Abstract
Background
Acute respiratory distress syndrome (ARDS) is a life-threating condition with high morbidity and mortality. Inflammation is the main factor in the pathogenesis of ARDS. Therefore systemic corticosteroids are a rational therapeutic approach, but the effect of corticosteroids is still unclear. In this study, we looked at the effects of corticosteroids in ventilated sheep with ARDS, induced by lung lavage.
Methods
We performed a prospective, randomised study in 64 ventilated sheep with ARDS, to evaluate the effect of corticosteroids and oxygen concentration on gas exchange and lung injury. Oxygenation index (OI) and ventilation efficacy index (VEI) were calculated to evaluate gas exchange. Lung injury was assessed by inflammatory response in broncho-alveolar lavage fluid (BALF) and plasma and histology of the lung.
Results
OI, VEI, lung inflammation, surfactant production, or lung histology was not influenced by corticosteroids. In the 100 % oxygen groups, OI was higher and total number of cells and disaturated phospholipids were lower in BALF.
Conclusion
Our study showed that corticosteroids did not influence inflammation in early phase ARDS and that hyperoxia aggravated lung injury which could not be modulated by dexamethasone in early phase ARDS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute respiratory distress syndrome (ARDS) is a life-threating condition with high morbidity and mortality [1]. It is characterized by hypoxemia and bilateral infiltrations on X-ray, in the absence of cardiac failure. This is caused by an intense host inflammatory reaction against the pulmonary parenchyma, triggered by insults, like pneumonia, sepsis, or trauma [2, 3]. The pathophysiological basis of ARDS is excessive lung injury due to protracted inflammation characterized by endothelial and epithelial injury, increased vascular permeability with extravasation of plasma and leucocyte infiltration [1]. This inflammation results in proinflammatory cytokine production, increased number of cells and increased total protein levels in the broncho-alveolar lavage fluid (BALF). The epithelial cell injury in ARDS may also result in increased expression of the receptor for advanced glycation end products (RAGE), a key mediator of the inflammatory response to endogenous and exogenous danger signaling [4]. Soluble RAGE (sRAGE) can leak from the lung into plasma due to increased permeability in ARDS. Increased sRAGE, in BALF or plasma, is therefore a biomarker for type I alveolar epithelial cell injury which is correlated with the severity of ARDS [4]. Another factor for lung injury and inflammation in ARDS is the use of mechanical ventilation and oxygen to treat the hypoxemia and inflammation. Oxygen, especially hyperoxia, is known to induce lung injury [5–7]. Since inflammation is the main factor in the pathogenesis of ARDS, systemic corticosteroids are a rational therapeutic approach [1]. Different clinical studies have evaluated the effect of corticosteroids in ARDS, but the results varied [3, 8–20]. The effects of corticosteroids on hyperoxia-induced lung injury have also varied, with positive results in newborns and augmentation of hyperoxic lung injury in adults [19, 20]. The therapeutic effect of corticosteroids in ARDS is therefore unclear.
We hypothesized that corticosteroids in ARDS would decrease the inflammatory response and thereby decrease lung injury. In addition, we hypothesized that hyperoxia would aggravate inflammation and increased lung injury and that corticosteroids amplified this inflammation and lung injury.
To investigate these hypotheses, we used ventilated adult sheep, in which ARDS was induced by lung lavage. These sheep were ventilated with 30 or 100 % oxygen, and respectively, received dexamethasone or placebo. To evaluate the short-term clinical effects of dexamethasone and oxygen, we calculated the oxygenation index (OI) and ventilation efficacy index (VEI). To evaluate the effects on lung injury and inflammation, we determined different parameters in BALF, blood, and performed histology on the lung. Lung injury was defined as an increased number of inflammatory cells, especially neutrophils, increased total protein levels, decreased disaturated phospholipids (DSPL), elevated Interleukin-1β (IL-1β), Interleukin-6 (IL-6), elevated levels of sRAGE, variation in mean alveolar size (MAS), and increased alveolar wall thickness (AWT).
Materials and Methods
The Animal Ethical Committee of the Maastricht University Medical Centre (MUMC+), the Netherlands, approved the study.
Experimental Preparation
Sixty-four adult Texel ewes were anesthetized with intravenous thiopental 25 mg/kg. Then the sheep were intubated orotracheally with a 10-mm cuffed tube and mechanically ventilated (Servo 900 ventilator, Siemens, Germany). The ventilator settings were set to pressure controlled ventilation (PCV), with a peak pressure to maintain a tidal volume (Vt) of 6–8 mL/kg, respiratory rate of 15 breaths per minute, inspiratory time of 50 %, and PEEP 10 cm H2O and FiO2 1.0 or 0.3, according to the study design. A central venous line, for sedation and fluid purposes, and an arterial catheter, for arterial blood pressure measurement and blood sampling, was inserted in the external jugular vein and in the carotid artery. The sheep were sedated and paralyzed during the experiment with intravenous midazolam (5 mg/h), ketamine (8 mg/kg/h), and repeated boluses of pancuronium (0.1 mg/kg) [21]. The sheep were connected to a cardio-respiratory monitor to monitor heart rate, blood pressure, mean arterial pressure, peak inspiratory pressure, mean airway pressure, and tidal volume. After a stabilization period of 30 min, baseline parameters (pre-injury) were obtained (cardio-respiratory parameters, ventilator settings, and a blood sample for gas exchange, IL-6, and sRAGE measurement).
Lung Lavage
Lung injury was established by broncho-alveolar lavage with 500 mL of sterile 0.9 % NaCl at 39 °C per 10 kg bodyweight. This procedure was repeated every 15 min until PaO2 was decreased to 15 kPa at PEEP 10 cm H2O and FIO2 of 1.0 or 0.3, depending on the group [21]. On average, 2–5 lavages were needed to achieve this lung injury. At this point post-lavage parameters (post-injury) were obtained (cardio-respiratory parameters, ventilator settings, and a blood sample for gas exchange).
Randomization
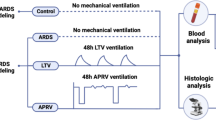
The sheep were randomly assigned into four groups. Group 1: 30 % oxygen without dexamethasone (Dexa –/30 % O2). Group 2: 30 % oxygen with dexamethasone Dexa +/30 % O2). Group 3: 100 % oxygen without dexamethasone (Dexa –/100 % O2). Group 4: 100 % oxygen with dexamethasone (Dexa +/100 % O2).
Experimental Protocol
After inducing lung injury by lung lavage, the sheep received dexamethasone 0.8 mg/kg or placebo intravenously, according to the study design. Then they were ventilated for 3 h and every 30 min blood was analyzed for gas exchange. After 3 h, the animals were euthanized by an intravenous injection of 50 mg/kg thiopental. Thoracotomy was performed and the lungs were removed. The left lung was lavaged with 0.9 % NaCl, and BALF was collected for differential cell counts, measurement of total protein, DSPL, IL-6, and sRAGE. The right lower lobe of the lung was fixed in buffered 4 % formaldehyde, and samples were taken from the dorsobasal (DB), dorsomedial (DM), and dorsocranial (DC) part of the lower lobe for histology [21].
Oxygenation Index (OI) and Ventilation Efficacy Index (VEI)
OI and VEI were calculated from the cardio-respiratory parameters and blood gas analyses before and after lavage and every 30 min during three hours. OI was calculated by multiplying the oxygen fraction times mean alveolar pressure (cm H2O) and dividing this by arterial PO2 (mm Hg) [(FiO2 × MAP)/PaO2]. VEI was calculated by dividing 3,800 by the pressure difference between PEEP and peak pressure (cm H2O) times breathing frequency (breaths/min) times PaCO2 (mm Hg) [3,800/(P × F × PaCO2)].
Inflammatory Cell Count and Differentiation in BALF
A part of the BALF was stored at 4 °C immediately after the experiment. A cell count was performed by mixing this BALF with 0.4 % trypan blue stain, (Gibco Invitrogen Corporation, California, USA) and using the modified Neubauer Hemocytometer (Hirschmann EM Techcolor) [22]. A May-Grünwald-Giemsa staining was performed on the BALF smears, in which all neutrophils, lymphocytes and monocytes were counted up to 200 cells. For each cell type, the total number of cells was calculated per kilogram body weight.
Total Protein in BALF
The protein concentration of the BALF was measured using the Micro BCA Protein Assay Reagent Kit (Thermo Fisher Scientific Inc., Illinois, USA) according to the manufacturer’s instructions. The microtiter plate was read at a wavelength of 562 nm. All photospectroanalyses were done using Multiskan Spectrum hardware and SkanIt RE for MSS 2.2 software (Thermo Electron Corporation, Massachusetts, USA). Translation of optical densities into concentrations was done using GraphPad Prism 5 software (GraphPad Software, California, USA) [23, 24].
DSPL in BALF
DSPL in BALF were measured after 10 min of centrifugation of BALF at 300 g and 4 °C, and then 1 mL of the supernatant BALF was evaporated overnight at 60 °C under continuous nitrogen gas flow. The dry BALF was dissolved in a mixture of carbon tetrachloride and osmium tetroxide and disaturated phospholipids were isolated according to Mason et al. [25]. DSPL were dissolved in chloroform and quantified according to Stewart with some minor modifications as described by Been et al. [26, 27].
IL-1β and IL-6 in BALF and Blood
In the blood samples that taken at the start and at the end of the experiment and in the BALF the concentration of IL-1β and IL-6 were quantified with a commercially available ELISA kit (Thermo Fischer Scientific Inc., Waltham, Massachusetts, USA).
SRAGE in BALF and Blood
Plasma and BALF sRAGE levels were determined by a cross-reacting mouse specific sandwich ELISA (R&D systems, Minneapolis, USA) according to the manufacturer’s instructions [28].
Histology
We evaluated the degree of lung injury using histology in three different locations of the right lower lobe of the lung, by measuring the mean alveolar size (MAS) and alveolar wall thickness (AWT). Samples of the three different locations of the right lower lobe of the lung were imbedded in paraffin, cut to 4 μm slices, deparaffinized in an ethanol series, stained with hematoxylin and eosin, dehydrated, and cover slipped. Per location ten representative microscopic images were made with a 10× magnification using the Leica microscope (Axioskop 4.0; Zeiss) and Leica Qwin Pro version 3.4.0 software (Leica Microsystems, Mannheim, Germany). All images were uploaded and analyzed by Matlab 6.0 software (The Mathworks, Inc. Massachusetts, USA) to measure MAS and AWT.
Statistical Analysis
Statistical analysis was performed using two-way ANOVA with a Bonferroni post hoc test in Graphpad Prism. Data are presented as mean ± SEM, p < 0.05 was considered to be statistically significant.
Results
Baseline Characteristics
Baseline characteristics are shown in Table 1. Three parameters showed significant differences. PO2 pre-lavage in both 100 % oxygen groups was significantly higher compared to both 30 % oxygen groups, due to administered oxygen concentration. PCO2 pre-lavage in the 100 % oxygen without dexamethasone group (Dexa −/100 % O2) was significantly higher compared to both 30 % oxygen groups. Furthermore, in the 100 % oxygen with dexamethasone group (Dexa +/100 % O2) the pCO2 pre-lavage was significantly higher compared to the 30 % oxygen with dexamethasone group (Dexa +/30 % O2). The OI post-lavage in both 100 % oxygen groups was significantly higher compared to both 30 % oxygen groups.
Effect of Dexamethasone and Oxygen on Oxygenation Index and Ventilation Efficacy Index
The OI was significantly higher in both 100 % oxygen groups when compared to the both 30 % oxygen groups, independent of the dexamethasone (Fig. 1). At t = 2.5 h, there was only a significantly higher OI in the 100 % oxygen with dexamethasone group (Dexa +/100 % O2) compared to both 30 % oxygen groups. There was a significantly higher OI at t = 3 h between the 100 % oxygen with dexamethasone group (Dexa +/100 % O2) compared to both 30 % oxygen groups and in the 100 % oxygen without dexamethasone group (Dexa –/100 % O2) compared to the 30 % oxygen without dexamethasone (Dexa –/30 % O2) (Fig. 1). The VEI was not different between the four groups at the different time points (Fig. 2).
Oxygenation index (OI) in time in the different groups. *OI was significantly higher in both 100 % oxygen groups compared to the both 30 % oxygen groups, independent of dexamethasone. **OI was significantly higher in the 100 % oxygen with dexamethasone group compared to both 30 % oxygen groups. ***OI was significantly higher in the 100 % oxygen with dexamethasone group compared to both 30 % oxygen groups and OI was significantly higher in the 100 % oxygen without dexamethasone group compared to the 30 % oxygen without dexamethasone
Effect of Dexamethasone and Oxygen on Lung Inflammation & Surfactant
The total number of cells was significantly lower in the 100 % oxygen groups compared to 30 % oxygen without dexamethasone group (Dexa –/30 % O2) (Fig. 3). Dexamethasone had no significant effect on total numbers of cells in the BALF in the same oxygen groups. DSPL were lower in the 100 % oxygen groups compared to the 30 % oxygen groups, but dexamethasone showed no significant difference (Fig. 4).
Total protein, IL-1β, IL-6, and sRAGE in BALF and IL-1β, IL-6, and sRAGE in blood, showed no significant differences between the four groups (Table 2).
Lung Histology
MAS and AWT showed no differences between the four groups (Table 2). There were also no differences in MAS and AWT between the three different locations of the lung, within the four groups.
Discussion
In our study, we could not show any effect of dexamethasone on clinical parameters, lung injury, or inflammation in BALF or serum. This is in contrast to Dombrowsky and Uhlig’s findings, who found anti-inflammatory effects of dexamethasone in isolated, ventilated mice lungs in a short-term study [29]. There are several differences between their study and our study. We used sheep instead of mice and whole animals instead of isolated lungs. As mentioned above, our study showed no results of dexamethasone in the early phase of ARDS under the standardized conditions of our animal model. In clinical studies, the positive and negative effects of corticosteroids, in the acute phase of ARDS, are still subject of discussion. Meduri et al. showed positive results of methylprednisolone in early severe ARDS with improvement in organ function, duration of mechanical ventilation, and ICU length of stay [8, 9]. Several other studies also showed positive results of low-dose steroids on early phase ARDS [3, 8–13]. On the other hand, there are also studies with no positive results of steroids in early phase ARDS [14–18]. A meta-analysis of Peter et al. in 2008 could not establish a definitive role of corticosteroids in the treatment of ARDS in adults, but trends were found in favor of treatment [1]. The Cochrane review of 2010 could also not conclude the effects of early high-dose corticosteroids due to heterogeneity and incomplete reporting [30]. The reasons of these variable results may be different kind of corticosteroids, different dose and duration of corticosteroids, different kind of patients and different phases of ARDS. Therefore a uniform conclusion of the use of corticosteroids in ARDS cannot be made.
Our study showed negative effects of high dose of oxygen, with or without dexamethasone, with higher OI, lower total of cells and DSPL in BALF in our 100 % oxygen groups. In literature hyperoxia-induced lung injury is a well known and studied model [5]. Hyperoxic exposure has been shown to induce apoptosis, as well as necrosis, in different cell lines, and therefore can explain the lower cell count in our 100 % oxygen groups [5, 31]. Furthermore, in our study DSPL in BALF were lower in both 100 % oxygen groups, probably as a result of more lung injury. Another factor which could explain the lower DSPL concentration in BALF may be alveolar cells death due to hyperoxia [32]. DSPL are the derived measure of surfactant which is produced by alveolar cells. In conclusion, hyperoxia, with 100 % oxygen, induced more lung injury and cell death in our study and clinically resulting in worse oxygenation. This negative effect of hyperoxia was not altered significantly by dexamethasone. Although the levels of sRAGE in BALF are elevated at 72 and 96 h in literature [4], the sRAGE levels in BALF and plasma in our study showed no differences between the groups. The primary injury in our lung lavage model is more due to surfactant depletion than injury to alveolar cells, which could explain the lack of effect observed on sRAGE.
Our study has several limitations which limits the clinical translation. We chose a lung lavage model. This model is a more homogenous lung injury model in which surfactant is depleted, more comparable to ARDS after drowning. This homogenous lung injury gave us the opportunity to do several different tests in different parts of the lung, which represent the injury of the whole lung. Therefore, our results cannot be generalized to human ARDS which is a highly heterogeneous disease group in which different mechanisms and causes of disease are known [33]. All our findings were short-term effects on clinical parameters and lung injury, which we assessed after 3 h in order to limit the confounding effects of long-term mechanical ventilation. Therefore, we cannot extrapolate to long term, more clinical relevant effects, like mortality or total days of mechanical ventilation. We chose an animal study to standardize ARDS, mechanical ventilation, oxygen supply, and treatment time of one dose of systemic dexamethasone. We also decided to define ARDS by a pO2 < 15 kPa, which was done to standardize the conditions in vivo. This, however, implies that the number of lavages per group were different. This may be a cause for different lung injuries in the groups, but there was, however, no significant difference within the 30 % oxygen and 100 % oxygen subgroups. The extrapolation to other corticosteroids, like methylprednisolone, or other doses, higher or lower, is very speculative. Dose studies and comparison of the different type of corticosteroids in longer exposure of ARDS should be done to identify effects of corticosteroids in later phases of ARDS.
Conclusion
Our study showed that corticosteroids did not influence inflammation in early phase ARDS and that hyperoxia aggravated lung injury, which could not be modulated by dexamethasone in early phase ARDS.
References
Peter JV, John P, Graham PL et al (2008) Corticosteroids in the prevention and treatment of acute respiratory distress syndrome (ARDS) in adults: meta-analysis. BMJ 336:1006–1009
The ARDS Definition Task Force (2012) Acute respiratory distress syndrome. the Berlin definition. JAMA 307(23):2526–2533
Tang BMP, Craig JC, Eslick GD et al (2009) Use of corticosteroids in acute lung injury and acute respiratory distress syndrome: a systematic review and meta-analysis. Crit Care Med 37:1594–1603
Guo WA, Knight PR, Raghavendran K (2012) The receptor for advanced glycation end products and acute lung injury/acute respiratory distress syndrome. Intensive Care Med 38:1588–1598
Pagano A, Barazzone-Argiroffo (2003) Alveolar cell death in hyperoxia-induced lung injury. Ann NY Acad Sci 1010:405–416
Gore A, Muralidhar M, Espey MG et al (2010) Hyperoxia sensing: from molecular mechanisms to significance in disease. J Immunotoxicol 7(4):239–254
Barazzone-Argiroffo C, Pagano A, Junge C et al (2002) Glucocorticoids aggrevate hyperoxia-induces lung injury through decreased nuclear factor-κB activity. Am J Physiol Lung Cell Mol Physiol 284:L197–L204
Meduri GU, Golden E, Freire AX et al (2007) Methylprednisolone infusion in early severe ARDS results of a randomized controlled trail. Chest 131:954–963
Meduri GU, Annane D, Chrousos GP et al (2009) Activation and regulation of systemic inflammation in ARDS. Rationale for prolonged glucocorticoid therapy. Chest 136:1631–1643
Meduri GU, Marik PE, Chrousos GP et al (2008) Steroid treatment in ARDS: a critical appraisal of the ARDS network trail and recent literature. Int Care Med 34:61–69
Wang XQ, Zhou X, Zhou Y et al (2008) Low-dose dexamethasone alleviates lipopolysaccharide-induced acute lung injury in rats and up regulates pulmonary glucocorticoid receptors. Respirology 13:772–780
Lee HS, Lee JM, Kim MS et al (2005) Low-dose steroid therapy at an early phase of postoperative acute respiratory distress syndrome. Ann Thorac Surg 79:405–410
Annane D, Sebille V, Bellissant E et al (2006) Effect of low doses of corticosteroids in septic patients with or without early acute respiratory distress syndrome. Crit Care Med 34:22–30
Brun-Buisson C, Richard JCM, Mercat A et al (2011) Early corticosteroids in severe influenza A/H1N1 pneumonia and acute respiratory distress syndrome. Am J Resp Crit Care Med 183:1200–1206
Xu T, Qiao J, Zhao L et al (2009) Effect of dexamethasone on respiratory distress syndrome induced by the H5N1 virus in mice. Eur Respir J 33:852–860
Agarwal R, Nath A, Aggarwal AN, Gupta D (2007) Do glucocorticoids decrease mortality in acute respiratory distress syndrome? A meta-analysis. Respirology 12:585–590
Thompson BT (2010) Corticosteroids for ARDS. Minerva Anestesiol 76:441–447
Deal EN, Hollands JM, Schramm GE, Micek ST (2008) Role of corticosteroids in the management of acute respiratory distress syndrome. Clin Ther 30:787–799
Ramsay PL, Smith CV, Geske RS et al (1998) Dexamethasone enhancement of hyperoxic lung inflammation in rats independent of adhesion molecule expression. Biochem Pharmacol 56(2):259–268
Town GI, Phillips GJ, Landreau M et al (1993) Dexamethasone treatment fails to reduce oxygen-induced lung injury in the preterm guinea pig. Biochem Pharmacol 46:1565–1572
Engel M, Nowacki RME, Reiss LK et al (2013) Comparison of recruitment manoeuvres in ventilated sheep with acute respiratory distress syndrome. Lung 191(1):77–86
Kramer BW, Moss TJ, Willet KE et al (2001) Dose and time response after intraamniotic endotoxin in preterm lambs. Am J Respir Crit Care Med 164:982–988
Kramer BW, Ladenburger A, Kunzmann et al (2009) Intravenous lipopolysaccharide-induced pulmonary maturation and structural changes in fetal sheep. Am J Obstet Gynecol 200(2):195.e1–10
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ (1951) Protein measurement with folin phenol reagent. J Biol Chem 193:265–275
Mason RJ, Nellenbogen J, Clements JA (1976) Isolation of disaturated phosphatidylcholine with osmium tetroxide. J Lipid Res 17(3):281–284
Stewart JCM (1980) Colometric determination of phospholipids with ammonium ferrothiocyanate. J Anal Biochem 104:10–14
Been JV, Zoer B, Kloosterboer N et al (2010) Pulmonary vascular endothelial growth factor expression and desaturated phospholipid content in a chicken model of hypoxia-induced fetal growth restriction. Neonatology 97:183–189
Hanssen NM, Engelen L, Ferreira I et al (2013) Plasma levels of advanced glycation endproducts Nepsilon-(carboxymethyl)lysine, Nepsilon-(carboxyethyl)lysine, and pentosidine are not independently associated with cardiovascular disease in individuals with or without type 2 diabetes: the Hoorn and CODAM studies. J Clin Endocrinol Metab 98(8):E1369–E1373
Dombrowsky H, Uhlig S (2007) Steroids and histone deacetylase in ventilation-induced gene transcription. Eur Respir J 30:865–877
Adhikari NKJ, Burns KEA, Meade MO, Ratnapalan M (2010) Pharmacologic therapies for adults with acute lung injury and acute respiratory distress syndrome (review). Cochrane Libary 7
Tang PS, Mura M, Seth R, Liu M (2008) Acute lung injury and cell death: how many way scan cells die? Am J Physiol Cell Mol Physiol 294:L632–L641
Huang YC, Caminiti SP, Fawcett TA et al (1994) Natural surfactant and hyperoxic lung injury in primates. I. Physiology and biochemistry. J Appl Physiol 76:991–1001
Frutos-Vivar F, Ferguson ND, Esteban A (2006) Epidemiology of acute lung injury and acute respiratory distress syndrome. Semin Respir Crit Care Med 27(4):327–336
Conflict of interest
All the authors have no conflict of interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Engel, M., Nowacki, R.M.E., Boden, P. et al. The Effects of Dexamethasone and Oxygen in Ventilated Adult Sheep with Early Phase Acute Respiratory Distress Syndrome. Lung 193, 97–103 (2015). https://doi.org/10.1007/s00408-014-9670-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-014-9670-x