Abstract
Purpose
Middle turbinate (MT) surgery is extremely common during endoscopic sinus surgery procedures, though no agreement exists on which techniques provide the best outcomes. This PRISMA-compliant systematic review aims to assess which MT surgery technique yields the least postoperative adverse effects and the best objective and subjective outcomes.
Methods
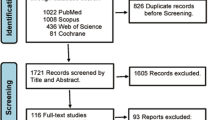
A comprehensive search criteria was conducted in multiple databases up to July 3, 2023, to identify studies reporting surgical treatments of the MT. After screening and quality assessment, 14 articles were included for analysis. Data on patients demographics, surgical approaches, postoperative treatment and follow-up, objective and subjective outcomes were extracted and reviewed.
Results
Out of 173 unique papers identified, 14 articles met the inclusion criteria, predominantly randomized controlled trials (n = 9). Antero-inferior middle turbinectomy was the predominant surgical approach. Most studies evaluated results with postoperative endoscopy, a superior outcome was documented in the intervention group (ten out of eleven cases). In four out five studies using the SNOT-22, the treatment group was associated with a statistically significant improvement. Olfactory questionnaires highlighted superior olfactory outcome in two out of three studies. The UPSIT score revealed no significant difference between groups. Objective olfactory assessments favored treatment groups in both studies utilizing olfactometry.
Conclusions
It seems that a partial MT surgical approach consistently yields subjective and objective improvements compared to conservative measures, also suggesting a positive impact on smell function. Despite it appears that better outcomes with fewer complications are consistently achieved with partial techniques, it remains challenging identifying which partial technique surpasses the others, due to significant heterogeneity among the studies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Middle turbinate (MT) plays a crucial role in the mechanism of nasal respiration, by regulating nasal airflow in response to autonomic nervous system stimulation. It modulates the turgidity of the cavernous corpses through the nasal cycle. However, pathological processes affecting the MT, such as concha bullosa [1], polypoid degeneration, paradoxical MT [2], and less common occurrences like duplication and triplication of the middle turbinate [3], can lead to nasal obstruction of various grade.
During nasal surgery, the rationale and techniques for septum and paranasal sinusesapproaches are generally unanimous. However, there is ongoing controversy regarding the surgical techniques and degree of radicality of MT approaches. Some surgeons, though their numbers have decreased in recent years, advocate for more radical approaches, such as total middle turbinectomy [4]. This approach is believed to offer benefits such as reduced incidence of postoperative synechiae, increased respiratory space, and improved postoperative visualization of the paranasal ostia.
Conversely, proponents of a less radical surgical approach highlight the MT significance as a fundamental anatomical landmark, its function in humidifying inspired air, and, to a lesser extent, contributing to olfactory function [5].
As a result, contemporary MT surgical techniques are extremely varied, ranging from total middle turbinectomy, to partial anterior or inferior middle turbinectomy, medial or lateral laminectomy [6], techniques involving medialization of the MT through the use of transeptal sutures [7], the placement of a stent in the middle meatus [8], and, not least, bolgerization [9].
As no consensus yet exists on which techniques yield the best results and grant the best balance towards surgical and functional risks, we aimed with this systematic review to analyse current knowledge about surgical techniques for MT, and compare them in terms of functional outcomes, incorporating subjective, objective and questionnaire-based assessments.
Materials and methods
A PRISMA-compliant review was performed between July 2023 and September 2023 after protocol registration on the Open Science Framework platform (registration available at https://archive.org/details/osf-registrations-uj2sq-v1). The review was designed to collect all original papers focusing on MT surgery in humans written in English, Italian, German, French, or Spanish.
On July 3, 2023, we systematically searched the MEDLINE, Scopus, Cochrane Library, Embase, Web of Science, and ClinicalTrials.gov databases using the following search string:
middle turbinectomy” OR “middle turbinate surgery” OR “middle turbinoplasty.
We included all original papers that collected original data on MT surgery in humans providing subjective, objective, and/or questionnaire-based results, regardless of the surgical technique used. There were no restrictions on the number of participants for every study or in the study design, though case reports were excluded.
The Population, Intervention, Comparison, Outcomes, and Study (PICOS) framework for the review was defined as follows:
-
P:
patients undergoing surgery on the MT
-
I:
any MT surgical treatment
-
C:
different techniques of MT surgery
-
O:
any reported subjective or objective outcome pertaining to nasal function
-
S:
all original studies excluding case reports
Studies identified through database searches underwent two selection stages, both performed by two independent authors. The first selection stage was performed on titles and abstracts. All studies proposed for inclusion by at least one author were considered eligible for the second selection stage, as to maximize inclusivity. The second selection stage was performed on full-texts, and any disagreement on the final inclusion of a study in the systematic review was solved by consensus.
All studies selected during the second review round underwent quality assessment. Case series and cohort studies were evaluated according to the “National Heart, Lung and Blood Institute Study Quality Assessment Tools” (NHI-SQAT). Articles were categorized as “Good” if they met at least 80% of the NHI-SQAT criteria, “Fair” if they met between 50% and the 80% of the criteria and “Poor” if the criteria met were less than 50%, using the methodology we consolidated in prior mixed-level-of-evidence reviews [10,11,12,13]. Randomized controlled trials (RCTs) were evaluated according to the “Cochrane Risk-of-Bias-Tool”. Levels of evidence were determined following the “Oxford Centre for Evidence-based Medicine” (OCEBM) guide. All studies of good or fair quality according to the NHI-SQAT rating or without significant risk of bias according to the Cochrane tool were included in the final systematic review.
For each included study, we collected the following data: type of study, number of patients included and number of MT treated per patient, male-to-female ratio, age of the participants, type of surgical treatment, surgical indications, post-surgery treatment type (if any), follow-up duration, postoperative endoscopic evaluation, with particular attention to the prevention of synechiae formation, middle turbinate medialization and its impact on olfactory fossa and osteomeatal complex (OMC) accessibility, reduction in middle turbinate hypertrophy or pneumatization (if present), and reported nasal outcomes. Two authors independently extracted and evaluated data, with disagreements resolved through consensus.
Due to the significant heterogeneity in the study populations and endpoints, a meta-analysis was not planned or performed a posteriori.
Results
Out of the 173 unique papers identified, two authors conducted a comprehensive full-text evaluation of 41 scientific papers. Subsequently, 14 articles published between 1995 and 2023 were retained for evaluation and potential inclusion in the systematic review as illustrated in Fig. 1.
Nine articles were randomized controlled trials, three were cohort studies and two were prospective case series. The level of evidence according to the OCEBM score was IV (n = 2), II (n = 3) and I (n = 9). Evaluation of prospective case series and the cohort studies, according to the NHI-SQAT, indicates the articles as “good” (n = 1) and “fair” (n = 4) respectively, with none classified under the category of “low” level of quality. The RCTs were classified, based on the “Cochrane Risk-of-Bias Tool”into “low concerns risk of bias” (LROB) (n = 5) and “some concerns risk of bias” (SROB) (n = 4), no article was considered at “high concerns risk of bias” (HROB). Moreover, no significant biases toward the specific objective of our systematic review emerged. The list of study types and corresponding quality ratings is presented in Table 1.
Data related to the surgical approach to the MT were extracted from 1016 patients, 458 males, 388 females, and 170 patients of unspecified gender. The total number of surgically treated MTs was 1903. The age range of treated patients was 15 to 87 years.
Various surgical techniques were analysed in the articles considered, with antero-inferior middle turbinectomy being the predominant approach described in eight studies. Submucosal middle turbinectomy was employed in one study, total middle turbinectomy in three cases while lateral laminectomy, medial laminectomy, and preservation of the MT were compared in one case. Two works identified generically the surgical approach as “middle turbinectomy” without any further details about the portion of the turbinate surgically removed.
Concerning post-surgical management, antibiotic therapy was prescribed in five cases, nasal washes with saline solution were mentioned in eight works, nasal spray corticosteroids in six, and outpatient nasal toileting in three cases. Postoperative treatment details were not specified in five papers. Demographics, clinical data, surgical techniques, and postoperative treatments are shown in Table 2, with afollow-up ranging from 3 to 50 months.
In most studies, postoperative evaluation was conducted using nasal endoscopy (n = 11), in ten out of eleven cases, a superior endoscopic outcome was documented in the MT surgery group versus control groups, regardless of the technique used. The improvement was noted in terms of reduction in nasal obstruction, width of the olfactory cleft, and reduction of postoperative synechiae.
We collected the surgical indications for middle turbinate surgery and categorized the endoscopic findings from eleven studies with postoperative nasal endoscopy intro three areas: prevention of synechiae formation, access of the middle meatus and permeability of the olfactory cleft (OC), and reduction in middle turbinate size when surgery aimed to relieve obstructive bulk. Notably, only nine studies reported these findings. Synechiae formation was evaluated in eight studies. None reported a reduction in adhesions in the intervention groups (partial or total middle turbinectomy). Notably, only three of these studies demostrated statistically significant findings.
Endoscopy of the middle meatus and OC permeability was notable in eight studies. Seven reported a better endoscopic appearance of the middle turbinate in the intervention groups, with five demonstrating significantly better outcomes compared to control groups, regardless the technique used. At last none of the 14 studies seems to report reduction of the concha bullosa or the obstructive bulk of the middle turbinate.
Only two studies evaluated postoperative imaging with computed tomography (CT). Both reported improved CT findings, with one study favoring submucosal middle turbinectomy and the other favoring total middle turbinectomy. Table 3 summarizes the endoscopic and imaging findings.
Among the papers under review, the use of questionnaires was well represented, with SNOT-22 (n = 5, one of which in its SNOT-20 variant) being the most frequently employed. SNOTquestionnaire highlighted a statistically significant improvement in the treatment groups in four out of five studies.
Olfactory evaluation was performed with objective tests (olfactometry) and subjective (questionnaires). Concerning the latter, two out of three studies reported a superior olfactory outcome in the treatment group. In one instance, testing the subjects with the “University of Pennsylvania Smell Identification Test” (UPSIT), revealed no significant difference. Both studies testing participants with olfactometry point out a better objective result in the treatment group subjected to total turbinectomy. The second study demonstrated a favorable outcome in treatment groups, comparable between medial and lateral laminectomy, as opposed to the control group. Table 4 summarizes the results of the surgical treatments.
Discussion
Our systematic review aimed to investigate whether a superior surgical approach to the MT exists, in terms of functional outcomes, nasal obstruction, and postoperative complications. To the best of our knowledge, this is the first scientific article attempting to explore this aspect of a crucial area in endoscopic rhinosurgery.
Analysis of the international literature clearly highlights how the debate has evolved over the years, shifting away from more radical surgical approaches, such as the total turbinectomy [14], which advocated for better outcomes in terms of reduced postoperative synechiae, improved visualization of the paranasal sinuses in the postoperative phase, and increased respiratory space [15]. There has been a progressive shift towards partial approaches, acknowledging the importance of the MT structure in humidifying inspired air and olfactory function [16]. Moreover, in endoscopic surgery, reliance on anatomical landmarks is crucial; the absence of the MT during revision surgery increases the risk of intra e postoperative complications [17] and the potential to cause atrophic rhinitis [18].
Several partial middle turbinectomy techniques exist beyond total removal. One example is antero-inferior middle turbinectomy, which removes the anterior third of the turbinate to reduce obstructive bulk while preserving the anatomical landmark However, this approach carries an increased risk of synechiae formation [5]. Submucosal middle turbinoplasty preserves the mucosa while removing the bone portion of the turbinate [19]. Medial and lateral laminectomy consists in the removal of the lateral portion of a middle turbinate with increased volume, its advantages and disadvantages are similar to those of partial middle turbinectomy [6]. Middle turbinate medialization aims to reposition the middle turbinate laterally to improve airflow: various techniques exist, including: temporary transseptal suture with adsorbable material [4], metallic clips, although this potentially could lead to synechiae and OC dysventilation [7], interposition of U-shaped synthetic implants (Es. Sylastic) through the OMC [8] or the positioning of non-adsorbable nasal packing [20]. Finally, creating a controlled adhesion between the middle turbinate and septum has been attempted. However, this can alter airflow and often leads to unpredictable adhesion size [21].
Regarding the articles in this systematic review, only two focused on total middle turbinectomy. Both are randomized controlled trials (RCTs). The study by Hudon et al. compares total middle turbinectomy in one nasal fossa while preserving the contralateral turbinate in 16 patients. No evidence of better endoscopic postoperative evaluation (Perioperative Sinus Endoscopy - POSE) was observed six months after surgery in terms of paranasal sinus patency and nasal airspace [22]. It is important to note the limited sample size in this study. The other article, evaluating total middle turbinectomy by Su et al., indicates a statistically significative difference (p < 0,001) in terms of endoscopic aspect (Lund-Kennedy score) and paranasal sinuses patency (Lund-Mackay score) in favor of the resection group in a series of 50 patients compared to their controls. The questionnaire SNOT-20 was utilized to assess the subjective perception of nasal functionality, demonstrating a statistically significant improvement in the resection group. It is noteworthy that olfactometry, conducted at two, four, and six months after surgery, also shows significantly better results in the total turbinectomy group. Regarding postoperative complications, the control group appears to be more affected, suggesting, despite conflicting opinions, that total middle turbinectomy could be considered a safe technique in selected cases [23].
Kumral et al. conducted a randomized controlled trial comparing two groups of patients subjected to medial and lateral laminectomy, respectively, with a third control group. Evaluation of 72 patients three months after surgery demonstrated statistically significant improvements in symptoms and quality of life (assessed via SNOT-22), olfactometry, and peak nasal inspiratory flow (PNIF) in both intervention groups compared to the preoperative phase. Interestingly, medial laminectomy yielded comparable results to lateral laminectomy, suggesting that the former is not associated with greater osteomeatal complex (OMC) obstruction or a higher likelihood of iatrogenic sinusitis [6].
Regarding submucosal middle turbinectomy, Akiyama et al. conducted a prospective cohort study involving 38 patients, identifying a statistically significant difference (p < 0,001) in olfactory cleft patency favoring the intervention group. The study also noted differences in the endoscopic postoperative appearance and synechiae formation, with better results in the intervention group, although without statistical significance [19].
In two of the 14 articles, the surgical technique used is termed “partial turbinoplasty”. The first, by Gopi et al., was a prospective cohort study involving 30 patients who underwent unilateral partial middle turbinoplasty, with the contralateral nasal fossa serving as a control group. The results showed statistically significant improvements in the intervention group in terms of postoperative synechiae formation and nasal obstruction, with a non-significant reduction in anterior rhinorrhea [24]. The second article, analysing partial middle turbinoplasty in 45 patients by Delarestaghi et al., was a randomized controlled trial highlighting a statistically significant improvement in postoperative SNOT-22 questionnaire scores compared to the control group, consistent with the trend elucidated by Kumral et al. [25].
The final section of the review encompasses eight articles considering partial anterior or antero-inferior middle turbinectomy. Organized according to study structure, two were prospective case series. The first, by Cook et al., included 31 patients evaluated with preoperative and postoperative rhinomanometry. The authors noted a statistically significant improvement in results, even when considering the subgroup of 16 patients not undergoing concomitant septoplasty, thus removing a potential confounding factor [26]. The second prospective case series, conducted by Mariano et al., involved 27 patients who were assessed preoperatively and postoperatively using the “University of Pennsylvania Smell Identification Test” (UPSIT). It is one the only two studies that did not highlight an improvement in olfactory functionality from the preoperative phase. However, the comparable results with the preoperative phase suggest that although the procedure did not improve olfactory functionality, it also did not worsen it [27].
In a prospective cohort study by Murali et al., evaluating antero-inferior turbinoplasty, 40 patients underwent the technique, with two other groups for comparison: one group underwent medialization with transeptal suture of the MT, and a third served as a control group. Endoscopic evaluation using Lund-Kennedy score and nasal fossa patency showed better results in the two intervention groups. The SNOT-22 questionnaire confirmed a statistically significant reduction in symptoms in the intervention groups. The authors also noted postoperative synechiae formation, with only three cases occurring in the control group. Furthermore, they observed a minimal improvement when comparing middle turbinoplasty with medialization, suggesting that the benefit of the transeptal suture may be limited over time [28].
The last five studies were RCTs, four of which considered nasal endoscopy as a parameter evaluated postoperatively. Tomoum et al., investigated the patency of the paranasal sinuses in 60 patients using the Likert scale, along with quality of life using the SNOT-22 questionnaire, both pre and postoperatively in both intervention and control groups. Both parameters showed improvement in the intervention group, with statistically significant and non-significant differences observed for the Likert scale and SNOT-22, respectively [29]. Similarly, Lasheen et al. evaluated endoscopically 30 patients using an arbitrary scoring system to assess postoperative appearance and paranasal sinus patency, concluding their article by highlighting a statistically significant improvement in the antero-inferior middle turbinectomy group [30].
In the study by Krishna Santosh et al., 50 patients were evaluated with a questionnaire, both pre and postoperatively, assessing nasal obstruction, anterior rhinorrhea, headache, olfactory perception, and facial pain. Each category was then compared between the antero-inferior middle turbinectomy and the control group, with a statistically significant improvement observed for the former (p < 0,001) [31]. Havas et al. also investigated a group of 509 patients using a smell questionnaire, alongside endoscopic evaluation of postoperative synechiae and the need for revision surgery. The intervention group undergoing antero-inferior middle turbinectomy showed statistically significant improvement in all categories assessed [32]. The final study by Gulati et al. employed a questionnaire similar to that utilized by Krishna Santosh et al., with minor variations in the parameters assessed, including nasal obstruction, anterior rhinorrhea, headache, posterior rhinorrhea, and sneezing. Both the intervention and control groups demonstrated improvement in the postoperative phase; however, once again, the difference was statistically significant for the group of 20 patients subjected to anterior middle turbinectomy. Additionally, the authors investigated synechiae formation and patency of the middle meatal antrostomy, revealing a non-statistically significant improvement [33].
An analysis of the results underscores that in nearly all cases, a partial approach to theMT appears to enhance subjective symptomatology and objective postoperative evaluation compared to a conservative approach. Notably, in the two studieswhere a significant improvement in the intervention group was not observed, assessing smell function using UPSIT score and endoscopic appearance evaluated with the Lund-Kennedy score, it is noteworthy that while there wasn’t a marked improvement in the intervention groups respect to the control groups, there was no deterioration compared to the preoperative phase or the control groups, highlighting the safety of these techniques.
A crucial factor in evaluating middle turbinate surgery effectiveness is the chosen postoperative assessment technique. Our review identified limitations in both common approaches: only two of 14 studies utilized CT scans for re-evaluation, likely due to cost and additional radiation exposure for patients, while easier to implement, only 11 out 14 studies reported an endoscopic follow-up. Furthermore of those reporting endoscopy, only nine described the surgical effectiveness. Despite these limitations, seven studies reported statistically significant improvements in either synechia reduction, middle meatus access, o olfactory cleft access in the intervention groups (regardless of the technique). This represents half of the studies reviewed.
Acknowledging the limitations of our analysis, several key points must be considered: firstly, there was considerable heterogeneity in the surgical techniques employed, encompassing both total approaches and partial turbinectomies. While a partial resection of the MT may appear advisable due to its significance as an anatomical landmark, it remains unclear which techniques yield fewer complications and superior outcomes. Skepticism persists regarding total turbinectomy, as only one out of two studies evaluated underscored its effectiveness and safety. Conversely, for partial approaches, none of the cited studies reported a higher incidence of postoperative complications in the intervention groups compared to the control groups.
In conclusion, a partial resection approach to theMT yields improved respiratory outcomes compared to conservatory approaches without an associated increase in postoperative risks. Moreover, there is no adverse impact on smell function, and in certain cases, improvement was observed, as evidence in several reviewed articles. Nevertheless, it is imperative to recognize that nasal pathology often entails additional issues such as nasal septum deviation, chronic rhinosinusitis with or without polyposis, complicating the attribution of postoperative benefits solely to the MT approach. Given the challenges in comparing different studies due to the heterogeneity in evaluating postsurgical effectiveness, standardizing methods for assessing in particular with objective methods as endoscopic, and imaging techniques beyond olfactometric, and questionnaire-based outcomes in future studies would be advantageous.
Conclusion
In conclusion, while the anatomical variations of the MT may impact nasal obstruction and potentially increase the risk of rhinosinusitis, the partial MT surgical approach consistently yields subjective and objective improvements compared to conservative measures. Furthermore, there is evidence suggesting a positive impact on smell function without any indication of deterioration in the reviewed studies. However, due to the significant heterogeneity among the studies, identifying a single surgical technique that surpasses others remains challenging. Nevertheless, it appears that better outcomes with fewer complications are consistently achieved by favoring partial techniques over total middle turbinectomy.
References
Kalaiarasi R, Ramakrishnan V, Poyyamoli S (2018) Anatomical Variations of the Middle Turbinate Concha Bullosa and its Relationship with Chronic Sinusitis: A Prospective Radiologic Study, Int Arch Otorhinolaryngol, vol. 22, no. 3, p. 297, Jul. https://doi.org/10.1055/S-0038-1625978
Belcher RH, Ikeda AK, Delgaudio JM (2018) Apr., Remodeling of the Paradoxical Middle Turbinate: Preserving Function While Gaining Access, vol. 32, no. 2, pp. 98–100, https://doi.org/10.1177/1945892418765002
Lechien JR, Rodriguez A, Kampouridis S, Horoi M (2019) Rare anatomic variation: Nasopharyngeal middle turbinate, Clin Case Rep, vol. 7, no. 9, pp. 1714–1716, Sep. https://doi.org/10.1002/CCR3.2344
Chen W, Wang Y, Bi Y, Chen W (Jan. 2015) Turbinate-septal suture for middle turbinate medialization: a prospective randomized trial. Laryngoscope 125(1):33–35. https://doi.org/10.1002/LARY.24820
Banfield GK, McCombe A (Feb. 1999) Partial resection of the Middle Turbinate at Functional endoscopic sinus surgery. BMJ Mil Health 145(1):18–19. https://doi.org/10.1136/JRAMC-145-01-05
Kumral TL et al (May 2015) Comparison of two partial middle turbinectomy techniques for the treatment of a concha bullosa. Laryngoscope 125(5):1062–1066. https://doi.org/10.1002/LARY.25065
Hanna BMN, Kilty SJ (2012) Middle turbinate suture technique: a cost-saving and effective method for middle meatal preservation after endoscopic sinus surgery, J Otolaryngol Head Neck Surg, vol. 41, no. 6, pp. 407–412, Dec. https://doi.org/10.2310/7070.2012.00058
Jae YL, Seung WL (2007) Preventing Lateral Synechia Formation After Endoscopic Sinus Surgery With a Silastic Sheet, Arch Otolaryngol Head Neck Surg, vol. 133, no. 8, pp. 776–779, Aug. https://doi.org/10.1001/ARCHOTOL.133.8.776
Bolger WE, Kuhn FA, Kennedy DW (1999) Middle Turbinate Stabilization After Functional Endoscopic Sinus Surgery: The Controlled Synechiae Technique, Laryngoscope, vol. 109, no. 11, pp. 1852–1853, Nov. https://doi.org/10.1097/00005537-199911000-00025
Martino B et al (Oct. 2022) Conversion rates in robotic thyroid surgery: a systematic review and meta-analysis. Int J Med Rob + Comput Assist Surg 18(5). https://doi.org/10.1002/RCS.2427
Bulfamante AM et al (Feb. 2023) Artificial intelligence, machine learning, and deep learning in rhinology: a systematic review. Eur Arch Otorhinolaryngol 280(2):529–542. https://doi.org/10.1007/S00405-022-07701-3
Saibene AM et al (2023) Aug., Sirolimus treatment for paediatric head and neck lymphatic malformations: a systematic review, European Archives of Oto-Rhino-Laryngology, vol. 280, no. 8, p. 3529, https://doi.org/10.1007/S00405-023-07991-1
Cozzi AT et al (Oct. 2023) Intraoperative neuromonitoring does not reduce the risk of Temporary and definitive recurrent laryngeal nerve damage during thyroid surgery: a systematic review and Meta-analysis of endoscopic findings from 73,325 nerves at risk. J Pers Med 13(10):1429. https://doi.org/10.3390/JPM13101429/S1
Kennedy DW (1998) Middle Turbinate Resection: Evaluating the Issues—Should We Resect Normal Middle Turbinates? Arch Otolaryngol Head Neck Surg, vol. 124, no. 1, pp. 107–107, Jan. https://doi.org/10.1001/ARCHOTOL.124.1.107
Choby GW, Hobson CE, Lee S, Wang EW (2014) Clinical effects of middle turbinate resection after endoscopic sinus surgery: a systematic review, Am J Rhinol Allergy, vol. 28, no. 6, pp. 502–507, Nov. https://doi.org/10.2500/AJRA.2014.28.4097
Giacchi RJ, Lebowitz RA, Jacobs JB (2000) Middle turbinate resection: issues and controversies. Am J Rhinol 14(3):193–197. https://doi.org/10.2500/105065800782102726
Revision endoscopic sinus surgery the Thomas Jefferson University experience - PubMed. Accessed: Oct. 25, 2023. [Online]. Available: https://pubmed.ncbi.nlm.nih.gov/9557409/
Talmadge J, Nayak JV, Yao W, Citardi MJ (2019) Management of Postsurgical Empty Nose Syndrome, Facial Plast Surg Clin North Am, vol. 27, no. 4, pp. 465–475, Nov. https://doi.org/10.1016/J.FSC.2019.07.005
Akiyama K, Samukawa Y, Takahashi S, Ouchi Y, Hoshikawa H (Aug. 2018) Clinical effects of submucosal middle turbinectomy for eosinophilic chronic rhinosinusitis. Auris Nasus Larynx 45(4):765–771. https://doi.org/10.1016/J.ANL.2017.11.013
Jebeles JA, Hicks JN (1993) Feb., The Use of Merocel® for Temporary Medialization of the Middle Turbinate During Functional Endoscopic Sinus Surgery, vol. 72, no. 2, pp. 145–148, https://doi.org/10.1177/014556139307200209
Friedman M, Landsberg R, Tanyeri H (2000) Middle Turbinate Medialization and Preservation in Endoscopic Sinus Surgery, Otolaryngology–Head and Neck Surgery, vol. 123, no. 1, pp. 76–80, Jul. https://doi.org/10.1067/MHN.2000.105921
Hudon MA, Wright ED, Fortin-Pellerin E, Bussieres M (Nov. 2018) Resection versus preservation of the middle turbinate in surgery for chronic rhinosinusitis with nasal polyposis: a randomized controlled trial. J Otolaryngol Head Neck Surg 47(1). https://doi.org/10.1186/S40463-018-0313-8
Su B, Han Q, Xi X, Zhou Z Effect of modified endoscopic sinus surgery combined with middle turbinate resection on olfactory function and stress response in patients with refractory chronic rhinosinusitis with nasal polyps. Am J Transl Res, 14, 2, pp. 1279–1287, 2022, Accessed: Oct. 28, 2023. [Online]. Available: www.ajtr.org
Gopi A, Nishant MB, Rajamma KB (2017) Comparative study between Middle Meatal Antrostomy with and without partial middle turbinectomy in patients with chronic sinusitis. Int J Sci Study 5(4):15–20. https://doi.org/10.17354/ijss/2017/327
Delarestaghi MM et al (2020) Evaluation of the effect of endoscopic partial middleturbinectomy surgery on the quality of life of patients with chronic rhinosinusitis and nasal polyps. Rhinology 58(3):208–212. https://doi.org/10.4193/RHIN19.258
Cook PR, Begegni A, Bryant WC, Davis WE (Oct. 1995) Effect of partial middle turbinectomy on nasal airflow and resistance. Otolaryngol Head Neck Surg 113(4):413–419. https://doi.org/10.1016/S0194-59989570078-1
Mariano FC, Hamerschmidt R, Soares CMC, Moreira AT (2018) The Middle Turbinate Resection and Its Repercussion in Olfaction with the University of Pennsylvania Smell Identification Test (UPSIT), Int Arch Otorhinolaryngol, vol. 22, no. 3, pp. 280–283, Jul. https://doi.org/10.1055/S-0037-1608679
Murali S, Vijayaraj GP, Saravanam PK, Thattarakkal VR (2022) Partial Middle Turbinectomy Versus Medialization Suturing of Middle Turbinate in the Management of Sinonasal Polyposis: A Comparative Study, Indian J Otolaryngol Head Neck Surg, vol. 74, no. Suppl 2, pp. 1472–1478, Oct. https://doi.org/10.1007/S12070-021-02609-6
Tomoum MO, ElSheikh MN, ElBasty H, Hagras MAE, El-Naggar A (May 2022) Anterior part middle turbinoplasty in endoscopic sinus surgery: a randomized controlled study. Eur Arch Otorhinolaryngol 279(5):2465–2471. https://doi.org/10.1007/S00405-021-07053-4
Lasheen HMN, Falah HYESA, Mahmoud GAF, Heiba MH, Abou-Zied MAMH (2023) Effect of Partial Middle Turbinectomy on the Recurrence of Allergic Fungal Sinusitis: A Comparative Study, Egyptian Journal of Ear, Nose, Throat and Allied Sciences, vol. 24, no. 24, pp. 1–8, Jan. https://doi.org/10.21608/EJENTAS.2023.162584.1558
Krishna Santosh B, Reddy NSS (Jul. 2015) A randomized control trial of partial middle turbinate resection in functional endoscopic sinus surgery. Indian J Public Health Res Dev 6(3):238–242. https://doi.org/10.5958/0976-5506.2015.00173.4
Havas TE, Lowinger DSG (2000) Comparison of functional endonasal sinus surgery with and without partial middle turbinate resection. Ann Otol Rhinol Laryngol 109(7):634–640. https://doi.org/10.1177/000348940010900704
Gulati SP, Wadhera R, Kumar A, Gupta A, Garg A, Ghai A (2010) Comparative evaluation of middle meatus antrostomy with or without partial middle turbinectomy, Indian J Otolaryngol Head Neck Surg, vol. 62, no. 4, pp. 400–402, Oct. https://doi.org/10.1007/S12070-010-0102-9
Acknowledgements
I would like to express my sincere gratitude to all individuals and institutions that contributed to the completion of this systematic review. First and foremost, I extend my heartfelt thanks to my collaborator, Federica Vultaggio who provided valuable insights and feedback during the course of this study. I’m deeply indebted to Vittorio Saginario and Giovanni Felisati whose constructive comments and suggestions helped to improve the quality of this manuscript. An heartfelt thanks to Alberto Maria Saibene whose expertise and dedication greatly enriched this work. I would like to acknowledge the authors and researchers of the primary studies included in this systematic review for their significant contributions to the field. Finally, I express my gratitude to our families, friends, and colleagues for their unwavering support and encouragement throughout this path.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Gabriele Alessandro Novarria, and Federica Vultaggio. The first draft of the manuscript was written by Gabriele Alessandro Novarria and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare they have no conflict of interest
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Novarria, G.A., Vultaggio, F., Saginario, V. et al. Efficacy and safety of middle turbinate surgery: a systematic review. Eur Arch Otorhinolaryngol (2024). https://doi.org/10.1007/s00405-024-08825-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00405-024-08825-4