Abstract
Background
Chronic rhinosinusitis (CRS) is highly prevalent, significantly decreases quality of life and leads to tremendous health care costs every year. No recent study has characterised the prevalence of potentially CRS-modifying patient characteristics and simultaneously shown their impact on CRS severity.
Aims
We sought to determine the prevalence of potential clinical and demographic CRS-modifying characteristics and their associations with CRS symptom severity in a large contemporary cohort of CRS patients.
Methods
Retrospective review of CRS patients who visited our rhinology clinics between February 2016 and February 2017 was conducted. CRS symptom severity was measured using the 22-item Sinonasal Outcomes Test (SNOT-22) questionnaire, which all patients received. Association was sought between SNOT-22 score (as dependent variable) and patients’ clinical and demographic characteristics using linear regression.
Results
Of the 572 included patients, the mean age was 51.1 years (SD = 15.8) and the mean SNOT-22 score was 34.3 (SD = 22.6). Prevalence of granulomatous diseases, immunodeficiency and cystic fibrosis were each approximately 5%. Prevalence of aeroallergen hypersensitivity was 42.3% and prevalence of asthma was 27.8%. More severe CRS symptomatology was associated with smoking tobacco (adjusted β = 5.47, p = 0.034) and comorbid asthma (adjusted β = 12.02, p < 0.001), whilst less severe symptomatology was associated with older age (adjusted β = −0.23, p = 0.002) and diagnosis of cystic fibrosis (adjusted β = −11.87, p = 0.009).
Conclusions
In a contemporary cohort of CRS patients, prevalence of disease-modifying comorbidities ranged from approximately 5 to over 40%. Smoking tobacco and asthma were associated with more severe CRS symptomatology, whilst older age and diagnosis of cystic fibrosis were associated with less severe CRS symptomatology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic rhinosinusitis (CRS) is an inflammatory disorder of the sinonasal mucosa that affects approximately 5% of the population in Western Europe and the USA [1, 2]. CRS has a significant and dramatic impact on afflicted patients by reducing quality of life (QOL) through chronic sinonasal symptoms, acute exacerbations and exacerbation of comorbid pulmonary conditions [3,4,5,6]. The QOL detriment associated with CRS is comparable to, or worse than, the QOL detriment due to chronic diseases such as asthma or diabetes [7, 8]. Additionally, the disease manifestations of CRS result in billions of Euros and dollars of costs every year related to direct health care costs, including doctor’s visits and treatments, as well as indirect costs related to lost productivity from missed days of work [8, 9].
Patients with CRS can present to physicians of all specialties, from general practitioners and internal medicine physicians to subspecialists such as allergists or otolaryngologists. Therefore, an understanding of CRS, including knowledge of comorbidities that can modify the disease course and factors that are associated with greater disease severity, is of benefit to all physicians. Previous studies have identified underlying conditions such as granulomatous diseases, ciliary dysfunction, immunodeficiency and cystic fibrosis that can predispose patients to develop CRS [10, 11]. Moreover, other conditions such as allergy and asthma, which are frequently associated with CRS, may modify the CRS disease course and potentially affect sinonasal symptomatology [2, 12,13,14]. However, a rigorous epidemiologic study of a contemporary CRS cohort to assess the prevalence of these disease-modifying characteristics and their association with CRS severity has not been performed. Additionally, of the over 5000 studies about CRS that have been indexed on PubMed, over 50% have been published in the just the last 5 years, indicating the rapid progress in study of this disease. Despite the proliferation of CRS studies, many clinical in nature which must incorporate disease-modifying characteristics into their study design and analyses, it is surprising that no single study has provided a rigorous analysis of clinical and demographic characteristics that may impact CRS disease severity.
There is therefore a pressing need for a centralised study of the clinical and demographic characteristics of CRS patients and how these characteristics may impact CRS disease severity. In order to address this need, we performed a retrospective analysis of a contemporary cohort of CRS patients seen at a single centre over a 1-year period to achieve the following two objectives: to provide a highly detailed, descriptive evaluation of the demographic and clinical characteristics of this general population of CRS patients and to identify the patient characteristics that are associated with CRS disease severity. We believe that the results of our study will not only be beneficial to the many physicians who care for CRS patients but also for the design and analysis of future clinical studies of CRS patients.
Methods
Approval for this study was obtained from the Massachusetts Eye and Ear Infirmary (MEEI) Human Studies Committee. A consecutive series of adult patients (with age of 18 years or older) diagnosed with CRS based on clinical consensus guideline criteria [1] by the authors between February 1, 2016 and February 1, 2017 was retrospectively identified and studied. The only other mandatory criteria for inclusion were availability of medical records and completion of a 22-item Sinonasal Outcomes Test (SNOT-22) questionnaire, which every patient to our clinic receives. The SNOT-22 is a questionnaire that is validated for use in evaluating rhinitis and rhinosinusitis, and quantitatively assesses the severity of sinonasal symptomatology [15, 16]. In the setting of CRS, the SNOT-22 not only measures the severity of CRS symptoms but also reflects the negative impact upon CRS-specific QOL. The SNOT-22 has a range of 0 (for no symptoms and QOL impact) to 110 (the most severe symptoms and greatest QOL impact) [16]. In this study, we use the SNOT-22 as our measure of CRS disease severity. If a patient visited our centre on more than one occasion during the study period, only the SNOT-22 score from the first visit was used for this study. Since we sought to fully characterise the CRS patient population, we did not implement any exclusion criteria.
At the time of diagnosis, all patients were assessed for allergic rhinitis based on formal skin or serological allergy testing, asthma based on clinical consensus guideline criteria [17] and nasal polyps based on nasal endoscopy. Diagnoses of immunodeficiency, vasculitis, sarcoidosis, cystic fibrosis, primary ciliary dyskinesia and aspirin sensitivity were also made based on clinical history and a prior established diagnosis. If the patient history was suggestive of any of these conditions but did not have a formal diagnosis, then the patient was sent for further evaluation by the appropriate subspecialist so that a formal diagnosis could be either definitively ruled out or confirmed. The presence of any of these comorbid conditions was collected as a part of our analysis.
All statistical analysis was performed with the statistical software, R (www.r-project.org). Associations between SNOT-22 score (as the dependent variable) and patients’ clinical and demographic characteristics (as the independent variables) was performed using the linear regression function ols() in the rms package [18]. Multivariable analysis was performed using all clinical and demographic variables. In the multivariable model, significant predictors were identified via backwards elimination, using a P value cutoff of 0.100, as recommended [18].
Results
Patient characteristics
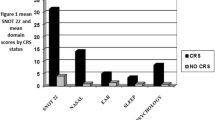
A total of 572 CRS patients were identified and their characteristics are summarised in Table 1. The mean age was 51.1 years (SD = 15.8), with a roughly normal distribution (Fig. 1a), and 47.7% of the patients were male and 52.2% were female. Our patient cohort was composed primarily of Caucasians (85.7%) and 25.5% of our patients reported a history of smoking tobacco. Nasal polyposis was noted in 44.8% of patients. In terms of comorbidities, aeroallergen hypersensitivity (42.3%) and asthma (27.8%) were the most common. Amongst asthmatics, 8.6% (2.4% of the overall study population) had aspirin exacerbated respiratory disease (AERD) (CRS with nasal polyps and concomitant aspirin sensitivity and asthma). Vasculitis (2.6%) and sarcoid (0.2%) were also present at small frequencies in our cohort. Likewise, comorbid diagnoses of immunodeficiency (4.2%), cystic fibrosis (6.5%) and primary ciliary dyskinesia (0.3%) were identified in our cohort. Amongst patients with vasculitis, the most common form was granulomatosis with polyangiitis (Wegener’s granulomatosis) (53.3%), followed by eosinophilic granulomatosis with polyangiitis (Churg Strauss syndrome) (33.3%). Amongst patients with immunodeficiency, 62.5% had some form of immunoglobulin deficiency, of which 20% had common variable immunodeficiency. In this group of patients with CRS, 37.8% had a prior history of endoscopic sinus surgery and 46.9% were taking intranasal corticosteroids on a consistent, daily basis. The mean SNOT-22 score of these CRS patients was 34.3 (SD = 22.6) with the distribution of SNOT-22 scores illustrated in Fig. 1b.
Clinical and demographic characteristics associated with more severe CRS symptomatology
We next investigated whether any of the above noted patient characteristics were associated with the SNOT-22 score, which reflects CRS symptom severity (Table 2). On univariate association, we found that age (linear regression coefficient [β] = −0.21, 95% CI −0.32–−0.09, p = 0.001) (Fig. 2) was associated with less severe CRS symptomatology (lower SNOT-22 score). Additionally, gender (β = 6.20, 95% CI 2.51–9.88, p = 0.001), a history of smoking (β = 6.18, 95% CI 1.92–10.45, p = 0.005), aeroallergen hypersensitivity (β = 6.77, 95% CI 3.05–10.49, p < 0.001) and comorbid asthma (β = 10.53, 95% CI 6.48–14.57, p < 0.001) were all associated with more severe CRS symptomatology (higher SNOT-22 score), whilst comorbid cystic fibrosis (β = −9.76, 95% CI −17.28–−2.25, p = 0.011) was associated with less severe symptomatology (Fig. 3), as we found for age. After performance of multivariable analysis, accounting for all clinical and demographic characteristics, we found a continued statistically significant association between more severe CRS symptomatology (higher SNOT-22 score) and a history of smoking (β = 5.47, 95% CI 0.41–10.53, p = 0.034) and comorbid asthma (β = 12.02, 95% CI 8.06–15.99, p < 0.001). In addition, age (β = −0.23, 95% CI −0.38–−0.09, p = 0.002) and comorbid cystic fibrosis (β = −11.87, 95% CI −20.82–−2.92, p = 0.009) continued to be associated with less severe CRS symptomatology (lower SNOT-22 score).
Discussion
CRS represents a common and significant QOL burden for the afflicted patient and an economic burden for society at large [2, 7]. Patients with CRS may present to and obtain care from physicians of many different specialties—from generalists to subspecialists—making it a disease with which physicians should be familiar. CRS is a highly heterogeneous disease and there are many comorbid conditions and patient characteristics that can potentially cause, exacerbate or affect management of CRS and its associated symptomatology [14, 19, 20]. Underlying conditions such as immunodeficiency or granulomatous disease affecting the sinonasal cavity may lead to development of CRS [2, 10, 21, 22]. A tendency towards greater airway inflammation, for example in those with aeroallergen hypersensitivity or asthma, may also contribute to greater sinonasal symptomatology [14, 23, 24]. Current clinical practice guidelines on the management of CRS highlight the importance of identifying comorbid conditions, which may underlie or contribute patients’ CRS. Identification of any such comorbid conditions should ideally be made early so that their treatment can be incorporated into management of the CRS [1, 2]. Awareness of the prevalence of such clinical or demographic characteristics in CRS patients is therefore necessary. Additionally, because chronic sinonasal symptomatology is the primary determinant of the QOL detriment that is associated with CRS [3, 6], it is important to understand how different patient characteristics might affect the severity of the disease and therefore the potential aggressiveness with which treatment may be needed. Finally, a thorough study of how clinical characteristics may impact CRS disease severity and the SNOT-22 score (a frequently used metric for sinonasal symptom severity in the research literature) is particularly timely given the rapid proliferation of studies on CRS in the last 5 years and the need for clinical studies of CRS to accurately account for confounding affects of patient characteristics in their study designs and analyses. In this study, we presented a comprehensive analysis of a large contemporary cohort of CRS patients, describing not only the prevalence of the many clinical and demographic characteristics that may cause or affect CRS, but we also determined which of these characteristics was associated with the severity of sinonasal symptomatology.
Previous large epidemiologic studies of CRS performed at the population level have reported an association between asthma and allergic rhinitis, and CRS [25,26,27]. For example, the Global Allergy and Asthma Network of Excellence (GA2LEN) study in Europe has reported an enrichment of asthma and allergic rhinitis in the CRS population [25, 26]. However, these previous studies of CRS and its associated comorbidities have been limited by either identifying CRS patients based on diagnostic codes in large national databases or basing the diagnosis of CRS on patient-reported symptoms—both methods that have been shown to be unreliable in accurately identifying CRS patients [28,29,30]. Additionally, although various studies have separately and independently reported the prevalences of various comorbidities, and their potential impact on CRS [2, 31], we have not been able to find any study of a large population of patients diagnosed with CRS based on clinical consensus guidelines that reports not only the prevalences of CRS-comorbidities but also their association with the severity of CRS symptomatology.
In this study, we addressed the need for such a study by examining almost 600 CRS patients seen in our rhinology clinics in just the last year, identifying not only the prevalences of potentially CRS-modifying comorbidities but also the association of these comorbidities and patient characteristics with the severity of CRS symptomatology. CRS is a complex and heterogeneous disease that may be impacted by many different clinical and demographic characteristics. Our finding that nearly half of our cohort had aeroallergen hypersensitivity and almost a quarter of our cohort had asthma underscores the need for consideration of allergy and asthma testing in patients with CRS [7, 14]. We have additionally shown in this large cohort of CRS patients that the prevalence of granulomatous diseases (vasculitis and sarcoidosis), immunodeficiency and cystic fibrosis were each approximately 5%. Moreover, we find that the most common granulomatous disease is granulomatosis with polyangiitis (Wegener’s granulomatosis), followed by eosinophilic granulomatosis with polyangiitis (Churg Strauss syndrome), and that the most common immunodeficiency is an immunoglobulin deficiency. Our findings indicate that these comorbidities exist at a frequency such that they should be routinely considered when evaluating and managing CRS patients. Early detection and treatment of these atypical causes of CRS should be considered, especially in patients that fail to respond to the standard treatment of CRS. In patients with a history of excessive recurrent acute rhinosinusitis or frequent acute exacerbations of CRS, evaluating for immunodeficiency with immunoglobulin levels might be considered. For patients with excessive nasal crusting and epistaxis or systemic signs suggestive of vasculitis, a laboratory evaluation including ESR and ANCA or a nasal biopsy might ultimately be necessary for diagnosis [10, 22, 32, 33].
In addition to these findings, we identified certain patient characteristics that are associated with the severity of CRS symptoms. A history of smoking tobacco and comorbid asthma were both associated with more severe CRS symptomatology. In contrast, higher age and a comorbid diagnosis of cystic fibrosis were associated with less severe CRS symptomatology. These findings should be interpreted in the context of the minimum clinically important difference of the SNOT-22 questionnaire, the validated instrument we used to quantify the severity of sinonasal symptomatology. The minimum clinically important difference of the SNOT-22, which is 9 points, reflects the minimum score change that is noticeable by CRS patients [16]. Comorbid asthma was associated with a 12-point increase, whilst comorbid cystic fibrosis was associated with a 12-point decrease in SNOT-22 score. Every 10-year increase in age was associated with a 2.3-point decrease in SNOT-22, requiring an approximate 40-year age difference to be associated with a 9-point decrease in SNOT-22. Additionally, a history of smoking was associated with a 5.5-point increase in SNOT-22. Although the effects of age and smoking history might not be expected to meet the minimum clinically important difference in SNOT-22, it is important to remember that the effects of these characteristics may be additive, and therefore, it is important to be aware of these associations. Finally, it is equally important that we found that none of the other demographic or clinical characteristics were associated with more severe CRS symptomatology, indicating that physicians cannot rely on more severe sinonasal symptomatology to detect comorbidities such as granulomatous disease, immunodeficiency or cystic fibrosis (which was associated with less severe sinonasal symptomatology in our cohort) but must instead be vigilant to the possibilities of these comorbidities. With the high prevalence of CRS, awareness of these comorbidities and determinants of CRS severity may improve and spare significant QOL for affected patients.
Our results should be interpreted in the context of our study’s limitations that primarily include its retrospective and cross-sectional design, which do not allow us to identify characteristics associated with better or worse treatment responses. For example, that we found cystic fibrosis to be associated with less severe CRS symptomatology is an interesting finding but we cannot be sure if this is due to factors such as systemic antibiotic use (or other cystic fibrosis-specific treatments) that we are unable to measure due to our retrospective study design. Additionally, we use CRS symptom severity as a reflection of CRS severity. However, there are other measures of CRS severity, such as frequency of acute CRS exacerbations or need for CRS-related systemic medication usage, that may be addressed in future studies. Additionally, although we find that previous sinus surgery by itself was not associated with lower SNOT-22 score in the general CRS population studied here, future study focused solely on CRS patients with (or without) a history of sinus surgery may be able to more finely characterise how clinical characteristics impact SNOT-22 score in these substrata of patients whilst accounting for modifying factors such as the number of previous sinus surgeries and the time since the last sinus surgery. Finally, all patients included in this study were from one centre, from clinics specialising in rhinology, which although is a strength with respect to the diagnostic accuracy of CRS, may limit full applicability of our results to patient populations from other centres or parts of the world.
Conclusions
There is a wide range of clinical and demographic characteristics amongst patients with CRS. Atopic comorbidities are most common but CRS-associated and—modifying comorbidities such as cystic fibrosis, immunodeficiency and granulomatous diseases may be prevalent at around 5%, indicating that these comorbidities should be considered and at least screened for through a careful history and examination. Additionally, when an extensive list of patient characteristics were accounted for and considered, only smoking tobacco and comorbid asthma were associated with worse CRS symptoms whilst older age and comorbid cystic fibrosis were associated with less severe CRS symptoms. These results should not only be considered in the clinical evaluation of CRS patients but also accounted for in the design and analysis of clinical studies on CRS patients.
References
Rosenfeld RM, Piccirillo JF, Chandrasekhar SS et al (2015) Clinical practice guideline (update): adult sinusitis. Otolaryngol Head Neck Surg 152(2 Suppl):S1–S39
Fokkens WJ, Lund VJ, Mullol J et al (2012) European position paper on rhinosinusitis and nasal polyps 2012. Rhinol Suppl 23:3 p preceding table of contents:1–298
Hoehle LP, Phillips KM, Bergmark RW et al (2016) Symptoms of chronic rhinosinusitis differentially impact general health-related quality of life. Rhinology 54(4):316–322
Phillips KM, Hoehle LP, Bergmark RW et al (2017) Acute exacerbations mediate quality of life impairment in chronic rhinosinusitis. J Allergy Clin Immunol Pract 5(2):422–426
Phillips KM, Hoehle LP, Caradonna DS et al (2016) Association of severity of chronic rhinosinusitis with degree of comorbid asthma control. Ann Allergy Asthma Immunol 117(6):651–654
Gray ST, Hoehle LP, Phillips KM, et al (2017) Patient-reported control of chronic rhinosinusitis symptoms is positively associated with general health-related quality of life. Clin Otolaryngol
Lange B, Holst R, Thilsing T et al (2013) Quality of life and associated factors in persons with chronic rhinosinusitis in the general population: a prospective questionnaire and clinical cross-sectional study. Clin Otolaryngol 38(6):474–480
Sahlstrand-Johnson P, Ohlsson B, Von Buchwald C et al (2011) A multi-centre study on quality of life and absenteeism in patients with CRS referred for endoscopic surgery. Rhinology 49(4):420–428
Campbell AP, Phillips KM, Hoehle LP, et al (2017) Depression symptoms and lost productivity in chronic rhinosinusitis. Ann Allergy Asthma Immunol 118(3):286–289
Ryan MW, Brooks EG (2010) Rhinosinusitis and comorbidities. Curr Allergy Asthma Rep 10(3):188–193
Carey RM, Adappa ND, Palmer JN et al (2016) Taste receptors: regulators of sinonasal innate immunity. Laryngoscope Investig Otolaryngol 1(4):88–95
Sedaghat AR, Gray ST, Wilke CO et al (2012) Risk factors for development of chronic rhinosinusitis in patients with allergic rhinitis. Int Forum Allergy Rhinol 2(5):370–375
Sedaghat AR, Gray ST, Chambers KJ et al (2013) Sinonasal anatomic variants and asthma are associated with faster development of chronic rhinosinusitis in patients with allergic rhinitis. Int Forum Allergy Rhinol 3(9):755–761
Steinke JW, Borish L (2016) Chronic rhinosinusitis phenotypes. Ann Allergy Asthma Immunol 117(3):234–240
Pynnonen MA, Kim HM, Terrell JE (2009) Validation of the Sino-Nasal Outcome Test 20 (SNOT-20) domains in nonsurgical patients. Am J Rhinol Allergy 23(1):40–45
Hopkins C, Gillett S, Slack R et al (2009) Psychometric validity of the 22-item Sinonasal Outcome Test. Clin Otolaryngol 34(5):447–454
EPR-3 (2007) NAEPP expert panel report 3: guidelines for the diagnosis and treatment of asthma. US Department of Health and Human Services; National Institutes of Health; National Heart, Lung, and Blood Institute, Bethesda
Harrell FE (2001) Regression modeling strategies: with applications to linear models, logistic regression, and survival analysis. Springer, New York
Dennis SK, Lam K, Luong A (2016) A review of classification schemes for chronic rhinosinusitis with nasal polyposis endotypes. Laryngoscope Investig Otolaryngol 1(5):130–134
London NR, Lane AP (2016) Innate immunity and chronic rhinosinusitis: what we have learned from animal models. Laryngoscope Investig Otolaryngol 1(3):49–56
Martinez Del Pero M, Chaudhry A, Jones RB et al (2009) B-cell depletion with rituximab for refractory head and neck Wegener’s granulomatosis: a cohort study. Clin Otolaryngol 34(4):328–335
Stevens WW, Peters AT (2015) Immunodeficiency in chronic sinusitis: recognition and treatment. Am J Rhinol Allergy 29(2):115–118
Emanuel IA, Shah SB (2000) Chronic rhinosinusitis: allergy and sinus computed tomography relationships. Otolaryngol Head Neck Surg 123(6):687–691
Kim JH, Cho C, Lee EJ et al (2016) Prevalence and risk factors of chronic rhinosinusitis in South Korea according to diagnostic criteria. Rhinology 54(4):329–335
Hastan D, Fokkens WJ, Bachert C et al (2011) Chronic rhinosinusitis in Europe—an underestimated disease. A GA(2)LEN study. Allergy 66(9):1216–1223
Jarvis D, Newson R, Lotvall J et al (2012) Asthma in adults and its association with chronic rhinosinusitis: the GA2LEN survey in Europe. Allergy 67(1):91–98
Soler ZM, Mace JC, Litvack JR et al (2012) Chronic rhinosinusitis, race, and ethnicity. Am J Rhinol Allergy 26(2):110–116
Lange B, Thilsing T, Baelum J et al (2013) Diagnosing chronic rhinosinusitis: comparing questionnaire-based and clinical-based diagnosis. Rhinology 51(2):128–136
Akkina SR, Novis SJ, Keshavarzi NR et al (2016) Academic institution pilot study shows far fewer diagnoses of sinusitis than reported nationally. Laryngoscope Investig Otolaryngol 1(5):124–129
Novis SJ, Akkina SR, Lynn S et al (2016) A diagnostic dilemma: chronic sinusitis diagnosed by non-otolaryngologists. Int Forum Allergy Rhinol 6(5):486–490
Orlandi RR, Kingdom TT, Hwang PH et al (2016) International consensus statement on allergy and rhinology: rhinosinusitis. Int Forum Allergy Rhinol 6 Suppl 1:S22–S209
Naclerio RM, Baroody FM (2016) Other phenotypes and treatment of chronic rhinosinusitis. J Allergy Clin Immunol Pract 4(4):613–620
Erickson VR, Hwang PH (2007) Wegener’s granulomatosis: current trends in diagnosis and management. Curr Opin Otolaryngol Head Neck Surg 15(3):170–176
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This study was approved by the Massachusetts Eye and Ear Infirmary Human Studies Committee.
Informed consent
Because this study was a retrospective study, a waiver of informed consent was given.
Rights and permissions
About this article
Cite this article
Hoehle, L.P., Phillips, K.M., Caradonna, D.S. et al. A contemporary analysis of clinical and demographic factors of chronic rhinosinusitis patients and their association with disease severity. Ir J Med Sci 187, 215–221 (2018). https://doi.org/10.1007/s11845-017-1639-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-017-1639-3