Abstract
Objectives
Sudden sensorineural hearing loss (SSNHL) is one of the common emergencies in otorhinolaryngology. Several studies have shown that chronic inflammation is associated with its onset and prognosis. However, the association between some inflammatory biomarkers and SSNHL is still unclear. Therefore, we conducted this meta-analysis to explore the value of inflammatory biomarkers in the occurrence and prognosis of SSNHL.
Methods
Pubmed, Embase, Cochrane and Web of Science databases were searched comprehensively, the eligible literatures were screened out by formulating the inclusion criteria and exclusion criteria. After extracting sample size, mean and standard deviation, we performed meta-analysis with standardized mean deviation (SMD) and 95% confidence interval (CI) as effect sizes.
Results
A total of 17 articles were included in this meta-analysis, including 2852 subjects, 1423 patients and 1429 healthy controls. The results of meta-analysis showed that the neutrophil-to-lymphocyte ratio (NLR) of the experimental group was significantly higher than the control group (SMD = 1.05, 95% CI 0.87–1.24, P < 0.001), the NLR of the recovery group was significantly lower than the unrecovered group (SMD = 0.68, 95% CI 0.27–1.08, P < 0.05); The platelet-to-lymphocyte ratio (PLR) of the experimental group was significantly higher than the control group (SMD = 0.55, 95% CI 0.34–0.76, P < 0.05), the PLR of the recovery group was significantly lower than the unrecovered group (SMD = 0.44, 95% CI 0.05–0.82, P < 0.05); The C-reactive protein-to-serum albumin ratio (CRP/Alb) of the experimental group was significantly higher than the control group (SMD = 0.39, 95% CI 0.04–0.74, P < 0.05).
Conclusions
The results showed that high NLR, PLR, and CRP/Alb indicated the occurrence of SSNHL, NLR and PLR could predict prognosis of SSNHL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sudden sensorineural hearing loss (SSNHL) occurs suddenly within 72 h, at least three adjacent frequencies of hearing loss > 30 dB. Meanwhile, SSNHL are often accompanied by tinnitus, dizziness, nausea and vomiting, etc. [1]. It is reported that the incidence of SSNHL ranges from 5 to 20 people per 100,000 people per year [2], showing a younger tendency. It is generally believed that SSNHL is caused by viral infections, circulatory disorders, autoimmune defects, tumors, ototoxic drugs, etc. Some scholars [3] believed that chronic inflammation may participate in the occurrence of SSNHL. On one hand [4], the cochlear blood supply mainly depends on a single labyrinthine artery. Long-term inflammation leads to vascular sclerosis and permeability change, resulting in insufficient blood supply to the inner ear, and the production of endolymphatic potential was decreased, affecting the hearing conduction [5, 6]; On the other hand [7], inflammation leads to endothelial dysfunction and hypercoagulability of blood, which accelerates thrombosis and disorders the auditory system. Studies [8] have shown that various inflammatory factors, such as leukocyte count, neutrophil count, platelet-related parameters, natural killer cell activity, interleukin-6 (IL-6), hypersensitivity C-reactive protein, tumor necrosis factor, are closely related to SSNHL. However, few scholars have paid attention to the relationship between compound inflammatory parameters and SSNHL. Stress theory [9] showed that excessive fatigue and negative life events can lead to SSNHL, and the depression score of SSNHL patients is significantly higher than that of normal people, which indicated that stress is also participates in the occurrence of SSNHL. When the body is in a state of stress, the hypothalamic–pituitary–adrenal cortical axis is activated, and the immune cells are induced to secrete pro-inflammatory factors, resulting in vascular endothelial function impaired. The accumulation of inflammatory factors represented by leukocytes, neutrophils and platelets, leading to the formation of thrombosis or plaque, and affecting the blood supply of inner ear. It is also reported [10] that IL-6 receptor is located in the supporting cells of Corti organ in the mouse cochlea, and long-term noise exposure can induce the expression of IL-6. The application of anti-IL-6 receptor antibody can reduce the binding of IL-6 to the receptor and improve the hearing impairment caused by noise exposure. SSNHL is caused by multiple genetic and environmental factors, and inflammatory pathway-related genes are identified as key factor. The IL-1A-889C/T and IL-1B-511C/T polymorphisms have been found to be associated with SSNHL, the platelet GPIaC807T [11] gene is related to negative outcomes of SSNHL.
In addition, several studies [12] demonstrated that neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio(PLR) can be used as new inflammatory biomarkers, which are independent prognostic factors of cardiovascular disease [13]. It is also associated with the prognosis of various malignant tumors (head and neck squamous cell carcinoma, gastric adenocarcinoma [12], non-small cell lung cancer [14], breast cancer [15], endometrial cancer [16]). Compared with single inflammatory biomarker, they are more stable and less affected by surrounding environment, reflect two immune pathways. Ulu et al. [17] first proposed that NLR can be used as a rapid and reliable new indicator for the occurrence and prognosis of SSNHL. Previous study [18] pointed out that PLR was associated with peripheral arterial diseases (such as limb ischemia and atherosclerosis) and low-grade systemic inflammatory response, which could be a potential prognostic marker. Many scholars [19,20,21] have confirmed that PLR was crucial in the occurrence and development of SSNHL. However, the results are still controversial due to the limited sample size and heterogeneity of studies. Based on the study of chronic inflammation, some scholars [22] paid attention to CRP, although it was an acute phase protein, but it was related to the prognosis of inflammatory response in some malignant tumors. Likewise, the chronic phase protein–Alb was thought to be associated with cancer survival outcomes. It has been [23] proved that CRP/Alb not only reflected the nutritional status of tumor patients, but also reflected the systemic inflammatory response. Therefore, some scholars have done relevant research and found that C-reactive protein-to-albumin ratio (CRP/Alb) is related to the prognosis of SSNHL [24], but this conclusion is still not clear. Therefore, we performed this meta-analysis to evaluate the value of NLR, PLR, and CRP/Alb in the occurrence and prognosis of SSNHL.
Materials and methods
Literature research
We comprehensively searched Pubmed, Embase, Cochrane, web of science databases with a computer. We used the following keywords, such as "Sudden sensorineural hearing loss", "Idiopathic sudden sensorineural hearing loss", "SSNHL", "ISSNHL", "Neutrophil-to-lymphocyte ratio", "NLR", "Platelet-to-lymphocyte ratio", "PLR", "C-reactive protein", "serum albumin", "CRP/ALB", making as many combinations as possible. The search period was from 2013 to 2021.
Inclusion and exclusion criteria
Inclusion criteria: the included literatures are randomized controlled trials, cohort studies or case–control studies. Each study contains at least one inflammatory marker related to SSNHL, and provides accurate data, including sample size, mean, and standard deviation for meta-analysis. Exclusion criteria: reviews, case reports, comments, conference abstracts, letter articles, and those lacking data are excluded.
Data extraction and quality assessment
Data extraction was performed by two investigators. Basic information was extracted from eligible studies, including: investigator, year of publication, country, gender, mean age, treatment style. The Newcastle scale was used to assess the methodological quality of 17 studies. Scores range from 0 to 9, Score ≥ 5 indicated that the literature was of high quality and can be included in the meta-analysis, and score < 5 indicated that the included literature was of poor quality and should be excluded. The results of quality assessment were shown in Table 1.
Statistical analysis
The original data were analyzed by Stata version 16.0. The relationship between NLR, PLR, CRP/Alb and the diagnosis and prognosis of SSNHL was evaluated by mean and standard deviation. The heterogeneity of the studies was assessed by I2. I2 > 50% indicated high heterogeneity, and we used random-effect model. Instead, I2 < 50% indicated less heterogeneity, and we used fixed-effect model. Meanwhile, sensitivity analysis was used to verify the stability of the conclusions. The Begg's and Egger's tests were used to assess the publication bias. P < 0.05 was considered statistically significant.
Results
Baseline characteristics of included studies
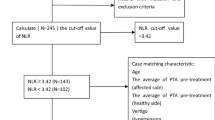
We identified 265 studies through systematic literature search, 248 studies that did not meet the requirements were excluded, and the final 17 studies were included in the meta-analysis (Fig. 1). The 17 studies were come from 4 countries (China, Korea, Turkey, Japan), with a total of 2852 subjects, including 1423 SSNHL patients and 1429 healthy controls. 13 studies provided NLR data for experimental and control groups, and 10 studies provided NLR data for recovered and unrecovered groups. 9 studies provided PLR data for experimental and control groups, 7 studies provided PLR data for recovered and unrecovered groups. 2 studies provided CRP/Alb data for experimental and control groups. The basic information for all included studies was shown in Table 1.
Results of meta-analysis
Meta-analysis of NLR in the occurrence of SSNHL
13 studies provided complete data, including 1107 SSNHL patients and 1208 healthy controls. The heterogeneity test showed that there was high heterogeneity among the studies (I2 = 70.9%, P < 0.001), so the random-effects model was used for analysis. The results of meta-analysis showed that NLR in SSNHL group was significantly higher than control group (SMD = 1.05, 95% CI 0.87–1.24, P < 0.001), indicating that high NLR may play a role in the occurrence of SSNHL (Fig. 2).
Meta-analysis of NLR in the prognosis of SSNHL
10 studies provided post-treatment NLR data, including 585 patients with hearing recovered and 366 patients with hearing unrecovered. The heterogeneity test indicated that high heterogeneity among the studies (I2 = 86.1%, P < 0.001), so the random-effects model was adopted. The results showed that NLR in the unrecovered group was significantly higher than the recovered group (SMD = 0.68, 95% CI 0.27–1.08, P < 0.05), indicating that SSNHL patients with high NLR has a worse prognosis (Fig. 3).
Meta-analysis of PLR in the occurrence of SSNHL
9 studies provided pre-treatment PLR data, including 792 SSNHL patients and 932 healthy controls. The heterogeneity test indicated that there was high heterogeneity among the studies (I2 = 68.1%, P < 0.05), so we selected the random-effects model. The results showed that PLR in the experimental group was significantly higher than the control group (SMD = 0.55, 95% CI 0.34–0.76, P < 0.05). Thus, high PLR may play a role in the occurrence of SSHNL (Fig. 4).
Meta-analysis of PLR in the prognosis of SSNHL
7 studies provided post-treatment PLR data, including 475 patients with hearing recovered and 288 patients with hearing unrecovered. The heterogeneity test indicated that high heterogeneity among studies (I2 = 79.4%, P < 0.001), so the random-effects model was adopted. The results showed that PLR in the unrecovered group was significantly higher than the recovered group (SMD = 0.44, 95% CI 0.05–0.82, P < 0.05), indicating that SSNHL patients with high PLR has a worse prognosis (Fig. 5).
Meta-analysis of CRP/Alb in the occurrence of SSNHL
2 studies provided CRP/Alb data, including 209 SSNHL patients and 177 healthy controls. The heterogeneity test showed that high heterogeneity (I2 = 54.7%, P = 0.138), so the random-effects model was adopted. The results showed that CRP/Alb in the experimental group was significantly higher than the control group (SMD = 0.39, 95% CI 0.04–0.74, P < 0.05), so high CRP/Alb may play an important role in the occurrence of SSNHL (Fig. 6).
Subgroup analysis
Due to high heterogeneity of the studies, we conducted the subgroup analysis to find the source of heterogeneity. The results showed that year, hormone type, quality score, sample size, and publication country were the sources of heterogeneity of relationship between NLR and the occurrence of SSNHL (Table 2).
Sensitivity analysis and publication bias
Owing to high heterogeneity of the included studies, we used sensitivity analysis to verify the reliability of the meta-analysis. After excluded each study, the results of the meta-analysis did not change, indicating that the conclusions of the meta-analysis are stable and reliable. Publication bias was assessed by Begg's test and Egger's test. In the Begg's test, the P values of NLR associated with the occurrence and prognosis of SSNHL were 0.583 and 0.107, respectively. The P values of PLR associated with the occurrence and prognosis of SSNHL were 0.466 and 0.764, respectively. The P values of CRP/Alb associated with the occurrence of SSNHL was 1.000. In the Egger's test, the P values of NLR associated with the occurrence and prognosis of SSNHL were 0.871 and 0.389, respectively. The P values of PLR associated with the occurrence and prognosis of SSNHL were 0.237 and 0.781, respectively. Therefore, there was no publication bias in our meta-analysis.
Discussion
With the development of social economy, people’s pressure is gradually increasing, and the incidence of SSNHL is also increasing, and the trend is younger. Early intervention is essential. Grasping the golden treatment period and save the residual hearing should understand the pathogenesis of SSNHL. In general, there are four recognized theories on the pathogenesis of SSNHL: virus infection and immunity theory[37], endolymphatic hydrops [9], stress theory [38, 39], microcirculation disorders [40, 41]. The treatment of SSNHL including hormone anti-inflammatory (methylprednisolone, dexamethasone), trophic nerve (Mecobalamin), vasodilator (salvia miltiorrhiza injection, ginkgo biloba extract injection), but the efficacy is varied. Recently, some scholars [3, 10] believed that chronic inflammation may be involved in the occurrence of SSNHL. SSNHL is mostly acute. The stress mechanism [9] of the body is activated, and inflammatory cells release inflammatory factors and chemokines. Due to the high sensitivity of cochlear vascular system to inflammatory factors, it may lead to vascular damaged and the disruption of blood labyrinth barrier, which is not conducive to the generation of endolymphatic potential and auditory conduction. Besides, the surface of vascular endothelial cells is covered with glycocalyx [42], which can block the damage of immune cells and serum macromolecules to vascular endothelium. Once the body is in an inflammatory state, it can stimulate endothelial cells to produce adhesion molecules, which will peel off the glycocalyx and destroy the tight connection, thus allowing inflammatory factors to enter the surrounding tissues and damaging the auditory homeostasis. On the other hand, long-term chronic inflammation makes the blood of SSNHL patients in a hypercoagulable state [43, 44], which is easy to form thrombus and cause microcirculation disorders of the inner ear system. However, the inner ear [45] system mainly relies on the labyrinthine artery for blood supply, and the lack of sufficient blood affects the growth and development of cochlear hair cells, and the auditory conduction cannot be completed. Various inflammatory factors [3] such as leukocytes, neutrophils, lymphocytes, platelets, interleukins, tumor necrosis factor, fibrinogen, hypersensitive C-reactive protein have been proved to be involved in the occurrence and development of SSNHL, but the predictive value is limited. Recently, a study [4] pointed out that the compound inflammatory markers NLR and PLR have higher value and lower cost for the occurrence and prognosis of SSNHL than single inflammatory indicator, which are easy to calculate. Furthermore, CRP is a marker for short-term inflammation and Alb is a marker for long-term inflammation. The prognostic value of CRP/Alb has been demonstrated in inflammation-based tumors [22, 46, 47].
In this meta-analysis, we included 17 studies with 2852 subjects, including 1423 SSNHL patients and 1429 healthy controls. The results of meta-analysis showed that NLR, PLR and CRP/Alb in the SSNHL group were significantly higher than the control group. NLR and PLR in the recovery group were significantly lower than the unrecovered group after hormone treatment. Due to the heterogeneity of study, subgroup analysis and sensitivity analysis were performed, and we found that the results of meta-analysis remained stable after excluded each study. Meanwhile, the Begg's test and the Egger's test indicated no publication bias. Therefore, NLR, PLR, and CRP/Alb could be used as inflammatory biomarkers for the occurrence of SSNHL. NLR and PLR could be used as indicators to evaluate the prognosis of SSNHL.
Although Ni et al. [48] conducted a meta-analysis on the relationship between SSNHL and NLR, PLR, but the conclusion was still controversial. First of all, in our meta-analysis, more studies were included, the sample size was larger, and the conclusions were more reliable. Second, we explored the sources of heterogeneity in this study through subgroup analysis. Year, the type of hormone, the score of literature quality, sample size, and the country of issue were the sources of heterogeneity. However, Ni's study only showed that hematology analyzers and brand audiometry device had an impact on the results. Moreover, we added the analysis of the relationship between CRP/Alb and SSNHL, and the results showed that CRP/Alb may play an important role in the occurrence of SSNHL. The research indicators selected in this paper are all composite indicators, which are more stable than single inflammatory parameters. In addition, they can give more clinical guidance and provide a new idea for exploring the impact of more composite indicators on SSNHL in the future.
However, this study also had some limitations. Firstly, most of included literatures in this meta-analysis were retrospective studies, which had lower quality compared with randomized controlled studies. Second, due to the difference of treatment plan, treatment cycle and follow-up time, the lack of unified standard, there had some heterogeneity. Finally, there were few studies on CRP/Alb and SSNHL, and the conclusions are not convincing. More prospective studies are needed to further verify the value of CRP/Alb in the occurrence and prognosis of SSNHL.
Conclusions
In conclusion, NLR, PLR and CRP/Alb are closely related to the occurrence of SSNHL. NLR, PLR and CRP/Alb are compound inflammatory markers, which are more stable than single inflammatory cells and CRP. Moreover, they are routine hematological parameters, easy to measure, cost-effective, which can be used as novel biomarkers for the occurrence and prognosis of SSNHL. In the future, large-sample and high-quality studies are needed to confirm this conclusion, while further explore the relationship between more compound inflammatory biomarkers and SSNHL, such as fibrinogen/albumin, fibrinogen/D-dimer, MPV/PDW, and triglyceride/cholesterol.
Availability of data and materials
The data sets used and analyzed during the current study are available from references on reasonable request.
References
Chandrasekhar SS, Tsai Do BS, Schwartz SR, Bontempo LJ, Faucett EA, Finestone SA, Hollingsworth DB, Kelley DM, Kmucha ST, Moonis G, Poling GL, Roberts JK, Stachler RJ, Zeitler DM, Corrigan MD, Nnacheta LC, Satterfield L, Monjur TM (2019) Clinical practice guideline: sudden hearing loss (Update) executive summary. Otolaryngol Head Neck Surg 161(2):195–210. https://doi.org/10.1177/0194599819859883
Jeon SY, Kang DW, Kim SH, Byun JY, Yeo SG (2022) Prognostic factors associated with recovery from recurrent idiopathic sudden sensorineural hearing loss: retrospective analysis and systematic review. J Clin Med. https://doi.org/10.3390/jcm11051453
Masuda M, Kanzaki S, Minami S, Kikuchi J, Kanzaki J, Sato H, Ogawa K (2012) Correlations of inflammatory biomarkers with the onset and prognosis of idiopathic sudden sensorineural hearing loss. Otol Neurotol 33(7):1142–1150. https://doi.org/10.1097/MAO.0b013e3182635417
Chen L, Zhang G, Zhang Z, Wang Y, Hu L, Wu J (2018) Neutrophil-to-lymphocyte ratio predicts diagnosis and prognosis of idiopathic sudden sensorineural hearing loss: A systematic review and meta-analysis. Medicine (Baltimore) 97(38):e12492. https://doi.org/10.1097/md.0000000000012492
Gates GA, Mills JH (2005) Presbycusis. The lancet 366(9491):1111–1120
Fischer ME, Schubert CR, Nondahl DM, Dalton DS, Huang GH, Keating BJ, Klein BE, Klein R, Tweed TS, Cruickshanks KJ (2015) Subclinical atherosclerosis and increased risk of hearing impairment. Atherosclerosis 238(2):344–349. https://doi.org/10.1016/j.atherosclerosis.2014.12.031
Berjis N, Moeinimehr M, Hashemi SM, Hashemi SM, Bakhtiari EK, Nasiri S (2016) Endothelial dysfunction in patients with sudden sensorineural hearing loss. Adv Biomed Res 5:5. https://doi.org/10.4103/2277-9175.174978
Cao Z, Li Z, Xiang H, Huang S, Gao J, Zhan X, Zheng X, Li B, Wu J, Chen B (2018) Prognostic role of haematological indices in sudden sensorineural hearing loss: review and meta-analysis. Clin Chim Acta 483:104–111. https://doi.org/10.1016/j.cca.2018.04.025
Merchant SN, Durand ML, Adams JC (2008) Sudden deafness: is it viral? Orl 70(1):52–62
Hiramatsu M, Teranishi M, Uchida Y, Nishio N, Suzuki H, Kato K, Otake H, Yoshida T, Tagaya M, Suzuki H (2012) Polymorphisms in genes involved in inflammatory pathways in patients with sudden sensorineural hearing loss. J Neurogenet 26(3–4):387–396
Rudack C, Langer C, Junker R (2004) Platelet GPIaC807T polymorphism is associated with negative outcome of sudden hearing loss. Hear Res 191(1–2):41–48. https://doi.org/10.1016/j.heares.2004.01.002
Varol E, Aksoy F, Ozaydin M, Erdogan D, Dogan A (2013) Relationship between mean platelet volume and mitral annular calcification. Blood Coagul Fibrinolysis 24(2):189–193. https://doi.org/10.1097/MBC.0b013e32835b7296
Liao Y, Liu K, Zhu L (2022) Emerging roles of inflammasomes in cardiovascular diseases. Front Immunol 13:834289. https://doi.org/10.3389/fimmu.2022.834289
Booka E, Kikuchi H, Haneda R, Soneda W, Kawata S, Murakami T, Matsumoto T, Hiramatsu Y, Takeuchi H (2022) Neutrophil-to-lymphocyte ratio to predict the efficacy of immune checkpoint inhibitor in upper gastrointestinal cancer. Anticancer Res 42(6):2977–2987. https://doi.org/10.21873/anticanres.15781
WiraWiguna IGW, IndraniRemitha NPS, Sadvika I, Wiranata S, Putra I, Adiputra PAT, Supadmanaba IGP, Wihandani DM (2022) Pretreatment leukocyte count ratios as metastatic predictive factors in luminal type breast cancer. Asian Pac J Cancer Prev 23(5):1595–1601. https://doi.org/10.31557/apjcp.2022.23.5.1595
Leng J, Wu F, Zhang L (2022) Prognostic significance of pretreatment neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, or monocyte-to-lymphocyte ratio in endometrial neoplasms: a systematic review and meta-analysis. Front Oncol 12:734948. https://doi.org/10.3389/fonc.2022.734948
Ulu S, Ulu MS, Bucak A, Ahsen A, Yucedag F, Aycicek A (2013) Neutrophil-to-lymphocyte ratio as a new, quick, and reliable indicator for predicting diagnosis and prognosis of idiopathic sudden sensorineural hearing loss. Otol Neurotol 34(8):1400–1404. https://doi.org/10.1097/MAO.0b013e31829b57df
Taşoğlu İ, Sert D, Colak N, Uzun A, Songur M, Ecevit A (2014) Neutrophil-lymphocyte ratio and the platelet-lymphocyte ratio predict the limb survival in critical limb ischemia. Clin Appl Thromb Hemost 20(6):645–650. https://doi.org/10.1177/1076029613475474
Koçak HE, Elbistanlı MS, Acıpayam H, Alakras WME, Kıral MN, Kayhan FT (2017) Are neutrophil/lymphocyte and platelet/lymphocyte ratios related with formation of sudden hearing loss and its prognosis? Eur Ann Otorhinolaryngol Head Neck Dis 134(6):383–386. https://doi.org/10.1016/j.anorl.2016.06.005
Ha R, Lim BW, Kim DH, Park JW, Cho CH, Lee JH (2019) Predictive values of neutroph il to lymphocyte ratio (NLR), platelet to lymphocyte ratio (PLR), and other prognostic factors in pediatric idiopathic sudden sensorineural hearing loss. Int J Pediatr Otorhino laryngol 120:134–139. https://doi.org/10.1016/j.ijporl.2019.02.023
Seo YJ, Jeong JH, Choi JY, Moon IS (2014) Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio: novel markers for diagnosis and prognosis in patients with idiopathic sudden sensorineural hearing loss. Dis Mark. https://doi.org/10.1155/2014/702807
Liu X, Sun X, Liu J, Kong P, Chen S, Zhan Y, Xu D (2015) Preoperative C-reactive protein/albumin ratio predicts prognosis of patients after curative resection for gastric cancer. Transl Oncol 8(4):339–345. https://doi.org/10.1016/j.tranon.2015.06.006
Kaplan M, Ates I, Akpinar MY, Yuksel M, Kuzu UB, Kacar S, Coskun O, Kayacetin E (2017) Predictive value of C-reactive protein/albumin ratio in acute pancreatitis. Hepatobil Pancreat Dis Int 16(4):424–430. https://doi.org/10.1016/s1499-3872(17)60007-9
Öçal R, Akın Öçal FC, Güllüev M, Alataş N (2020) Is the C-reactive protein/albumin ratioa prognostic and predictive factor in sudden hearing loss? Braz J Otorhinolaryngol 86(2):180–184. https://doi.org/10.1016/j.bjorl.2018.10.007
Özler GS (2014) Increased neutrophil-lymphocyte ratio in patients with idiopathic sudden sensorineural hearing loss. J Craniofac Surg 25(3):e260-263. https://doi.org/10.1097/scs.0000000000000565
İkincioğulları A, Köseoğlu S, Kılıç M, Atan D, Özcan KM, Çetin MA, Ensari S, Dere HH (2014) New inflammation parameters in sudden sensorineural hearing loss: neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio. Int Adv Otol 10(3):197–200
Kum RO, Ozcan M, Baklaci D, Yurtsever Kum N, Yilmaz YF, Unal A, Avci Y (2015) Investigation of neutrophil-to-lymphocyte ratio and mean platelet volume in sudden hearing loss. Braz J Otorhinolaryngol 81(6):636–641. https://doi.org/10.1016/j.bjorl.2015.08.009
Durmuş K, Terzi H, Karataş TD, Doğan M, Uysal I, Şencan M, Altuntaş EE (2016) Assessment of hematological factors involved in development and prognosis of idiopathic sudden sensorineural hearing loss. J Craniofac Surg 27(1):e85-91. https://doi.org/10.1097/scs.0000000000002241
Nonoyama H, Tanigawa T, Shibata R, Nakao Y, Horibe Y, Katahira N, Nishimura K, Murotani K, Murohara T, Ueda H (2016) Red blood cell distribution width predicts prognosis in idiopathic sudden sensorineural hearing loss. Acta Otolaryngol 136(11):1137–1140. https://doi.org/10.1080/00016489.2016.1195919
Lee JS, Hong SK, Kim DH, Lee JH, Lee HJ, Park B, Choi HG, Kong IG, Song HJ, Kim HJ (2017) The neutrophil-to-lymphocyte ratio in children with sudden sensorineural hearing loss: a retrospective study. Acta Otolaryngol 137(1):35–38. https://doi.org/10.1080/00016489.2016.1217561
Bulğurcu S, Dikilitaş B, Arslan İB, Çukurova İ (2017) Neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios in pediatric patients with idiopathic sudden hearing loss. J Int Adv Otol 13(2):217–220. https://doi.org/10.5152/iao.2017.3404
Qiao XF, Li X, Wang GP, Bai YH, Zheng W, Li TL (2019) Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in patients with sudden sensorineural hearing loss. Med Princ Pract 28(1):23–27. https://doi.org/10.1159/000494556
Sancaktar ME, Ağrı İ, Çeçen AB, Akgül G, Çelebi M (2020) The prognostic value of circulating inflammatory cell counts in sudden sensorineural hearing loss and the effect of cardiovascular risk factors. Ear Nose Throat J 99(7):464–469. https://doi.org/10.1177/0145561320920968
Cayir S, Kayabasi S, Hizli O (2021) Predictor parameters for poor prognosis in patients with sudden sensorineural hearing loss: fibrinogen to albumin ratio vs C-reactive protein to albumin ratio. Braz J Otorhinolaryngol 87(4):457–461. https://doi.org/10.1016/j.bjorl.2020.06.010
Çiçek T, ÖzbilenAcar G, Özdamar O (2021) Evaluation of neutrophil/lymphocyte and platelet/lymphocyte ratios in sudden sensorineural hearing loss and relationship with hyperbaric oxygen therapy. J Int Adv Otol 17(2):96–102. https://doi.org/10.5152/iao.2020.7943
Guo Y, Liu J (2021) The roles played by blood inflammatory parameters in sudden sensorineural hearing loss. Ear Nose Throat J. https://doi.org/10.1177/0145561320960355
Shi X, Dong Y, Li Y, Zhao Z, Li H, Qiu S, Li Y, Guo W, Qiao Y (2015) Inflammasome activation in mouse inner ear in response to MCMV induced hearing loss. J Otol 10(4):143–149. https://doi.org/10.1016/j.joto.2015.12.001
Capaccio P, Pignataro L, Gaini LM, Sigismund PE, Novembrino C, De Giuseppe R, Uva V, Tripodi A, Bamonti F (2012) Unbalanced oxidative status in idiopathic sudden sensorineural hearing loss. Eur Arch Otorhinolaryngol 269(2):449–453. https://doi.org/10.1007/s00405-011-1671-2
Gul F, Muderris T, Yalciner G, Sevil E, Bercin S, Ergin M, Babademez MA, Kiris M (2017) A comprehensive study of oxidative stress in sudden hearing loss. Eur Arch Otorhinolaryngol 274(3):1301–1308. https://doi.org/10.1007/s00405-016-4301-1
Guo Y, Zhang C, Du X, Nair U, Yoo TJ (2005) Morphological and functional alterations of the cochlea in apolipoprotein E gene deficient mice. Hear Res 208(1–2):54–67. https://doi.org/10.1016/j.heares.2005.05.010
Mutlu A, Cam I, Dasli S, Topdag M (2018) Doppler ultrasonography can be useful to determine the etiology of idiopathic sudden sensorineural hearing loss. Auris Nasus Larynx 45(3):456–460. https://doi.org/10.1016/j.anl.2017.08.013
Trune DR, Nguyen-Huynh A (2012) Vascular pathophysiology in hearing disorders. Semin Hear 33(3):242–250. https://doi.org/10.1055/s-0032-1315723
Li X, Chen B, Zhou X, Ye F, Wang Y, Hu W (2021) Identification of dyslipidemia as a risk factor for sudden sensorineural hearing loss: a multicenter case-control study. J Clin Lab Anal 35(12):e24067. https://doi.org/10.1002/jcla.24067
Shao M, Xiong G, Xiang G, Xu S, Zhang L (2021) Correlation between serum lipid and prognosis of idiopathic sudden sensorineural hearing loss: a prospective cohort study. Ann Transl Med 9(8):676. https://doi.org/10.21037/atm-21-907
Hesse G (2016) [Inner ear hearing loss part II: sudden sensorineural hearing loss]. Therapeutic options. Laryngorhinootologie 95(7):461–469. https://doi.org/10.1055/s-0042-108379
Zhou T, Zhan J, Hong S, Hu Z, Fang W, Qin T, Ma Y, Yang Y, He X, Zhao Y, Huang Y, Zhao H, Zhang L (2015) Ratio of C-reactive protein/albumin is an inflammatory prognostic score for predicting overall survival of patients with small-cell lung cancer. Sci Rep 5:10481. https://doi.org/10.1038/srep10481
Kinoshita A, Onoda H, Imai N, Iwaku A, Oishi M, Tanaka K, Fushiya N, Koike K, Nishino H, Matsushima M (2015) The C-reactive protein/albumin ratio, a novel inflammation-based prognostic score, predicts outcomes in patients with hepatocellular carcinoma. Ann Surg Oncol 22(3):803–810. https://doi.org/10.1245/s10434-014-4048-0
Ni W, Song SP, Jiang YD (2021) Association between routine hematological parameters and sudden sensorineural hearing loss: a meta-analysis. J Otol 16(1):47–54. https://doi.org/10.1016/j.joto.2020.07.006
Acknowledgements
We would like to thank Professor Zhenhua Zhong and Dr Maohua Wang for reviewing and providing advice on the final search strategy. We thank LetPub (https: //www.letpub.com) for its linguistic assistance during the preparation of this manuscript.
Funding
This work was supported by grants from Jiangsu Province Natural Science Foundation (BK20181221, BK20201220), Doctoral Startup Foundation (2021BS-ZZH).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, L., Wang, M., Zhang, W. et al. The value of inflammatory biomarkers in the occurrence and prognosis of sudden sensorineural hearing loss: a meta-analysis. Eur Arch Otorhinolaryngol 280, 3119–3129 (2023). https://doi.org/10.1007/s00405-022-07806-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07806-9