Abstract
Purpose
Chronic rhinosinusitis (CRS) disease burden is associated with pulmonary status in asthmatic CRS patients. Asthma-related emergency department (ED) usage is a predictor of asthma-related mortality. We sought to determine whether measures of CRS disease burden are associated with asthma-related ED usage.
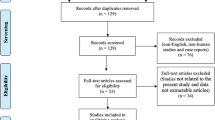
Methods
We prospectively recruited 263 asthmatic CRS patients for this cross-sectional study. CRS burden was measured using the 22-item Sinonasal Outcome Test (SNOT-22), and patient-reported CRS-related antibiotic usage and CRS-related oral corticosteroids usage over the preceding year. Asthma-related ED visits over the prior year were also assessed.
Results
Of all participants, 18.6% had at least 1 asthma-related ED visit (mean 0.3 ED visits for the whole cohort). Asthma-related ED usage was associated with SNOT-22 score [adjusted rate ratio (RR) = 1.02, 95% CI 1.01–1.03, p = 0.040] and CRS-related oral corticosteroids usage in the past year (RR = 1.52, 95% CI 1.26–1.83, p < 0.001). From the SNOT-22 score, asthma-related ED usage was only associated with the nasal subdomain score (RR = 1.08, 95% CI 1.03–1.13, p = 0.001). These measures of CRS disease burden could be used with good sensitivity and specificity to detect patients with asthma-related ED usage in the past year, the majority of whom were undertreated for their asthma.
Conclusions
Measures of CRS disease burden are associated with and can be used to detect, patients having asthma-related ED usage. These results further solidify the connection between CRS and asthma disease courses, and also present an opportunity to use CRS disease burden as a tool for identifying—and implementing greater treatment of—patients at highest risk for asthma-related mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic rhinosinusitis (CRS) is a common inflammatory disease of the paranasal sinus mucosa that results in loss of productivity and a significant quality of life detriment. CRS affects up to 10% of the population and its clinical manifestations lead patients to seek care and treatments totaling billions of dollars in healthcare costs every year [1, 2]. CRS decreases both quality of life (QOL) and productivity through the chronic symptomatology that patients experience [3,4,5,6]. The burden of CRS is not only derived from chronic symptomatology but also other elements of the disease process [7]. Previous research has demonstrated that patient-reported CRS-related antibiotics and systemic corticosteroids usage are distinct aspects of CRS disease burden and independent drivers of decreased QOL and productivity loss [7, 8]. CRS-related antibiotics and oral corticosteroids usage is reflective of poor CRS symptom control1 and is hypothesized to reflect acute exacerbations of CRS [5, 7].
Additionally, it has been shown that there is a strong association between the severity of CRS and the degree of asthma control experienced by asthmatic CRS patients [9, 10]. Both symptom burden and the usage of CRS-related antibiotics and corticosteroids have been shown to be associated with not only asthma control but also QOL and productivity loss in asthmatic CRS patients [8, 10, 11]. In fact, the direct impact of CRS to drive poor asthma control may be a distinct mechanism for decreased QOL in asthmatic CRS patients [12]. Asthma, like CRS, manifests not only as baseline chronic symptomatology but also with acute exacerbations of those symptoms, all of which may lead to life-threatening complications. Poorly controlled asthma is a risk factor for mortality [13]. In this vein, asthma-related emergency department (ED) usage in the prior year has been associated with asthma-related mortality [14] and has recognized by international consensus to be a measure of the frequency of severe asthma exacerbations [15]. Given the epidemiologic and pathophysiologic associations between CRS and asthma, a natural question is whether CRS disease burden may be a driver of asthma exacerbations. In this study, we take the first step in studying this question by seeking to determine whether CRS disease burden, as measured by symptom burden and sinus-related systemic medication usage, would be associated with asthma-related ED usage.
Materials and methods
Study participants
This study was approved by our institution’s Human Studies Committee. Adult patients (age 18 years or older) with CRS were recruited prospectively and provided informed consent for inclusion into this study. All participants met consensus, guideline-established criteria for CRS [16]. Exclusion criteria included comorbid diagnoses of (1) vasculitis, (2) cystic fibrosis, (3) sarcoidosis, and (4) immunodeficiency. To remove the confounding effect of recent endoscopic sinus surgery, patients who had endoscopic sinus surgery within the last 6 months were excluded.
Study design and data collection
This is a cross-sectional study. All data were collected at enrollment. Demographic information including age and gender was collected. Any patient who was an active smoker or reported a history of being a tobacco smoker in the past was considered a smoker [17, 18]. At enrollment, participants were assessed by the evaluating physician for a history of asthma diagnosed based on consensus guidelines as well as a history of aeroallergen hypersensitivity based on formal allergy testing. Participants were interviewed to determine if they had a history of a previous sinus surgery or a history of aspirin sensitivity. The presence of nasal polyps was determined based on nasal endoscopy. Intranasal corticosteroids (spray or irrigation) use as well as the use of an inhaled corticosteroid were also assessed. The numbers of CRS-related antibiotic courses taken and CRS-related oral corticosteroids courses taken in the last 12 months, as reported by the participant, were also assessed [5, 19]. All participants completed the validated 22-item Sinonasal Outcome Test (SNOT-22) [20]. The validated nasal, sleep, ear/facial discomfort and emotional subdomains of the SNOT-22 were calculated as previously described [21, 22]. Specifically, the SNOT-22 nasal subdomain score was calculated by summing SNOT-22 items 1-6, 21 and 22. The SNOT-22 ear/facial discomfort subdomain score was calculated by summing SNOT-22 items 7-10. The SNOT-22 sleep subdomain score was calculated by summing SNOT-22 items 11-18. The SNOT-22 emotional subdomain score was calculated by summing SNOT-22 items 19 and 20 [21, 22]. All participants completed the Asthma Control Test (ACT) [23] and reported the number asthma-related visits to an ED in the past year.
Statistical analysis
All analysis was performed using the statistical software package R (www.r-project.org) [24]. Correlation was performed with Spearman correlation. Associations between asthma-related ED visits as dependent variable, and measures of CRS disease burden (SNOT-22 score and number of patient-reported CRS-related antibiotic or oral corticosteroids in the past year), as independent variables, were determined with univariate and multivariable negative binomial regression. Multivariable models controlled for age, gender, smoking history, aeroallergen hypersensitivity, inhaled corticosteroid use, polyps and history of previous sinus surgery. To identify and characterize the sensitivity and specificity of using metrics of CRS disease burden for detecting participants with at least one prior asthma-related ED visit in the prior year, we analyzed receiver operating characteristic (ROC) curves with the pROC package [25]. The area under the ROC curve (AUC) was calculated with the trapezoid rule using the auc() function and the 95% confidence interval of the AUC was calculated by performing 2000 bootstraps of the data with the ci() function. p value for the significance of the ROC curve was determined by Wilcoxon’s rank-sum test.
Results
Characteristics of study participants
A total of 263 asthmatic CRS patients were included in the study. The characteristics of the study participants are summarized in Table 1. The mean age of the study participants was 50.2 years [standard deviation (SD): 16.5]. As previously described, [11, 26, 27] there was a predominance of women (61.6%) in this group of asthmatic CRS patients. The mean SNOT-22 score was 43.4 (SD: 22.6). Participants reported a mean 2.0 (SD: 2.0) number of CRS-related antibiotics courses and mean 1.4 (SD: 1.8) number of CRS-related oral corticosteroids in the past year. Of all participants, 66.5% reported at least one CRS-related antibiotics course and 52.8% reported at least one CRS-related oral corticosteroids course in the past year.
Participants had a mean ACT score of 20.0 (SD: 4.9) and they reported a mean 0.3 (SD: 0.7) visits to EDs for asthma in the past year. Of all participants, 18.6% reported at least one ED visit for asthma in the past year. Of the participants who reported at least 1 asthma-related ED visit in the prior year, the mean ACT score was 16.6 (SD: 5.9), 69.4% reported using a daily corticosteroid inhaler and 49.0% reported use of a short-acting beta-agonist rescue inhaler multiple times per day indicative of very poor asthma control [28].
CRS disease burden is associated with asthma-related ED usage
We sought to determine if measures of CRS disease burden, SNOT-22 score and CRS-related antibiotics usage, and CRS-related corticosteroids usage was associated with asthma-related ED usage (Table 2). On univariate analysis, asthma-related ED visits in the past year was associated with SNOT-22 score [rate ratio (RR) = 1.02, 95% CI 1.01–1.04, p = 0.001], CRS-related antibiotics usage (RR = 1.19, 95% CI: 1.03–1.37, p = 0.016), and CRS-related oral corticosteroids usage (RR = 1.44, 95% CI 1.26–1.65, p < 0.001). On multivariable analysis, asthma-related ED usage in the past year was associated with the SNOT-22 score (RR = 1.02, 95% CI 1.01–1.03, p = 0.040) and CRS-related oral corticosteroids usage in the past year (RR = 1.52, 95% CI 1.26–1.83, p < 0.001). Asthma-related ED usage in the past year was not associated with CRS-related antibiotics usage in the past year (RR = 0.85, 95% CI 0.71–1.03, p = 0.107).
Because the SNOT-22 encompasses different types of symptoms associated with CRS, we next sought to determine what symptoms of CRS most associated with asthma-related ED visits. We, therefore, sought association between asthma-related ED usage and the nasal, sleep, ear/facial discomfort and emotional subdomains of the SNOT-22. While accounting for all subdomains simultaneously in a multivariable regression model (Table 3), we found that asthma-related ED usage was only associated with the nasal subdomain score (RR = 1.08, 95% CI 1.03–1.13, p = 0.001).
CRS disease burden may identify patients with asthma-related ED utilization in the past year
We next sought to determine whether any metrics of CRS severity could be used to detect asthmatic CRS patients who have reported at least one asthma-related ED visit in the prior year. We performed ROC analysis to detect the accuracy of SNOT-22, as well as CRS-related antibiotics and CRS-related oral corticosteroids in the past year for detecting patients with at least one asthma-related ED visit in the prior year. We found that all three measures of CRS disease burden—SNOT-22 score as well as CRS-related antibiotics and CRS-related oral corticosteroids taken in the last year—were statistically significant predictors of asthma-related ED usage in the past year (Table 4). SNOT-22 score (SNOT-22 score > 30, sensitivity: 89.8%, specificity: 35.5%) and CRS-related antibiotics usage in the past year (antibiotics courses \(\ge\) 1, sensitivity: 85.7%, specificity: 37.9%) are sensitive but not specific. As we found with the SNOT-22 score, the nasal subdomain score of the SNOT-22 (nasal subdomain score > 18, sensitivity: 83.7%, specificity: 46.7%) was sensitive but not specific for detecting patients with asthma-related ED usage in the past year. However, having SNOT-22 score > 30 and having used at least 1 CRS-related antibiotics course in the last year had 77.0% sensitivity and 59.9% specificity for detecting asthmatic CRS patients who had had at least 1 asthma-related ED visit in the past year. Having a SNOT-22 nasal subdomain score > 18 and having used at least 1 CRS-related antibiotics course in the last year had 71.7% sensitivity and 66.9% specificity for detecting asthmatic CRS patients who had had at least 1 asthma-related ED visit in the past year. In comparison, CRS-related oral corticosteroids usage greater than 1 course in the past year had 65.3% sensitivity and 74.3% specificity for detecting patients who had asthma-related ED usage in the past year.
Discussion
There is a strong association between CRS disease burden and pulmonary status in asthmatic CRS patients. Poorly controlled asthma is a risk factor for mortality [13] and acute exacerbations of CRS may be important drivers of asthma exacerbations [15]. In this study, we sought to determine whether CRS disease burden is associated with asthma-related ED usage. We found that asthma-related ED visit in the past year was associated with and could be predicted by SNOT-22 score, CRS- related antibiotic usage, and CRS- related oral corticosteroid usage. We also found that the nasal subdomain of the SNOT-22 was the only subdomain associated with asthma-related ED usage.
There is abundant evidence for a pathophysiologic connection and relationship between CRS and asthma. For example, there are cellular and molecular mediators of inflammation that are common to both CRS and asthma [29] and there are common histopathologic changes that occur in the sinuses of CRS patients compared to the lungs of asthmatics [30]. In fact, histopathologic changes in sinus mucosa during CRS, such as basement membrane thickening, may be accentuated in asthmatic CRS patients compared to non-asthmatic CRS patients [30]. Severe asthmatics with CRS have been found to have higher levels of eosinophils both in their serum and sputum compared to severe asthmatics without CRS [31]. The pathophysiologic relationship between CRS and asthma extends to therapeutic potential as well—specifically, treatment of CRS in asthmatic CRS patients is associated with improved asthma outcomes as well [32,33,34,35,36,37,38].
Our results showing that CRS disease burden is associated with asthma-related ED usage is in line with previous studies finding associations between clinical measures of CRS burden and clinical asthma outcomes. For example, in asthmatics with CRS, the radiographic burden of sinus disease is positively correlated with the severity of asthma [39, 40]. CRS disease burden, measured using symptom burden or the burden of CRS-related systemic medication (antibiotics and corticosteroids) has also been shown to be positively associated with poor asthma control and lost productivity in asthmatic CRS patients [8,9,10,11,12, 41] Our present study goes further in characterizing the association between CRS disease burden and asthma control by examining a highly significant consequence of poor asthma control—asthma-related ED usage—which is reflective of not only severe asthma exacerbations and healthcare utilization but also asthma-related mortality. That we found CRS symptom burden (SNOT-22 score) and CRS-related oral corticosteroid usage to be associated with asthma-related ED usage is intuitive and follows from past associations between CRS disease burden and clinical outcomes of asthma. In comparison. We did not find an association between asthma-related ED usage and CRS- related antibiotic usage. This may be because physicians may have a lower threshold for prescribing antibiotics than corticosteroids, and thus antibiotic prescriptions may be written for less severe disease. Alternatively, the relationship between CRS and asthma exacerbations is due to exacerbations of the underlying pathophysiology of CRS (i.e., an inflammatory process) rather than an infectious process.
To our knowledge, no prior study of asthmatic CRS patients has assessed the relationship between CRS disease burden and asthma-related ED usage. As the first study of this topic, we sought to determine whether CRS disease burden would be associated with asthma-related ED usage. We found that 18.6% of asthmatic CRS patients reported that they had at least one ED visit for asthma in the past year. We also found this ED usage was associated with CRS disease burden measures, specifically SNOT-22 score (nasal subdomain) and CRS-related oral corticosteroids. Therefore, these measures of CRS disease burden may be used to predict and identify/screen for asthmatic CRS patients who have had asthma-related ED visits.
Screening asthmatic CRS patients who have required asthma-related ED usage provides an opportunity to improve quality of life, reduce asthma-related health care costs and potentially reduce the risk of asthma-related mortality by making sure asthma in these patients asthma is appropriately managed. Asthma-related ED usage is one asthma outcome measure that is reflective of patient access to care, disease severity, and socioeconomic factors [42]. A number of asthma-related ED visits are for potentially preventative asthma crises [43]. If these patients had improved access to comprehensive asthma care in primary care seating, they may not have needed to seek out acute care. A greater understanding of CRS and its impact on asthma-related ED usage will improve patent well-being and safety as well as save healthcare costs.
Our results should be interpreted in the context of the limitations of our study. First, a cross-sectional study does not show causation. Second, this data was collected from patients in a single center. Third, while ED usage is mostly driven by disease severity, when patients are forced to seek treatment due to deterioratation of their condition, their social determinants of health and healthcare access may also play a role in ED utilization [44,45,46].
Conclusion
The burden of CRS is associated with asthma-related morbidity. This extends to asthma-related ED usage, which we find to be associated with and predicted by SNOT-22 score, CRS- related antibiotic usage, and CRS- related oral corticosteroid usage. Amongst CRS symptom, the burden of nasal symptoms is dominantly associated with asthma-related ED usage.
References
Fokkens WJ, Lund VJ, Mullol J et al (2012) European position paper on rhinosinusitis and nasal polyps 2012. Rhinol Suppl 23:298
Orlandi RR, Kingdom TT, Hwang PH et al (2016) International consensus statement on allergy and rhinology: rhinosinusitis. Int Forum Allergy Rhinol 6(Suppl 1):S209
Campbell AP, Phillips KM, Hoehle LP et al (2017) Depression symptoms and lost productivity in chronic rhinosinusitis. Ann Allergy Asthma Immunol 118:286–289
Hoehle LP, Phillips KM, Bergmark RW, Caradonna DS, Gray ST, Sedaghat AR (2016) Symptoms of chronic rhinosinusitis differentially impact general health-related quality of life. Rhinology 54:316–322
Phillips KM, Hoehle LP, Bergmark RW, Caradonna DS, Gray ST, Sedaghat AR (2017) Acute exacerbations mediate quality of life impairment in chronic rhinosinusitis. J Allergy Clin Immunol Pract 5:422–426
Speth MM, Hoehle LP, Phillips KM, Caradonna DS, Gray ST, Sedaghat AR (2018) Changes in chronic rhinosinusitis symptoms differentially associate with improvement in general health-related quality of life. Ann Allergy Asthma Immunol 121:195–199
Sedaghat AR, Hoehle LP, Gray ST (2018) Chronic rhinosinusitis control from the patient and physician perspectives. Laryngoscope Investig Otolaryngol 3:419–433
Banoub RG, Phillips KM, Hoehle LP, Caradonna DS, Gray ST, Sedaghat AR (2018) Relationship between chronic rhinosinusitis exacerbation frequency and asthma control. Laryngoscope 128:1033–1038
Phillips KM, Hoehle LP, Bergmark RW et al (2017) Chronic rhinosinusitis severity is associated with need for asthma-related systemic corticosteroids. Rhinology 55:211–217
Phillips KM, Hoehle LP, Caradonna DS, Gray ST, Sedaghat AR (2016) Association of severity of chronic rhinosinusitis with degree of comorbid asthma control. Ann Allergy Asthma Immunol 117:651–654
Phillips KM, Bergmark RW, Hoehle LP, Caradonna DS, Gray ST, Sedaghat AR (2018) Chronic rhinosinusitis exacerbations are differentially associated with lost productivity based on asthma status. Rhinology 56:323–329
Phillips KM, Talat R, Caradonna DS, Gray ST, Sedaghat AR (2019) Quality of life impairment due to chronic rhinosinusitis in asthmatics is mediated by asthma control. Rhinology 57:430–435
Jalaludin BB, Smith MA, Chey T, Orr NJ, Smith WT, Leeder SR (1999) Risk factors for asthma deaths: a population-based, case-control study. Aust NZ J Public Health 23:595–600
To T, Zhu J, Williams DP et al (2016) Frequency of health service use in the year prior to asthma death. J Asthma 53:505–509
Reddel HK, Taylor DR, Bateman ED et al (2009) An official American Thoracic Society/European Respiratory Society statement: asthma control and exacerbations: standardizing endpoints for clinical asthma trials and clinical practice. Am J Respir Crit Care Med 180:59–99
Rosenfeld RM, Piccirillo JF, Chandrasekhar SS et al (2015) Clinical practice guideline (update): adult sinusitis. Otolaryngology–head and neck surgery. Off J Am Acad Otolaryngol Head Neck Surg 152:S39
Hoehle LP, Phillips KM, Caradonna DS, Gray ST, Sedaghat AR (2018) A contemporary analysis of clinical and demographic factors of chronic rhinosinusitis patients and their association with disease severity. Ir J Med Sci 187:215–221
Phillips KM, Hoehle L, Bergmark RW, Caradonna DS, Gray ST, Sedaghat AR (2017) Reversal of smoking effects on chronic rhinosinusitis after smoking cessation. Otolaryngol Head Neck Surg 157:737–742
Yamasaki A, Hoehle LP, Phillips KM et al (2018) Association between systemic antibiotic and corticosteroid use for chronic rhinosinusitis and quality of life. Laryngoscope 128:37–42
Hopkins C, Gillett S, Slack R, Lund VJ, Browne JP (2009) Psychometric validity of the 22-item sinonasal outcome test. Clinical otolaryngology: official journal of ENT-UK. Off J Nether Soc Oto-Rhino-Laryngol Cervico-Facial Surg 34:447–454
Sedaghat AR, Gray ST, Caradonna SD, Caradonna DS (2015) Clustering of chronic rhinosinusitis symptomatology reveals novel associations with objective clinical and demographic characteristics. Am J Rhinol Allergy 29:100–105
Feng AL, Wesely NC, Hoehle LP et al (2017) A validated model for the 22-item sino-nasal outcome test subdomain structure in chronic rhinosinusitis. Int Forum Allergy Rhinol 7:1140–1148
Schatz M, Sorkness CA, Li JT et al (2006) Asthma control test: reliability, validity, and responsiveness in patients not previously followed by asthma specialists. J Allergy Clin Immunol 117:549–556
Team RDC (2011) R: a language and environment for statistical computing. R foundation for statistical computing, Vienna, Austria
Robin X, Turck N, Hainard A et al (2011) pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinform 12:77
Jarvis D, Newson R, Lotvall J et al (2012) Asthma in adults and its association with chronic rhinosinusitis: the GA2LEN survey in Europe. Allergy 67:91–98
Stevens WW, Peters AT, Suh L et al (2015) A retrospective, cross-sectional study reveals that women with CRSwNP have more severe disease than men. Immun Inflamm Dis 3:14–22
EPR-3. NAEPP expert panel report 3: guidelines for the diagnosis and treatment of asthma. Bethesda (MD): US Department of Health and Human Services; National Institutes of Health; National Heart, Lung, and Blood Institute 2007
Cao PP, Wang ZC, Schleimer RP, Liu Z (2019) Pathophysiologic mechanisms of chronic rhinosinusitis and their roles in emerging disease endotypes. Ann Allergy Asthma Immunol 122:33–40
Harlin SL, Ansel DG, Lane SR, Myers J, Kephart GM, Gleich GJ (1988) A clinical and pathologic study of chronic sinusitis: the role of the eosinophil. J Allergy Clin Immunol 81:867–875
ten Brinke A, Grootendorst DC, Schmidt JT et al (2002) Chronic sinusitis in severe asthma is related to sputum eosinophilia. J Allergy Clin Immunol 109:621–626
Alobid I, Benitez P, Bernal-Sprekelsen M, Guilemany JM, Picado C, Mullol J (2005) The impact of asthma and aspirin sensitivity on quality of life of patients with nasal polyposis. Qual Life Res 14:789–793
Batra PS, Kern RC, Tripathi A et al (2003) Outcome analysis of endoscopic sinus surgery in patients with nasal polyps and asthma. Laryngoscope 113:1703–1706
Jankowski R, Moneret-Vautrin DA, Goetz R, Wayoff M (1992) Incidence of medico-surgical treatment for nasal polyps on the development of associated asthma. Rhinology 30:249–258
Slavin RG (1992) Asthma and sinusitis. J Allergy Clin Immunol 90:534–537
Senior BA, Kennedy DW, Tanabodee J, Kroger H, Hassab M, Lanza DC (1999) Long-term impact of functional endoscopic sinus surgery on asthma. Otolaryngology–head and neck surgery. Off J Am Acad Otolaryngol-Head Neck Surg 121:66–68
Lund VJ (1999) The effect of sinonasal surgery on asthma. Allergy 54(Suppl 57):141–145
Schlosser RJ, Smith TL, Mace J, Soler ZM (2017) Asthma quality of life and control after sinus surgery in patients with chronic rhinosinusitis. Allergy 72:483–491
Bresciani M, Paradis L, Des Roches A et al (2001) Rhinosinusitis in severe asthma. J Allergy Clin Immunol 107:73–80
Pearlman AN, Chandra RK, Chang D et al (2009) Relationships between severity of chronic rhinosinusitis and nasal polyposis, asthma, and atopy. Am J Rhinol Allergy 23:145–148
Campbell AP, Phillips KM, Hoehle LP et al (2018) Association between asthma and chronic rhinosinusitis severity in the context of asthma control. Otolaryngol Head Neck Surg 158:386–390
Johnson LH, Chambers P, Dexheimer JW (2016) Asthma-related emergency department use: current perspectives. Open Access Emerg Med 8:47–55
Nath JB, Hsia RY (2015) Children’s emergency department use for asthma, 2001–2010. Acad Pediatr 15:225–230
Bergmark RW, Hoehle LP, Chyou D et al (2018) Association of socioeconomic status, race and insurance status with chronic rhinosinusitis patient-reported outcome measures. Otolaryngol Head Neck Surg 158:571–579
Bergmark RW, Ishman SL, Phillips KM, Cunningham MJ, Sedaghat AR (2018) Emergency department use for acute rhinosinusitis: insurance dependent for children and adults. Laryngoscope 128:299–303
Bergmark RW, Sedaghat AR (2017) Disparities in health in the United States: an overview of the social determinants of health for otolaryngologists. Laryngoscope Investig Otolaryngol 2:187–193
Acknowledgements
The authors gratefully acknowledge the contribution of the patients who participated in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no potential conflicts or financial relationships.
Ethical approval
This study and its design was approved by the institutional human studies committee.
Informed consent
All patients provided informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gleadhill, C., Speth, M.M., Gengler, I. et al. Chronic rhinosinusitis disease burden is associated with asthma-related emergency department usage. Eur Arch Otorhinolaryngol 278, 93–99 (2021). https://doi.org/10.1007/s00405-020-06259-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-020-06259-2