Abstract
mFISH analysis of chromosome aberration profiles of 47 and 144 h lymphocyte cultures following exposure to 193 mGy α-particle radiation confirmed that the frequency of stable aberrant cells and stable cells carrying translocations remains constant through repeated cell divisions. Age-specific rates and in vitro dose–response curves were used to derive expected translocation yields in nine workers from the Mayak nuclear facility in Russia. Five had external exposure to γ-radiation, two of whom also had exposure to neutrons, and four had external exposure to γ-radiation and internal exposure to α-particle radiation from incorporated plutonium. Doubts over the appropriateness of the dose response used to estimate translocations from the neutron component made interpretation difficult in two of the workers with external exposure, but the other three had translocation yields broadly in line with expectations. Three of the four plutonium workers had translocation yields in line with expectations, thus supporting the application of the recently derived in vitro α-particle dose response for translocations in stable cells. Overall this report demonstrates that with adequate reference in vitro dose–response curves, translocation yield has the potential to be a useful tool in the validation of red bone marrow doses resulting from mixed exposure to external and internal radiation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In vitro studies on the induction of chromosome aberrations by α-particle radiation have revealed the complexity of the damage (Anderson et al. 2000; Moquet et al. 2001; Anderson et al. 2002, 2003; Barquinero et al. 2004; Anderson et al. 2007; Tawn et al. 2007, 2008; Curwen et al. 2012). A densely ionizing α-particle will only intersect a small fraction of the cell volume and the deposition of energy and resulting DNA damage will be localized along the particle track, resulting in multiple rearrangements. The complexity of these rearrangements is such that the vast majority will be unstable and hence incapable of successful cell division (Anderson et al. 2000, 2003; Tawn et al. 2007; Curwen et al. 2012). The profile of chromosome damage seen in peripheral blood lymphocytes of nuclear workers with internally deposited plutonium will therefore only represent a small fraction of the chromosomally aberrant cells that arose from exposure of precursor cells to plutonium deposited in the bone marrow or on bone surfaces. Attempts to characterize and quantify the chromosome aberrations induced by α-particle radiation should focus on those that are likely to be transmitted through cell division if chromosome aberrations in peripheral blood lymphocytes are to be used as a reliable marker of exposure.
The early application of fluorescence in situ hybridization (FISH) techniques to the analysis of chromosome aberrations induced by α-particle radiation highlighted the presence of multiple breaks within a single chromosome and led to suggestions that insertions and inversions could be potential markers of exposure (Anderson et al. 2000, 2003, 2005; Hande et al. 2003; Mitchell et al. 2004). However, more detailed analyses revealed that most insertions and inversions were part of complex unstable aberrations, and therefore very few would be transmissible (Barquinero et al. 2004; Tawn et al. 2007, 2008; Curwen et al. 2012). Nevertheless, the application of multi-coloured FISH (mFISH) has shown that, whilst the majority of α-particle-irradiated cells will suffer complex non-transmissible chromosome damage, a significant proportion survive with simple exchanges, in particular translocations, that can be passed on to descendant cells (Anderson et al. 2005; Curwen et al. 2012).
A number of studies have characterized the chromosome aberrations observed in peripheral blood lymphocytes from nuclear workers exposed to α-particle-emitting internally deposited plutonium and attempted to relate these to the cumulative internal dose to the bone marrow (Brandom et al. 1979; Tawn et al. 1985; Brandom et al. 1990; Whitehouse et al. 1998; Hande et al. 2003; Mitchell et al. 2004; Anderson et al. 2005; Hande et al. 2005; Tawn and Whitehouse 2005; Livingston et al. 2006; Tawn et al. 2006; Sotnik et al. 2014). The majority have identified translocations as the predominant aberration but, although their frequency is greater than that expected from any associated external low LET γ-ray exposure, little has been achieved in terms of using translocation frequency to quantify the response following in vivo α-particle exposure.
In a previously reported study using mFISH (Curwen et al. 2012), we derived dose responses for the in vitro induction of chromosome aberrations by α-particle radiation with particular emphasis on categorizing the stability and potential transmissibility of the different aberrant cell types. Cells were cultured for 47 h to ensure that all cells analysed were in their first in vitro division. Additional to this, and presented here, lymphocytes exposed to 193 mGy were analysed for aberrations after 144 h in culture in order to test assumptions regarding aberration transmissibility. A group of nine workers from the Mayak nuclear facility were also examined with the aim of comparing translocation frequencies associated with occupational exposure to both internal α-particle radiation and external γ-rays with occupational exposure only to external γ-rays. However, application of a new dosimetry system (Khokhryakov et al. 2013) after the chromosome analysis was completed revealed that two of the five workers identified originally as having only external γ-ray exposure were now assessed as having additional neutron exposure. The men were analysed for chromosome aberrations in relation to recorded doses and comparisons made with expectations from in vitro dose response data.
Materials and methods
In vitro studies
Cell irradiation and culture
Full details of the irradiation procedure and cell culture have been previously reported (Curwen et al. 2012). Briefly, peripheral blood from a healthy volunteer at Westlakes Research Institute (WRI) was transported to Oxford for irradiation. Informed consent was provided, and ethical approval was obtained from the National Health Service (NHS) Local Research Ethics Committee. Following centrifugation, lymphocytes were extracted from the blood sample, resuspended in Roswell Park Memorial Institute (RPMI-1640) medium (Sigma-Aldrich, Dorset, UK), plated on to a Hostaphan-based irradiation dish (Hoeschst, Weisbaden, Germany) and spread using a TASTRAK CR39 plastic disc (Track Analysis Systems Limited, Bristol, UK) to form a cell monolayer, thus ensuring that all cells would be irradiated. Irradiation was performed using a versatile 238Pu α-particle irradiator, designed and constructed in-house specifically for the in vitro irradiation of mammalian cells with α-particles of well-defined energy, LET, direction and dose (Goodhead et al. 1991). Cells were irradiated with α-particles with incident energy of 3.26 MeV (LET 121 keV µm−1), producing a mean dose to the cell population of 193 mGy, assuming a spherical cell geometry with a 7.1 μm diameter (Anderson et al. 2000) and stopping power data for liquid water (Biersack and Haggmark 1980; Curwen et al. 2012) to take into account variation in energy and LET.
After irradiation, cells were washed in complete medium [RPMI-1640 medium supplemented with 15 % foetal calf serum (Invitrogen Limited, Paisley, UK), 1 % l-glutamine (Invitrogen Limited), 100 IU/ml penicillin (Invitrogen Limited) and 100 µg/ml streptomycin (Invitrogen Limited)] and incubated at 37 °C for a minimum of 2 h to allow for DNA repair. Cultures were established using pre-gassed (5 % CO2/95 % air) RPMI-1640 complete medium, and the T-lymphocytes were stimulated to divide by the addition of 1 % phytohaemagglutinin (PHA) (M-form) (Invitrogen Limited). Culture flasks were transported to WRI at 37 °C before being transferred to a humidified 5 % CO2-gassed incubator (Binder, Germany). In order to study aberration induction, cells were cultured for 47 h, it previously having been established that at this time >95 % of cells were in their first in vitro division. Separate cultures were also established for 144 h, based on a recommended method for long-term culture (Boei et al. 1996), to determine aberration transmissibility through cell division. For the 144 h cultures, bromodeoxyuridine (BrdU) (final concentration 10μM) (Invitrogen Limited) was added to determine in vitro cell division kinetics. Initial studies with unirradiated cells indicated that at this time, 95 % of cells were in their third or subsequent division. However, a subsequent check following 193 mGy α-particle irradiation revealed that this had reduced to 66 %. Nevertheless, 30 % were in second division, so overall 96 % had gone through one or more complete divisions. For both 47 and 144 h cultures, colcemid (final concentration of 0.1 µg/ml) (Invitrogen Limited) was added for the final 4 h of cell culture. Cells were harvested by the addition of a hypotonic solution (0.075 M potassium chloride (KCl)) (VWR International, Leicestershire, UK) followed by fixation with a 3:1 methanol:glacial acetic acid solution (VWR International). Fixed cells were stored at −20 °C overnight, or longer, prior to slide preparation.
In vivo studies
Study group
The nine workers in this study come from the original cohort from the Mayak Production Association (PA) in Russia, which comprises men hired to one of the main plants (reactor, plutonium production, radiochemical) in 1948–1958. Details of the original Mayak PA worker cohort have been previously reported (Azizova et al. 2008). The individuals invited to participate in the current study signed a form of informed consent to voluntary participation according to the Russian Federation legislation concerning public health protection. All nine men had spent their working lives in the nuclear industry. Individual total absorbed red bone marrow doses were derived from the recently introduced Mayak Worker Dosimetry System (MWDS–2008). This is the latest dosimetry system developed within the framework of Russian–U.S. cooperation and provides updated occupational histories and improved individual dose estimates for internal α-particle, external γ-ray and neutron exposures in various tissues and organs (Khokhryakov et al. 2013). Individual information for workers in the study group is provided in Table 1.
Cell culture
Peripheral blood lymphocytes were cultured according to a standard protocol. Lymphocytes were precipitated by centrifugation of whole blood samples and the lymphocyte film obtained (1.2 ml) placed into a 25-cm2 culture flask (Corning, Amsterdam, The Netherlands) containing 10 ml Gibco® PB-MAX™ Karyotyping Medium (Life Technologies, Carlsbad, USA). In order to ensure that all cells are in their first in vitro division, peripheral blood lymphocytes are usually cultured for 48 h in accordance with international consensus (IAEA 2011). However, in the current study, the advanced donor age resulted in insufficient metaphase spreads at 48 h and experiments were performed in order to select a more suitable culture time. Peripheral blood lymphocyte cultures were supplemented with BrdU (Sigma, St. Louis, US) (final concentration 15 μM) in order to check cell cycle progression, and it was found that at 68–72 h 87 % of metaphases were still in first mitosis. Culturing conditions were therefore adjusted to 68 h. Colchicine (Sigma, St. Louis, USA) (0.01 μg/ml) was added 4 h before fixation. Cells were then treated with 0.075 M KCl (Panreac, Barcelona, Spain) hypotonic solution for 15 min at 37 °C, pelleted and fixed with ice-cold 3:1 ethanol (Hippocrate, Samara, Russia): glacial acetic acid (Panreac, Darmstadt, Germany) solution. The cell suspension was dropped on pre-cooled wet slides (Menzel-Gläser, Braunshweig, Germany) and dried in the steam of a hot water bath.
Multicoloured fluorescence in situ hybridisation (mFISH)
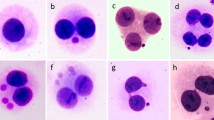
The mFISH procedure uses various fluorescent dyes to detect at least 24 different chromosome painting probes at the same time offering the simultaneous presentation of all 24 human chromosomes in one hybridization reaction. Each paint is labelled with either one or a unique combination of the five fluorochromes (biotin and four fluorochromes with emission spectra equivalent to FITC, Spectrum Orange, TexasRed and DEAC), resulting in an unequivocal colour signature for each chromosome pair labelled.
All procedures were performed at room temperature unless otherwise specified. The pH of 1× PBS solution, each stock solution of SSC (2×, 1×, 0.1×) and 4× SSCT solution was tested before every procedure to ensure the value was between 7.0 and 7.5. Slides were pretreated with pepsin (Sigma, Poole, UK) [1:50 × 103 in 10 mM HCl (VWR International)] at 37 °C for 2 min to remove cytoplasmic proteins prior to washing in 1× PBS (Sigma) for 3 min. 100 µl post-fixation solution [1 % formaldehyde (Sigma) in 1× PBS + 50 mM MgCl2 (Sigma)] was applied and slides overlaid with a coverslip, incubated for 10 min, and washed for 3 min in 1× PBS. Following stabilization in 0.1 × SSC (Sigma) for 1 min and incubation in 2 × SSC (Sigma) at 70 °C for 30 min, slides were allowed to cool to approximately 37 °C before rinsing again in 0.1× SSC for 1 min. For denaturation, slides were treated with 0.07 N NaOH (Sigma) for 1 min, washed for 1 min in 0.1× SSC at 4 °C and 1 min in 2× SSC at 4 °C and finally dehydrated through an ethanol series (1 min each in 30, 50, 70 and 100 %). In parallel to the pretreatment and denaturation of the chromosome spreads, 24XCyte chromosome probe cocktail (10 µl per slide) (Metasystems, Altlussheim, Germany) was denatured at 75 °C for 5 min, placed briefly on ice and incubated for 30 min at 37 °C. The probe was pipetted onto the denatured chromosome slide preparation, overlaid with a coverslip, sealed with rubber cement and left to hybridize in a humidified chamber for 72 h at 37 °C. For the detection of biotin labelled probes with Cy5, rubber cement and coverslips were carefully removed from the metaphase slides, which were then washed in 1× SSC (Sigma) at 75 °C for 5 min and incubated in 4× SSCT [4× SSC (Sigma) + 0.05 % Tween™20 (Sigma)] for 5 min to remove unspecified probe binding. To each slide, 50 µl of blocking reagent (Metasystems) was applied prior to overlaying with a coverslip and slides incubated for 10 min at 37 °C in a humidified chamber followed by a brief wash in 4× SSCT. A mixture of 2 µl of detection reagent 1 + 3 (Metasystems) and 50 µl blocking reagent was then applied to each slide, coverslips added and slides incubated at 37 °C for 20 min followed by two washes with 4× SSCT for 3 min on a shaking plate. Finally slides were washed in 1× PBS for 3 min on a shaking plate, air-dried and counter-stained with 20 µl of 4′, 6-diamidino-2-phenylindole (DAPI) in Vectashield anti-fade solution (Metasystems), overlaid with coverslips, sealed and stored in the dark at 4 °C prior to chromosome analysis or long-term storage at −20 °C.
Chromosome analysis
Microscope analysis was performed using a Zeiss Axioplan II imaging fluorescence microscope (Imaging Associates, Bicester, England) with motorized stage and filter sets for FITC, Spectrum Orange, Texas Red, Cy5, DEAC and DAPI. Images were auto-captured, processed and analysed using Metafer4 and Isis software (Metasystems), which assigns ‘‘pseudo colours’’ based on particular combinations of fluorochromes enabling the identification of all 22 pairs of autosomes plus the X and Y sex chromosomes. All slides were coded prior to chromosome analysis.
Chromosome aberrations are commonly classified as simple, involving one or two breaks in one or two chromosomes, or as complex, involving three or more breaks in two or more chromosomes (Savage and Simpson 1994). For the vast majority of aberrant cells, this classification is straightforward. However, in the case of α-particle irradiation, which produces multiple correlated breaks along the particle track, occasions can arise where the resulting aberration can be resolved into a number of what appear to be discrete independent simple exchanges rather than one complex aberration. Therefore, in this analysis, aberrant cells with aberrations involving one or two chromosome breaks have been classified as having one simple aberration, i.e. an acentric, dicentric or translocation, and cells with chromosome rearrangements involving three or more breaks have been included into one category of cells with multiple aberrations. Chromosomally aberrant cells were further classified as stable or unstable, the presence of an acentric, dicentric or centric ring conferring instability. In addition, a number of cells with deletions of portions of chromosome arms were noted in the 144 h in vitro cultures and in some of the workers’ samples. Whilst technically such cells can be stable and can pass through cell division unhindered, they are derived from unstable cells with acentric fragments. Furthermore, because they are chromosomally unbalanced it is likely that they will eventually be eliminated. Such cells have therefore been placed in the unstable category.
Aberration frequencies were tested for heterogeneity using a two-sided χ2 test. Standard errors (SE) are based on Poisson assumptions.
Results
In vitro studies
Data from 47 and 144 h cultures of cells irradiated with 193 mGy of α-particle radiation are presented in Fig. 1. A total of 1,052 cells were analysed from the 47 h and 1,016 cells from the 144 h cultures. Frequencies of cells with one simple aberration were similar at the two culture times, being 26.62 ± 5.03 × 10−3 at 47 h and 31.50 ± 5.57 × 10−3 at 144 h (χ 21 = 0.44; P = 0.51), whereas frequencies of cells with multiple aberrations dropped significantly from 55.13 ± 7.24 × 10−3 at 47 h to 7.87 ± 2.78 × 10−3 at 144 h (χ 21 = 37.36; P < 0.001). When aberrant cells were examined for stability, no significant difference for stable cells was found between the frequency of 13.31 ± 3.56 × 10−3 at 47 h and 12.80 ± 3.55 × 10−3 at 144 h (χ 21 = 0.01; P = 0.92). In contrast, the frequency of unstable cells declined significantly from 68.44 ± 8.07 × 10−3 at 47 h to 26.57 ± 5.11 × 10−3 at 144 h (χ 21 = 19.88; P < 0.001). Frequencies of simple translocations in stable cells did not differ significantly between 10.20 ± 3.23 × 10−3 at 47 h and 11.12 ± 3.35 × 10−3 after 144 h of culture (χ 21 = 0.04; P = 0.84). However, the frequency of dicentrics (including dicentric equivalents) in all cells fell significantly from 50.38 ± 6.92 × 10−3 at 47 h to zero at 144 h (χ 21 = 52.53; P < 0.001).
In vivo studies
Table 2 provides numbers and frequencies of aberrant cell types for all nine men. Considering the men with external radiation as a whole revealed that 67 % of the aberrant cells were stable compared with 82 % for the plutonium workers. The predominant aberrant cell type was a stable cell with one simple aberration (Table 3), and all the aberrations in these cells were translocations. Only one unstable cell with multiple aberrations was observed, this being in a plutonium worker. One worker with only external radiation and two plutonium workers had stable cells with multiple aberrations. Frequencies of dicentrics (including dicentric equivalents) in total cells are presented in Table 3. Because each cell was analysed fully, we have chosen to give the frequency of translocations in stable cells (Table 3) rather than total cells although with few unstable cells being observed there is little difference in the frequencies.
Expected frequencies of translocations were derived for each worker based on age and recorded dose (Table 4). For age, estimates were determined from data from a large international pooled analysis (Sigurdson et al. 2008). For the induction of translocations by low LET γ-irradiation, the recommended dose response of 1.5 per 100 cells per Gy (Edwards et al. 2005) was applied. Dose records for two of the men with predominantly external irradiation also contained a contribution from neutrons with a mean effective energy spectrum of 300 keV. In the absence of any data on the dose response for translocations in stable cells for 300 keV neutrons, it was decided to use a published dose response for 1 MeV neutrons for two-way translocations following 20 cell divisions (Littlefield et al. 2000) to derive expected translocation numbers. The rationale for this, and the uncertainties in these estimates, are discussed below. For the four workers with significant exposure to α-particle radiation from incorporated plutonium, expected numbers of translocations were calculated using the dose response for translocations in stable cells of 4.1 ± 1.3 × 10−2 per Gy recently derived in our laboratory (Curwen et al. 2012).
Discussion
The detection of frequencies of translocations in peripheral blood lymphocytes by fluorescence in situ hybridization techniques is an established procedure for assessing the extent of chronic and past exposures to low LET radiation (Edwards et al. 2005, 2007; IAEA 2011). Background levels, and their dependence on age, have been well established (Whitehouse et al. 2005; Sigurdson et al. 2008), and in vitro dose–response curves can provide the reference for establishing the relationship between translocation frequencies and dose (Edwards et al. 2005, 2007; IAEA 2011). In vivo studies have shown that, although the peripheral lymphocyte pool is increasingly populated by descendents of irradiated precursor cells, restricting the analysis to translocations in stable cells results in no appreciable reduction in frequencies over time, indicating that there is little difference in sensitivity between bone marrow stem cells and peripheral blood lymphocytes (Edwards et al. 2007). Dose estimations can, therefore, be undertaken with some confidence (Edwards et al. 2005, 2007; IAEA 2011). The majority of peripheral blood lymphocytes sampled in cases of past exposure will have arisen from progenitor cells present in the bone marrow at time of exposure (Ainsbury et al. 2014), and therefore translocation frequencies will reflect the cumulative dose to the red bone marrow. Since chronic occupational exposure to highly penetrating external γ-radiation usually results in uniform exposure, and thus similar tissue doses, the dose estimated from translocation frequency can usually be assumed to equate to whole body dose. However, the distribution of intakes of radionuclides can be tissue specific, and for α-particle-emitting plutonium, this will result in the distribution of dose being highly heterogeneous. A major site of deposition of plutonium is the bone surface, which can result in irradiation of the bone marrow (Leggett et al. 2005) and consequently irradiation of the precursor cells of peripheral blood lymphocytes. Previous in vitro work in this laboratory has applied mFISH to identify aberrations induced by Pu α-particle radiation (Curwen et al. 2012) and to derive dose–response relationships for the induction of chromosomally aberrant stable and unstable cells. The most prevalent aberration in stable cells was a single translocation with a linear dose response for predominantly single-hit nuclei of 4.1 ± 1.3 × 10−2 per Gy. Whilst lifetime occupational doses to α-particles emitted from internally deposited plutonium can exceed the acute doses associated with one-hit kinetics, the doses received by radiation workers will have been accumulated in small increments over many years, and so the response for single-hit cells will be appropriate for establishing a reference dose–response curve for retrospective dose estimations to the red bone marrow following in vivo exposure.
The in vitro work reported here, albeit limited, provides some reassurance that assumptions regarding transmissibility of stable cells, which are derived mainly from studies of low LET irradiation (Edwards et al. 2005, 2007), can also be applied to the induction of chromosome aberrations by α-particle irradiation. Thus, whilst the frequencies of unstable cells carrying simple and multiple aberrations were significantly lower in cells from the 144 h cultures in comparison with the frequencies of cells from the 47 h cultures, the frequencies of stable cells with simple and multiple aberrations remained similar. More specifically, the frequency of translocations in stable cells remained constant. In contrast, the frequency of dicentrics (including dicentric equivalents) had dropped to zero at 144 h, reflecting the inability of cells containing them to pass unhindered through cell division.
For seven of the nine Mayak workers, cells with stable aberrations predominated (Table 2). However, Individual 2 had the same frequencies of stable and unstable cells and Individual 8 had more unstable cells. In both these cases, it was the low frequency of stable cells that was notable. For both the group with external exposure and the group with combined external and internal α-particle exposure, the majority of stable aberrant cells contained a single simple translocation with values of 92 and 89 %, respectively. This is an established aberration profile for cumulative in vivo external low dose, low dose rate, cumulative γ-ray exposure as radiation-induced aberrant cells will usually contain just one single simple aberration (Tawn et al., in preparation). In vitro studies have demonstrated that the most likely outcome of a single nuclear traversal by an α-particle is a complex aberration involving multiple breaks in multiple chromosomes (Anderson et al. 2002, 2005; Tawn et al. 2007; Curwen et al. 2012). However, the vast majority of the cells containing such damage will be unstable and eliminated during subsequent cell divisions, and it is the cells with the less frequently induced simple translocations that survive. Support for this comes from the in vitro work on long-term cultures reported here. Nevertheless, stable cells containing multiple aberrations are induced by α-particle radiation, albeit in small numbers, and have been observed in studies of workers exposed to internally deposited plutonium (Tawn et al. 1985; Whitehouse et al. 1998; Anderson et al. 2005; Hande et al. 2005; Livingston et al. 2006; Tawn et al. 2006; Sotnik et al. 2014). In the current study, such cells were found in three of the nine men (Table 3). Three of the 11 stable aberrant cells observed in Individual 1 contained chromosome interchanges involving three, four and five chromosome breaks, respectively. Dose records indicate that this man had been exposed solely to external γ-radiation, and therefore this finding is somewhat unexpected and worthy of further investigation. Two of the four plutonium workers also contained stable cells with multiple chromosome rearrangements, Individual 7 with four out of a total of 29 stable aberrant cells and Individual 9 with five out of 25 stable aberrant cells. Of the four cells with multiple aberrations observed in Individual 7, two had rearrangements involving four and two involving six chromosome breaks. For Individual 9, one cell contained an insertion, two had interchanges involving three chromosome breaks, and the remaining two cells had rearrangements involving five and 11 chromosome breaks, respectively. In the study group as a whole, only one unstable aberrant cell with multiple aberrations was observed, this being in Individual 6 who was a plutonium worker. The cell had a complex stable interchange involving three breaks in three chromosomes together with a deletion with an associated acentric fragment in a fourth chromosome. Thus, only the presence of an acentric made it unstable. Clearly this peripheral blood lymphocyte has not been through many, if any, cell divisions and was perhaps irradiated directly, not as a result of plutonium in the bone marrow, but as it passed by plutonium deposited in the lymph nodes. Therefore, three of the four plutonium workers exhibited cells with multiple chromosome rearrangements, supporting suggestions that their presence can be used as indicative of exposure to α-particle radiation (Anderson et al. 2000, 2005; Barquinero et al. 2004; Hande et al. 2005; Curwen et al. 2012). Dicentrics were observed in three of the five men with external exposure and two of the plutonium workers (Table 3). However, the low numbers observed and the small numbers of cells scored resulted in large errors being attached to individual frequencies. Overall dicentric frequency was 1.79 ± 0.73 × 10−3 per cell which, although a little higher than reported background levels (IAEA 2011; Edwards et al. 2007), suggests that, in the main, there is a little ongoing direct exposure of peripheral blood lymphocytes.
In order to test the proposition that α-particle exposure could account for a proportion of translocations seen in workers with occupational exposure to α-particle radiation from incorporated plutonium, we derived expected values for translocation frequencies based on age and recorded dose (Table 4). Whilst the original intention was to compare a group of men with external γ-ray exposure with a group with mixed exposure to γ-radiation and α-particle radiation, when the doses were rechecked following the chromosome analysis, new dosimetry methodology (Khokhryakov et al. 2013) indicated that two of the men with external exposure also had a neutron component to their dose.
Deriving the expected translocations for this neutron exposure is problematic since no dose response data for the induction of translocations by 300 keV neutrons are available. Dose responses for translocation induction by 1 MeV neutrons have been reported (Littlefield et al. 2000) and, although no information on cell stability is provided, the study included analysis of cells following 20 in vitro cell divisions. It can be assumed that the aberrant cells observed at this time will predominantly be stable. In the absence of more appropriate data, we used this study to derive expected values for the numbers of translocations resulting from recorded neutron doses received by Individuals 2 and 3. The dose response for two-way translocation data following 20 cell divisions was applied since this is most likely to approximate to simple translocations in stable cells. However, it must be noted that in a similar study conducted shortly afterwards (Fomina et al. 2001), the frequency of translocations induced by 1 Gy of 1 MeV neutrons observed after one in vitro cell division was substantially less than that derived from the earlier study, the implication being that there would also be fewer translocations surviving repeated cell divisions. In vitro studies have shown that dicentric yields vary with neutron energy with those with an energy of 300–400 keV being most efficient (Sevankaev et al. 1979; Ballarini et al. 2003; Schmid et al. 2003). Whilst this might suggest that by using in vitro data for 1 MeV neutrons we have underestimated the translocations expected from the workers’ neutron exposure, this would only be the case if the distribution of aberrations between cells for 300 keV neutrons was the same as for 1 MeV neutrons. Indeed, the more efficient 300 keV neutrons may induce proportionally more cells with multiple aberrations that are likely to be unstable. Clearly more work needs to be performed on the aberration profiles induced by neutrons of different energies before in vitro dose response curves can be applied with confidence to in vivo exposures.
Examination of expected numbers of translocations for the five men with solely external exposure (Table 4) revealed that three, Individuals 1, 4 and 5, had observed numbers roughly in line with expectations albeit the translocation yield in Individual 1 was somewhat lower than expected. However, it was the two workers with neutron exposure who stood out as being out of line with expectations, with expected numbers of translocations greatly exceeding the observed values. This confirms suspicions regarding the appropriateness of the dose response used to derive the expected contribution from neutron exposure, but also must raise questions regarding the nature and extent of this exposure. In this respect, it should be noted that the Mayak dosimetry system is still evolving and doses could be subject to change following updated reassessments. Consideration of the four plutonium workers (Table 4) revealed that for three individuals the observed numbers of translocations are in line with expectations. Moreover, it is the same three, i.e. Individuals 6, 7 and 9, who exhibited cells with multiple aberrations (Table 3). Whilst the main contributions to expected numbers of translocations are age and external γ-ray exposure, the numbers derived from the in vitro dose response curve for α-particle radiation also provide a substantial contribution, ranging from 11 to 30 % of the expected yield. Indeed the similarity between expected and observed yields for these three plutonium workers provides confidence in the use of our previously derived in vitro dose response for α-particle radiation (Curwen et al. 2012). Despite having high recorded doses of γ-ray and α-particle radiation, a very low yield of translocations was observed in Individual 8 and the observed yield could solely be accounted for by his age. Unlike the other workers in the study group, who received their exposure over a long-time period, this individual only worked as a radiation worker for 8 years (Table 1). Having started work in a radioactive environment aged 18 years, he was moved to inactive work 6 years later after receiving a number of greater daily and monthly doses than was considered regular at the time. At age 55 years, he returned to radioactive work for 2 years during which time he received low-level γ-ray exposure. Whereas his exposure record indicates that he has a cumulative red bone marrow γ-ray dose of 1.61 Gy and a cumulative red bone marrow dose of α-particle radiation of 0.425 Gy, this is not borne out by the chromosome results. Further chromosome studies to confirm these findings together with a review of his dose history would seem warranted.
This report demonstrates that with adequate reference in vitro dose response curves, translocation yield can be extended from its current application in cases of exposure to external γ-radiation and can be used in the validation of red bone marrow doses resulting from mixed exposure to external and internal radiation. Whilst appropriate dose response curves are still required for neutron exposure, the expected contribution to translocation yield from internal deposits of plutonium in the bone marrow can be assessed with some confidence. This is the first attempt to quantify individual doses in workers with mixed exposure to external radiation and internally deposited plutonium and, whilst it is recognized that the study group is small, it is hoped that these results will encourage further studies of occupationally exposed workers. Reliable dose reconstruction is essential for epidemiological studies, and translocation frequency in peripheral blood lymphocytes from those with mixed exposures has the potential to be an important tool in this process.
References
Ainsbury EA, Moquet J, Rothkamm K, Darroudi F, Vozilova A, Degteva M, Azizova TV, Lloyd DC, Harrison J (2014) What radiation dose does the FISH translocation assay measure in cases of incorporated radionuclides for the Southern Urals populations? Radiat Prot Dosim 159:26–33
Anderson RM, Marsden SJ, Wright EG, Kadhim MA, Goodhead DT, Griffin CS (2000) Complex chromosome aberrations in peripheral blood lymphocytes as a potential biomarker of exposure to high-LET alpha-particles. Int J Radiat Biol 76:31–42
Anderson RM, Stevens DL, Goodhead DT (2002) M-FISH analysis shows that complex chromosome aberrations induced by alpha -particle tracks are cumulative products of localized rearrangements. Proc Natl Acad Sci USA 99:12167–12172
Anderson RM, Marsden SJ, Paice SJ, Bristow AE, Kadhim MA, Griffin CS, Goodhead DT (2003) Transmissible and nontransmissible complex chromosome aberrations characterized by three-color and mFISH define a biomarker of exposure to high-LET alpha particles. Radiat Res 159:40–48
Anderson RM, Tsepenko VV, Gasteva GN, Molokanov AA, Sevan’kaev AV, Goodhead DT (2005) mFISH analysis reveals complexity of chromosome aberrations in individuals occupationally exposed to internal plutonium: a pilot study to assess the relevance of complex aberrations as biomarkers of exposure to high-LET alpha particles. Radiat Res 163:26–35
Anderson RM, Stevens DL, Sumption ND, Townsend KM, Goodhead DT, Hill MA (2007) Effect of linear energy transfer (LET) on the complexity of alpha-particle-induced chromosome aberrations in human CD34 + cells. Radiat Res 167:541–550
Azizova TV, Day RD, Wald N, Muirhead CR, O’Hagan JA, Sumina MV, Belyaeva ZD, Druzhinina MB, Teplyakov II, Semenikhina NG, Stetsenko LA, Grigoryeva ES, Krupenina LN, Vlasenko EV (2008) The “clinic” medical-dosimetric database of Mayak production association workers: structure, characteristics and prospects of utilization. Health Phys 94:449–458
Ballarini F, Biaggi M, Edwards A, Ferrari A, Ottolenghi A, Pelliccioni M, Scannicchio D (2003) Estimating mixed field effects: an application supporting the lack of a non-linear component for chromosome aberration induction by neutrons. Radiat Prot Dosim 103:19–28
Barquinero JF, Stephan G, Schmid E (2004) Effect of americium-241 alpha-particles on the dose-response of chromosome aberrations in human lymphocytes analysed by fluorescence in situ hybridization. Int J Radiat Biol 80:155–164
Biersack JP, Haggmark L (1980) A Monte Carlo computer program for transport of ions in amorphous targets. Nucl Instrum Methods 174:257–269
Boei JJ, Vermeulen S, Natarajan AT (1996) Detection of chromosomal aberrations by fluorescence in situ hybridization in the first three postirradiation divisions of human lymphocytes. Mutat Res 349:127–135
Brandom WF, Archer PG, Bloom AD, Archer VE, Bistline RW, Saccomanno G (1979) Chromosome changes in somatic cells of workers with internal depositions of plutonium, vol II. Biological implications of radionuclides released from nuclear industries. International Atomic Energy Agency, Vienna
Brandom WF, McGavran L, Bistline RW, Bloom AD (1990) Sister chromatid exchanges and chromosome aberration frequencies in plutonium workers. Int J Radiat Biol 58:195–207
Curwen GB, Tawn EJ, Cadwell KK, Guyatt L, Thompson J, Hill MA (2012) mFISH analysis of chromosome aberrations induced in vitro by alpha-particle radiation: examination of dose-response relationships. Radiat Res 178:414–424
Edwards AA, Lindholm C, Darroudi F, Stephan G, Romm H, Barquinero J, Barrios L, Caballin MR, Roy L, Whitehouse CA, Tawn EJ, Moquet J, Lloyd DC, Voisin P (2005) Review of translocations detected by FISH for retrospective biological dosimetry applications. Radiat Prot Dosim 113:396–402
Edwards AA, Szluinska M, Lloyd DC (2007) Reconstruction of doses from ionizing radiation using fluorescence in situ hybridization techniques. Br J Radiol 80:S63–S67, Spec No 1
Fomina J, Darroudi F, Natarajan AT (2001) Accurate detection of true incomplete exchanges in human lymphocytes exposed to neutron radiation using chromosome painting in combination with a telomeric PNA probe. Int J Radiat Biol 77:1175–1183
Goodhead DT, Bance DA, Stretch A, Wilkinson RE (1991) A versatile plutonium-238 irradiator for radiobiological studies with alpha-particles. Int J Radiat Biol 59:195–210
Hande MP, Azizova TV, Geard CR, Burak LE, Mitchell CR, Khokhryakov VF, Vasilenko EK, Brenner DJ (2003) Past exposure to densely ionizing radiation leaves a unique permanent signature in the genome. Am J Hum Genet 72:1162–1170
Hande MP, Azizova TV, Burak LE, Khokhryakov VF, Geard CR, Brenner DJ (2005) Complex chromosome aberrations persist in individuals many years after occupational exposure to densely ionizing radiation: an mFISH study. Genes Chromosomes Cancer 44:1–9
IAEA (2011) Cytogenetic dosimetry: applications in preparedness for and response to radiation emergencies. International Atomic Energy Agency, IAEA-EPR, Vienna
Khokhryakov VV, Khokhryakov VF, Suslova KG, Vostrotin VV, Vvedensky VE, Sokolova AB, Krahenbuhl MP, Birchall A, Miller SC, Schadilov AE, Ephimov AV (2013) Mayak worker dosimetry system 2008 (MWDS-2008): assessment of internal dose from measurement results of plutonium activity in urine. Health Phys 104:366–378
Leggett RW, Eckerman KF, Khokhryakov VF, Suslova KG, Krahenbuhl MP, Miller SC (2005) Mayak worker study: an improved biokinetic model for reconstructing doses from internally deposited plutonium. Radiat Res 164:111–122
Littlefield LG, McFee AF, Sayer AM, O’Neill JPO, Kleinerman RA, Maor MH (2000) Induction and persistence of chromosome aberrations in human lymphocytes exposed to neutrons in vitro: implications of findings in ‘retrospective’ biological dosimetry. Radiat Protect Dosim 88:59–68
Livingston GK, Falk RB, Schmid E (2006) Effect of occupational radiation exposures on chromosome aberration rates in former plutonium workers. Radiat Res 166:89–97
Mitchell CR, Azizova TV, Hande MP, Burak LE, Tsakok JM, Khokhryakov VF, Geard CR, Brenner DJ (2004) Stable intrachromosomal biomarkers of past exposure to densely ionizing radiation in several chromosomes of exposed individuals. Radiat Res 162:257–263
Moquet JE, Fernandez JL, Edwards AA, Lloyd DC (2001) Lymphocyte chromosomal aberrations and their complexity induced in vitro by plutonium-239 alpha-particles and detected by FISH. Cell Mol Biol 47:549–556
Savage JR, Simpson PJ (1994) FISH “painting” patterns resulting from complex exchanges. Mutat Res 312:51–60
Schmid E, Schlegel D, Guldbakke S, Kapsch RP, Regulla D (2003) RBE of nearly monoenergetic neutrons at energies of 36 keV-14.6 MeV for induction of dicentrics in human lymphocytes. Radiat Environ Biophys 42:87–94
Sevankaev AV, Zherbin EA, Luchnik NV, Obaturov GM, Kozlov VM, Tyatte EG, Kapchigashev SP (1979) Neutron-induced cytogenetic effects of neutrons of different energies on various types of chromosome aberrations. Genetika 15:1046–1060
Sigurdson AJ, Ha M, Hauptmann M, Bhatti P, Sram RJ, Beskid O, Tawn EJ, Whitehouse CA, Lindholm C, Nakano M, Kodama Y, Nakamura N, Vorobtsova I, Oestreicher U, Stephan G, Yong LC, Bauchinger M, Schmid E, Chung HW, Darroudi F, Roy L, Voisin P, Barquinero JF, Livingston G, Blakey D, Hayata I, Zhang W, Wang C, Bennett LM, Littlefield LG, Edwards AA, Kleinerman RA, Tucker JD (2008) International study of factors affecting human chromosome translocations. Mutat Res 652:112–121
Sotnik NV, Osovets SV, Scherthan H, Azizova TV (2014) mFISH analysis of chromosome aberrations in workers occupationally exposed to mixed radiation. Radiat Environ Biophys 53:347–354
Tawn EJ, Whitehouse CA (2005) Chromosome intra- and inter-changes determined by G-banding in radiation workers with in vivo exposure to plutonium. J Radiol Protect 25:83–88
Tawn EJ, Hall JW, Schofield GB (1985) Chromosome studies in plutonium workers. Int J Radiat Biol 47:599–610
Tawn EJ, Whitehouse CA, Riddell AE (2006) FISH chromosome analysis of plutonium workers from the Sellafield nuclear facility. Radiat Res 165:592–597
Tawn EJ, Whitehouse CA, De Ruyck K, Hodgson L, Vandenbulcke K, Thierens H (2007) The characterization and transmissibility of chromosome aberrations induced in peripheral blood lymphocytes by in vitro alpha-particle radiation. Radiat Res 168:666–674
Tawn EJ, Whitehouse CA, Holdsworth D, De Ruyck K, Vandenbulcke K, Thierens H (2008) mBAND analysis of chromosome aberrations in lymphocytes exposed in vitro to alpha-particles and gamma-rays. Int J Radiat Biol 84:447–453
Tawn EJ, Curwen GB, Whitehouse CA, Jonas P, Hodgson L, Cadwell K (in preparation) Chromosome aberrations determined by FISH in radiation workers from the Sellafield Nuclear Facility
Whitehouse CA, Tawn EJ, Riddell AE (1998) Chromosome aberrations in radiation workers with internal deposits of plutonium. Radiat Res 150(4):459–468
Whitehouse CA, Edwards AA, Tawn EJ, Stephan G, Oestreicher U, Moquet JE, Lloyd DC, Roy L, Voisin P, Lindholm C, Barquinero J, Barrios L, Caballin MR, Darroudi F, Fomina J (2005) Translocation yields in peripheral blood lymphocytes from control populations. Int J Radiat Biol 81:139–145
Acknowledgments
The authors would like to thank Liz Ainsbury and David Lloyd for helpful discussions on the interpretation of the workers’ translocation data. This work was funded by grant no. RRX117 from the UK Department of Health Radiation Protection Research programme and by the EU Framework 7 SOLO project (Proposal Number 249675).
Author information
Authors and Affiliations
Corresponding author
Additional information
G. B. Curwen, K. K. Cadwell, E. J. Tawn: formerly of Westlakes Research Institute (WRI), Westlakes Science and Technology Park, Moor Row, Cumbria CA24 3LN, UK (WRI closed in 2010).
Rights and permissions
About this article
Cite this article
Curwen, G.B., Sotnik, N.V., Cadwell, K.K. et al. Chromosome aberrations in workers with exposure to α-particle radiation from internal deposits of plutonium: expectations from in vitro studies and comparisons with workers with predominantly external γ-radiation exposure. Radiat Environ Biophys 54, 195–206 (2015). https://doi.org/10.1007/s00411-015-0585-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00411-015-0585-6