Abstract
Purpose
Sinonasal nuclear protein in testis carcinoma (SNUTC) is a rare, aggressive malignancy caused by genetic rearrangements in the NUTM1 gene. The prognosis of SNUTC ranks among the most unfavorable within the naso-sinusal district, with an overall survival of 9.7 months. This systematic review aimed to determine the best therapeutic strategy for SNUTC.
Methods
We reviewed eligible articles for patient demographics, TNM and stage at presentation, best response after primary treatment, disease-free survival and overall survival (OS) times, other following therapy lines, and final outcomes.
Results
Among 472 unique citations, 17 studies were considered eligible, with reported treatment data for 25 patients. Most studies (n = 12) were case reports. The most frequently administered treatment regimen was surgery as primary treatment and combined radiochemotherapy as second-line or adjuvant treatment. Four patients were alive at follow-up.
Conclusion
Basing on the existing literature, a standardized line in the treatment of SNUTC is not yet well delineated. A self-personalized strategy of therapy should be drawn on each patient affected by SNUTC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nuclear protein in testis (NUT) carcinomas are rare, highly aggressive malignancies, caused by genetic rearrangements in the NUTM1 gene. They generally arise in midline structures of head and neck or thorax, but every organ can be virtually affected. The most frequent mutation involves the translocation of the NUTM1 gene to form a fusion protein with the BRD4 gene on chromosome 19p13.1 [1]. Other translocation variants involve the fusion of the NUTM1 gene on 15q14 with another gene such as BRD3 on 9q34.2 [2]. From a histological perspective, these tumors generally show non-specific features, ranging from poorly differentiated carcinomas to carcinomas with prominent squamous differentiation. For this reason, their morphological diagnosis is often difficult and must be integrated with molecular methods to demonstrate a rearrangement of the NUTM1 gene (i.e., fluorescent in situ hybridization—FISH) [1, 3].
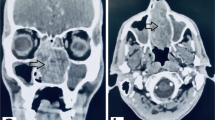
Primary SNUTC (sinonasal NUT carcinomas) of the nasal cavity and paranasal sinuses are extremely rare, causing diagnostic and therapeutic difficulties. Presenting symptoms are usually non-specific and represented by nasal obstruction, rhinorrhea, epistaxis, acute sinusitis with or without diplopia, exophthalmos, and proptosis [4, 5]. Therefore, SNUTCs are often confused with infection processes or with benign nasal conditions, leading to delayed diagnosis. Given the rarity of the SNUTC, its frequent diagnostic delay due to the lack of characteristic clinical and histopathological features and its poor diagnosis (with a median overall survival of 9.7 months [6]), recommended treatments have not been established yet.
This review aims to summarize and analyze the currently available therapeutic strategies for nonmetastatic SNUTC in terms of disease-specific survival and disease-free survival.
Materials and methods
Search strategy
After registering with the PROSPERO database (ID CRD42023390827), we conducted a systematic review between January 11, 2023, and May 3, 2023, according to PRISMA reporting guidelines [7]. Systematic electronic searches were carried out in English, Italian, German, French, and Spanish, for articles reporting original data on therapeutic strategies for SNUTC.
On January 11, 2023, a primary search was performed on the MEDLINE, Embase, Web of Science, Cochrane Library, Scopus, and ClinicalTrials.gov databases combining the terms “(NUT OR NUT carcinoma OR NUT midline carcinoma) AND (nose OR sinus OR maxillary OR frontal OR sphenoid OR ethmoid)”. Complete search strategies and the number of items retrieved from each database are provided in Table 1. The references of selected publications were then examined to identify further reports that were not found by database searching, and the same selection criteria were applied.
We included all article types excluding meta-analyses and systematic or narrative reviews, which were nevertheless hand-checked for additional potentially relevant papers. Exclusion criteria were as follows: non-human studies, papers carried out in other languages than English, Italian, German, French, or Spanish, patients presenting NUT carcinomas of head and neck regions other than the sinonasal tract, and studies that reported follow-up periods of less than 12 months (unless the patient died within the year). No minimum study population was required. No publication date restriction was applied. Given the rarity of this neoplasm, we included only articles which stated that the diagnosis had been confirmed by molecular identification of the NUT gene.
Abstract and full texts were reviewed in duplicate by different authors. At the abstract review stage, we included all studies that were deemed eligible by at least one rater. At the full-text stage, disagreements were resolved by achieving consensus among raters.
PICOS criteria
The Population, Intervention, Comparison, Outcomes, and Study (PICOS) framework for the review was defined as follows:
-
P: all patients with a primary sinonasal NUT carcinoma (SNUTC)
-
I: any kind of treatment for SNUTC, either surgical, radiotherapeutic, chemotherapeutic, or combined
-
C: comparisons between different kinds of treatments and with no treatment
-
O: disease-specific survival and disease-free survival
-
S: original studies of any kind and clinical setting (except meta-analyses)
Data extraction and quality assessment
For each article included, we recorded: study type, the overall number of patients included, female to male ratio, patients’ age at diagnosis, TNM and stage at presentation, prior therapy (any therapy carried out before the final diagnosis of SNUTC), primary treatment (i.e., surgery, chemotherapy, radiotherapy, combined therapy), adjuvant therapy (when performed), best treatment response (i.e., partial response, complete response, disease progression), disease-free survival (DFS) time in months, overall survival (OS) time in months, type of further therapy lines (second, third, etc.…) and respective progression-free survival, and final outcome (i.e., death from disease—DFD, alive with disease—AWD, alive without disease—AWOD). We excluded papers that reported follow-up periods of less than 12 months (unless the patient died within a year). Two authors extracted data and rated studies in duplicate, and disagreements were resolved by consensus.
Studies were assessed for both quality and methodological bias according to the National Heart, Lung, and Blood Institute Study Quality Assessment Tools (NHI-SQUAT) [8] for case series and cohort studies and the Joanna Briggs Institute Critical Appraisal tools (JBI-CAT) for case reports [9]. With the same methodology adopted for systematic reviews with middle-to-low evidence levels in comparable recent reviews [10], items were rated as “good” if they fulfilled at least 80% of the items reported in the JBI-CAT or NHI-SQUAT, “fair” if they fulfilled between 50 and 80% of the items, and “poor” if they fulfilled less than 50% of the items, respectively.
The level of evidence for clinical studies was scored according to the Oxford Centre for Evidence-based Medicine (OCEBM) level of evidence guide [11].
Due to the considerable heterogeneity of study populations, study methods, and the predominantly qualitative nature of collected data, no initial meta-analysis was planned or performed a posteriori.
Results
Among the 472 unique research items initially identified, 65 published reports were selected for full-text evaluation. No further report was identified from full-text evaluation after reference checking. Overall, 17 studies published between 2011 and 2022 were retained for analysis (Fig. 1) [3, 4, 12,13,14,15,16,17,18,19,20,21,22,23,24,25,26].
5 articles were case series, and the remaining 12 articles were case reports. All articles had a level of evidence IV according to the OCEBM scale. Articles were rated as good (n = 13), fair (n = 3), or poor (n = 1) according to NHI-SQAT or JBI-CAT tools. No significant biases toward the objectives of our systematic review were identified, while most articles lacked ample information allowing for patient comparison. Table 2 reports the study type, evidence, and quality rating for all studies included.
The 17 included studies had 25 participants whose ages at diagnosis ranged from 14 to 65 years (median 46, interquartile range 12). Patients were more frequently male (15 male vs. 9 female), while one paper did not report gender information. TNM and stage at presentation were reported only in a few studies. In the remaining cases, TNM and stage were derived from the description of the extent of the malignancy or from the provided radiological images. In particular, stages IV and III were the most common (18 out of 25 patients), both stage II and stage I were found only in 1 case, and for 5 patients the initial stage could not be assessed. Table 3 shows the demographic and clinical information for the treated patients.
Before the final diagnosis of SNUTC, in 9 out of 25 patients a prior therapy consisting of endoscopic resection (n = 7) and chemotherapy (CT, n = 2) with vincristine/cyclophosphamide/doxorubicin or docetaxel/cisplatin/fluorouracil was carried out. Most patients (n = 11) underwent surgery as primary treatment, followed by combined chemoradiotherapy (CRT) (n = 6), exclusive radiotherapy (RT, n = 3), a combination of surgery and CT (n = 3), exclusive CT (n = 1), exclusive immunotherapy (IT) (n = 1), and combined IT + RT. Adjuvant therapy was administered in ten patients and consisted of exclusive CT, combined CT and RT, and exclusive RT (also extended to the thoracic and lumbar spine for palliative intent). After the failure of initial treatments, five patients in total received other than second-line therapies, which contemplated CT for four patients and CRT for one subject as third-line therapy, CT for two patients and IT for one patient as fourth-line therapy, and CT for one patient as fifth and sixth-line therapy. DFS and OS were extremely variable, ranging from 1 to 96 months and from 2 to 108 months, respectively. Table 4 shows the data on primary and following treatment approaches, the DFS and OS of each patient, and the final outcome at the end of follow-up time.
Concerning the treatment response, most patients (n = 9) showed complete response to primary therapy but only three of them were AWOD at the end of their follow-up period [19, 20, 22]. On the other hand, the primary treatment of nine patients resulted in a disease progression and three patients showed only partial response to the therapy. As shown in Table 4, 10 out of 25 patients underwent a second-line treatment which consisted of exclusive CT (n = 1), exclusive RT (n = 3), combined CT and RT (n = 4), and surgical treatment (n = 2). Of all patients who received second-line treatment, only one resulted in complete recovery. In particular, his first-line treatment consisted of CT (vincristine, doxorubicin, and cyclophosphamide, alternating with ifosfamide and etoposide) combined with RT, while as the second-line treatment he received proton beam radiotherapy (BPR) [22].
As for the final outcome at the end of the follow-up period, the majority (n = 19) were DFD, three patients were AWOD, and one was AWD. There is no outcome information for two patients.
Discussion
To the best of our knowledge, this represents the first systematic review to analyze the currently available therapeutic approaches to treat SNUTC. Analyzing the existing literature, we found out only few eligible studies with a low level of evidence (case series and case reports); this demonstrates the huge variability upon this theme and the absence of a standardized therapy strategy for treatment of SNUTC. The lack of current guidelines on this topic is attributable to the rarity of the neoplasm and to its intrinsic aggressivity, to the unusual patient presentation, and to the rapid onset of symptoms that often occur when the disease is already in an advanced stage. All these factors contribute to SNUTC being a malignancy burdened with a diagnostic delay and an unfavorable prognosis. For all the reasons listed above, the current literature lacks randomized controlled trials. We identified only five case series and a few case reports (12 out of 17 selected works), which represent therefore only a starting point for building a standardized approach to this disease.
In total, 18 out of 25 patients in our review showed an advanced stage of SNUTC at the time of first diagnosis, which can be explained by at least 2 reasons. First of all, this late diagnosis could be a direct result of the poor differentiation characterizing SNUTCs, which are therefore characterized by high aggressiveness and by a dramatically rapid growth rate [27]. On the other hand, this might be due to the unspecific semeiology of SNUTCs. Presenting symptoms are varied and extremely non-specific, ranging from headache, rhinorrhea, and nasal obstruction to blurred vision, diplopia, and conjunctival chemosis. For this reason, it is not uncommon for this neoplasm to be treated initially as a benign condition (e.g., with antibiotics and systemic steroids), thus contributing to delaying proper treatment. In our review, only two patients presented with an early stage of SNUTC at diagnosis. In particular, a 54-year-old woman presented with a stage II neoplasm (cT2N0Mx) consisting in a 2.5 × 2 cm mass that involved her right nasal bone without evidence of regional or distant metastasis. She received intensity-modulated radiation therapy (IMRT) and concurrent CT (cisplatin) with no benefit on tumor growth and, subsequently, a second-line therapy based on CRT with ifosfamide/etoposide with concurrent RT, achieving only a partial response that ultimately resulted in the patient’s death only 7 months after diagnosis [3]. The second patient who presented in an early stage was a 65-year-old man with a cT1N0 SNUTC (stage I) arising in his nasal cavity. He was treated with radical surgical resection and with RT as adjuvant therapy with a complete response and without evidence of disease at the end of his follow-up period (which lasted for 108 months) [19].
High stage at diagnosis and aggressive behavior account for the dramatically poor prognosis of this condition, well-represented by collected data. If we consider the final outcome of treatment for patients included in this review, only three out of 25 patients were AWOD at the end of follow-up, and 1 patient was reported as AWD. Since our goal in this work is to provide the more appropriate therapeutic strategy for the treatment of SNUTC, a detailed treatment profile of each of these subjects is shown. In addition to the patient of Laco et al. already reported in the previous paragraph (who survived without disease for at least 108 months after surgery and adjuvant RT) [19], Lee et al. in their case series presented, among the other patients affected by the same malignancy, a 45-year-old woman which showed at her diagnosis a IVa SNUTC (pT4) of left ethmoid sinus initially treated with radical surgery for the suspicion of a cancerous change of inverted papilloma. After the right diagnosis of SNUTC, she received another radical surgical procedure consisting of a left anterior skull base craniofacial resection and a medial maxillectomy. She also received adjuvant concurrent CRT with cisplatin, obtaining a complete response without being reminded of a second-line therapy and showing an OS of 36 months [20]. Muramatsu et al. presented an 18-year-old woman with a SNUTC of the nasal cavity already in a IVb stage (cT4bN0) at diagnosis, treated with CRT based on vincristine, doxorubicin, cyclophosphamide plus RT (70 Gy/35 Fr) as primary treatment, which obtained complete response with a DFS of 9 months. She successively received second-line treatment with proton beam radiotherapy (PBR) due to a recurrence of the tumor in her left ethmoid sinus with skull base invasion. Her OS at the end of her follow-up period was 18 months without recurrence of the SNUTC [22]. Lastly, the only patient who resulted as AWD was a 39-year-old man who presented with a IVc SNUTC and, due to the high PD-L1 score on his specimen, consented to a clinical trial combining a PD-L1 checkpoint inhibitor and a Toll-like receptor 7 (TLR7) agonist, resulting in progression of disease at the end of the treatment. Therefore, he received RT as second-line therapy followed by CT with gemcitabine and paclitaxel (obtaining a progression-free survival of 9 months) and, lastly, he started another clinical trial based on a Bromodomain and extra terminal protein (BET) inhibitor. At the end of his follow-up period, he was AWD showing an OS of 21 months [24]. An important limitation of this review consists of the huge variability of the follow-up period of the included patients, which could lead to an important bias in the interpretation of the presented data. For example, the patient presented by Muramatsu et al. ended her follow-up period as AWOD after 18 months [22] but, on the other hand, the case reported by Klijanienko et al. showed a DFD outcome with a longer follow up-period and with a longer OS (22 months) [18]. This means that the length of the follow-up invariably affects the final outcome of the patients.
In conclusion, on the basis of our extrapolated data, some considerations are mandatory. First of all, even if most patients presented with an already advanced stage, an early stage (I or II) at presentation does not represent a guarantee of better success of the proposed therapy. In fact, of the two subjects which showed an early stage SNUTC, only one resulted as AWOD at his final outcome. Conversely, we detected other two patients who were AWOD despite presenting with a IVa and IVb stage, respectively. Moreover, among the three patients who showed no recurrence at the end of their follow-up period, we did not detect a similar strategy approach among them. In fact, they all received an individualized therapy scheme that varied with each other and that does not allow a common and standardized line of treatment to be defined. This may lead to the assertion that a self-personalized strategy of therapy should be drawn on each patient affected by SNUTC, which could be ideally based on the patient’s age and history, on the molecular characterization of his illness, and on the experience of the oncological team of each center.
Data availability
All data pertaining to this systematic review are available from the corresponding author upon reasonable request.
References
French CA, Kutok JL, Faquin WC, Toretsky JA, Antonescu CR, Griffin CA et al (2004) Minline carcinoma of children and young adults with NUT rearrangement. J Clin Oncol 22(20):4135–4139. https://doi.org/10.1200/JCO.2004.02.107
Haack H, Johnson LA, Fry CJ, Crosby K, Polakiewicz RD, Stelow EB et al (2009) Diagnosis of NUT midline carcinoma using a NUT-specific monoclonal antibody. Am J Surg Pathol 33(7):984–991. https://doi.org/10.1097/PAS.0b013e318198d666
Davis BN, Karabakhtsian RG, Pettigrew AL, Arnold SM, French CA, Brill YM (2011) Nuclear protein in testis midline carcinomas: a lethal and underrecognized entity. Arch Pathol Lab Med 135(11):1494–1498. https://doi.org/10.5858/arpa.2010-0389-CR
Elkhatib SK, Neilsen BK, Sleightholm RL, Baine MJ, Zhen W (2019) A 47-year-old woman with nuclear protein in testis midline carcinoma masquerading as a sinus infection: a case report and review of the literature. J Med Case Rep 13(1):57. https://doi.org/10.1186/s13256-019-2015-x
Hsieh MS, French CA, Liang CW, Hsiao CH (2011) NUT midline carcinoma: case report and review of the literature. Int J Surg Pathol 19(6):808–812. https://doi.org/10.1177/1066896909353600
Chau NG, Hurwitz S, Mitchell CM, Aserlind A, Grunfeld N, Kaplan L et al (2016) Intensive treatment and survival outcomes in NUT midline carcinoma of the head and neck. Cancer 122(23):3632–3640. https://doi.org/10.1002/cncr.30242
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700. https://doi.org/10.1136/bmj.b2700
National Heart, Lung and Blood Institute (2013) Study quality assessment tools. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
The Joanna Briggs Institute (2017) Critical appraisal tools—checklist for cases reports. https://jbi.global/sites/default/files/2019-05/JBI_Critical_Appraisal-Checklist_for_Case_Reports2017_0.pdf
Saibene AM, Rosso C, Felisati G, Pignataro L, Schindler A, Ghilardi G et al (2023) Sirolimus treatment for paediatric head and neck lymphatic malformations: a systematic review. Eur Arch Otorhinolaryngol 280(8):3529–3540. https://doi.org/10.1007/s00405-023-07991-1
Centre for Evidence-Based Medicine (2011) OCEBM levels of evidence. https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence
Abreu RF, Oliveira TB, Hertzler H, Toledo RN, D’Almeida Costa F, Lopes Pinto CA et al (2022) NUT carcinoma, an under-recognized malignancy: a clinicopathologic and molecular series of 6 cases showing a subset of patients with better prognosis and a rare ZNF532::NUTM1 fusion. Hum Pathol. 126:87–99. https://doi.org/10.1016/j.humpath.2022.05.015
Arimizu K, Hirano G, Makiyama C, Matsuo M, Sasaguri T, Makiyama A (2018) NUT carcinoma of the nasal cavity that responded to a chemotherapy regimen for Ewing’s sarcoma family of tumors: a case report. BMC Cancer 18(1):1134. https://doi.org/10.1186/s12885-018-5087-x
Bishop JA, Westra WH (2012) NUT midline carcinomas of the sinonasal tract. Am J Surg Pathol 36(8):1216–1221. https://doi.org/10.1097/PAS.0b013e318254ce54
Chan W, Bullock MJ, Samad AF, Archibald CW, Heathcote JG (2018) NUT carcinoma of the sinonasal tract infiltrating the orbit in a man with birdshot chorioretinitis. Saudi J Ophthalmol Jan-Mar 32(1):62–65. https://doi.org/10.1016/j.sjopt.2018.02.018
Crocetta FM, Botti C, Fornaciari M, Castellucci A, Murri D, Santandrea G et al (2021) Sinonasal NUT carcinoma: delayed diagnosis due to the COVID-19 pandemic and a review of the literature. Head Neck Pathol 15(4):1409–1414. https://doi.org/10.1007/s12105-021-01311-x
Huang WP, Gao G, Qiu YK, Yang Q, Song LL, Chen Z et al (2022) Multimodality imaging and treatment of paranasal sinuses nuclear protein in testis carcinoma: a case report. World J Clin Cases 10(33):12395–12403. https://doi.org/10.12998/wjcc.v10.i33.12395
Klijanienko J, Le Tourneau C, Rodriguez J, Caly M, Theocharis S (2016) Cytological features of NUT midline carcinoma arising in sino-nasal tract and parotid gland: report of two new cases and review of the literature. Diagn Cytopathol 44(9):753–756. https://doi.org/10.1002/dc.23506
Laco J, Kovarikova H, Chmelarova M, Vosmikova H, Sieglova K, Bubancova I et al (2018) Analysis of DNA methylation and microRNA expression in NUT (nuclear protein in testis) midline carcinoma of the sinonasal tract: a clinicopathological, immunohistochemical and molecular genetic study. Neoplasma 65(1):113–123. https://doi.org/10.4149/neo_2018_161122N581
Lee T, Cho J, Baek CH, Son YI, Jeong HS, Chung MK et al (2020) Prevalence of NUT carcinoma in head and neck: analysis of 362 cases with literature review. Head Neck 42(5):924–938. https://doi.org/10.1002/hed.26067
Maloley L, Helvey J, Bridge J, DiMaio D, Ghate D, Kedar S (2019) A tough NUT to crack: a 47-year-old with diplopia from a rare malignancy. J Neuroophthalmol 39(1):129–133. https://doi.org/10.1097/WNO.0000000000000747
Muramatsu J, Takada K, Sugita S, Tsuchiya T, Yamamoto K, Takagi M et al (2022) Complete response induced by concurrent chemoradiotherapy in a patient with NUT carcinoma. Intern Med 61(8):1299–1304. https://doi.org/10.2169/internalmedicine.7741-21
Oliveira LJC, Gongora ABL, Latancia MT, Barbosa FG, Gregorio JVAM, Testagrossa LA et al (2019) The first report of molecular characterized BRD4-NUT carcinoma in Brazil: a case report. J Med Case Rep 13(1):279. https://doi.org/10.1186/s13256-019-2213-6
Patel SA, Singer B, Shen C, Zanation AM, Yarbrough WG, Weiss J (2021) A case of metastatic NUT carcinoma with prolonged response on gemcitabine and nab-paclitaxel. Clin Case Rep 9(8):e04616. https://doi.org/10.1002/ccr3.4616
Stirnweiss A, McCarthy K, Oommen J, Crook ML, Hardy K, Kees UR et al (2015) A novel BRD4-NUT fusion in an undifferentiated sinonasal tumor highlights alternative splicing as a contributing oncogenic factor in NUT midline carcinoma. Oncogenesis 4(11):e174. https://doi.org/10.1038/oncsis.2015.33
Tosic L, Voglis S, Reuss AM, Rushing EJ, Regli L, Serra C (2022) Intra-, para-, and suprasellar nuclear protein of testis carcinoma with infiltration of cavernous sinus and clivus-a case report. Acta Neurochir (Wien) 164(4):1105–1110. https://doi.org/10.1007/s00701-021-05065-x
French CA (2018) NUT carcinoma: clinicopathologic features, pathogenesis, and treatment. Pathol Int 68(11):583–595. https://doi.org/10.1111/pin.12727
Funding
Open access funding provided by Università degli Studi di Torino within the CRUI-CARE Agreement. The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no potential conflict of interest or financial disclosures pertaining to this article.
Ethical standards
The review did not involve human participants and/or animals. For this reason, no informed consent was collected.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Urbanelli, A., Nitro, L., Pipolo, C. et al. Therapeutic approaches to sinonasal NUT carcinoma: a systematic review. Eur Arch Otorhinolaryngol 281, 3361–3369 (2024). https://doi.org/10.1007/s00405-024-08489-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-024-08489-0