Abstract
Purpose
Despite the combination of chalkboard lectures and cadaveric models, the ear remains a complex anatomical structure that is difficult for medical students to grasp. The aim of this study was to evaluate the contribution of a 3D-printed ear model for educating undergraduate medical students by comparing it with a conventional cadaveric model.
Methods
Models of the ear comprising the outer ear, tympanic membrane, ossicles and inner ear were modeled and then 3D-printed at 6:1 and 10:1 scales based on cadaveric dissection and CT, cone-beam CT and micro/nano CT scans. Cadaveric models included two partially dissected dry temporal bones and ossicles. Twenty-four 3rd year medical students were given separate access to cadaveric models (n = 12) or 3D-printed models (n = 12). A pre-test and two post-tests were carried out to assess knowledge (n = 24). A satisfaction questionnaire focusing solely on the 3D-printed model, comprising 17 items assessed on a 5-point Likert scale, was completed by all study participants. A 5-point Likert scale questionnaire comprising four items (realism, color, quality and satisfaction with the 3D-printed ear model) was given to three expert anatomy Professors.
Results
The test scores on the first post-test were higher for the students who had used the 3D-printed models (p < 0.05). Overall satisfaction among the students and the experts was very high, averaging 4.7 on a 5-point Likert-type satisfaction scale.
Conclusion
This study highlights the overall pedagogical value of a 3D-printed model for learning ear anatomy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The ear is a complex anatomical structure, composed of three distinct anatomical parts: the outer, middle and inner ear. All medical students must learn the main anatomical elements of the ear during their studies, no matter their future orientation. In France, this knowledge is imparted by anatomy teachers during the first cycle of medical studies. At the Université de Franche-Comté, third-year medical students receive a one-hour lecture on a chalkboard, followed by non-mandatory tutorials delivered by anatomy laboratory assistants using cadaveric models.
Despite the combination of theoretical and practical classes, ear anatomy remains difficult to grasp. The theoretical course, based on 2D drawings, limits the spatial representation of the external acoustic meatus to the cochlea, which is an obstacle to learning about this anatomical region. During guided instruction, students are then faced with a problem of scale: the enlarged organ they have been shown is now its actual size. Despite extensive dissection, the inner ear remains contained within the temporal bone, which is a second obstacle to representation and learning. These long-acknowledged obstacles had prompted William Hunter, a pioneer in anatomy teaching in the eighteenth century, to dissect elegant specimens to reduce the complexity of spatial representation of this organ [29]. More recent studies have highlighted the value of new technologies in promoting this understanding [1, 2, 11, 12, 14,15,16, 20, 23, 25, 27, 34]. However, no study has looked at the pedagogical contribution of 3D printing in facilitating the spatial representation of the ear.
The aim of this study was to evaluate the contribution of a 3D-printed ear model for educating undergraduate medical students, by comparing it with a conventional cadaveric model.
Materials and methods
This was a prospective, controlled, randomized study.
Conventional cadaveric anatomical model
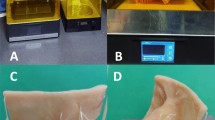
The conventional cadaveric model used consisted of dry temporal bones on metal supports. Half of the temporal bones were dissected to reveal the relief of the semicircular canals, and the other half were cut along the long axis of the bone, then a hinge system was added to provide open-book access to the contents of the tympanic cavity (Fig. 1).
Design of the 3D-printed anatomical model
The 3D-printed model was based on scan data from an 86-year-old male who had donated his body to the Department of Anatomy at the Université de Franche-Comté. The choice of a non-pathological, anatomically normal ear necessitated a conventional CT scan centered on the hemi-skulls of cadavers, constituting a bank of ten ears from which one was selected after careful analysis of the scans by a specialized radiologist. The first CT acquisitions were made of the complete right temporal bone with lateral soft tissues including the external ear within a hemi-skull sectioned in the horizontal plane above the temporal bone and at neck level, using a conventional SOMATOM Definition Edge scanner (Siemens Healthineers, Erlangen, Germany) and a cone-beam Artis Q biplane angiography system (Siemens Healthineers). The slice thickness was 0.4 mm and 0.19 mm, respectively. Subsequent acquisitions were made of a segment of the temporal bone centered on the tympanic cavity after its dissection, as close as possible to the anatomical boundaries of the ear. These acquisitions were carried out on an EasyTom S micro/nano CT system (RX Solutions, Chavanod, France) equipped with a Hamamatsu Open Type Microfocus L12161 X-ray source with a maximum voltage of 150 keV and 0.5 mA, and a 2530DX detector with 2176 × 1792 pixels. The tube voltage and the tube current used were 70 keV and 0.126 mA, respectively, for each tomography. The exposure time and the average frame rate are listed in Table 1. For all scans, 1440 projections were collected except for the tomography of the ear at 40 µm where a stack of three tomography scans were done to capture the full height of the piece. The entire volume was reconstructed using filtered back-projection; the resolution and the field of view are listed in Table 1.
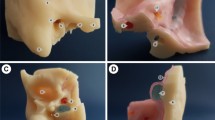
The data were processed using medical imaging software (Carestream Image Suite V4, New York, NY, USA). The segmentation was performed using Mimics Medical 24.0 software (Materialise, Leuven, Belgium) to separate the different anatomical parts using a thresholding method (Fig. 2). The outer ear, tympanic membrane, ossicles, cochlea and semi-circular canals were segmented. Then, the files were converted to STL and exported to 3-matic Medical 16.0 software (Materialise) for the design steps (smoothing, connectors, base). The total design time was about 12 h. The final files were exported to STL and sent to the 3D printers. The cochlea, ossicles and tympanic membrane were printed in Form 3 (Formlabs, Somerville, MA, USA) with White resin and Elastic 50A resin (Formlabs). Post-processing was needed to clean the resin and fully cure the models. The outer ear and the base were printed in Ultimaker S5 with PLA filament (Ultimaker, Utrecht, Netherlands). Three full models were printed at a 6:1 scale plus a base. Three other models consisting of only the ossicles and inner-ear were printed at a 10:1 scale plus the connectors needed to manipulate them. The total print time was about 8 days. Once printed, the inner ear elements of the models were spray-painted blue-grey (Fig. 3).
Student sample
Twenty-four third-year medical students were selected to participate in the study. These students had voluntarily enrolled in the Anatomy—Imaging—Morphogenesis Master 1 course run by the Department of Anatomy. At the beginning of the 2022–2023 academic year, like all students at that level (n = 250), the selected students (n = 24) received a one-hour chalkboard lecture on ear anatomy given by the head of the Department of Anatomy, followed by 30 min of directed teaching on cadaveric models given by assistants from the Department of Anatomy.
Study design
Each student was randomly assigned a number from 1 to 24. A pre-test and two identical post-tests—designated Test 1 and Test 2—were performed, each lasting 5 min. Following the pre-test, the students were assigned to two separate rooms one with the cadaveric model and the other with the 3D-printed model, depending on whether their number was odd or even. No communication was allowed between rooms. A supervisor was stationed in each room, who was instructed to tell the students in the cadaveric model room that they could not touch the human material provided, while the students in the other room were told the opposite. Students worked in subgroups of four around three identical stations in each room. Three A4 definition sheets of anatomical terms from Wolfgang Dauber’s Feneis Illustrated Anatomical Lexicon [10] were provided at each station. Students in each subgroup were allowed to communicate with each other. After 15 min in each room, the students took Test 1, with no communication allowed between the two study groups. Test 2 was administered 6 h later, the students could communicate with each other in the interim, but during the tests, no communication was allowed. All tests were anonymous and included only the number randomly assigned to each student before the pre-test (Fig. 4). These assessments were done on June 21, 2023.
Knowledge assessment
The pre-test consisted of 14 items to be scored as true or false on anatomical concepts from levels 1 and 2 of Bloom’s Anatomical Taxonomy [37] (Fig. 5). The test was scored out of 14 by a person who was not involved in the study’s procedures.
Evaluation of student satisfaction
A satisfaction questionnaire focusing solely on the 3D-printed model, comprising 17 items assessed on a 5-point Likert scale, was completed by all study participants. The questionnaire included a three-item evaluation of teaching methods, a five-item evaluation of personal satisfaction and a seven-item assessment of the effectiveness of 3D-printed models. One item assessed the students’ opinion of their university’s investment in 3D-printed models. Another item assessed their willingness to participate in the design of these models. The questionnaire ended with three open-ended questions. The first question asked students to choose three regions of the human body for which they would like to see a 3D model from among ten proposed regions, the second asked them to write down one or more regions or organs they would like to see 3D printed, and the final question left room for comments. Only the 12 students who had had access to the 3D-printed model as a learning tool filled out this questionnaire (Fig. 6). The 12 students who had not used the 3D-printed model were given access to it at the end of the study.
Evaluation of experts’ feelings and satisfaction
A 5-point Likert scale questionnaire comprising four items covering realism, color, quality and satisfaction with the 3D-printed ear model was given to three anatomy Professors, each with over 20 years of teaching experience (Fig. 7).
Data analysis
A Wilcoxon test was used to compare the two groups. A threshold value of p ≤ 0.05 was taken as significant.
Results
Knowledge assessment test results
The pre-test evaluation scores were lower in the “3D models” group, but not significantly (p = 0.11) (Fig. 8). Test 1 results were significantly better for the “3D models” group than for the “cadaveric models” t group (p = 0.035) (Fig. 9). This difference persisted in Test 2 but was no longer statistically significant (p = 0.052) (Fig. 10).
Evaluation of students' feelings and satisfaction
Overall satisfaction among students (n = 12) who used the 3D models was high, with an average of 4.7 out of 5 points (Fig. 11).
Their assessment of the perceived effectiveness of the 3D-printed models was equally so, with an average of 4.4 (Fig. 12).
Ten of the 12 students (83%) were very positive about their university’s investment in 3D-printed anatomical models. Seven of the 12 students (58%) were interested in participating in model design.
The brain was the most popular region for 3D printed models (75%, n = 9), followed by the facial mass and pelvis (58%, n = 7). The regions cited as the most desirable for 3D printed models were the heart, vertebrae, limbic lobe, talus, nerve plexuses, basal ganglia, brainstem and its cranial nerves, lesser pelvis, tarsus, carpus, skull base, orbital cavity and sphenoethmoidal recess.
Seven students (58%) made comments about the teaching methods used. Eight students (67%) were in favor of the self-learning method used. Five students (42%) would have preferred to have a teacher instead of the explanatory sheets provided, while four students (33%) would not. Four students (33%) were in favor of, and four students (33%) were against, being left alone with the 3D-printed model.
Assessment of experts’ feelings and satisfaction
Overall satisfaction among the experts (n = 3) was high, averaging 4.7 on a 5-point rating scale. All the experts were very positive about the realism of the model and were satisfied with it. Model quality was rated at 4 (Fig. 13).
Discussion
The results of our study demonstrate that a 3D-printed ear model provides a valuable pedagogical contribution on three levels. Assessment of the students’ knowledge showed a significant improvement in the group that used the 3D model, compared with the conventional anatomical model. Student satisfaction was rated as very high on a Likert scale. Experts rated the 3D model very favorably in terms of realism, color, quality and satisfaction.
Model creation
Model design was the most time-consuming part of the study. The resolution of conventional CT scans was insufficient (0.4 mm) for segmentation of the ossicles, particularly the stapes. Despite the much better resolution of cone-beam CT (0.19 mm) compared to conventional CT, the resolution was still insufficient for good-quality segmentation of the stapes. Spatial resolution by micro CT was conditioned by the size of the specimen. The cadaver’s right ear was therefore dissected until its anatomical boundaries were reached, enabling subsequent acquisitions to focus on the stapes. In their review of literature, Shelmerdine et al. mentioned using cadaver micro/nano-CT for teaching purposes in 2018 [32]. Mukherjee et al. used cone-beam and microCT with resolutions of 125 µm and 40 µm respectively to reconstruct and print human ossicles with good precision, taking the incus as a reference [22]. In our study, the stapes required the highest resolution for the modeling work. The 24 µm resolution obtained on the ossicular chain enabled us to see vascular entry points and to highlight the hollow hemi-cylindrical shape of the stapes branches. The contours of the plate were perfectly transcribed at 12 µm final resolution. To our knowledge, no other micro/nano CT study of human ossicles has been able to produce such high resolution. The resulting file provides a solid basis for future work on modeling and 3D printing elements of the human ossicular chain.
Soft colors were chosen for the model. The study conducted by Radzi et al. disapproved of the colors of their cardiac model, deeming them too bright [28]. Garas et al. contend that using colors makes it easier to recognize the different parts of their 3D-printed models [13]. Our study therefore employed colors for pedagogical purposes, to help students quickly identify the three parts of the ear. This facilitation was confirmed by the students, as the vast majority agreed that the colors had helped them recognize the parts of the ear. The colors chosen were consistent with the colors used in anatomy atlases (ossicles in white, inner ear in blue and outer part in flesh color). Post-painting is commonly used in the production of 3D-printed anatomical models [4, 7, 17, 18, 33, 36, 40]. Backhouse et al. had students perform this step, adding pedagogical value to teaching with the model [3].
Our model required the use of two printers to combine soft and hard plastics. Assembly was carried out at the end of the printing process. This technique requires a perfect match between the parts. PolyJet printers are ideal for these types of models, as they can print in several colors and several materials in a single block, combining speed and efficiency. However, the final cost is much higher with this type of printer. Mogali et al. printed a full-size heart for $310 and a complete model of the head and neck reduced to 95% scale for $160 using a PolyJet printer [21].
Choosing the scale was tricky, as the difference in size between the outer and inner ear made it impossible to print a complete model on a 10:1 scale. The platens of our printers were too small, and an outer ear had no educational value at such a scale, as it would restrict manipulations of the model and hinder observations. It therefore seemed necessary to print two models, reasonably increasing the scale on the model with the ossicles and inner ear. Pedagogical value was prioritized over realism. Most educational anatomical models are printed at 1:1 scale [6, 8, 19, 35]. Saleh et al. also opted for a larger scale—140% for their temporal bone model [31]. Bannon et al. reported excessive fragility of their 3D-printed 1:1 scale pterygopalatine fossa model, leading them to reprint it at a 2:1 scale [4]. Similarly, our model was fragile at the junction between the ossicles. For the 6:1 scale model, the ossicles were printed contiguous, modeling a small discoid junction element to maintain the correct position of the ossicles relative to each other, from the tympanic membrane to the vestibular window. For our 10:1 scale model, the ossicles were printed separately. Two fully detachable translucent soft-plastic studs were modeled to allow the malleus and stapes to be nested and un-nested, giving access to the joint cavity between the two. A transparent translucent soft plastic sleeve was modeled to allow assembly of the incus and stapes. This step required several trials to create a sleeve that was discreet yet strong enough to keep the ossicles attached.
Evaluation of expert satisfaction
Despite the change in scale of our 3D-printed model compared with the conventional cadaveric model, the experts' assessment was favorable, with all the experts rating its realism as 5/5. This is probably due to the pedagogical objective achieved by our model, which is focused on teaching normal anatomy to undergraduate medical students. The experts’ very positive assessment of our model testifies to the value of using a new technology to enhance existing models (bodies donated to science), models that can be modified and adapted to the teaching content that a teacher wishes to convey. This is a fundamental notion, as it also underlines the fact that creating 3D-printed anatomical models requires collaboration between anatomists and engineers. The commoditization of models is undesirable, as the added value of this technology in anatomy teaching might be lost.
Student assessment
The student assessment was based on level one and two questions according to Bloom’s Anatomical Taxonomy [37]. Level one tested pure knowledge and level two tested comprehension. Anatomical comprehension is assessed through the students' ability to find information from the spatial representation of an anatomical region. Applications (level three) and analytical ability (level four) are learning levels applicable to 3D-printed training models such as that of Nguyen et al., who tested a 3D-printed temporal bone model for piston prosthesis placement on the stapes [24]. The better Test 1 results obtained by students who used the 3D-printed ear model can probably be explained by the optimized 3D representation of ear anatomy. Although the questions in Test 1 and Test 2 were identical to those on the pre-test, the students had not been informed of this beforehand. The time allotted to answer the assessment questions was considered sufficient by all students.
The results of the second test are probably biased for two reasons: the first being the possibility for students to communicate with each other in the interval between the first and second tests (with identical tests) and the second being the absence of sufficient spacing to properly assess the effects of the different models on long-term knowledge retention. This choice of a second post-test only few hours later is explained by our fear of being confronted with a large number of lost to follow-up if we had summoned the students several weeks later (which would have corresponded to the following academic year). During this interval, the students took an anatomy exam that did not concern the ear and was supposed to lead to a washout effect.
Our work is part of a larger project to test on an entire class of students (n = 250) a more complex model (currently being designed and requiring over a hundred hours of modeling by engineers and anatomists). Under these conditions, a second test several weeks after the first would seem desirable. Our test questions focused on knowledge of the bony elements of the middle ear and the organization of the inner ear, comparing two models that did not include nerve or vascular structures. The evaluation of a more complex model incorporating this type of anatomical structures will provide a more comprehensive test of knowledge, in line with the objectives of learning about ear anatomy during the first cycle of medical studies. It is likely that results will be better in the group with the more complex 3D-printed model, since this latter allows visualization of structures that the cadaveric model does not. Several recent meta-analyses have demonstrated the effectiveness of 3D-printed models in teaching anatomy [30, 38, 39]. However, certain criteria need to be met to conclude that they are effective, notably the use of 3D-printed anatomical models representing anatomical structures deemed to be complex, and their use with students with little knowledge (the effects of these models are often negligible with residents) [9]. To our knowledge, no study has yet been carried out to assess the effectiveness of 3D-printed anatomical models of the ear. The results of our pilot study, based on the experience of numerous authors in the creation and evaluation of 3D-printed anatomical models, thus justify evaluating with a more complex 3D-printed ear model for an entire class of students [5].
Evaluation of student satisfaction
There was no doubt about the student’s satisfaction with the 3D-printed model and their feelings about its effectiveness, but their opinions on the teaching methods were mixed. This new technology might motivate some students to learn and reinforce existing teaching methods to help them succeed. Unsurprisingly, opinions on future practice were divided. A model representing normal ear anatomy on a modified scale is unsuitable for training. To meet this objective, 3D-printed models for training in endoscopy [34], milling [12, 16] or prosthesis fitting [24] have already been described in the literature. They are aimed at students who are more advanced in their studies, most of whom are ENT residents. All the students in our study supported their university’s investment in 3D-printed models. The acquisition of a 3D printing platform could be beneficial. This is all the more important as the majority of students would have participated in designing the model. The most desired region for a 3D model was the head and neck area. The fineness and entanglement of the anatomical structures that make up the ear easily explain this choice. Thus, 3D-printed models appear to be an appropriate tool insofar as modeling can simplify, embellish, increase the size or intensify the colors of the true anatomical structure.
Limit
The sample size was small in our study due to the low number of places in the Anatomy-Imaging-Morphogenesis Master’s program at our university. However, all the subjects participated from start to finish, enabling us to collect data on knowledge and satisfaction. Our results can be used as pilot data for future studies. We did not carry out a cross-over study because all the students had already participated in a guided teaching session on the cadaveric model at the beginning of the academic year. This meant that only 12 students were able to evaluate the 3D-printed model, even though they had already benefited from conventional teaching on the cadaveric model.
Our model contained minimal information. The walls of the cavity were not represented, nor were the vascular and nerve elements. This is a perfectible aspect of our model, given that the experts' rated its quality as 4/5. No long-term evaluation was carried out to assess how our 3D-printed ear model affected knowledge retention. O’Brien et al. demonstrated this benefit with their 3D-printed model of the tracheobronchial tree [26]. It is likely that this effect is attributable to 3D printing and reproducible with other models.
To conclude, this study found a significant benefit of using a 3D-printed ear model to teach anatomy to third-year medical students, in addition to traditional teaching methods. This benefit was seen in both knowledge assessment and student satisfaction. Our 3D-printed model of the ear was viewed favorably by anatomy professors with over 20 years’ teaching experience. Our results suggest that a more complex anatomical model of the ear may be highly effective for 3rd-year medical students and may justify medical universities investing in 3D-printed anatomical models for educational purposes, particularly ones created by anatomists in collaboration with engineers specialized in modeling the human body Table 2.
Data availability
Not applicable.
References
Abou-Elhamd KEA, Al-Sultan AI, Rashad UM (2010) Simulation in ENT medical education. J Laryngol Otol 124(3):237–241. https://doi.org/10.1017/S0022215109991885
Anschuetz L, Huwendiek S, Stricker D, Yacoub A, Wimmer W, Caversaccio M (2019) Assessment of middle ear anatomy teaching Methodologies using microscopy versus endoscopy: a randomized comparative study. Anat Sci Educ 12(5):507–517. https://doi.org/10.1002/ase.1837
Backhouse S, Taylor D, Armitage JA (2019) Is this mine to keep? Three-dimensional printing enables active, personalized learning in anatomy. Anat Sci Educ 12(5):518–528. https://doi.org/10.1002/ase.1840
Bannon R, Parihar S, Skarparis Y, Varsou O, Cezayirli E (2018) 3D printing the pterygopalatine fossa: a negative space model of a complex structure. Surg Radiol Anat 40(2):185–191. https://doi.org/10.1007/s00276-017-1916-x
Brumpt E, Bertin E, Tatu L, Louvrier A (2023) 3D printing as a pedagogical tool for teaching normal human anatomy: a systematic review. BMC Med Educ 23(1):783. https://doi.org/10.1186/s12909-023-04744-w
Chae R, Sharon JD, Kournoutas I et al (2020) Replicating skull base anatomy with 3D technologies: a comparative study using 3D-scanned and 3D-printed models of the temporal bone. Otol Neurotol 41(3):e392–e403. https://doi.org/10.1097/MAO.0000000000002524
Chen S, Pan Z, Wu Y et al (2017) The role of three-dimensional printed models of skull in anatomy education: a randomized controlled trail. Sci Rep 7(1):575. https://doi.org/10.1038/s41598-017-00647-1
Chen Y, Qian C, Shen R et al (2020) 3D printing technology improves medical interns’ understanding of anatomy of gastrocolic trunk. J Surg Educ 77(5):1279–1284. https://doi.org/10.1016/j.jsurg.2020.02.031
Chytas D, Salmas M, Demesticha T, Troupis T (2023) Three-dimensional printing in anatomy education: is it similarly useful for teaching of all anatomical regions and structures? Anat Sci Educ 16(1):5–6. https://doi.org/10.1002/ase.2216
Dauber W (2007) Lexique illustré d’anatomie FENEIS. Médecine- Sciences Flammarion, Paris
Fieux M, Zaouche S, Philouze P, Truy E, Hermann R, Tringali S (2021) Low-fidelity otoscopy simulation and anatomy training: a randomized controlled trial. Eur Ann Otorhinolaryngol Head Neck Dis 138(4):231–234. https://doi.org/10.1016/j.anorl.2020.09.010
Frithioff A, Frendø M, Weiss K et al (2023) 3-D-printed models for temporal bone training: a validity study. Otol Neurotol 44(7):e497–e503. https://doi.org/10.1097/MAO.0000000000003936
Garas M, Vaccarezza M, Newland G, McVay-Doornbusch K, Hasani J (2018) 3D-printed specimens as a valuable tool in anatomy education: a pilot study. Ann Anat Anat Anz 219:57–64. https://doi.org/10.1016/j.aanat.2018.05.006
Gnanasegaram JJ, Leung R, Beyea JA (2020) Evaluating the effectiveness of learning ear anatomy using holographic models. J Otolaryngol Head Neck Surg 49(1):63. https://doi.org/10.1186/s40463-020-00458-x
Guy J, Muzaffar J, Coulson C (2021) Teaching middle ear anatomy using a novel three-dimensional papercraft model. Eur Arch Oto-Rhino-Laryngol 278(8):2769–2774. https://doi.org/10.1007/s00405-020-06350-8
Hochman JB, Rhodes C, Wong D, Kraut J, Pisa J, Unger B (2015) Comparison of cadaveric and isomorphic three-dimensional printed models in temporal bone education. Laryngoscope 125(10):2353–2357. https://doi.org/10.1002/lary.24919
Javan R, Herrin D, Tangestanipoor A (2016) Understanding spatially complex segmental and branch anatomy using 3D printing. Acad Radiol 23(9):1183–1189. https://doi.org/10.1016/j.acra.2016.04.010
Javan R, Rao A, Jeun BS, Herur-Raman A, Singh N, Heidari P (2020) From ct to 3D printed models, serious gaming, and virtual reality: framework for educational 3D visualization of complex anatomical spaces from within—the pterygopalatine fossa. J Digit Imaging 33(3):776–791. https://doi.org/10.1007/s10278-019-00315-y
Krishnasamy S, Mokhtar RAR, Singh R, Sivallingam S, Aziz YFA, Mathaneswaran V (2021) 3D rapid prototyping heart model validation for teaching and training—a pilot project in a teaching institution. Braz J Cardiovasc Surg. https://doi.org/10.21470/1678-9741-2020-0433
Lee DJ, Fu TS, Carrillo B, Campisi P, Forte V, Chiodo A (2015) Evaluation of an otoscopy simulator to teach otoscopy and normative anatomy to first year medical students: simulation-based otoscopy training. Laryngoscope 125(9):2159–2162. https://doi.org/10.1002/lary.25135
Mogali SR, Chandrasekaran R, Radzi S et al (2022) investigating the effectiveness of three-dimensionally printed anatomical models compared with plastinated human specimens in learning cardiac and neck anatomy: a randomized crossover study. Anat Sci Educ 15(6):1007–1017. https://doi.org/10.1002/ase.2128
Mukherjee P, Cheng K, Chung J, Grieve SM, Solomon M, Wallace G (2021) Precision medicine in ossiculoplasty. Otol Neurotol 42(2):e177–e185. https://doi.org/10.1097/MAO.0000000000002928
Ng CL, Liu X, Chee SCJ, Ngo RYS (2015) An Innovative 3-dimensional model of the epitympanum for teaching of middle ear anatomy. Otolaryngol Neck Surg 153(5):832–837. https://doi.org/10.1177/0194599815584600
Nguyen Y, Mamelle E, De Seta D, Sterkers O, Bernardeschi D, Torres R (2017) modifications to a 3D-printed temporal bone model for augmented stapes fixation surgery teaching. Eur Arch Otorhinolaryngol 274(7):2733–2739. https://doi.org/10.1007/s00405-017-4572-1
Nicholson DT, Chalk C, Funnell WRJ, Daniel SJ (2006) Can virtual reality improve anatomy education? A randomised controlled study of a computer-generated three-dimensional anatomical ear model. Med Educ 40(11):1081–1087. https://doi.org/10.1111/j.1365-2929.2006.02611.x
O’Brien C, Souza CA, Sheikh A, Miguel O, Wood T (2021) Use of tracheobronchial tree 3-dimensional printed model: does it improve trainees’ understanding of segmentation anatomy? A prospective study. Print Med 7(1):2. https://doi.org/10.1186/s41205-020-00092-3
Park HS, Chung MS, Shin DS, Jung YW, Park JS (2013) Accessible and informative sectioned images, color-coded images, and surface models of the ear: accessible and informative images of ear. Anat Rec 296(8):1180–1186. https://doi.org/10.1002/ar.22719
Radzi S, Tan HKJ, Tan GJS et al (2020) Development of a three-dimensional printed heart from computed tomography images of a plastinated specimen for learning anatomy. Anat Cell Biol 53(1):48–57. https://doi.org/10.5115/acb.19.153
Roth H, Smith RA, Mackay S (2013) Modern day relevance of William Hunter’s approach to teaching “The organ of hearing”: William Hunter and the organ of hearing. Clin Anat 26(5):551–555. https://doi.org/10.1002/ca.22220
Salazar D, Thompson M, Rosen A, Zuniga J (2022) Using 3D printing to improve student education of complex anatomy: a systematic review and meta-analysis. Med Sci Educ 32(5):1209–1218. https://doi.org/10.1007/s40670-022-01595-w
Saleh Y, Piper R, Richard M, Jeyaretna S, Cosker T (2022) Designing a 3D Printed model of the skull-base: a collaboration between clinicians and industry. J Med Educ Curric Dev 9:238212052210807. https://doi.org/10.1177/23821205221080703
Shelmerdine SC, Simcock IC, Hutchinson JC et al (2018) 3D printing from microfocus computed tomography (micro-CT) in human specimens: education and future implications. Br J Radiol. https://doi.org/10.1259/bjr.20180306
Shen Z, Yao Y, Xie Y et al (2019) The process of 3D printed skull models for anatomy education. Comput Assist Surg 24(sup1):121–130. https://doi.org/10.1080/24699322.2018.1560101
Stramiello JA, Wong SJ, Good R, Tor A, Ryan J, Carvalho D (2022) Validation of a three-dimensional printed pediatric middle ear model for endoscopic surgery training. Laryngoscope Investig Otolaryngol 7(6):2133–2138. https://doi.org/10.1002/lio2.945
Tan L, Wang Z, Jiang H et al (2022) Full color 3D printing of anatomical models. Clin Anat 35(5):598–608. https://doi.org/10.1002/ca.23875
Tanner JA, Jethwa B, Jackson J et al (2020) A three-dimensional print model of the pterygopalatine fossa significantly enhances the learning experience. Anat Sci Educ 13(5):568–580. https://doi.org/10.1002/ase.1942
Thompson AR, O’Loughlin VD (2015) The blooming anatomy tool (BAT): a discipline-specific rubric for utilizing bloom’s taxonomy in the design and evaluation of assessments in the anatomical sciences: blooming anatomy tool for evaluating MCQs. Anat Sci Educ 8(6):493–501. https://doi.org/10.1002/ase.1507
Ye Z, Dun A, Jiang H et al (2020) The role of 3D printed models in the teaching of human anatomy: a systematic review and meta-analysis. BMC Med Educ 20(1):335. https://doi.org/10.1186/s12909-020-02242-x
Ye Z, Jiang H, Bai S et al (2023) Meta-analyzing the efficacy of 3D printed models in anatomy education. Front bioeng biotechnol 11:1117555. https://doi.org/10.3389/fbioe.2023.1117555
Zhang X, Xu Z, Tan L et al (2019) Application of three-dimensional reconstruction and printing as an elective course for undergraduate medical students: an exploratory trial. Surg Radiol Anat 41(10):1193–1204. https://doi.org/10.1007/s00276-019-02248-1
Acknowledgements
The authors sincerely thank those who donated their bodies to science so that anatomical research could be performed. Results from such research can potentially increase mankind's overall knowledge that can then improve patient care. Therefore, these donors and their families deserve our highest gratitude.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by EB, AL, XG, CC and EB. The first draft of the manuscript was written by EB and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
No ethical clearance was required as cadavers are used for research purpose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Brumpt, E., Bertin, E., Gabrion, X. et al. Are 3D-printed anatomical models of the ear effective for teaching anatomy? A comparative pilot study versus cadaveric models. Surg Radiol Anat 46, 103–115 (2024). https://doi.org/10.1007/s00276-023-03276-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-023-03276-8