated PMCT improved the image quality of aerated lungs irrespective of the method used. Average lung Hounsfield units decreased significantly with ventilation from pre-vPMCT values (−134.1 ± 215.1 vs post-vPMCT −531.8 ± 190.1; p < 0.001). LMA with continuous positive pressure ventilation subjectively provided the best results.
Conclusion
Ventilated PMCT significantly improves lung aeration in children and can aid recognition of areas of abnormality in paediatric lungs. Such advances will improve accuracy and uptake of imaging-assisted autopsies in children.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Postmortem imaging now plays a significant role in the paediatric and perinatal less invasive autopsy, with postmortem magnetic resonance imaging (PMMR) demonstrating high overall diagnostic accuracy [1]. However, accuracy is greater for some organs than others, with postmortem changes in the lungs in particular being difficult to distinguish from pathology; pneumonia in particular is both over- and under-diagnosed on paediatric PMMR [2].
Postmortem computed tomography (PMCT) has not been evaluated in detail in this regard, since in general, PMCT typically provides a lower diagnostic yield in children for several reasons. As PM imaging examinations are acquired in natural expiration which increases pulmonary opacification, together with normal postmortem changes (inner lividities), this can make the lungs appear densely opaque and imaging diagnostically uninterpretable.
There is now interest in expanding the lungs at postmortem in adult cadavers, using ventilation-assisted CT. Germerott et al. published the first description of using ventilation during PMCT (vPMCT), which other groups have now adopted [3–7]. They used a ventilator to give continuous positive pressure ventilation, effectively mimicking a breath-hold in inspiration during imaging, although gastric dilatation was a complication. Robinson et al. have recently shown that by ventilating adult lungs during postmortem CT using a supraglottic airway and clinical portable ventilator, significant lung expansion and reduction in lung density was achieved, with an overall improvement in diagnostic yield for thoracic pathology [5].
Here, we evaluated vPMCT in the paediatric setting to determine whether this was feasible in this patient population and whether the technique was associated with improvement in imaging appearances in children. All patients underwent conventional autopsy and histology to verify the imaging findings.
Methods
Study design and population
vPMCT was performed in patients for whom parental consent for conventional autopsy including imaging was available. Inclusion criteria were documentation of prior spontaneous lung inflation in life, and therefore, we excluded all foetuses, stillbirths or perinatal deaths where there was any doubt. All cases underwent two thoracic CT examinations (pre-PMCT and vPMCT using a ventilator). Five cases were scanned twice following ventilation, with an additional intermediate vPMCT (‘first stage’) following artificial breaths using a conventional paediatric self-inflating resuscitation bag and then a second stage using a ventilator.
Imaging protocols
All bodies were stored in standard mortuary refrigeration units at 4 °C before postmortem imaging. Whole-body PMCT imaging was performed on a 64-slice multidetector system (Siemens SOMATOM Definition; Siemens Healthcare, Erlangen, Germany). All patients were examined using our standard PMCT protocol which consists of brain PMCT imaging at contiguous 1 mm axial slice thickness with 5 mm gap at 120 kV and variable milliamps, followed by volumetric whole-body PMCT from the vertex down to the toes at 120 kV with variable milliamps, a pitch of 1 and 0.625 mm collimation.
Airway
Some children had been unsuccessfully resuscitated prior to death and had an appropriately sized endotracheal (ET) tube in situ. We attempted to use this where possible, but there was a significant leak around the ET tube, and gastric dilatation occurred in two patients almost immediately. These were therefore removed to allow other airway access to be attempted.
In some cases (n = 5), a two-stage ventilation procedure was employed. A conventional paediatric self-inflating resuscitation bag (Lifesaver® Disposable Manual Resuscitator; Teleflex, Buckinghamshire, UK) with an added filter was used to give several inflation breaths, until the chest was seen to inflate fully, and the CT thorax was repeated (‘first stage’; Table 1).
The second stage in some patients (n = 5), and the only technique tried in the majority of patients (n = 7), was to use a ventilator to generate continuous positive end expiratory pressure (PEEP) in an attempt to maintain chest wall height for the duration of the scan, to evaluate whether PEEP was necessary for good results. For this, we inserted a supraglottic single-use Integral Silicone Laryngeal Mask airway (Fannin UK Ltd, Wellingborough, Northamptonshire, UK), which is in routine clinical use in our hospital. A radiologist with neonatal intubation experience performed the insertion (OJA), with a laryngeal mask airway (LMA) tube size selected appropriate to the weight of the patient (e.g. size 1.5, 5–10 kg; size 2, 11–20 kg, etc.). The LMA was lubricated with water-soluble lubricant and then inserted into the mouth with the neck in an extended position until resistance was met at the entrance to the airway. Inflation of the cuff provided confirmation of appropriate location, as well as giving airway stability and obscuring the oesophagus. Correct position was checked by palpation of the anterior neck and confirmed on CT imaging. The thoracic CT was repeated with the chest fully mechanically inflated.
Image reporting
Images were reconstructed with a mediastinal, lung and bone algorithm to provide 5 and 1 mm slice thicknesses and viewed on standard soft tissue, lung and bone window settings. Further 3D reconstruction of the body was performed on an Apple Mac workstation using Osirix MD software (Pixmeo, Switzerland; open source code; http://www.osirix-viewer.com). Conventional reporting of PMCT was performed according to normal clinical institutional standards by a single paediatric radiologist with 8 years of radiology experience and 3 years of postmortem imaging experience (OJA), blinded to the autopsy findings, which were only revealed at the end of the study. In addition, images were recorded as being diagnostic or non-diagnostic (normal or abnormal lung parenchyma could not be distinguished by the reporter), and the Hounsfield units (HU) of lung parenchyma in the densest and least dense areas were measured using a 1-cm region of interest. Lung volumes were not measured as they could not be accurately identified in all pre-ventilated cases.
Autopsy
All cases subsequently underwent full autopsy with standard routine histological lung sampling, performed by one of two experienced perinatal/paediatric pathologists (LK, NJS; 8–27 years of experience) in accordance with national guidelines [8]. All organs (heart, lungs, liver, etc.) were routinely examined in the unfixed state, and tissue samples obtained from all major organs for subsequent histological examination using routine haematoxylin and eosin staining. Autopsy findings were reported with all clinical information available including pre-vPMCT findings (e.g. fractures, intracranial changes), but vPMCT findings were not yet revealed.
Statistical analysis
Primary outcomes were diagnostic or non-diagnostic imaging, pre- and postventilation and change in Hounsfield units following ventilation. Results are presented using mean percent changes and standard deviation of the mean. SPSS (Version 19 for Macintosh, SPSS Inc., IBM, NY, USA) was used for data analysis, using Student’s paired t test (or chi-squared test to test between proportions) at the p < 0.05 significance level. Preliminary sensitivity and specificity data with 95 % confidence intervals (CIs) were obtained.
Results
Demographics
Twelve patients underwent vPMCT, median age 52 days (range 3–304 days), consisting of six males and six females. Full demographic details are provided in Table 1.
Airways and complications
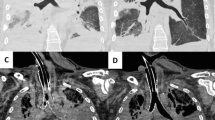
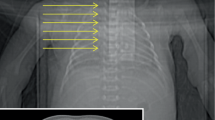
Two cases (cases 1 and 4) had ET tubes in situ, which had been placed during resuscitation prior to demise. In both of these cases, there was a leak around the tip of the airway and air was seen to distend the stomach following ventilation, and thus, they were replaced by LMAs. LMAs were successfully introduced in all patients and used for all subsequent vPMCT attempts. An LMA airway, compared to an ET tube, produced an adequate seal around the epiglottis and airway which prevented air from entering the stomach and bowel (Fig. 1). Using the LMA, no patient needed a nasogastric tube passing to reduce gastric or bowel distension. However, there were two cases of pneumothorax after PEEP vPMCT (Table 1; Fig. 2).
There were no differences between left and right lung values pre-vPMCT (overall mean −134.1 ± 215.1; left lung −122.9 ± 210.1 vs right lung −145.3 ± 228.8; p = 0.81) nor post-vPMCT (overall mean −531.7 ± 190.1; left lung −539.6 ± 180.6 vs right lung −523.9 ± 207.0; p = 0.85), and therefore, we used mean values from both normal lungs (n = 24) for further comparisons to identify the effects of ventilation.
Diagnostic PMCT and lung abnormalities
Seventy-five percent (9/12) of examinations were judged non-diagnostic (typically a ‘white-out’) prior to ventilation, compared to 100 % (12/12) judged diagnostic following ventilation (p < 0.005; Fig. 3). We were unable to distinguish between normal and abnormal lung areas on the basis of HU on the conventional PMCT images as most were non-diagnostic. Seven patients had lung parenchymal abnormalities identified on vPMCT images, although only four of these had these abnormalities confirmed at autopsy. On pre-vPMCT images, mean HU for normal lungs (−134.1 ± 215.1) were lower (more aerated) but not significantly different from abnormal lungs (−45.3 ± 135.2; p = 0.22; Fig. 4). We did not find a relationship between postmortem interval and lung opacification nor an effect on ventilation, although our range of postmortem interval values was narrow (Table 1).
Example of two-stage vPMCT in a 28-day-old infant (case 6). Axial (a–c) and coronal (d–f) PMCT are shown: before ventilation (a, d), after a bag/mask ventilation (b, e) and after PEEP ventilation (c, f). The ET tube tip was in the right main bronchus prior to ventilation (black arrow) and therefore removed. A nasogastric tube is also demonstrated (white arrow)
Effect of ventilation on normal lungs
Five patients underwent a two-stage vPMCT, the first stage involving vPMCT scan after being given several inflation breaths using a bag and mask system. Mean normal lung HU decreased significantly with bag/mask ventilation from pre-vPMCT values (−213.4 ± 270.8 vs post-vPMCT −464.5 ± 217.4; p < 0.05).
All 12 patients underwent vPMCT using PEEP ventilation, to maintain lung volumes. Overall mean normal lung Hounsfield units decreased significantly with PEEP ventilation from pre-vPMCT values (−134.1 ± 215.1 vs post-vPMCT −531.8 ± 190.1; p < 0.001) and further decreased significantly from first-stage vPMCT values in five patients (−464.5 ± 217.4 vs −659.1 ± 146.4; p < 0.05; Fig. 4).
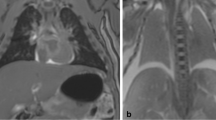
Effect of ventilation on abnormal lung areas
Seven patients had areas of lung abnormalities identified on vPMCT. Mean abnormal lung HU did not change significantly with ventilation (pre-vPMCT −45.3 ± 135.2 vs post-PEEP vPMCT −70.5 ± 164.5; p = 0.70; Fig. 4; Table 1). In two cases, lung consolidation or collapse was identified on vPMCT but not confirmed at autopsy; in one case, this may have been due to a sampling error as the lingula was not sampled at autopsy (Fig. 5; case 9). In one other case, patchy consolidation was identified in a child who also developed a pneumothorax following vPMCT, which may have led to under-aeration of the lungs and a false positive diagnosis. All five cases in which the vPMCT appearances were normal were confirmed as normal at autopsy. Preliminary sensitivity and specificity of vPMCT were 100 % (95 % CI 51.5, 100) and 62.5 % respectively (95 % CI 30.6, 86.2; Table 2). The negative predictive value was 100 % (95 % CI 56.5, 100).
Discussion
The findings of this study have demonstrated that vPMCT is feasible and relatively straightforward and gives good results in children with minimal complications. Where other imaging techniques such as PMMR are not available, vPMCT can help to identify areas of abnormality in paediatric lungs at autopsy and should be considered. Such advances in PM imaging approaches will improve uptake of imaging-assisted autopsies in children in the future.
Although this is a preliminary study, several important findings are apparent. Laryngeal masks were superior to face mask or direct intubation in this clinical group for achieving lung expansion. Rutty et al. reported that a surgical tracheostomy provided the best, most secure and reliable airway in adults, primarily due to its ease of use, and was not associated with gastric air dilatation from inappropriate tube placement [6]. In children, laryngeal masks achieved good results without encountering gastric air dilatation as a common complication. Whilst we did not test surgical airways, it was felt that a non-surgical supraglottic airway would be more in keeping with the concept of less invasive autopsy which is currently being developed for children [7, 9]. As in previous studies, the airway can be imaged prior to ventilation if there is concern about accurate placement [6].
Secondly, in contrast to adult PMCT imaging, the majority of paediatric PMCTs were non-diagnostic for the lungs prior to ventilation, largely due to almost complete white-out of the lungs on non-ventilated imaging. The reasons for this are currently unclear but are likely to involve a combination of small airway collapse and loss of elastic recoil in the paediatric chest in the postmortem state, perhaps compounded by the weight of the anterior chest wall. The near total white-out on pre-vPMCT allowed us to make significant differences with a minimum of ventilator effort, with only a few breaths giving good distension of the lungs in some cases. Delineation of the ‘minimum effective’ ventilation in this setting is an area for future research. We also acknowledge that in adults, increasing lung opacification, including pleural fluid, has been demonstrated with increasing postmortem interval [10, 11]. We did not find a relationship between postmortem interval and lung opacification nor an effect on ventilation, although our range of postmortem interval values was narrow (Table 1). There is no evidence from our preliminary study that ventilation was less effective with increasing postmortem interval.
Thirdly, whilst simple bag/mask ventilation improved lung aeration compared to no ventilation, better results (significant reduction in lung HU) were associated with the use of PEEP ventilation. This is similar to the findings in adults [5], and thus, we also recommend the use of PEEP ventilation to optimise vPMCT lung imaging in children.
Following ventilation and lung expansion, PMCT could be used to distinguish between normal and abnormal lungs in children, since inflation of the normal lung helped to identify abnormal areas of uninflated lung. The HU of lung areas which did not change significantly following ventilation were associated with true lung pathology, including pneumonia and chronic lung disease of prematurity, although this finding was also associated with false positive diagnoses. Interestingly, one of these false positives was made in a case which underwent a pneumothorax as a complication of vPMCT, implying that the lungs were incompletely inflated (Table 1), which may lead to over-interpretation of collapsed or underinflated lungs.
Previous studies have attempted to use unventilated PMCT in the paediatric setting. Proisy et al. found a high concordance between PMCT and autopsy in a group of 47 children, although the cause of death remained unexplained in over 60 % of cases [12], similar to the 50 % unexplained rate in our study. Specifically assessing the lungs, they also identified ground glass opacification in almost all (41/47; 87 %) subjects, which they considered to be a normal postmortem finding where no other lung changes were identified. Only two cases had pneumonia at autopsy, but 10 others had appearances suggestive of bilateral consolidation which represented pulmonary oedema in nine cases and pneumonia in only one. Noda et al. performed PMCT on 38 children, with discordance identified in the majority of thoracic lung pathology: they reported that PMCT could not differentiate between aspiration pneumonia, cardiac failure and infectious pneumonia [13]. One study of almost 100 paediatric forensic PMCTs revealed only four respiratory deaths, with several false negatives, and the authors acknowledge that postmortem consolidation and livor mortis interfere with assessment of the lungs, which postmortem ventilation might improve [14].
These studies are largely in agreement with other PM imaging modalities: PMMR has been evaluated to detect lung pathology in the paediatric autopsy setting and has been shown to be relatively insensitive to several different types of pathology, with pneumonia particularly difficult to identify on conventional PMMR imaging [2]. Our results suggest that vPMCT may be of use in differentiating normal from abnormal lung areas, although ventilated PMMR may give similar results, provided MR-compatible airways and ventilation techniques are used, although this remains to be evaluated.
Limitations
We acknowledge that this is a preliminary feasibility study; however, these are good initial results using a simple airway insertion technique, which may be useful in future clinical practice. Initial sensitivity and specificity data from this study have confidence intervals that are too wide to be meaningful due to small sample size, but the high negative predictive value likely suggests that vPMCT could be useful to exclude lung pathology in future clinical use. Although only demonstrated in a small numbers of patients, we would expect that the additional use of vPMCT would be useful in differentiating normal and abnormal lung areas in larger studies of PM imaging in this patient group, which may be useful in directing the pathologist to areas of abnormality for potential tissue sampling or image-guided biopsy.
Conclusion
vPMCT is feasible, relatively simple to perform and associated with good results in children, with minimal complications. vPMCT may help to highlight areas of abnormality in the paediatric lungs at autopsy and, therefore, may be useful to exclude paediatric lung disease and to guide sampling if required. Together with other imaging techniques, vPMCT may encourage wider uptake of imaging-assisted autopsies in children.
Abbreviations
- HU:
-
Hounsfield units
- LMA:
-
Laryngeal mask airway
- PEEP:
-
Positive end expiratory pressure
- (PM)MR:
-
(Postmortem) magnetic resonance imaging
- vPMCT:
-
Ventilated postmortem computed tomography
References
Thayyil S, Sebire NJ, Chitty LS, Wade A, Chong WK, for the MARIAS collaborative group et al (2013) Post-mortem MRI versus conventional autopsy in fetuses and children: a prospective validation study. Lancet 382:223–233
Arthurs OJ, Thayyil S, Olsen OE, Addison S, Wade A, Jones R, Norman W, Scott RJ, Robertson NJ, Taylor AM, Chitty LS, Sebire NJ, Owens CM (2014) Diagnostic accuracy of post-mortem MRI for thoracic abnormalities in fetuses and children. Eur Radiol 24:2876–2884
Germerott T, Preiss US, Ebert LC et al (2010) A new approach in virtopsy: postmortem ventilation in multislice computed tomography. Legal Med (Tokyo) 12:276–279
Germerott T, Flach PM, Preiss US, Ross SG, Thali MJ (2012) Postmortem ventilation: a new method for improved detection of pulmonary pathologies in forensic imaging. Legal Med (Tokyo) 14:223–228
Robinson C, Biggs MJ, Amoroso J, Pakkal M, Morgan B, Rutty GN (2014) Post-mortem computed tomography ventilation; simulating breath holding. Int J Legal Med 128:139–146
Rutty GN, Biggs MJP, Brough A, Robinson C, Mistry R, Amoroso J, Deshpande A, Morgan B (2015) Ventilated post-mortem computed tomography through the use of a definitive airway. Int J Legal Med 129(2):325–334, IJLM-D-14-00316
Arthurs OJ, Taylor AM, Sebire NJ (2013) The less invasive perinatal autopsy: current status and future directions. Fetal Matern Med Rev 24:45–59
Royal College of Pathologists Working Party on the Autopsy (2006) Guidelines on autopsy practice: scenario 9: stillborn infant (singleton). June 2006. http://www.rcpath.org/Resources/RCPath/ Migrated_Resources/Documents/G/G001Autopsy-Stillbirths-Jun06.pdf. Accessed Jan 2015
Sebire NJ, Weber MA, Thayyil S, Mushtaq I, Taylor A, Chitty LS (2012) Minimally invasive perinatal autopsies using magnetic resonance imaging and endoscopic postmortem examination (“keyhole autopsy”): feasibility and initial experience. J Matern Fetal Neonatal Med 25:513–518
Shiotani S, Kobayashi T, Hayakawa H, Kikuchi K, Kohno M (2011) Postmortem pulmonary edema: a comparison between immediate and delayed postmortem computed tomography. Legal Med (Tokyo) 13:151–155
Hyodoh H, Shimizu J, Watanabe S, Okazaki S, Mizuo K, Inoue H (2015) Time-related course of pleural space fluid collection and pulmonary aeration on postmortem computed tomography (PMCT). Legal Med (Tokyo). doi:10.1016/j.legalmed.2015.01.002
Proisy M, Marchand AJ, Loget P et al (2013) Whole-body post-mortem computed tomography compared with autopsy in the investigation of unexpected death in infants and children. Eur Radiol 23:1711–1719
Noda Y, Yoshimura K, Tsuji S et al (2013) Postmortem computed tomography imaging in the investigation of nontraumatic death in infants and children. Biomed Res Int 2013:327903
Sieswerda-Hoogendoorn T, Soerdjbalie-Maikoe V, de Bakker H, van Rijn RR (2014) Postmortem CT compared to autopsy in children; concordance in a forensic setting. Int J Legal Med 128:957–965
Acknowledgments
OA is funded by an NIHR Clinician Scientist AWARD, and NJS is funded by an NIHR Senior Investigator award, Great Ormond Street Children’s Charity and the Great Ormond Street Hospital Biomedical Research Centre.
This article presents independent research funded by the National Institute for Health Research (NIHR) and supported by the Great Ormond Street Hospital Biomedical Research Centre. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Ethical standards
This study complies with the current laws and ethical standards required in the UK.
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Arthurs, O.J., Guy, A., Kiho, L. et al. Ventilated postmortem computed tomography in children: feasibility and initial experience. Int J Legal Med 129, 1113–1120 (2015). https://doi.org/10.1007/s00414-015-1189-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-015-1189-z