Abstract
Purpose
We aimed to evaluate the power of 18F-fluorocholine (FCH) positron emission tomography/magnetic resonance (PET/MR) imaging in unlocalized primary hyperparathyroidism.
Methods
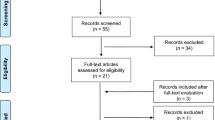
Thirty-four patients were included. In 17/34 patients, PET/MR was performed immediately after a negative 18F-FCH PET/CT. Sensitivity, specificity, positive and negative predictive values were calculated for MR only (blinded to PET data) and PET only (blinded to MR data) findings.
Results
18F-FCH PET/MR was positive in 26/34 (76%) patients. PET/MR was also positive in 12/17 (71%) patients with a negative PET/CT. Among 11/34 (32%) patients where 18F-FCH PET-only and MR-only results were discordant, MR was false positive in 7/11 patients (3/7 of the lesions were not 18F-FCH avid and in 4/7 of them PET and MRI pointed different locations. Postoperative histopathology revealed that 18F-FCH-positive ones were true positives). Sensitivity, specificity, PPV, NPV and accuracy of neck MR evaluated blinded to PET data were 80%, 50%, 70%, 64% and 68%, respectively, and all were calculated as 100% for PET/MR.
Conclusion
18F-FCH PET/MR is very effective in preoperative localization of parathyroid adenomas even if 18F-FCH PET/CT is negative. Neck MR alone is insufficient in detecting parathyroid adenomas but PET/MR combination helps in precise localisation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Primary hyperparathyroidism is a common endocrine disorder in routine clinical practice. Single adenoma is the most common cause of primary hyperparathyroidism and minimally invasive parathyroid surgery is now the preferred therapeutic method [1]. Accurate preoperative localization of the hyper functioning parathyroid gland is essential for a successful selective regional approach in surgery. Neck ultrasonography (USG) performed in experienced hands and Tc-99 m MIBI dual-phase parathyroid SPECT and SPECT/CT provide efficient preoperative anatomical localization in a great majority of patients with a given high positive predictive value [2]. These relatively simple, cheap and widely available conventional methods may be inconclusive in some patients. 18F-choline PET/CT has emerged as an alternative functional imaging method in primary hyperparathyroidism with inconclusive USG and scintigraphy. There exists an accumulated data on the efficacy of this new tracer in this era. In a recent study, reported sensitivity, positive predictive value (PPV) and overall diagnostic rate (DR) for 18F-FCH PET/CT in primary hyperparathyroidism was 95%, %97 and %91, respectively [3].
Being the preferred imaging method for local staging of head and neck tumors, neck MRI was also proposed as an alternative for parathyroid imaging. MRI provides anatomical information very close to real anatomy confronted during surgery. The exact number and localization of the parathyroid lesions can be seen by MRI. Negligible radiation exposure compared to CT or scintigraphy and easier discrimination of adenomas from thyroid nodules are the other advantages reported for neck MRI. However, the reported sensitivity of 1.5 T neck MR in parathyroid localization ranges between 40 and 80% [4]. Special imaging protocols have also been defined for 3 T imaging so that detection of a parathyroid adenoma with a typical elongated morphology and T2-hyperintensity could be possible, but efficacy of 3 T MRI and superiority over other imaging methods in parathyroid imaging is still uncertain [5].
PET/MR technology provides better anatomical data from PET/CT due to the obvious superiority of MRI in soft tissue imaging [6]. Quality of PET images obtained by PET/MRI is also argued to be better than PET/CT [7]. Thus, 18F-choline PET/MR is hypothetically predicted to be very effective as it combines the best anatomical and the most sensitive functional imaging data with a more favorable radiation dosimetry. However, there is no efficient data about its specific role in parathyroid imaging. In this study, we aimed to evaluate the power of 18F-FCH PET/MR imaging in localization of hyperfunctioning parathyroid gland in primary hyperparathyroidism.
Methods
Patients
Data of the patients (age > 18) who were referred to Ankara University Medical Faculty Nuclear Medicine Department for 18F-FCH PET imaging between October 2018 and March 2019 with clinically and/or biochemically diagnosed primary hyperparathyroidism were reviewed retrospectively. According to local regulations, no institutional ethics committee approval is needed for retrospectively designed studies. All patients included had previously performed inconclusive neck USG and Tc-99 m MIBI SPECT examinations. Contraindications for a PET/MR study were (i) claustrophobia, (ii) implanted non-MR safe devices, cerebral aneurysm clips or cochlear implants, (iii) inability to cooperate with breath-hold instructions, (iv) overweight, and (v) existence of serious other cardiac-respiratory diseases with high risk of decompensation.
Criteria for exclusion from the study were (i) secondary or tertiary hyperparathyroidism, (ii) existence of chronic renal disease, and (iii) evidence of any other malignancy including thyroid and parathyroid carcinoma. History of previous thyroid/parathyroid surgery, osteoporosis or nephrolithiasis, recent serum PTH, Ca, P levels, urinary Ca excretion/24 h, neck ultrasonography and Tc-99 m MIBI parathyroid SPECT/CT findings, clinical follow-up results as well as results of histopathological examinations in cases who underwent parathyroidectomy were recorded.
18F-FCH PET/MR protocol
PET/MR images of the neck and thorax were acquired with a combined PET/MR scanner (Signa PET/MR, 3.0 T, General Electric Company, USA) 45–60 min after intravenous injection of approximately 100 MBq 18F-FCH in supine position. Simultaneous PET and MR images of neck and thorax were acquired for a total of 20 min (Fig. 1). MR imaging protocol parameters were as follows: coronal T2 turbo spin echo (TSE): FOV: 26 cm, slice thickness/gap: 4 mm/1 mm, TR: 3000, TE: 85, flip angle (FA): 140, NEX: 2; coronal T1 fast spin echo (FSE): FOV: 26 cm, slice thickness/gap: 4 mm/1 mm, TR: 680, TE: min full, FA: 110, NEX: 2; axial T2 FSE: FOV: 26 cm, slice thickness/gap: 5 mm/1 mm, TR: 3100, TE: 85, FA: 140, NEX: 2; axial T1 FSE: FOV: 26 cm, slice thickness/gap: 5 mm/1 mm, TR: 469, TE: min full, FA: 110, NEX: 2 PET images were reconstructed with MR images on Advance Workstation Volume share 5 (GE Medical Systems).
Image and data interpretation
All PET/MR images were separately reevaluated by a nuclear medicine specialist and a radiologist retrospectively. A focal uptake higher than adjacent background activity located in the neck or mediastinum with a corresponding nodular lesion on MR was accepted as positive for parathyroid adenoma on PET images. A nodular lesion was defined to be suspicious for a parathyroid adenoma on MRI in case the lesion showed intermediate-low signal intensity on T1 images but high signal intensity on STIR images and had elongated appearance. MR images alone were reevaluated to seek for a parathyroid lesion, blinded to the PET data and compatibility of the results of PET alone and MR alone studies were investigated.
Statistical analysis
The descriptive statistics of the variables were performed (mean, median and 25–75% range). Results of 18F-FCH PET/MR results were confirmed by clinical follow-up and/or histopathological examination results. Compatibility of PET/MR and MR studies were statistically analyzed using Pearson’s Chi-square test. Per patient sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy were calculated for 18F-FCH PET/MR and MR alone without PET data. Values of p less than 0.05 were significant. Statistical analysis was performed using the Statistical Package for Social Sciences—SPSS 17.0 (Chicago, Illinois, USA).
Results
A total of 34 patients (12 M, 23F, mean age: 49.5 ± 13.5 min: 18 max: 70) who met the inclusion criteria were enrolled in the study. Among these patients, 17 patients who were eligible to MRI study had directly undergone PET/MRI. In 17 patients; however, a PET/MR study was performed following 18F-FCH PET/CT, due to inconclusive PET/CT results.
In 26/34 (76%) patients, 18F-FCH PET/MR was positive for a parathyroid adenoma. Confirmation was made by histopathology in 18/26 (69%) patients and by parathormone washout in 2/26 (8%) patients. Surgery was not performed due to unavailability of patient’s consent or non-complicated disease in 6/26 (23%) patients but were accepted as true positives by clinical follow-up. In 8/34 (24%) patients, 18F-FCH PET/MR was normal. They were accepted as true negatives and none of them underwent surgery. Thus, overall sensitivity, specificity, PPV, NPV and accuracy of 18F-FCH PET/MR was 100%.
Separate head-to-head comparison results were as follows: In 23/34 (68%) of the patients, 18F-FCH PET only (blinded to MR data) results were compatible with MR only (blinded to PET data) evaluation results (K = 0.31 p < 0.05). In this concordant group, 7/23 (30%) patients were clinically accepted true negatives and 16/23 (70%) true positives. Confirmation was done by histopathology in 12/16 (75%) patients, by parathormone washout in 1/16 (6%) patients and by clinical follow-up results in 3/16 (19%) patients.
In 11/34 (32%) patients, 18F-FCH PET only and MR alone were discordant. MR was false positive in 7/11 patients. Among these, 3/11 of the lesions were not 18F-FCH avid and patients were not directed to surgery, in 4/11 of them choline avid lesion and the lesion suggestive of an adenoma on MRI were completely two different lesions. Postoperative histopathology revealed that the choline-positive ones were adenomas and MRI was misdirecting, the surgically removed choline avid lesion was not suggestive of an adenoma on MRI (false negative for MR study). Sensitivity, specificity, PPV, NPV and accuracy of neck MR study evaluated blinded to PET data were calculated as 80%, 50%, 70%, 64% and 68%, respectively. Together with descriptive characteristics, detailed results of separate evaluation findings are given in Table 1.
In 17/34 (50%) patients, PET/MR was performed immediately after PET/CT study, due to inconclusive or negative PET/CT results. In 12/17 (71%) patients, PET/MR was positive for a parathyroid adenoma (confirmed histopathologically in 7/12 (58%), with washout in 2/12 (17%) and clinically in 3/12 (25%) patients (Fig. 2). In 5/17 of them, PET/MR was also negative (true negatives).
18F-FCH PET/CT and PET/MR images of a 54-year-old male (Patient no.: 11). Blood biochemical tests were as follows: serum PTH: 90.9 ng/L, Ca:11.0 mg/dL, P:2.2 mg/dL. The patient had no coexisting thyroid disease. No pathological uptake suggestive of a parathyroid adenoma was detectable by PET/CT but and intense focal pathological uptake (SUVmax:6.1) was detected corresponding to 6X4mm nodular lesion visualized isointense on T1-weighed images and hyperintense on T2-weighed images and located in the posterior neighborhood of the inferior pole of the left lobe of the thyroid gland
Discussion
18F-choline has recently gained popularity in parathyroid imaging by many studies published one after another, showing its superiority over Tc-99 m MIBI and by PET/CT cameras became available now worldwide. Some authors have argued that 18F-choline is ready to replace Tc-99 m MIBI, with high accuracy in localization of hyper functioning parathyroid tissue [8,9,10]. MRI is frequently used in head and neck tumors but its use in parathyroid tumors is still unclear [11]. The leading anatomical imaging modality for parathyroid is USG because it is a safe and a simple method to scan the neck at a lower cost. However, in challenging cases where scintigraphy and USG combination is insufficient, together with other tracers for functional imaging, further radiological protocols have also been suggested to be effective in unlocalized disease. The detectability of parathyroid glands has been reported to be increased by new developments in MR technology. Additionally, negligible radiation exposure is a very important advantage of MR over 4D CT, scintigraphy and PET/CT [12, 13]. Now that PET/MR is also available in selected centers, investigations have changed direction to prove the hypothesis that PET/MR with 18F-choline is probably the most accurate method for parathyroid imaging, due to the reasons previously mentioned. In this study, we also aimed to investigate overall accuracy of 18F-choline PET/MR in primary hyperparathyroidism. The accuracy of 18F-choline PET alone and MR alone were also compared and a head-to-head comparison of PET/CT and PET/MR in the same subjects was also partially possible.
The results proved that 18F-choline PET/MR has a very high accuracy rate in localization of parathyroid adenomas, as expected. However, there exists an important limitation of the study in this context, as histopathological confirmation or PTH washout was not possible for all cases, although imaging findings were strongly suggestive of a parathyroid adenoma for cases rated as true positives and laboratory findings were not typical for primary hyperparathyroidism for cases clinically rated as true negatives. Neck exploration for preoperatively unlocalized disease was not preferred for uncomplicated disease.
3 T MRI provides a higher magnetic power than 1.5 T machines and thus a much effective and homogenous fat suppression. Parathyroid lesions, which are very poor in fat content, were demonstrated to be visible on 3 T MR, even in subcentimetric dimensions and neck MR with 3 T was reported to be effectively used as a second step in parathyroid imaging. Hyperintensity on T2-weighted images and elongated morphology were defined as common features of a parathyroid adenoma on MR [5]. However, the authors underlined that both two characteristics were not specific enough to define a parathyroid adenoma, as other pathologies of the same anatomic region like exophytic thyroid nodules or lymph nodes may also appear the same [14,15,16]. Our findings support these previous data, as we calculated a sensitivity of 80% and a specificity of 50% for MR only evaluation of the neck, while the accuracy was 100% when PET and MR data were combined. Compared to evaluation according to 18F-choline avidity, these parameters fail to distinguish some parathyroid adenomas from other pathologies regarding to the false-positive lesions on MR. Thus, MR imaging was mainly helpful in precise anatomic localization rather than identifying the hyperfunctioning parathyroid.
Contrast-enhanced imaging protocols on MR were also developed for parathyroid imaging. Faster and higher enhancement was suggested to be helpful in defining a parathyroid adenoma [4, 17,18,19]. Intravenous contrast was not administered in this study protocol. One may advocate that it would be helpful in distinguishing parathyroid lesions from other pathologies if contrast was injected and that MR would reach a higher success rate, close to 18F-choline-only interpretation. However, it has been reported that lesions with typical contrast enhancement suggestive of a parathyroid adenoma were already recognized on precontrast T2-weighted images and contrast usage can be spared only for crosscheck in borderline cases [5]. Thus, imaging protocol used in this study seems to be reliable enough for a head-to-head comparison of detection abilities of blinded MR only and blinded 18F-choline PET only images. 18F-choline is more sensitive than neck MR alone in detecting parathyroid adenomas. However, neck MR is highly informative in defining soft tissue lesions corresponding to the focal 18F-choline uptake site and precise localization of parathyroid lesions by demonstrating adjacent anatomical structures in the neck.
To the best of our knowledge, this study presents the first data on head-to-head comparison of 18F-choline PET/MR and PET/CT in the same patients. It is obvious that PET/MR outperforms PET/CT in parathyroid imaging by 18F-choline. In this study, PET/MR was positive for a parathyroid adenoma in 12/17 (71%) patients with a negative PET/CT. One reason for higher detectability of PET/MR over PET/CT is the improved PET instrumentation adopted in hybrid PET/MR devices. Higher sensitivity provided by digital PET technology, more successful registration and superior motion correction abilities, all contribute to much better image quality [20].
Another thing is that PET/MR was performed immediately after PET/CT in this study. This sooner acquisition of the second PET study may have led to higher target to background ratio and thus better delineation of parathyroid lesions. Similar dual time point imaging techniques have been proven to be useful in some other tumors, although it is not yet defined for parathyroid imaging with 18F-choline [21]. Unlike the settled PET/CT protocol, where CT and PET scans were performed one after another, PET and MR acquisitions were performed simultaneously on PET/MR. This provided a longer PET acquisition time with PET/MR and higher count statistics compared to PET/CT which probably also has increased the detectability rate.
It was reported that absorbed radiation doses for 18F-choline PET/CT were much less than Tc-99 m MIBI SPECT/CT [22]. Hybrid PET/MR imaging instead of PET/CT of course provides even better dosimetric results compared to standard scintigraphic method in hyperparathyroidism. This is another important advantage of PET/MR over PET/CT and SPECT/CT.
Despite several advantages of PET/MR over PET/CT, it also has some disadvantages. First of all, MR imaging is relatively troublesome for the patients. Longer acquisition time of MR imaging usually interrupts patient comfort, especially in claustrophobic patients. Second, the higher cost and much less availability of PET/MR devices around the world is probably the most important and limiting disadvantage to mention.
This study presents the novel data on the head-to-head comparison of detectability power of 18F-choline only and MR only studies as well as 18F-choline PET/CT and PET/MR in the same patients for preoperative localization in primary hyperparathyroidism, despite some limitations. The patient group is relatively small for other primary hyperparathyroidism series published, but still seems to be a good representative of the interested population, as unlocalized primary hyperparathyroidism cases referred to choline PET/MR are relatively rare and that not all patients could undergo surgery due to previously mentioned reasons. Some true-positive and true-negative cases were regarded so according to clinical follow-up.
Conclusion
18F-FCH PET/MR has an excellent performance for preoperative localization of parathyroid adenomas where neck USG and Tc-99 m MIBI scintigraphy are negative. Neck MR alone may not be efficient enough in the preoperative assessment of primary hyperparathyroidism, but combined 18F-FCH PET/MR data is much superior in identification of parathyroid adenoma. 18F-FCH PET/MR may be also be considered as an effective second step in patients whom 18F-FCH PET/CT has failed.
References
Ruda JM, Hollenbeak CS, Stack BCA Jr (2005) systematic review of the diagnosis and treatment of primary hyperparathyroidism from 1995 to 2003. Otolaryngol Head Neck Surg 132:359
Eslamy HK, Ziessman HA (2008) Parathyroid scintigraphy in patients with primary hyperparathyroidism: 99mTc sestamibi SPECT and SPECT/CT. Radiographics 28:1461
Treglia G, Piccardo A, Imperiale A, Strobel K, Kaufmann PA, Prior JO, Giovanella L (2019) Diagnostic performance of choline PET for detection of hyper functioning parathyroid glands in hyperparathyroidism: a systematic review and meta-analysis. Eur J Nucl Med Mol Imaging 46:751–765
Kabala JE (2008) Computed tomography and magnetic resonance imaging in diseases of the thyroid and parathyroid. Eur J Radiol 66:480–492
Sacconi B, Argirò R, Diacinti D, Iannarelli A, Bezzi M, Cipriani C, Pisani D, Cipolla V, De Felice C, Minisola S, Catalano C (2016) MR appearance of parathyroid adenomas at 3 T in patients with primary hyperparathyroidism: what radiologists need to know for pre-operative localization. Eur Radiol 26(3):664–673
Drzezga A, Souvatzoglou M, Eiber M, Beer AJ, Fürst S, Martinez-Möller A, Nekolla SG, Ziegler S, Ganter C, Rummeny EJ, Schwaiger M (2012) First clinical experience with integrated whole-body PET/MR: comparison to PET/CT in patients with oncologic diagnoses. J Nucl Med 53(6):845–855
Balyasnikova S, Löfgren J, de Nijs R, Zamogilnaya Y, Højgaard L, Fischer BM (2012) PET/MR in oncology: an introduction with focus on MR and future perspectives for hybrid imaging. Am J Nucl Med Mol Imaging 2(4):458–474
Broos W, van der Zant FM, Knol R, Wondergem M (2019) Choline PET/CT in parathyroid imaging: a systematic review. Nucl Med Commun 40(2):96–105
Hocevar M, Lezaic L, Rep S, Zaletel K, Kocjan T, Sever MJ, Zgajnar J, Peric B (2017) Focused parathyroidectomy without intraoperative parathormone testing is safe after pre-operative localization with 18F-Fluorocholine PET/CT. Eur J Surg Oncol 43(1):133–137
Broos W, Wondergem M, Knol R, van der Zant FM (2019) Parathyroid imaging with 18F-fluorocholine PET/CT as a first-line imaging modality in primary hyperparathyroidism: a retrospective cohort study. EJNMMI Res 9(1):72
Wakamatsu H, Noguchi S, Yamashita H, Yamashita H, Tamura S, Jinnouchi S, Nagamachi S, Futami S (2003) Parathyroid scintigraphy with 99mTc-MIBI and 123I subtraction: a comparison with magnetic resonance imaging and ultrasonography. Nucl Med Commun 24(7):755–762
Mahajan A, Starker LF, Ghita M, Udelsman R, Brink JA, Carling T (2012) Parathyroid four-dimensional computed tomography: evaluation of radiation dose exposure during preoperative localization of parathyroid tumors in primary hyperparathyroidism. World J Surg 36(6):1335–1339
Aroquaux A, Rager O, Poncet A, Delattre BM, Ratib O, Becker CD, Dulguerov P, Dulguerov N, Zaidi H, Becker M (2014) Detection and quantification of focal uptake in head and neck tumours: (18)F-FDG PET/MR versus PET/CT. Eur J Nucl Med Mol Imaging 41(3):462–475
Numerow LM, Morita ET, Clark OH, Higgins GB (1995) Hyperparathyroidism: a comparison of sestamibi scintigraphy, MRI, and ultrasonography. J Magn Reson Imaging 5(6):702–708
McDermott VG, Fernandez RJ, Meakem TJ 3rd, Stolpen AH, Spritzer CE, Gefter WB (1996) Preoperative MR imaging in hyperparathyroidism: results and factors affecting parathyroid detection. AJR Am J Roentgenol 166(3):705–710
Ernst O (2009) Hyperparathyroïdie: applications du scanner et de l’IRM [Hyperparathyroidism: CT and MR findings]. J Radiol 90(3 Pt 2):409–412
Gotway MB, Higgins CB (2000) MR imaging of the thyroid and parathyroid glands. Magn Reson Imaging Clin N Am 8(1):163–168
Lopez Hänninen E, Vogl TJ, Steinmüller T, Ricke J, Neuhaus P, Felix R (2000) Preoperative contrast-enhanced MRI of the parathyroid glands in hyperparathyroidism. Invest Radiol 35(7):426–430
Gotway MB, Reddy GP, Webb WR, Morita ET, Clark OH, Higgins CB (2001) Comparison between MR imaging and 99mTc MIBI scintigraphy in the evaluation of recurrent of persistent hyperparathyroidism. Radiology 218(3):783–790
Slomka PJ, Pan T, Germano G (2016) Recent advances and future progress in PET instrumentation. Semin Nucl Med 46(1):5–19
Broos WAM, Wondergem M, van der Zant FM, Knol RJJ (2019) Dual-time-point 18F-Fluorocholine PET/CT in parathyroid imaging. J Nucl Med 60(11):1605–1610
Rep S, Hocevar M, Vaupotic J, Zdesar U, Zaletel K, Lezaic L (2018) 18F-choline PET/CT for parathyroid scintigraphy: significantly lower radiation exposure of patients in comparison to conventional nuclear medicine imaging approaches. J Radiol Prot 38(1):343–356
Funding
None to declare.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Araz, M., Nak, D., Soydal, Ç. et al. Detectability of 18F-choline PET/MR in primary hyperparathyroidism. Eur Arch Otorhinolaryngol 279, 2583–2589 (2022). https://doi.org/10.1007/s00405-021-07046-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-07046-3