Abstract
Purpose
To relate the creation and expert validation (face and content validity) of an affordable three-dimensional (3-D) printed model of temporal bones with chronic otitis media with cholesteatoma (COMC) as a simulator for mastoidectomy.
Methods
We performed computed tomography (CT) of the temporal bones of a patient with COMC followed at the University of São Paulo (USP) Hospital with 3-D Slicer to create a 3-D model of the affected bone using light-curing resin and silicone (cholesteatoma). The final 3-D printed images were scored by 10 otologists using a customized version of the Michigan Standard Simulation Scale Experience (MiSSES). Internal consistency and inter-rater reliability were assessed using Cronbach’s α and intraclass correlations.
Results
Otologists consistently scored the model positively for fidelity, educational value, reactions, and the overall model quality. Nine otologists agreed that the model was a good educational device for surgical training of COMC. All experts deemed the model ready—or nearly ready—for use. The final cost of the model, including raw materials and manufacturing, was 120 USD.
Conclusions
Using 3-D printing technology, we created the first anatomically accurate, low-cost, disease-reproducing 3-D model of temporal bones for mastoidectomy training for cholesteatoma.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The application of previously validated methods for teaching surgical skills is modifying the medical, educational environment. Physicians are expected to learn rapidly—especially considering the 80-h weekly limit and increasing demand for operating room efficiency. Current surgical training learning models result in sporadic opportunities to perform specific and uncommon tasks. The role of simulation has gained considerable relevance across all areas, including otolaryngology. Therefore, there is a need for validated physician training simulators for surgical techniques before their use in patients [1,2,3].
Simulations are novel means of providing opportunities to physicians to develop technical skills without jeopardizing patient safety. They are promising and can address the need for training and assessing surgical time efficiency [2, 4, 5].
Advanced computer technology and commercially available three-dimensional (3-D) printing allow simulation of various surgical interventions. Published reports on surgical simulation include applications in general surgery, otolaryngology, neurosurgery, gastroenterology, urology, and cardiovascular surgery [2,3,4,5,6]. In the field of otolaryngology, simulations have been used with excellent results for various procedures; however, no study has reported on temporal bone simulation involving diseases that alter normal anatomy [3, 4].
Cadaveric bone is the gold standard for temporal bone surgical practice. Unfortunately, cadaveric temporal bones are expensive and scarce. Moreover, there are increasingly stringent regulations governing cadaver use. Use of cadavers also precludes use of standardized materials to assess surgical skills and may not adequate depict a patient’s specific features, such as chronic ear disease. This is particularly important for cholesteatoma, which is both common and aggressive. There is an ongoing and unmet need to accurately train otolaryngologists and other specialists without relying on cadaveric specimens [7,8,9,10].
Notwithstanding their standard utility as a training tool, human cadaver bones have various restrictions. Poorly selected donors put persons in contact with temporal bones from human cadavers at risk for illnesses. Moreover, human cadaver bones have a finite “lifespan.” They must be carefully stocked under refrigeration to postpone the decomposition of cadaveric tissues. Moreover, laboratories incur high maintenance costs for collecting bones from cadavers [11].
The use of printed temporal bones is an alternative training method that allows surgeons in training to gain knowledge and develop consistent and assessed skills. This concern gets magnified in the context of competency-based medical education [7].
This study aimed to address a challenging scenario characterized by the dichotomy between the need to increase surgical training and the difficulties imposed by professional training, particularly in otology. In otorhinolaryngology, chronic otitis media with cholesteatoma (COMC) and its therapeutic interventions—including mastoidectomy—challenge even the most experienced surgeons. Use of simulated disease specimens is an innovative alternative for surgical training considering the lack of access to cadaveric temporal bones with corresponding pathology reports.
Here we present the unprecedented creation of a 3D temporal bone with COMC, with our method to design, manufacture and evaluate a high fidelity 3D printed otologic simulator for training in otologic surgery for cholesteatoma. Faced with the difficulty of cadaveric bones for surgical training, the simulator was constructed for various reasons, including low cost, replicability, easy transfer, intuitiveness, ease of assembly, fidelity to real structures, and possibility of surgical training in pathological temporal bone in 3D. Considering the above factors, we designed a 3-D temporal bone with cholesteatoma to simulate mastoidectomy for epitympanic cholesteatoma.
Method
Study design
This descriptive qualitative study used quantitative methods for data analysis and was conducted at the Department of Otorhinolaryngology within the medical school at the University of São Paulo (FMUSP). It was approved by the research ethics committee of the USP Hospital, under opinion 4,734,389.
The project comprised two phases. In phase 1, we created a 3-D printed model of the mastoid of a patient with COMC who was followed at the USP Hospital. The model was evaluated by two experienced in-house otologists. The initial subjective analyses aimed at improving manufacturing, correcting excesses and possible deformities. Following initial evaluation, the model was evaluated in phase 2 by external surgeons with > 20 years of experience in ear surgery, who trained otolaryngologists in tertiary hospitals.
The surgeons were invited to in-person evaluate the model in a monitored environment at the FMUSP Otorhinolaryngological Skills Laboratory Surgery. The work environment was carefully planned to resemble a real operating room and create an experience that simulated daily practice by closely replicating surgical conditions during practice.
Development of a 3-D model of temporal bone with cholesteatoma
The patient selected, with a clinical and radiological diagnosis of pars flaccida cholesteatoma, underwent a non-contrast computed tomography (CT) (Discovery CT750HD—GE medical systems; helical mode; slice thickness 0.625 mm; 120 KVP; Spaces between slices: − 0.312; Data Collection Diameter: 320.0 mm; Rows/Columns: 512 × 512; Window width: 4000; Window level: 800) scan of the temporal bones at the FMUSP Institute of Radiology (InRad). Images were evaluated using the IntelliSpace PACS DCX 3.1, Philips Healthcare software. We digitized high-resolution images with specific reconstruction for the mastoid in DICOM format and imported them into the Slicer 4.11 image computing platform (HTTP: //www. slicer. org). The mastoid bone, internal carotid artery, sigmoid and other venous sinuses, jugular bulb, and dura mater were segmented in this platform. We additionally identified the path of the facial nerve and inner ear structures, whose air spaces were represented. Following the 3-D slicing, we exported as STL file, which represented the mastoid bone and its internal details.
Three-dimensional printing
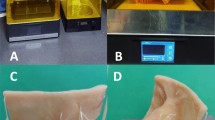
The model was printed, by Form Labs 3L printer, using a light-curing resin (Formlabs White Resin). Nylon filaments were embedded in their pathways represented the facial, cochlear, and vestibular nerves, during the printing.
The cholesteatoma was represented by silicone glue deposited on the topography occupied by the lesion, as identified in the CT study. The insertion of the glue took place during the impression of the model, and the objective was to simulate the cholesteatoma in terms of visual appearance, consistency and removal compared to the in vivo procedure.
The final model weighed 75 g and was 75 × 70 × 45 mm.
Simulator design
The simulator was designed to reproduce the patient’s mastoid dimensions. Considering the surgical position for mastoidectomy, we used the Bento temporal bone support created by the FMUSP, whose mobility can simulate the movements performed in a patient’s ear during in vivo surgery.
To increase realism and didactic potential, the color and appearance of some structures, such as the dura mater of the middle fossa, sigmoid sinus, endolymphatic sac, facial nerve, carotid artery, jugular artery, and internal auditory meatus with cranial nerves VII and VIII, were preserved, facilitating their identification during dissection.
The simulated procedure consisted of mastoidectomy performed on a right temporal bone created in 3-D, which was oriented to expose the anatomical limits/references of the temporal bone (middle fossa dura mater, digastric groove, sigmoid sinus, and lateral canal) to identify the cholesteatoma adjacent to the ossicular chain and for its subsequent removal. The specialist evaluated other otological procedures that might be practiced using the piece.
External evaluation
All external evaluators were selected based on their satisfactory surgical results, recognition by the Brazilian and international otorhinolaryngology communities, and history of teaching otorhinolaryngology—including participation in otorhinolaryngology medical residency programs in Brazil. Inclusion criteria: (i) otologists working in Brazil, according to data from the Brazilian Society of Otology (SBO) and from the Brazilian Association of Otorhinolaryngology and Cervicofacial Surgery (ABORL-CCF), (ii) associated with a public or private university, with its own university hospital, and (iii) current medical residency in Otorhinolaryngology, wherein the otologist acted as a member/preceptor or professor with experience in teaching ear surgery. All external evaluators held at least a doctorate in medical sciences and an academic profile characterized by regular scientific publications in otolaryngology. Moreover, all had performed more than 50 mastoidectomies for upper COMC.
Healthcare professionals were invited to participate in the project through an institutional letter, with space available for surgical simulation at the otolaryngology skills laboratory, USP Hospital.
Evaluation methods
In the second evaluation, the otologists were instructed and trained to submit a questionnaire adapted to the MiSSES template upon completing the simulation.
The MiSSES is an innovative appliance for analyzing subjective experiences with surgical simulation and provides information on the face (i.e., if the model tests or teaches its intended use) and content (i.e., the appropriateness of individual components of the model) validity. It was created as an individualizable template for simulating surgical procedures and includes a Likert-scale questionnaire about surgical fidelity, educational value, and overall quality. Moreover, open-ended questions were added to the model for qualitative assessment. We assessed its internal consistency and inter-rater reliability using Cronbach’s α and intraclass correlation, respectively [4, 12].
The participants were requested to score the 3-D model of cholesteatoma according to each statement on the five-point Likert scale (1 = strongly disagree; 2, disagree; 3, neither agree nor disagree; 4, agree; and 5 = strongly agree). The questionnaire also included questions on demographic and surgical experiences and a comment section for open feedback.
The questionnaire comprised 36 items subdivided into four areas: fidelity/anatomical realism (face validity); educational value, including task-based usefulness and utility as a training tool (content validity); general reactions (overall validity); and overall rating. It was predominantly based on the MiSSES protocol, with questions adapted from other 3-D temporal bone validation studies and 3-D creations focusing on otorhinolaryngology [4, 11, 13,14,15,16].
A score of 3 demonstrated the 3-D-printed synthetic bone as an alternative to human cadaver bone/human temporal bone in a patient with COMC; whereas scores < 3 suggested that the synthetic bone was a pauper substitute for cadavers. Scores ≥ 4 indicated that the 3-D-printed bone was a great replacement for human cadaver temporal bones [11].
Statistical analysis
The categorical variables are presented as relative and absolute frequencies. The questionnaire items are presented as medians and quartiles, without data loss.
We analyzed the internal consistency using Cronbach’s α. The α coefficient fluctuated from 0 to 1, with scores > 0.7 suggesting appropriate reliability. Moreover, we assessed the inter-rater reliability using the intraclass correlation coefficient (ICC). A bidirectional, mixed-effects ICC (“two-way mixed-effects “) was used for single-rater reliability. An ICC of 1 represented complete reliability, whereas a score > 0.8 was considered excellent.
All tests were two-tailed, and p values < 0.05 were considered statistically significant. All analyses were conducted in R programming language (R Core Team, 2021) with the packages “irr” [17] and “ltm” [18].
Results
3-D model construction and development
The 3-D model aimed to reproduce the major anatomical structures of the temporal bone commonly used in surgical dissections as anatomical repair points (Fig. 1). True-to-life colors were used to ensure a realistic simulation. Cholesteatoma was simulated using silicone glue (Fig. 2).
Visual appearance of the 3-D model. A Lateral view of the temporal bone model (1: zygomatic arch, 2: glenoid cavity, 3: mastoid tip, 4: suprameatal spine, 5: external ear canal, and 6: temporal bone scale); B medial view of the temporal bone model (7: sigmoid sinus, 8: internal carotid, 9: jugular vein, and 10: internal ear canal with cranial nerves vii (facial) and viii (vestibulocochlear); C inferior view of the temporal bone model (11: facial nerve); D posterior view of the temporal bone model (12: dura mater)
The dissection by drilling the model also allowed the identification of the internal anatomical structures of the temporal bone, commonly used in otologic surgeries, which were faithfully reproduced in the created model (Figs. 1 and 3).
3D temporal bone dissection with COMC and identification of internal temporal bone anatomical structures. A EAC external ear canal, PWEAC posterior wall of the external auditory canal, MP mastoid tip, MC mastoid cellularity; B SS sigmoid sinus; MA mastoid antrum. C DM dura mater, OC ossicular chain, CT cholesteatoma, HSSC horizontal semi-circular canal, D INC incus, E FN facial nerve, F CO cochlea—visualized by posterior tympanotomy, RW round window, TT stapedius tendon, ST stapes
The model visually reproduced, by silicone glue, the layers of skin that constitute the cholesteatoma, as well as the visual appearance of its removal, with the cleavage plane between the tumor and the temporal bone, as visualized in the in vivo surgery. In addition, the location of the tumor in the specimen reproduced the findings of the patient's CT scan (Fig. 4).
Biomodel validation
Following adjustments in line with the first feedback from the initial assessment (N = 2, Table 1), we presented the final model to 10 otologists from across Brazil between May 2021 and September 2021. Based on the MiSSES survey structure (Tables 1 and 2). All healthcare professionals involved in the evaluation completed all required activities.
The model was highly rated, with items of 4 or higher on all available areas as follows: fidelity, educational value (task-based usefulness and based teaching tool), and overall quality/responsiveness measures, except for cholesteatoma consistency (Table 2, median = 3).
In qualitative assessments, the otologists described the cholesteatoma as denser than normal human tissues, with a more rigid ossicular chain requiring a more malleable dura mater, internal carotid, and sigmoid sinus. Despite these limitations, all (100%) raters stated that the 3-D printed bone could be used in its current state, or with minor changes (Tables 1 and 3).
Overall, the temporal bone model with cholesteatoma received high scores for its use in mastoidectomy training, both in anatomical realism and educational value. The raters agreed that its use would likely facilitate the transfer of skills to the operating room and communication with the patient about the disease before surgery. Moreover, they strongly agreed that the inclusion of the model in the curriculum would systematize teaching mastoidectomy for cholesteatoma; all (100%) raters agreed that the simulator was a good educational device for the surgical treatment of COMC (Table 2). All external evaluators agreed that use of the 3-D simulation model before real-life surgery would likely prepare the trainee surgeon. The evaluators also recommended use of the simulation for training otological residents/surgeons (Table 2).
The Cronbach’s α coefficient scale displayed acceptable overall reliability (α = 0.956), thus demonstrating its ability to consistently measure the results. The inter-rater mean in measuring the ICC was 0.804, with a 95% confidence interval of 0.69″ 0.88, thus indicating a strong correlation.
Each simulation model cost approximately 120 USD, which included all raw materials, equipment costs (printer and curing chamber), physical space, electricity, labor, and chemical products for post-print treatment.
Discussion
Modern medicine and 3-D technology printing are intertwined and the subject of increasing interest within the medical sciences. 3-D printing systems are a subset of rapid prototyping suitable for the low-cost production of custom 3-D objects from easily manageable digital data. 3-D printers are used for surgical training or custom surgical planning by otolaryngologists for their ability to generate geometrically complex targets using various materials [19].
Considering the need for optimized training, novel teaching methods are continually being developed. Despite their limitations (e.g., human anatomy simplifications and lack of validation research), simulations are in common use and offer advantages over traditional surgery. These advantages include the opportunity to practice in a low-risk setting, repeat procedures until mastery is achieved, receive immediate feedback and objective performance evaluation, and simulate less frequently performed procedures. The number of simulation schools has recently increased, partly due to the emergence of advanced modeling technology systems, such as computer-aided design, 3-D printing, and virtual reality [4].
Otology simulators include physical and virtual reality models for performing otoscopy, myringotomy for ventilation tube practice, surgery for otosclerosis, mastoidectomy, and endoscopic otologic surgery. These systems allow better understanding of the movements required during surgery. Some benefits of the otology prototypes include a substantial increase in the hand's precision and stability, increase surgeon’s confidence and a reduction in the surgical time. [3, 20] Our model represented the first simulator on COMC with high fidelity, which used computer-aided design and 3-D printing technologies for its construction. Besides its low cost, the simulator is a unique educational tool for otolaryngologists. This model facilitated the practice of advanced procedure (mastoidectomy) for cholesteatoma, which represents a challenge even for experienced surgeons.
The use of available and affordable materials (such as light-curing resin, nylon filaments and silicone glue) and the availability of surgical skill laboratories made the model accessible and practicable. Moreover, its low cost and portability may facilitate its deployment globally and in international surgical education. This model will add versatility, thereby facilitating the ability to practice specific procedures associated with mastoidectomy, such as canaloplasty, posterior tympanotomy, ossicular chain reconstruction, and training with osteo-anchored prostheses.
In addition to limitations regarding the most valuable resources that hinder otorhinolaryngology training, the ideal training is inexpensive and readily available, but with good face, content, and structure validity [15]. The simulator achieved a good overall rating for its face and content validity; the realism of the temporal bone simulator while evaluating domains—such as anatomical appearance, design, ergonomics, depth perception, and graphical interface—scored favorably in all categories related to face validity. We determined the level to which the simulator taught the intended subject of cortical mastoidectomy across the following domains: surgical anatomy, surgical planning, coordination, and overall usefulness as a training tool. The simulator was comprehensively tested for the domains above and individual temporal bone insertions; it consistently generated positive ratings. The remaining limitations—such as the consistency of cholesteatoma, the absence of tympanic membrane, and the inability to reproduce bleeding/other accidents—did not compromise the rating of the model in the general context, with all raters recommending its use for training.
Most external evaluators stated that 3-D temporal bones with cholesteatoma should be included in the temporal bone dissection training curriculum and that they would recommend the 3-D temporal bone model to other learners. In other words, the 3-D printed model of the temporal bone is an important alternative for training and learning otological procedures [11, 14].
The use of surgical simulators adds real value and enables the acquisition of skill sets that are transferable to the operating room. Moreover, simulation protects all patients by reducing iatrogenic events. These simulations will likely progress sufficiently for their use in pattern testing and certification, particularly for otolaryngology [7].
In otology, numerous 3-D models reproduce anatomical features and represent most studies globally [3] thus, they often become a base for the development of more robust applications of 3-D technology, as in the creation of the Otobone® in our department [21]. However, few studies have reproduced temporal bone diseases, despite being a promising medical development area, particularly considering the possibility of reproducing the disease and simulating the surgical procedure.
With proper physical and anatomical properties to replicate the procedure in the operating room, printed models represent a renewable, safe, and convenient way of introducing the master technique in the absence of biological materials [7].
Microdissection in 3-D printed prototypes improves residents’ surgical performance [9]. Skills developed through the simulator progressively improve student performance on tasks, reduce surgical time and errors, and improve overall patient safety [5]. 3-D printing for surgery planning may be able to reduce surgical time and increase patient and surgeon comfort during surgery [22].
Our study had some limitations. The model necessitated some simplifications for 3-D printing, particularly in the temporal bone. Consequently, it lacked a tympanic membrane and soft structures represented by the ear, skin, and subcutaneous cellular tissue overlapping the temporal bone. Moreover, it did not simulate complications inherent to ear surgery. The facilitations above were minutely planned to avoid hampering the educational criteria and were irrelevant for using the model based on external raters.
Validity limitations included the non-anonymous selection of specialists, which may have resulted in evaluation bias, and the sample size (i.e., our evaluators were a small group of expert surgeons). Likewise, the validity evidence was restricted to the model's content as a training tool. It did not include the breadth of the evidence required for determining the value of the 3-D printed bone as a testing tool, with the ability to distinguish between the performance of experienced and inexperienced physicians. Our findings should be validated in educational environments, such as surgical training centers or medical schools. We intend to conduct a prospective and randomized study with otorhinolaryngology students to compare simulator-based with conventional training in the future, and also to compare the accuracy of the printed piece with the tomography of the model patient.
Conclusions
The 3-D printed temporal bone model is an efficient alternative to cadaver temporal bones as a surgical training tool in otology. This method is particularly useful for reproducing diseases, such as cholesteatoma. We developed a 3-D model that imitated the COMC. Our model demonstrated adequate face and content validity and provided an anatomically realistic dissection experience with educational value. Furthermore, the versatility of 3-D modeling enables future training applications, thus expanding the horizons for surgical skills training.
Availability of data and materials
My manuscript has no associated data.
Code availability
Not applicable.
References
Yoshiyasu Y, Chang DR, Bunegin L et al (2019) Construct validity of a low-cost medium-fidelity endoscopic sinus surgery simulation model. Laryngoscope 129(7):1505–1509
Deonarain AR, Harrison RV, Gordon KA et al (2021) Synthetic simulator for surgical training in tracheostomy and open airway surgery. Laryngoscope 131(7):E2378–E2386
de Souza MA, Bento RF, Lopes PT, de Pinto Rangel DM, Formighieri L (2021) Three-dimensional printing in otolaryngology education: a systematic review. Eur Arch Otorhinolaryngol 1–1
Lee M, Ang C, Andreadis K, Shin J, Rameau A (2021) An open-source three-dimensionally printed laryngeal model for injection laryngoplasty training. Laryngoscope 131(3):E890–E895
Lee AY, Fried MP, Gibber M (2017) Improving rhinology skills with simulation. Otolaryngol Clin N Am 50(5):893–901
Vaitaitis VJ, Dunham ME, Kwon YC et al (2020) A surgical simulator for tympanostomy tube insertion incorporating capacitive sensing technology to track instrument placement. Otolaryngol Head Neck Surg 162(3):343–345
Wong V, Unger B, Pisa J, Gousseau M, Westerberg B, Hochman JB (2019) Construct validation of a printed bone substitute in otologic education. Otol Neurotol 40(7):e698–e703
Gadaleta DJ, Huang D, Rankin N et al (2020) 3-D printed temporal bone as a tool for otologic surgery simulation. Am J Otolaryngol 41(3):102273
McMillan A, Kocharyan A, Dekker SE et al (2020) Comparison of materials used for 3-D-printing temporal bone models to simulate surgical dissection. Ann Otol Rhinol Laryngol 129(12):1168–1173
Gabrysz-Forget F, Rubin S, Nepomnayshy D, Dolan R, Yarlagadda B (2020) Development and validation of a novel surgical simulation for parotidectomy and facial nerve dissection. Otolaryngol Head Neck Surg 163(2):344–347
Chien WW, da Cruz MJ, Francis HW (2021) Validation of a 3-D-printed human temporal bone model for otology surgical skill training. World J Otorhinolaryngol Head Neck Surg 7(2):88–93
Seagull FJ, Rooney DM (2014) Filling a void: Developing a standard subjective assessment tool for surgical simulation through focused review of current practices. Surgery 156(3):718–722
Da Cruz MJ, Francis HW (2015) Face and content validation of a novel three-dimensional printed temporal bone for surgical skills development. J Laryngol Otol 129(suppl 3):S23–S29
Meyer C, Noda F, Folsom CR (2020) Hybrid surgical simulator: a temporal bone simulator validation study of the Stryker surgical simulator (S3). Mil Med 185(11–12):e2026–e2031
Chang DR, Lin RP, Bowe S et al (2017) Fabrication and validation of a low-cost, medium-fidelity silicone injection molded endoscopic sinus surgery simulation model. Laryngoscope 127(4):781–786
Alwani MM, Svenstrup TJ, Bandali EH et al (2020) Validity testing of a three-dimensionally printed endoscopic sinonasal surgery simulator. Laryngoscope 130(12):2748–2753
Gamer M, Lemon J, Fellows I, Singh P (2019) IRR: various coefficients of interrater reliability and agreement. R package version, 0.84.1
Rizopoulos D (2018 ) Latent trait models under IRT. R package version 1. 1–1
Canzi P, Capaccio P, Marconi S et al (2020) Feasibility of 3-D printed salivary duct models for sialendoscopic skills training: Preliminary report: preliminary report. Eur Arch Otorhinolaryngol 277(3):909–915
Nguyen Y, Mamelle E, De Seta D, Sterkers O, Bernardeschi D, Torres R (2017) Modifications to a 3-D-printed temporal bone model for augmented stapes fixation surgery teaching. Eur Arch Otorhinolaryngol 274(7):2733–2739
Bento RF, Rocha BA, Freitas EL, Balsalobre FA (2019) Otobone ®: three-dimensional printed temporal bone biomodel for simulation of surgical procedures. Int Arch Otorhinolaryngol 23(4):e451–e454
Vimawala S, Gao T, Goldfarb J et al (2020) Initial experience using 3-dimensional printed models for head and neck reconstruction in Haiti. Ear Nose Throat J 10:145561320938920
Acknowledgements
The authors thank the members of the Otorhinolaryngology Foundation for providing access to their 3D-printing facility and expert consultation, specially Dr Lucas Formighieri, radiologist.
Funding
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Author information
Authors and Affiliations
Contributions
RFB and MAdS conceived the idea for this article. MAdS collected relevant data and coordinated the creation of the model. PTL and RFB analyzed the data after discussions with MAdS. MAdS and PTL drafted the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethics approval
It was approved by the research ethics committee of the USP Hospital, under opinion 4.734.389.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Souza, M.A., Bento, R.F. & Lopes, P.T. A three-dimensionally printed otological model for cholesteatoma mastoidectomy training. Eur Arch Otorhinolaryngol 280, 671–680 (2023). https://doi.org/10.1007/s00405-022-07536-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07536-y