Abstract
Objectives
The inferior and middle turbinates have crucial roles in nasal function, but their enlargement can cause obstructive effects, which can lead to breathing difficulties, sleep and smell disorders, and headaches. Partial turbinectomy is a common surgical technique used to address this issue during septorhinoplasty, but it carries risks such as empty nose syndrome. A clinical trial was designed to evaluate the functional outcomes of middle and inferior partial turbinectomy with a holistic approach.
Methods
Patients with NOSE questionnaire scores of 30 or higher, and grade 4 inferior turbinates and/or advanced middle concha bullosa were included. Patients completed questionnaires related to breathing, empty nose syndrome, headache, and olfaction preoperatively and at one-month, three-month, six-month, and first-year periods postoperatively. The partial excisions of the inferior and middle turbinates were carried out with serrated scissors while trying to preserve adequate turbinate size to maintain function.
Results
This study found that NOSE scores, headache frequency, and severity improved postoperatively. The olfactory-related quality of life of the patients with impairments in this area significantly improved found to be improved at all postoperative evaluations. None of the patients experienced prolonged bleeding requiring surgical intervention. No cases of anosmia and empty nose syndrome were reported.
Conclusion
Partial turbinectomy of middle and inferior turbinates during septorhinoplasty can alleviate symptoms of turbinate hypertrophy, such as breathing issues, olfactory disorders, and headaches. It is an easy, reliable, and efficient surgical maneuver. Proper technique can minimize the risk of empty nose syndrome and other complications of turbinectomy surgery.
Level of Evidence III
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Septorhinoplasty is a commonly performed surgery to address both aesthetic and functional issues in the nose. While the aesthetic outcomes of the surgery may receive more attention, the functional results are equally important for patient satisfaction [1]. Functional problems include but are not limited to difficulty breathing, sleep disorders, sinus infections, headaches, and a reduced sense of smell [2, 3]. While septal deviation is generally accepted as the main cause of these symptoms, enlarged turbinates can also contribute to them [4].
The inferior and middle turbinates play important roles in warming, filtering, and moistening air and olfaction [5]. However, excessive enlargement of these structures can lead to obstructions, hindering airflow and causing difficulty in breathing, loss of sense of smell, and sleep disturbances [6]. Various medical and interventional treatment modalities are used to alleviate these symptoms [7, 8]. Medical therapy is used for turbinate hypertrophy, but when symptoms are non-responsive, turbinate reduction surgery can be considered [9]. The interventional treatment modalities include but are not limited to turbinate outfracture, bipolar and monopolar cauterization, submucosal reduction, and partial and total turbinectomy [10]. Partial turbinectomy surgery can alleviate symptoms, but it also carries potential complications, such as bleeding, crusting, loss of sense of smell, paradoxical breathing problems, and the most dreaded empty nose syndrome (ENS) [11, 12]. Therefore, proper preoperative evaluation, surgical technique, and postoperative care are crucial for optimal results [13].
Despite numerous studies on the benefits and complications of inferior and middle turbinate interventions separately [10], there is a lack of prospective clinical studies that comprehensively investigate the long-term functional outcomes of middle and inferior turbinectomy together. To address this gap, a prospective study has been designed to investigate the effects of inferior and middle turbinate surgery on breathing, headaches, sense of smell, and ENS.
Materials and Methods
This was a single-center, pragmatic, interventional, prospective study investigating the effect of partial middle and inferior turbinectomies on the patients’ breathing, olfaction, headache, and ENS. This study was approved by a local ethics committee. The study was conducted in our clinic between February 2021 and February 2023. All patients scheduled for septorhinoplasty were enrolled in the study. Patients with a history of septorhinoplasty, turbinate reduction, or turbinectomy, under 18 years of age were excluded from the study.
Patient Selection
The study recruited individuals who applied for septorhinoplasty and evaluated their respiratory problems using The Nasal Obstruction Symptom Evaluation (NOSE) Scale, a widely recognized questionnaire designed to assess nasal obstruction [14]. Patients with a score above 30 were further examined and considered for turbinectomy. Nasal endoscopy and anterior rhinoscopy were conducted before and after applying topical decongestants to assess the size of the inferior and middle turbinates. In this study, the grading system developed by Camacho et al. [15] was utilized to assess the degree of inferior turbinate hypertrophy. Patients with grade 4 (76–100% of total airway space) inferior turbinates were recommended for inferior turbinectomy, while those with concha bullosa or severely hypertrophic middle turbinates were recommended for middle turbinectomy. A middle turbinate was considered severely hypertrophic if the distance between the septum and middle turbinates was less than 2 mm.
Patients were excluded from the study if they had a history of septorhinoplasty or allergic rhinitis, underwent any intervention on the turbinates, were under 18 or over 65 years of age, or had a NOSE score of less than 30. The study group consisted of patients who had undergone partial inferior or middle turbinectomy, or a combination of both, during septorhinoplasty (Fig. 1).
Evaluation of Functional Results
The NOSE scale is useful in identifying changes in breathing before and after surgery and determining the extent of nasal obstruction in the patient. Scores range from 0 to 100, with 0 representing no nasal obstruction and 100 indicating the most severe nasal obstruction.
The ASOF questionnaire, which stands for "The assessment of self-reported olfactory functioning and olfaction-related quality of life," is a validated tool for assessing subjective olfactory functions in normosmic subjects and patients with olfactory dysfunction [16]. It consists of three components: olfactory-related quality of life (ASOF-ORQ), subjective olfactory capability (ASOF-SOC), and self-reported smell-related problems scale (ASOF-SRP). In this study, the third component, ASOF-SRP, was not employed to simplify the study and, due to patient reluctance to respond to ASOF-SRP-related questions. A validated Turkish version of the ASOF questionnaire was used for this study [17]. ASOF-SOC ranges from 0 being the inability to smell and 10 being the best possible ability to smell. Patients were accepted as having abnormal olfactory capability when the ASOF-SOC score was equal to or less than 3. ASOF ORQ has 6 items and scores range from, 1 very much impaired to 5, not at all impaired. Patients were asked if they have been impaired in those six items in the last four weeks because of their sense of smell. The mean scores of the items give the ASOF-ORQ. Patients were accepted as having smell-related problems that affect their life quality when ASOF-ORQ was equal to or less than 3,7.
For the assessment of headaches, patients were asked to report the number of headaches they experienced in the previous month, with a range from 0 to 10 attacks. They were also asked to rate the severity of their pain using a visual analog scale (VAS) that ranges from 0 to 10.
To evaluate the development of ENS, patients completed the Empty Nose Syndrome 6-Item Questionnaire(ENS6-Q), which did not have a Turkish version [18]. The questionnaire was translated into Turkish by a fluent English speaker, then back-translated into English by another translator and compared with the original one to ensure accuracy. Patients with post-operative scores above 12 were considered to have ENS.
Patient demographic data, excised turbinates, and postoperative bleeding were also recorded.
Operative Technique
The same surgeon (A.K) used the same surgical technique for partial turbinectomies, including endoscopic examination of middle and inferior turbinates during septorhinoplasty. Partial turbinectomy procedures were carried out on patients with grade 4 hypertrophic turbinates or severely hypertrophic concha bullosa, and submucosal electrocauterization was used for concomitant grade 2 (26–50%) and grade3 (51–75%) inferior turbinates (Fig. 2). All turbinectomy procedures were performed endoscopically, and intraoperative correction of cartilaginous and/or osseous septal deviations was performed on all patients.
For inferior turbinate excision, first, the area was infiltrated with a 1% lidocaine and 1/80000 adrenaline solution. A Freer elevator was used to lateralize and then medialize the inferior turbinate before excision. A Gorney-Freeman serrated scissors were used to partially remove the mucosa, soft tissue, and bone along the entire length of the inferior 1/3 of the inferior turbinate. Following the partial excision, bipolar cautery was used to cauterize the rough surface to prevent postoperative bleeding. The amount of excision was based on the size, shape, and position of the turbinate, with care taken to leave approximately 60–65% of the inferior turbinate to prevent complications (Fig. 3).
Patients with obstructive middle turbinates had the inferior 2/3 of the middle turbinate or the entire concha bullosa removed along its entire length using Gorney-Freeman serrated scissors. After the area was infiltrated a 1% lidocaine and 1/80000 adrenaline solution excision was carried out. The stalk of the concha bullosa, which corresponds to the upper 1/3 of the middle turbinate, was left intact to prevent anosmia. Bipolar cautery was used to cauterize the rough surface following the partial excision to prevent postoperative bleeding (Fig. 4).
After a 1-day inpatient follow-up, all patients were discharged with anti-inflammatory drugs and antibiotics. Oral H1-antihistamine treatment was given to all patients for a period of one month. On the fifth day, patients were called back for the removal of their Doyle splint and to receive additional recommendations. Routine follow-up appointments were scheduled for the first, third, sixth months, and 1-year periods. During these periods patients were checked for possible complications and filled out the questionnaires.
Statistical analysis was performed using the R program [19]. Kruskall Wallis test was used to analyze the variance, and Mann Whitney-U test was used to compare medians of the data. Descriptive statistics are used to calculate and summarize the data logically.
Results
Over the course of 2 years, we performed rhinoplasty on 212 patients. 30 of these patients were included in the study, as they underwent partial inferior and/or middle turbinectomy. 3 patients were lost to follow-up and excluded from the study. 27 patients completed the study and their data were analyzed in the study (Figs. 5 and 6). Of the 27 patients included, 8 had unilateral inferior turbinate excisions, 10 had unilateral middle turbinate excisions, and 9 had combined middle and inferior turbinate excisions (Fig. 7). The study group had a total of 25 female patients and 2 male patients, with an average age of 26.6 ± 6.
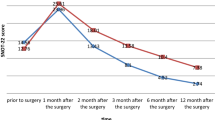
The mean NOSE scores were 61.5 ± 20.4 preoperatively, 34.3 ± 20.2 at 1 month, 21.2 ± 12.7 at 3 months, 19.4 ± 14.6 at 6 months, and 18 ± 20.1 at 1 year postoperatively (Fig. 8). The NOSE scores showed a continuous decline with time. Kruskal Wallis Test showed there was a difference between preoperative and postoperative periods and the Mann-Whitney U test showed this difference was statistically significant (p < 0.05).
Before the operation, the mean number of headaches was 4.37 ± 3.04. At 1 month, it was 3.63 ± 2.5, at 3 months it was 2.74 ± 1.93, at 6 months it was 2.7 ± 1.71, and at 1 year postoperative, it was 2.15 ± 1.38. A statistically significant difference was found between pre-operative and first-year-postoperative periods (p < 0.05).
Headache VAS scores were, 5.59 ± 2.44 preoperatively, 4.22 ± 2.58 at 1 month, 3.33 ± 2.13 at 3 months, 3.56 ± 2.04 at 6 months, and 2.56 ± 1.89 at 1 year postoperatively. A statistically significant difference was observed between all periods, particularly at the 3rd, 6th month, and 1 year postoperative (p < 0,05). The severity of headaches was noted to decrease gradually from the pre-operative period until the first year after the operation (p < 0.05).
The mean ASOF-ORQ scores of all patients did not show any significant difference across all periods. The analysis of 8 patients with smell-related problems affecting their quality of life preoperatively (as indicated by ASOF-ORQ scores below the cutoff point) showed statistically significant improvement between all postoperative periods compared to preoperative results (p < 0.05). At the postoperative first month, the number decreased to 5 patients, and at the postoperative third, sixth months, and 1 year, only one patient reported a smell-related quality of life problem according to their ASOF-ORQ scores.
The mean ASOF-SOC score was worsened postoperative first month compared to before the operation. It gradually got better and there was no difference compared to the preoperative period by the end of first-year post-operatively. Two out of the three patients with abnormal olfactory capabilities showed normal capabilities at the post-operative first year according to their ASOF-SOC scores.
The ENS6-Q scores were measured at different time points after the surgery, and the results were as follows: 6.78 ± 4.92 at 1 month postoperatively, 3.48 ± 2.93 at 3 months postoperatively, 3.04 ± 3.11 at 6 months postoperatively, and 2.22 ± 4.13 at the first year postoperatively. No patients had an ENS6-Q score higher than 12.
No serious bleeding was observed in any of the patients. In the anterior rhinoscopy examination performed at the first year postoperatively, adhesions and abnormal crusting were not observed in any of the patients.
Discussion
While medical treatments are available, advanced turbinate hypertrophy cases may require surgery. The excision of the inferior and middle turbinates is a topic of debate since they are important for nasal functions but they can cause serious symptoms if enlarged [20, 21]. Preserving their structure through partial turbinectomies is vital to avoid severe complications like atrophic rhinitis, anosmia, and ENS [22]. However, even with a conservative approach, complications may occur, so selecting the right patients is essential to balance the surgery's risks and benefits [23].
Several alternative methods for treating turbinate hypertrophy include turbinate outfracture, radiofrequency ablation, submucosal reduction, and electrocauterization [24]. Despite being one of the oldest methods among these options, electrocauterization of turbinates is an effective and safe procedure. It can preserve nasal epithelium and provide a minimal risk of crusting [25]. In a prospective study comparing radiofrequency ablation with electrocauterization, it was found that electrocauterization demonstrated superior results [26]. Even though less invasive options such as the turbinate fracture and the electrocauterization of the mucosa could have improved our patients’ problems, we believe that for selective cases like in our article (grade 4 inferior turbinates and extensive concha bullosa), the partial turbinectomy can be superior to other options. But this hypothesis needs further clarification beyond our experience.
In this study, the preoperative mean NOSE score of patients improved significantly, decreasing from 61.5 to 18 at the postoperative first year. This finding showed partial turbinectomy can resolve obstruction problems in nasal airways which correlate with the literature [27]. However, it should be noted septoplasty, submucosal electrocauterization, and functional rhinoplasty might also impact NOSE scores.
Even though the analysis of ASOF-ORQ scores for all patients did not reveal any difference, those with scores below the cutoff points demonstrated a statistically significant improvement. This shows partial turbinectomy can be effective against olfactory disorders in selected patients. This finding also can be considered as a new possible indication for partial turbinectomy but further clinical studies with larger patient groups are needed to support this.
The origins of rhinogenic headaches are not yet fully comprehended, but plausible factors include agger nasi cell, hypertrophy of the inferior turbinate, concha bullosa of the middle turbinate, and mucosal contact points [28, 29]. In this particular study, 19 patients had severe concha bullosa and 17 had severe inferior turbinate hypertrophy. The number of headaches decreased significantly at the postoperative first year compared to the preoperative period. Also, VAS scores gradually improved over time, the lowest score being the postoperative first year. This study indicates that turbinectomy surgery can relieve headaches in patients with impaired NOSE scores. This finding may indicate that addressing obstructive elements causing rhinogenic headaches can improve these patients' symptoms. Obstructive elements such as enlarged turbinates and deviated septum should be managed intraoperatively according to patients’ preoperative symptoms.
Middle concha bullosa, a condition that causes nasal obstruction and difficulty breathing, may be improved through excision. Research has shown that patients who undergo rhinoplasty and have concha bullosa may experience improved breathing post-operation [30]. Patients with concha bullosa, as determined by nasal endoscopy or anterior rhinoscopy, may benefit from excision in terms of improved smell and breath [31].
ENS is a feared and controversial complication of excessive turbinectomy surgery, first coined by Kern and Moore [32]. This condition can occur when the remaining turbinates are unable to perform their functions, such as humidifying the air, regulating airflow, and protecting the mucosa from dryness. Surgeons must be cautious to avoid this complication, as treatment is not always successful and can greatly reduce a patient's quality of life [33]. No ENS cases were encountered among our patients, perhaps it was because we took care not to damage the surrounding mucosa and performed partial excisions.
Our study had several limitations, including a small sample size, no control groups, and a lack of randomization. The number of patients was limited by the time frame of the study and strict inclusion criteria. The inclusion criteria was very selective, only including patients with advanced middle concha bullosa or severe inferior turbinate hypertrophy. Our results might also have been affected by the functional rhinoplasty and septoplasty procedures. We also did compare the inferior and middle turbinate surgeries separately due to the heterogeneity of our data as we performed isolated or combined partial turbinectomies in our patients.
Conclusion
Inferior and middle partial turbinectomy procedures, often done in conjunction with septorhinoplasty, are effective options for treating inferior and middle turbinate hypertrophy. This study showed these procedures can improve breathing, enhance the sense of smell and reduce headaches with correct patient selection. Although there is a risk of the development of ENS, this risk can be minimized with appropriate techniques. Further studies with larger patient groups are needed to clarify and fully demonstrate the safety and effectiveness of partial inferior and middle turbinectomy.
References
Balikci HH, Gurdal MM (2014) Satisfaction outcomes in open functional septorhinoplasty: prospective analysis. J Craniofac Surg 25(2):377–379. https://doi.org/10.1097/scs.0000000000000638
Georgalas C (2011) The role of the nose in snoring and obstructive sleep apnoea: an update. Eur Arch Otorhinolaryngol 268(9):1365–1373. https://doi.org/10.1007/s00405-010-1469-7
Shapiro GG (1988) The role of nasal airway obstruction in sinus disease and facial development. J Allergy Clin Immunol 82(5 Pt 2):935–940. https://doi.org/10.1016/0091-6749(88)90036-x
Nurse LA, Duncavage JA (2009) Surgery of the inferior and middle turbinates. Otolaryngol Clin North Am 42(2):295–309. https://doi.org/10.1016/j.otc.2009.01.009
Smith DH, Brook CD, Virani S, Platt MP (2018) The inferior turbinate: an autonomic organ. Am J Otolaryngol 39(6):771–775. https://doi.org/10.1016/j.amjoto.2018.08.009
Lenders H, Schaefer J, Pirsig W (1991) Turbinate hypertrophy in habitual snorers and patients with obstructive sleep apnea: findings of acoustic rhinometry. Laryngoscope 101(6 Pt 1):614–618. https://doi.org/10.1288/00005537-199106000-00007
Garcia JPT, Moura BH, Rodrigues VH, Vivan MA et al (2022) Inferior turbinate reduction during rhinoplasty: is there any effect on rhinitis symptoms? Int Arch Otorhinolaryngol 26(1):e111–e118. https://doi.org/10.1055/s-0041-1726046
Gunhan K, Unlu H, Yuceturk AV, Songu M (2011) Intranasal steroids or radiofrequency turbinoplasty in persistent allergic rhinitis: effects on quality of life and objective parameters. Eur Arch Otorhinolaryngol 268(6):845–850. https://doi.org/10.1007/s00405-010-1462-1
Mohamed NN, Khamis W, Abdelbary EH, Alkabeer TY (2022) Diode laser-assisted inferior turbinoplasty in resistant cases of allergic rhinitis: a clinical and histopathological study. Lasers Med Sci 37(3):2053–2061. https://doi.org/10.1007/s10103-021-03477-w
Zhang K, Pipaliya RM, Miglani A, Nguyen SA et al (2023) Systematic review of surgical interventions for inferior turbinate hypertrophy. Am J Rhinol Allergy 37(1):110–122. https://doi.org/10.1177/19458924221134555
Gordiienko IM, Gubar OS, Sulik R, Kunakh T et al (2021) Empty nose syndrome pathogenesis and cell-based biotechnology products as a new option for treatment. World J Stem Cells 13(9):1293–1306. https://doi.org/10.4252/wjsc.v13.i9.1293
de Moura BH, Migliavacca RO, Lima RK, Dolci JEL et al (2018) Partial inferior turbinectomy in rhinoseptoplasty has no effect in quality-of-life outcomes: a randomized clinical trial. Laryngoscope 128(1):57–63. https://doi.org/10.1002/lary.26831
Levy E, Ronen O, Sela E, Layos E et al (2022) Inferior turbinate reduction: comparing post-operative bleeding between different surgical techniques. J Laryngol Otol 136(5):427–432. https://doi.org/10.1017/s0022215121003297
Stewart MG, Witsell DL, Smith TL, Weaver EM et al (2004) Development and validation of the nasal obstruction symptom evaluation (NOSE) scale. Otolaryngol Head Neck Surg 130(2):157–163. https://doi.org/10.1016/j.otohns.2003.09.016
Camacho M, Zaghi S, Certal V, Abdullatif J et al (2015) Inferior turbinate classification system, grades 1 to 4: development and validation study. Laryngoscope 125(2):296–302. https://doi.org/10.1002/lary.24923
Pusswald G, Auff E, Lehrner J (2012) Development of a brief self-report inventory to measure olfactory dysfunction and quality of life in patients with problems with the sense of smell. Chemosens Percept. https://doi.org/10.1007/s12078-012-9127-7
Saatci Ö, Arici Duz O, Altundag A (2020) Reliability and validity of the Turkish version of the questionnaire for the assessment of self-reported olfactory functioning and olfaction-related quality of life. J Acad Res Med 10:277–282. https://doi.org/10.4274/jarem.galenos.2020.3579
Velasquez N, Thamboo A, Habib AR, Huang Z et al (2017) The empty nose syndrome 6-item questionnaire (ENS6Q): a validated 6-item questionnaire as a diagnostic aid for empty nose syndrome patients. Int Forum Allergy Rhinol 7(1):64–71. https://doi.org/10.1002/alr.21842
Chan BKC (2018) Data analysis using R programming. Adv Exp Med Biol 1082:47–122. https://doi.org/10.1007/978-3-319-93791-5_2
Chen XB, Lee HP, Chong VF, De Wang Y (2010) Impact of inferior turbinate hypertrophy on the aerodynamic pattern and physiological functions of the turbulent airflow - a CFD simulation model. Rhinology 48(2):163–168. https://doi.org/10.4193/Rhin09.093
Kennedy DW (1998) Middle turbinate resection: evaluating the issues–should we resect normal middle turbinates? Arch. Otolaryngol Head Neck Surg 124(1):107. https://doi.org/10.1001/archotol.124.1.107
Hong HR, Jang YJ (2016) Correlation between remnant inferior turbinate volume and symptom severity of empty nose syndrome. Laryngoscope 126(6):1290–1295. https://doi.org/10.1002/lary.25830
Karamatzanis I, Kosmidou P, Ntarladima V, Catalli B et al (2022) Inferior Turbinate hypertrophy: a comparison of surgical techniques. Cureus 14(12):e32579. https://doi.org/10.7759/cureus.32579
Sinno S, Mehta K, Lee ZH, Kidwai S et al (2016) Inferior turbinate hypertrophy in rhinoplasty: systematic review of surgical techniques. Plast Reconstr Surg 138(3):419e–429e. https://doi.org/10.1097/prs.0000000000002433
Cavaliere M, Mottola G, Iemma M (2007) Monopolar and bipolar radiofrequency thermal ablation of inferior turbinates: 20-month follow-up. Otolaryngol Head Neck Surg 137(2):256–263. https://doi.org/10.1016/j.otohns.2007.01.001
Kilavuz AE, Songu M, Ozkul Y, Ozturkcan S et al (2014) Radiofrequency versus electrocautery for inferior turbinate hypertrophy. J Craniofac Surg 25(6):1998–2001. https://doi.org/10.1097/scs.0000000000001032
Law RH, Bazzi TD, Van Harn M, Craig JR et al (2021) Predictors of long-term nasal obstruction symptom evaluation score stability following septoplasty with inferior turbinate reduction. Laryngoscope 131(7):E2105-e2110. https://doi.org/10.1002/lary.29229
Anselmo-Lima WT, de Oliveira JA, Speciali JG, Bordini C et al (1997) Middle turbinate headache syndrome. Headache 37(2):102–106. https://doi.org/10.1046/j.1526-4610.1997.3702102.x
Tosun F, Gerek M, Ozkaptan Y (2000) Nasal surgery for contact point headaches. Headache 40(3):237–240. https://doi.org/10.1046/j.1526-4610.2000.00034.x
Inan S, Gultekin G, Yilmaz I, Buyuklu AF (2023) Effect of functional Septorhinoplasty with concha bullosa resection on Sinonasal symptoms. Laryngoscope 133(6):1375–1381. https://doi.org/10.1002/lary.30428
Akkoca Ö, Tüzüner A, Ünlü CE, Şimşek G et al (2020) Comparison of the effects of 2 surgical techniques used in the treatment of concha bullosa on olfactory functions. Ear Nose Throat J 99(7):437–441. https://doi.org/10.1177/0145561319881061
Moore EJ, Kern EB (2001) Atrophic rhinitis: a review of 242 cases. Am J Rhinol 15(6):355–361
Chhabra N, Houser SM (2009) The diagnosis and management of empty nose syndrome. Otolaryngol Clin North Am 42(2):311–330. https://doi.org/10.1016/j.otc.2009.02.001
Funding
The authors received no financial support for this article's research, authorship, and publication.
Author information
Authors and Affiliations
Contributions
MÇ: Substantial contributions to Conception and design, analysis and interpretation of the data, drafting the article or revising it critically for important intellectual content; and (3) final approval of the version to be published. SKA: Substantial contributions to Conception and design, analysis and interpretation of the data, drafting the article critically for important intellectual content; and (3) final approval of the version to be published. UK: Substantial contributions to design, analysis, and interpretation of the data, drafting the article for important intellectual content; and (3) final approval of the version to be published. AK: Substantial contributions to Conception and design, analysis and interpretation of the data, drafting the article or revising it critically for important intellectual content; and (3) final approval of the version to be published
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no potential conflicts of interest concerning this article's research, authorship, and publication.
Ethical Approval
This material is the author’s original work, which has not been previously published elsewhere. This study was performed by research ethical guidelines. There are no human subjects in this article and informed consent is not applicable. All authors have contributed to the paper and have permitted their names to be included as co-authors. This manuscript is not submitted to or is currently under review at any other journal.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Çelik, M., Altunal, S.K., Kocer, U. et al. Comprehensive Assessment of the Functional Outcomes of Partial Turbinectomy: A Prospective Clinical Trial. Aesth Plast Surg 48, 1547–1556 (2024). https://doi.org/10.1007/s00266-023-03503-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-023-03503-y