Abstract
Purpose
We compared respiratory mechanics between the positive end-expiratory pressure of minimal respiratory system elastance (PEEPminErs) and three levels of PEEP during low-tidal-volume (6 mL/kg) ventilation in rats.
Methods
Twenty-four rats were anesthetized, paralyzed, and mechanically ventilated. Airway pressure (Paw), flow (F), and volume (V) were fitted by a linear single compartment model (LSCM) Paw(t) = Ers × V(t) + Rrs × F(t) + PEEP or a volume- and flow-dependent SCM (VFDSCM) Paw(t) = (E1 + E2 × V(t)) × V(t) + (K1 + K2 × |F(t)|) × F(t) + PEEP, where Ers and Rrs are respiratory system elastance and resistance, respectively; E1 and E2× V are volume-independent and volume-dependent Ers, respectively; and K1 and K2 × F are flow-independent and flow-dependent Rrs, respectively. Animals were ventilated for 1 h at PEEP 0 cmH2O (ZEEP); PEEPminErs; 2 cmH2O above PEEPminErs (PEEPminErs+2); or 4 cmH2O above PEEPminErs (PEEPminErs+4). Alveolar tidal recruitment/derecruitment and overdistension were assessed by the index %E2 = 100 × [(E2 × VT)/(E1 + |E2| × VT)], and alveolar stability by the slope of Ers(t).
Results
%E2 varied between 0 and 30% at PEEPminErs in most respiratory cycles. Alveolar Tidal recruitment/derecruitment (%E2 < 0) and overdistension (%E2 > 30) were predominant in the absence of PEEP and in PEEP levels higher than PEEPminErs, respectively. The slope of Ers(t) was different from zero in all groups besides PEEPminErs+4.
Conclusions
PEEPminErs presented the best compromise between alveolar tidal recruitment/derecruitment and overdistension, during 1 h of low-VT mechanical ventilation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
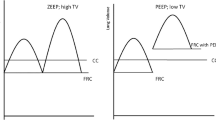
Atelectasis and intermittent airway closure may be common intraoperative findings [1] that can expose the lungs to high levels of shear stress generated during tidal recruitment/derecruitment [2]. This excessive stress in the lung tissue during anesthesia may increase the risk of ventilator induced lung injury (VILI), even in patients with healthy lungs [3,4,5,6]. Positive end-expiratory pressure (PEEP) has been successfully used to minimize atelectasis and tidal recruitment/derecruitment during anesthesia, especially after an alveolar recruitment maneuver (ARM) [7,8,9]. This effect of PEEP is one of the suggested mechanisms to explain the lower levels of pulmonary and systemic inflammation observed during anesthesia in patients without previous lung disease, when compared with those in the absence of PEEP [6]. Consequently, PEEP has been used in protocols of protective ventilation [10, 11]. However, higher levels of PEEP are associated with alveolar hyperinflation and overdistension [12, 13], which can also be a triggering condition for VILI [4, 14]. Consequently, an optimal level of PEEP would provide a balance between alveolar tidal recruitment/derecruitment and overdistension.
Different criteria have been used to define “optimal” PEEP to be used in protective ventilation, including the determination of PEEP of minimal respiratory system elastance (PEEPminErs) [12, 13, 15, 16]. Indeed, PEEPminErs was associated with a better balance between alveolar overdistension and tidal recruitment/derecruitment during a descendent PEEP titration in healthy and injured lung [12, 13, 16]. Nevertheless, whether PEEPminErs maintains this balance over time has yet to be determined.
The fraction of the volume-dependent respiratory system elastance (%E2) derived from a nonlinear model of respiratory mechanics has been used to quantify alveolar tidal recruitment/derecruitment and overdistension in healthy as well as in injured lungs [9, 12, 13, 16,17,18] and could potentially be used to guide strategies of protective ventilation in patients with healthy lungs. The hypothesis of this study was that PEEPminErs, when used as a criterion to select optimal PEEP, would maintain the best balance between alveolar tidal recruitment/derecruitment and overdistension during mechanical ventilation in a lung-healthy model. A secondary hypothesis was that %E2 is able to differentiate patterns of tidal recruitment/derecruitment and overdistension when different levels of end-expiratory pressure were used during ventilation with low tidal volume (VT).
In the present study, we aimed at comparing the occurrence of indices of tidal recruitment/derecruitment and overdistension among PEEPminErs and three other levels of end-expiratory pressure used during 1 h of low-VT mechanical ventilation in lung-healthy anesthetized rats.
Methods
This study was approved by the Ethics Committee on the Animal Use of the Health Sciences Centre, Federal University of Rio de Janeiro (CEUA CCS, IBCCF-019).
Animal Preparation
Twenty-four rats were anesthetized with intraperitoneal ketamine (60 mg/kg) and midazolam (3 mg/kg), followed by IV administration of both agents at 60 mg/kg/h and 3 mg/kg/h, respectively. A tracheal cannula was placed and they were maintained in spontaneous ventilation with room air during instrumentation, comprising electrocardiogram, blood pressure, and rectal temperature. After instrumentation, the animals were placed in dorsal recumbency, paralyzed and ventilated (Inspira ASV, Harvard Apparatus Inc., Road Holliston, MA, USA) with room air in a volume-controlled mode with VT of 6 mL/kg, no PEEP, inspiratory-to-expiratory time ratio (I:E) of 1:2, and respiratory rate (RR) of 90 breaths/min (initial settings).
Experimental Protocol
The experimental timeline is presented in Fig. 1. After a 5-min period under initial settings, an ARM of a plateau pressure (Pplat) of 20 cmH2O maintained for 20 s was followed by a decremental PEEP trial from 6 to 0 cmH2O in 1-min steps of 1 cmH2O. VT was maintained at 6 mL/kg during the PEEP titration and PEEPminErs was determined (see “Data Acquisition and Processing” section). Another ARM, identical to the first one, was performed after the PEEP trial and the animals were randomly assigned to one of following groups: (1) PEEP = 0 cmH2O (ZEEP), PEEPminErs, PEEPminErs + 2 cmH2O (PEEPminErs+2), and PEEPminErs + 4 cmH2O (PEEPminErs+4). Each group had 6 rats ventilated for 1 h with room air and VT of 6 mL/kg, RR of 90 breaths/min, and I:E of 1:2. At the end of the 1-h ventilation, the animals were euthanized during anesthesia by laparotomy and sectioning of abdominal aorta and caudal vena cava.
Data Acquisition and Processing
Airway pressure (Paw) and airflow were recorded in a computer with a sampling rate of 1000 Hz and Paw was fitted to one of the two models of respiratory mechanics: linear single compartment model (LSCM—Eq. 1), [19] or volume- and flow-dependent single compartmental model (VFDSCM—Eq. 2) [20]:
where Rrs represents the linear resistance of the respiratory system; K1 and K2 are the flow-independent and flow-dependent components of Rrs, respectively; E1 and E2 are the volume-independent and volume-dependent components of Ers, respectively; and PEEP represents the airway pressure when volume and flow are zero. From Eq. 2, the fraction of the volume-dependent elastance (%E2) was calculated as
During the PEEP trial, the mechanical parameters of Eq. 1 were estimated on-line for the immediate identification of PEEPminErs. An offline estimation encompassing the 60 min of ventilation was used for the parameters of Eq. 2 and %E2. The dynamics of Ers(t) and %E2(t) were assessed by the slopes (a and c) of Eqs. 4 and 5, respectively, estimated as in Eq. 1:
The average of Ers and %E2 from 50 respiratory cycles within the fifth (M5) and the sixtieth minute of ventilation (M60) were calculated for each group.
Statistics
Data normality was assessed by the Shapiro–Wilk test, and normally distributed data were expressed as mean (SD) and nonnormally distributed data as median (first and third quartiles).
Comparisons among groups were performed by one-way ANOVA or Kruskal–Wallis ANOVA, when appropriate, followed by the Student’s t-test or the Mann–Whitney test, respectively, and the Bonferroni–Holm method [21] was used for the adjustment for multiple comparisons.
The null hypothesis was also tested for the slopes of %E2 and Ers with the Student’s t-test or Mann–Whitney with a p < 0.05 considered sufficient to reject the null hypothesis. Statistical analysis as well as figures and graphs were made in MATLAB (The Mathworks Inc., MA, USA).
Results
PEEPminErs achieved during each PEEP trial ranged from 3 to 6 cmH2O in all groups and it was significantly higher in PEEPminErs+4 (ranging from 4 to 6 cmH2O) than in ZEEP and PEEPminErs+2.
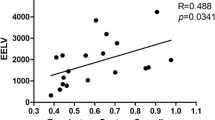
The dynamics of Ers in all animals is presented in Fig. 2. At the beginning of the protocol, Ers, estimated by the intercept of Ers(t), was higher in PEEPminErs+4 and ZEEP groups than in PEEPminErs. The slope of Ers(t) was positive in all but PEEPminEsr+4 group, being larger in magnitude in ZEEP and smaller in PEEPminErs+4 than in PEEPminErs. By contrast, there was a significant temporal effect on %E2 [slope of %E2(t)] only in PEEPminErs. %E2 at the beginning of the protocol [intercept of %E2(t)] was larger in PEEPminErs+2 and PEEPminErs+4 and smaller in ZEEP when compared to PEEPminErs (Fig. 3). The distribution of %E2 in all groups is shown in Fig. 4 and was characterized by tidal recruitment/derecruitment in 79% of the respiratory cycles with ZEEP, and an overdistension occurrence of 100%, 97%, and 28% of the respiratory cycles in PEEPminErs+4, PEEPminErs+2, and PEEPminErs, respectively. In PEEPminErs, 72% of the respiratory cycles had %E2 between 0 and 30%. Ers and %E2 at M5 and M60 are presented in Table 1. %E2 was lower in M60 than in M5 only in PEEPminErs, and was different from PEEPminErs in all groups and in M5 and M60. Ers was higher at M60 than M5 in ZEEP, PEEPminErs, and PEEPminErs+2, and was higher in ZEEP and PEEPminErs+4 than in PEEPminErs.
Temporal dynamics of respiratory system elastance (Ers) in all rats ventilated for 60 min with a tidal volume of 6 mL/kg and different levels of PEEP. PEEP presented for each animal in groups PEEPminErs, PEEPminErs+2, and PEEPminErs+4 is the actual PEEP that each animal was ventilated during the 60 min of ventilation. ZEEP = no PEEP; PEEPminErs = PEEP of minimal Ers; PEEPminErs+2 = PEEP of minimal Ers + 2 cmH2O; and PEEPminErs+4 = PEEP of minimal Ers + 4 cmH2O. Red lines represent the linear function estimated with the linear regression of Ers as a function of time in each animal
Slope (left column) and intercept (right column) of the temporal linear function estimated to the fraction of volume-dependent respiratory system elastance (Panel A) and the respiratory system elastance (Ers, Panel B) in all six rats ventilated for 60 min with tidal volume of 6 mL/kg at different levels of PEEP. ZEEP = no PEEP; MinErs = PEEP of minimal Ers; MinErs + 2 = PEEP of minimal Ers + 2 cmH2O; and MinErs + 4 = PEEP of minimal Ers + 4 cmH2O. v significantly different from PEEPMinErs; x significantly different from zero (p < 0.05). The values connecting all groups are the medians
Histogram of the fraction of volume-dependent respiratory system elastance (%E2) frequency distribution during 1 h of ventilation with 6 mL/kg and different levels of PEEP in rats. Red = %E2 > 30%; Blue = %E2 between 0 and 30%; and Black = %E2 < 0. ZEEP = no PEEP; PEEP E = PEEP of minimal Ers; PEEP E + 2 = PEEP of minimal Ers + 2 cmH2O; and PEEP E + 4 = PEEP of minimal Ers + 4 cmH2O
Discussion
The main results of Ers as well as tidal recruitment/derecruitment and overdistension assessed by %E2 in lung-healthy anesthetized rats mechanically ventilated with protective VT for 1 h were as follows: (1) PEEPminErs presented the best compromise between alveolar tidal recruitment/derecruitment; (2) ZEEP was associated with a positive temporal drift of Ers and a predominance of tidal recruitment/derecruitment; (3) PEEPminErs+4 was the only PEEP that provided temporal stability of Ers but at the expense of overdistension; and (4) %E2 was able to discriminate patterns of alveolar recruitment/derecruitment and overdistension among the different levels of PEEP.
%E2 increased with PEEP and was very similar to values previously reported in rats [22]. As a dynamic method to assess respiratory mechanics, it does not interfere with the current ventilation of the patient, and can be used noninvasively and at the bedside [23]. %E2 higher than 30% has been associated with alveolar overdistension and was predominantly observed with PEEPminErs+2 and PEEPminErs+4, while negative values were more frequent during ZEEP and were potentially related to tidal recruitment/derecruitment [17, 18]. %E2 was always positive and was lower than 30% in the vast majority of cycles with PEEPminErs. Consequently, PEEPminErs seemed to yield a better balance between alveolar tidal recruitment/derecruitment and overdistension.
Atelectasis can develop promptly after the induction of anesthesia [24] contributing to intraoperative increases in venous admixture and decreases in PaO2, particularly in the absence of PEEP [25]. Atelectasis can also be a substrate for elevated shear stress in the lungs generated by the tidal alveolar recruitment/derecruitment at the interface between normal and nonaerated areas of the lung [2]. The higher occurrence of negative %E2 in the rats ventilated with ZEEP suggested that more tidal recruitment/derecruitment ensued in these animals, likely due to significant atelectasis, as found in pigs [13]. Indeed, tidal recruitment/derecruitment was already expected in the rats ventilated with ZEEP and low VT probably because of progressive atelectasis, as observed in an ex vivo rat model [26] and an in vivo model in mice [27]. However, ZEEP was included in the experimental design because it is still commonly used during anesthesia [28] and also to test whether %E2 would be able to identify alveolar tidal recruitment/derecruitment distinctly from the PEEP levels.
PEEP can reverse or prevent atelectasis as well as improve respiratory mechanics and oxygenation during anesthesia [8, 12, 29]. In a recent clinical trial with anesthetized patients with healthy lungs, PEEP of 12 cmH2O was able to minimize tidal recruitment/derecruitment without increasing the levels of overdistension when compared to low levels of PEEP (≤ 2 cmH2O) [9]. Different methods have been used to identify the best PEEP to be used during mechanical ventilation, including the PEEPminErs [12, 16, 30]. The concept of “optimal PEEP” was defined as the PEEP of minimal Ers by Suter and colleagues [15] and resulted in the best oxygen delivery and the lowest dead-space fraction in ARDS patients. In the present study, PEEPminErs was considered the optimal PEEP because it was associated with the best balance between alveolar tidal recruitment/derecruitment and overdistension, similarly to the computerized tomography findings in a pig model of healthy and injured lung [12, 13, 16], as well as in a computational model of injured canine lungs [31]. Differently from studies that evaluated alveolar tidal recruitment/derecruitment and overdistension during PEEP titration [11,12,13], the evaluation during the whole period of ventilation, as presented here, provided a more meaningful information about the effectiveness of PEEPminErs as a method of PEEP choice for protective ventilation during anesthesia. In addition, to offer an objective assessment of tidal recruitment/derecruitment and overdistension in the lungs, %E2 detected dynamic changes in these patterns that could occur during ventilation, as observed in the rats ventilated with PEEPminErs. If the period of ventilation used with PEEPminErs was longer, possibly %E2 would reach negative levels, indicating tidal recruitment/derecruitment due to progressive atelectasis. In this case, %E2 could be a parameter to identify the best moment for an ARM during protective ventilation using PEEPminErs. This strategy of ARM seems more rational than performing an ARM every 30 min as previously described in a protective ventilation protocol [10].
The temporal increase in Ers observed in ZEEP, PEEPminErs, and PEEPminErs+2 can be an additional indication of progressive alveolar derecruitment. This deterioration of Ers during ventilation has been demonstrated before in models of healthy and injured lungs and seems to be related to alveolar derecruitment and progressive decrease in lung aeration [32,33,34,35]. However, the interpretation of the temporal increase in Ers in the context of protective ventilation needs to be further investigated because its association with VILI seems to be variable in different experimental settings [33,34,35]. Probably, the combined evaluation of %E2 and ErsErs and their temporal progression can provide valuable information to guide ventilatory settings, as well as the timing for ARMs.
When similar criteria were used to select low PEEP levels in ARDS patients, a large clinical trial observed increased mortality at 28 days when PEEPminErs+2 [36], while a smaller clinical trial reported less organ dysfunction and a trend toward decreased mortality when PEEPminErs was used [30]. This discrepancy between the results may be explained by the higher incidence of overdistension in the higher PEEP group, as observed when PEEPminErs+2 and PEEPminErs+4 were used in the present study. In fact, the PEEP difference between the low and high PEEP groups in the two previously mentioned studies was between 2 and 4 cmH2O. Recent studies have shown that low driving pressure was the ventilatory variable most strongly correlated with improvements in clinical outcome in ARDS [37] and lung-healthy surgical patients [38]. These findings provide substantial support for the use of PEEPminErs as a method to choose the ideal PEEP, because it will always be associated with the lowest driving pressure given a fixed VT. Consequently, PEEPminErs has the potential to improve the beneficial effects in outcome found with moderate PEEP (6 to 8 cmH2O) and ARM in surgical patients at risk for postoperative pulmonary complications (PPC) [10]. Future clinical trials in patients with healthy lungs are warranted to shed some light on the clinical application of using PEEPminErs as a method of PEEP choice during anesthesia.
PEEP levels higher than PEEPminErs were used to explore the concept of “open-lung PEEP,” since in lung-healthy rats it seemed to be associated with the mathematical inflection point of the PV curve—approximately 4 cmH2O above PEEPminErs (PEEPminErs+4) [22]. In fact, the only PEEP that maintained alveolar stability was PEEPminErs+4, but at the expense of detrimental alveolar overdistension.
Despite the lack of lung computerized tomography (CT) scans or other standard methods to confirm the results achieved by the %E2, this method has been able to detect alveolar tidal recruitment/derecruitment and overdistension more consistently in healthy than injured lungs [13], which reinforce the reliability of our results. Moreover, the mathematical model used in this study included a nonlinear component of Rrs, which was shown to improve the estimation of %E2, especially when inspiratory waveforms other than constant flow are used or when nonlinearities associated with the endotracheal tube resistance are present [19, 39]. Future studies correlating %E2 with levels of inflammatory biomarkers in the lungs and/or plasma, lung histology, and more importantly patient outcome should be performed for a rational clinical use of this technique to evaluate protective ventilation in the lung-healthy patient.
This study presents some limitations such as the short duration of ventilation, ventilation with room air, and the respiratory mechanics differences between rats and humans. Webb and Tierney [40] reported that significant pulmonary edema developed after few minutes of using high Ppeak in rats. However, the same degree of lung injury requires a much longer period of mechanical ventilation in larger species [41, 42]. Consequently, we believe that our model possibly represent the majority of anesthetic procedures, considering the differences in the time course of VILI within species [40,41,42]. Ventilation with room air does not necessarily represent the usual clinical anesthesia scenario, but was used to minimize reabsorption atelectasis, which is commonly seen with high FiO2 [43]. Probably, if higher FiO2 were used in the present study, a magnification of atelectasis and alveolar instability would be observed as previously reported in humans [43]. Finally, the respiratory mechanics of rats is somewhat different from humans [44, 45]. First, the temporal evolution of Ers seen in rats would probably take longer in humans because of the much faster respiratory rate in the later. Second, the body weight-normalized chest wall elastance of rats is approximately a fourth of that in humans [44, 45]. This difference, associated with the smaller vertical gradient in the rat respiratory system and the lower pleural pressure at functional residual capacity, affects the transpulmonary pressure and the end-expiratory lung volume at a given PEEP in such way that the PEEP needed to provide less alveolar collapse as well as PEEPminErs should be higher in humans than in rats. However, PEEPminErs is determined in an individual basis and should represent the PEEP with the best compromise between alveolar overdistension and tidal recruitment/derecruitment independently of variations between subjects or species, as demonstrated in pigs with healthy and injured lungs [12, 13, 16], as well as in the rats of the present study.
In conclusion, PEEPminErs presented the best balance between alveolar tidal recruitment/derecruitment and overdistension, and is a promising clinical criterion to select the best PEEP during protective ventilation of the healthy lung. Future studies evaluating the outcomes of patients using PEEPminErs and %E2 to guide protective ventilation are warranted to define the clinical importance of this method to optimize protective ventilation in the anesthesia clinical scenario.
References
Hedenstierna G, Edmark L (2005) The effects of anesthesia and muscle paralysis on the respiratory system. Intensive Care Med 31(10):1327–1335. https://doi.org/10.1007/s00134-005-2761-7
Mead J, Takishima T, Leith D (1970) Stress distribution in lungs: a model of pulmonary elasticity. J Appl Physiol 28(5):596–608. https://doi.org/10.1152/jappl.1970.28.5.596
Bregeon F, Roch A, Delpierre S, Ghigo E, Autillo-Touati A, Kajikawa O, Martin TR, Pugin J, Portugal H, Auffray JP, Jammes Y (2002) Conventional mechanical ventilation of healthy lungs induced pro-inflammatory cytokine gene transcription. Respir Physiol Neurobiol 132(2):191–203
dos Santos CC, Slutsky AS (2006) The contribution of biophysical lung injury to the development of biotrauma. Annu Rev Physiol 68:585–618. https://doi.org/10.1146/annurev.physiol.68.072304.113443
Michelet P, D’Journo XB, Roch A, Doddoli C, Marin V, Papazian L, Decamps I, Bregeon F, Thomas P, Auffray JP (2006) Protective ventilation influences systemic inflammation after esophagectomy: a randomized controlled study. Anesthesiology 105(5):911–919
Wolthuis EK, Choi G, Dessing MC, Bresser P, Lutter R, Dzoljic M, van der Poll T, Vroom MB, Hollmann M, Schultz MJ (2008) Mechanical ventilation with lower tidal volumes and positive end-expiratory pressure prevents pulmonary inflammation in patients without preexisting lung injury. Anesthesiology 108(1):46–54. https://doi.org/10.1097/01.anes.0000296068.80921.10
Neumann P, Rothen HU, Berglund JE, Valtysson J, Magnusson A, Hedenstierna G (1999) Positive end-expiratory pressure prevents atelectasis during general anaesthesia even in the presence of a high inspired oxygen concentration. Acta Anaesthesiol Scand 43(3):295–301
Tusman G, Bohm SH, Vazquez de Anda GF, do Campo JL, Lachmann B (1999) ‘Alveolar recruitment strategy’ improves arterial oxygenation during general anaesthesia. Br J Anaesth 82(1):8–13
D’Antini D, Huhle R, Herrmann J, Sulemanji DS, Oto J, Raimondo P, Mirabella L, Hemmes SNT, Schultz MJ, Pelosi P, Kaczka DW, Vidal Melo MF, Gama de Abreu M, Cinnella G, European Society of A., The PVN (2018) Respiratory system mechanics during low versus high positive end-expiratory pressure in open abdominal surgery: a substudy of PROVHILO randomized controlled trial. Anesth Analg 126(1):143–149. https://doi.org/10.1213/ANE.0000000000002192
Futier E, Constantin JM, Paugam-Burtz C, Pascal J, Eurin M, Neuschwander A, Marret E, Beaussier M, Gutton C, Lefrant JY, Allaouchiche B, Verzilli D, Leone M, De Jong A, Bazin JE, Pereira B, Jaber S, Group IS (2013) A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med 369(5):428–437. https://doi.org/10.1056/NEJMoa1301082
Fernandez-Bustamante A, Hashimoto S, Serpa Neto A, Moine P, Vidal Melo MF, Repine JE (2015) Perioperative lung protective ventilation in obese patients. BMC Anesthesiol 15(1):56. https://doi.org/10.1186/s12871-015-0032-x
Carvalho AR, Jandre FC, Pino AV, Bozza FA, Salluh JI, Rodrigues R, Soares JH, Giannella-Neto A (2006) Effects of descending positive end-expiratory pressure on lung mechanics and aeration in healthy anaesthetized piglets. Crit Care 10(4):R122. https://doi.org/10.1186/cc5030
Carvalho AR, Spieth PM, Pelosi P, Vidal Melo MF, Koch T, Jandre FC, Giannella-Neto A, de Abreu MG (2008) Ability of dynamic airway pressure curve profile and elastance for positive end-expiratory pressure titration. Intensive Care Med 34(12):2291–2299. https://doi.org/10.1007/s00134-008-1301-7
Slutsky AS, Ranieri VM (2013) Ventilator-induced lung injury. N Engl J Med 369(22):2126–2136. https://doi.org/10.1056/NEJMra1208707
Suter PM, Fairley B, Isenberg MD (1975) Optimum end-expiratory airway pressure in patients with acute pulmonary failure. N Engl J Med 292(6):284–289. https://doi.org/10.1056/NEJM197502062920604
Carvalho AR, Jandre FC, Pino AV, Bozza FA, Salluh J, Rodrigues R, Ascoli FO, Giannella-Neto A (2007) Positive end-expiratory pressure at minimal respiratory elastance represents the best compromise between mechanical stress and lung aeration in oleic acid induced lung injury. Crit Care 11(4):R86. https://doi.org/10.1186/cc6093
Kano SH, Lanteri CJ, Duncan AW, Sly PD (1994) Influence of nonlinearities on estimates of respiratory mechanics using multilinear regression-analysis. J Appl Physiol 77(3):1185–1197
Bersten AD (1998) Measurement of overinflation by multiple linear regression analysis in patients with acute lung injury. Eur Respir J 12(3):526–532
Rohrer F (1915) Der Strömungswiderstand in den menschlichen Atemwegen und der Einfluss der unregelmässigen Verzweigung des Bronchialsystems auf den Atmungsverlauf in verschiedenen Lungenbezirken. Pflügers Archiv Eur J Physiol 162(5–5):225–299
Carvalho AR, Pacheco SA, de Souza Rocha PV, Bergamini BC, Paula LF, Jandre FC, Giannella-Neto A (2013) Detection of tidal recruitment/overdistension in lung-healthy mechanically ventilated patients under general anesthesia. Anesth Analg 116(3):677–684. https://doi.org/10.1213/ANE.0b013e318254230b
Holm S (1979) A simple sequentially rejective multiple test procedure. Scand J Stat 6(2):65–70
Carvalho AR, Bergamini BC, Carvalho NS, Cagido VR, Neto AC, Jandre FC, Zin WA, Giannella-Neto A (2013) Volume-independent elastance: a useful parameter for open-lung positive end-expiratory pressure adjustment. Anesth Analg 116(3):627–633. https://doi.org/10.1213/ANE.0b013e31824a95ca
Stenqvist O (2003) Practical assessment of respiratory mechanics. Br J Anaesth 91(1):92–105
Brismar B, Hedenstierna G, Lundquist H, Strandberg A, Svensson L, Tokics L (1985) Pulmonary densities during anesthesia with muscular relaxation–a proposal of atelectasis. Anesthesiology 62(4):422–428
Hedenstierna G (2012) Oxygen and anesthesia: what lung do we deliver to the post-operative ward? Acta Anaesth Scand 56(6):675–685
Muscedere JG, Mullen JB, Gan K, Slutsky AS (1994) Tidal ventilation at low airway pressures can augment lung injury. Am J Respir Crit Care Med 149(5):1327–1334. https://doi.org/10.1164/ajrccm.149.5.8173774
Hauber HP, Karp D, Goldmann T, Vollmer E, Zabel P (2010) Effect of low tidal volume ventilation on lung function and inflammation in mice. BMC Pulm Med 10:21. https://doi.org/10.1186/1471-2466-10-21
Jaber S, Coisel Y, Chanques G, Futier E, Constantin JM, Michelet P, Beaussier M, Lefrant JY, Allaouchiche B, Capdevila X, Marret E (2012) A multicentre observational study of intra-operative ventilatory management during general anaesthesia: tidal volumes and relation to body weight. Anaesthesia 67(9):999–1008. https://doi.org/10.1111/j.1365-2044.2012.07218.x
Neumann P, Rothen HU, Berglund JE, Valtysson J, Magnusson A, Hedenstierna G (1999) Positive end-expiratory pressure prevents atelectasis during general anaesthesia even in the presence of a high inspired oxygen concentration. Acta Anaesthesiol Scand 43(3):295–301
Pintado MC, de Pablo R, Trascasa M, Milicua JM, Rogero S, Daguerre M, Cambronero JA, Arribas I, Sanchez-Garcia M (2013) Individualized PEEP setting in subjects with ARDS: a randomized controlled pilot study. Respir Care 58(9):1416–1423. https://doi.org/10.4187/respcare.02068
Amini R, Herrmann J, Kaczka DW (2017) Intratidal overdistention and derecruitment in the injured lung: a simulation study. IEEE Trans Biomed Eng 64(3):681–689. https://doi.org/10.1109/TBME.2016.2572678
Mead J, Collier C (1959) Relation of volume history of lungs to respiratory mechanics in anesthetized dogs. J Appl Physiol 14(5):669–678
Thammanomai A, Hamakawa H, Bartolak-Suki E, Suki B (2013) Combined effects of ventilation mode and positive end-expiratory pressure on mechanics, gas exchange and the epithelium in mice with acute lung injury. PloS ONE 8(1):e53934. https://doi.org/10.1371/journal.pone.0053934
Camilo LM, Avila MB, Cruz LF, Ribeiro GC, Spieth PM, Reske AA, Amato M, Giannella-Neto A, Zin WA, Carvalho AR (2014) Positive end-expiratory pressure and variable ventilation in lung-healthy rats under general anesthesia. PloS ONE 9(11):e110817. https://doi.org/10.1371/journal.pone.0110817
Pecchiari M, Monaco A, Koutsoukou A, Della Valle P, Gentile G, D’Angelo E (2014) Effects of various modes of mechanical ventilation in normal rats. Anesthesiology 120(4):943–950. https://doi.org/10.1097/ALN.0000000000000075
Writing Group for the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial I, Cavalcanti AB, Suzumura EA, Laranjeira LN, Paisani DM, Damiani LP, Guimaraes HP, Romano ER, Regenga MM, Taniguchi LNT, Teixeira C, Pinheiro de Oliveira R, Machado FR, Diaz-Quijano FA, Filho MSA, Maia IS, Caser EB, Filho WO, Borges MC, Martins PA, Matsui M, Ospina-Tascon GA, Giancursi TS, Giraldo-Ramirez ND, Vieira SRR, Assef M, Hasan MS, Szczeklik W, Rios F, Amato MBP, Berwanger O, Ribeiro de Carvalho CR (2017) Effect of lung recruitment and titrated positive end-expiratory pressure (PEEP) vs low PEEP on mortality in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA 318 (14):1335–1345. https://doi.org/10.1001/jama.2017.14171
Amato MB, Meade MO, Slutsky AS, Brochard L, Costa EL, Schoenfeld DA, Stewart TE, Briel M, Talmor D, Mercat A, Richard JC, Carvalho CR, Brower RG (2015) Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med 372(8):747–755. https://doi.org/10.1056/NEJMsa1410639
Neto AS, Hemmes SNT, Barbas CSV, Beiderlinden M, Fernandez-Bustamante A, Futier E, Gajic O, El-Tahan MR, Ghamdi AAA, Günay E, Jaber S, Kokulu S, Kozian A, Licker M, Lin W-Q, Maslow AD, Memtsoudis SG, Miranda DR, Moine P, Ng T, Paparella D, Ranieri VM, Scavonetto F, Schilling T, Selmo G, Severgnini P, Sprung J, Sundar S, Talmor D, Treschan T, Unzueta C, Weingarten TN, Wolthuis EK, Wrigge H, Amato MBP, Costa ELV, de Abreu MG, Pelosi P, Schultz MJ (2016) Association between driving pressure and development of postoperative pulmonary complications in patients undergoing mechanical ventilation for general anaesthesia: a meta-analysis of individual patient data. Lancet Respir Med 4(4):272–280. https://doi.org/10.1016/s2213-2600(16)00057-6
Jandre FC, Modesto FC, Carvalho AR, Giannella-Neto A (2008) The endotracheal tube biases the estimates of pulmonary recruitment and overdistension. Med Biol Eng Comput 46(1):69–73. https://doi.org/10.1007/s11517-007-0227-5
Webb HH, Tierney DF (1974) Experimental pulmonary-edema due to intermittent positive pressure ventilation with high inflation pressures. Protection by positive end-expiratory pressure. Am Rev Respir Dis 110(5):556–565
Kolobow T, Moretti MP, Fumagalli R, Mascheroni D, Prato P, Chen V, Joris M (1987) Severe impairment in lung function induced by high peak airway pressure during mechanical ventilation. An experimental study. Am Rev Respir Dis 135(2):312–315. https://doi.org/10.1164/arrd.1987.135.2.312
Parker JC, Hernandez LA, Longenecker GL, Peevy K, Johnson W (1990) Lung edema caused by high peak inspiratory pressures in dogs. Role of increased microvascular filtration pressure and permeability. Am Rev Respir Dis 142(2):321–328. https://doi.org/10.1164/ajrccm/142.2.321
Rothen HU, Sporre B, Engberg G, Wegenius G, Hogman M, Hedenstierna G (1995) Influence of gas composition on recurrence of atelectasis after a reexpansion maneuver during general anesthesia. Anesthesiology 82(4):832–842
Pelosi P, Ravagnan I, Giurati G, Panigada M, Bottino N, Tredici S, Eccher G, Gattinoni L (1999) Positive end-expiratory pressure improves respiratory function in obese but not in normal subjects during anesthesia and paralysis. Anesthesiology 91(5):1221–1231
Zin WA, Martins MA, Silva PR, Sakae RS, Carvalho AL, Saldiva PH (1989) Effects of abdominal opening on respiratory system mechanics in ventilated rats. J Appl Physiol 66(6):2496–2501. https://doi.org/10.1152/jappl.1989.66.6.2496
Funding
This study was supported by grants from the Brazilian Council for Scientific and Technology Development (CNPq)—140047/2008-5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in this study were in compliance with the “Principles of Laboratory Animal Care” formulated by the National Society for Medical Research and the “Guiding Principles in the Care and Use of Animals” approved by the Council of the American Physiological Society, USA. The present study was approved by the Institutional Animal Care and Use Committee (CEUA CCS, IBCCF-019).
Rights and permissions
About this article
Cite this article
Soares, J.H.N., Carvalho, A.R., Bergamini, B.C. et al. Alveolar Tidal recruitment/derecruitment and Overdistension During Four Levels of End-Expiratory Pressure with Protective Tidal Volume During Anesthesia in a Murine Lung-Healthy Model. Lung 196, 335–342 (2018). https://doi.org/10.1007/s00408-018-0096-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-018-0096-8