Abstract
Purpose
Nausea and vomiting occur in up to 70% of children after adenotonsillectomy, ingested blood during procedure being one of the reasons for emesis. Hypopharyngeal packing (HP) is a common practice among otolaryngologists to prevent blood from being swallowed, but studies in nasal surgeries in adults failed to show efficacy of this technique in reducing postoperative nausea and vomiting (PONV). There are no studies evaluating the effect of HP in adenotonsillectomy in children. The aim of this study is to evaluate the efficacy HP during adenotonsillectomy in children in the prevention of PONV.
Methods
This is a randomized, double-blinded, controlled trial. Children aged 4–16 years, scheduled for adenotonsillectomy due to sleep-disordered breathing were enrolled in Hospital da Criança Santo Antônio (Brazil). 192 participants were screened, while 129 were enrolled and completed follow-up for primary outcome. Patients were randomized in a consecutive manner to receive HP or not during adenotonsillectomy. PONV occurrence was assessed in the first 24 h after surgery in HP and control group and relative risk with 95% confidence interval was calculated.
Results
There were 129 patients randomized, 64 in the HP and 65 in the control group. Female were 40.3% and mean ± SD age was 7.3 ± 2.9. Baseline characteristics and surgery variables were distributed similarly between the groups. Incidence of PONV was 20.3% in the HP and 23.1% in the control group. The relative risk for PONV was 0.88 (95% CI 0.46–1.70).
Conclusion
Our results suggest that there is no benefit of HP during adenotonsillectomy in children for the prevention of PONV.
Trial registration
Brazilian Register of Randomized Trials (REBEC) identifier: RBR-3zjn27; Universal Trial Number U1111-1197-7461.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
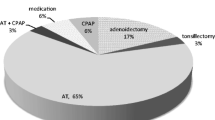
Adenotonsillectomy is the most frequent major surgery performed in children, and suspect or diagnosed obstructive sleep apnea syndrome due to adenotonsillar hyperplasia is the most common indication for this procedure nowadays [1]. Although it is a simple surgical procedure, adenotonsillectomy carries morbidity. Postoperative nausea and vomiting (PONV) occur frequently, with incidence being nearly 70% of all patients operated when no prophylactic antiemetic medication is used [2,3,4]. The etiology of PONV is multifactorial, but it is believed that the presence of swallowed blood from the surgical site is an important factor [5,6,7].
The hypopharyngeal packing (HP) is used in nasal and oral surgeries after orotracheal intubation to keep blood from being swallowed during surgery, avoiding its emetic potential in the aerodigestive tract. Some authors suggest, however, that the HP could increase postoperative pain [8] and also that there is a possibility of aspiration of an accidentally forgotten packing [9]. Besides, previous studies were unable to show efficacy of HP in preventing PONV in nasal surgeries in adults [10,11,12,13]. Despite these evidences, HP is a common practice during adenotonsillectomy in children, even with not a single paper evaluating its efficacy in reducing PONV in this scenario.
The objective of this study is to evaluate the effectiveness of the HP in the prevention of PONV in children who undergo adenotonsillectomy.
Materials and methods
We conducted a randomized, double-blinded, controlled trial to determine the effect of HP during tonsillectomy in children to reduce PONV. Patients from the pediatric otolaryngology clinic of our hospital aged between 4 and 16 years with indication of adenotonsillectomy due to adenotonsillar hyperplasia and associated symptoms of sleep-disordered breathing with or without tympanostomy tube insertion were selected. Patients who showed evidence of clinically significant hematopoietic, neurological, psychiatric, systemic disease or any remarkable history of gastrointestinal disorder were excluded from the study. The convenience sample was selected in a consecutive manner and was composed by children who met inclusion criteria and whose caregiver agreed with participation in the study. All caregivers signed an informed consent. The main investigator, patient/caregiver and nursing team were blinded for the intervention. A diary was provided to be filled out by parents/guardians every morning with regard to the variables of the study during the first 14 postoperative days.
For calculation of sample size, we accepted a type I error of 5% (α = 0.05) and a type II error of 20% (β = 0.20), setting a statistical power of 80 percent. Considering the incidence of PONV as being 30% [14,15,16] in the control group and 10% in the intervention group, and admitting a loss of 15%, we needed to enroll 71 patients for each group, with a total sample of 142 patients.
Patients who met the inclusion criteria were randomized into the two groups—intervention (HP) or control—using randomization.com website (https://www.randomization.com). General anesthesia was performed according to the protocol described in previous studies [17,18,19], without the use of pre-anesthetic midazolam. Patient remained in the company of one parent/guardian until inhalation induction was achieved. Intravenous propofol was administered at the time of induction. After parents left surgery room, the surgeon opened a sealed opaque envelope containing the randomization. Dexamethasone (0.5 mg/kg, until maximum dose of 4 mg) and ondansetron (0.15 mg/kg) were administered intravenously (IV) during anesthesia for antiemetic purposes to all patients. HP was made with two tied gauzes with a silk suture, wet in 0.9% saline solution. It was placed after exposure of the hypopharynx with a McIvor mouth gag and before incision. Adenoidectomy was performed using adenoid curettes and hemostasis was obtained with nasopharyngeal packing, used in both groups. Tonsillectomy was performed using cold dissection technique, and hemostasis was achieved by compression with moist gauze and/or absorbable sutures. After finishing the hemostasis and before extubation, nasopharyngeal and HP were gently removed. The main association (HP and PONV) was controlled by the following confounders: anesthesia and surgical duration (in minutes), number of suture in the tonsil bed, trans-operatory bleeding volume (as percentage of body total blood volume), use of nonsteroidal anti-inflammatory (ketorolac) during procedure and by the necessity of tympanostomy tube insertion.
During postoperative period in the hospital, rescue ondansetron IV was used if postoperative nausea and vomiting occurred. Vomiting was defined as the forceful expulsion of gastrointestinal contents from the mouth. These episodes were recorded by the nursing team and parents and registered in a standard way by a trained investigator, all blinded to the intervention. Analgesia with dipyrone and paracetamol was administered if necessary. Morphine IV was administered (until a maximum dose of 0.09 mg/kg) as a rescue treatment for pain if children presented strong pain with no response to the previous medications. The use of nonsteroidal anti-inflammatory drugs was avoided in the postoperative period. Intravenous fluids were continued until oral liquids were tolerated.
After hospital discharging, paracetamol and dipyrone drops were prescribed, every 6 h, in an intercalated way. It was recommended initially (first postoperative day) the diet to be liquid and soft, making it optional in subsequent days. Parents were instructed to complete the diary with information of occurrence of PONV, secondary bleeding (defined as the presence of flowing blood) and type of oral intake (liquid/soft or solid) in the first 14 postoperative days. The main investigator examined patients on the 7th and 14th postoperative days. Patients were advised to contact the investigator for evaluation of any postoperative complication. Data on PONV episodes, postoperative length of stay or secondary bleeding were collected from the hospital medical record and matched to the information from parents’ diary.
The main outcome was the occurrence of nausea and vomiting in the first 24 h after surgery. The occurrence of nausea and vomiting in the first seven postoperative days, the occurrence of postoperative bleeding until the 14th postoperative day, hospital discharge less than 24 h after surgery and number of days for recovering solid diet intake were considered as secondary outcomes.
The database was stored in the program SPSS version 22. Categorical data are shown by counting and percentage. Quantitative data are shown as mean, standard deviation, or median, minimum and maximum when asymmetry was present. The t test or non-parametric equivalent (Mann–Whitney) was used for comparing quantitative variables. Chi-square test or Fisher’s exact test was used for comparing categorical data. For binary outcomes, relative risk and its 95% confidence interval were calculated.
This study was submitted to and approved by the Research and Ethics Committee of Irmandade da Santa Casa de Misericórdia de Porto Alegre—ISCMPA, under number 12630013500005335, as recommended by the Brazilian National Health Council. The study was registered in the Brazilian Register of Randomized Trials (REBEC), under registry number RBR-3zjn27, Universal Trial Number U1111-1197-7461.
Results
On the basis of an interim analysis, a total of 129 patients were included in the study (Fig. 1). Table 1 shows the baseline characteristics of the patients after the randomization. There is no significant statistical difference between the two groups. Table 2 shows the surgery characteristics, which did not differ between the two groups. No significant statistical difference was found in the use of anesthetics between the two groups. Table 3 demonstrates the incidence of the primary outcomes and Table 4 the incidence of secondary outcomes between both groups, along with the relative risks and 95% confidence intervals. The use of HP did not significantly reduce the occurrence of PONV. The occurrence of postoperative bleeding and discharge with less than 24 h from surgery also did not differ between groups. The median time period for recovering solid oral intake after surgery was 4.0 days in both groups (range 4.0–14.0), with no significant difference between groups. None of the patients who presented postoperative bleeding required the return to operating room.
There was no higher incidence of nausea and vomiting in the subgroup submitted to adenotonsillectomy with tympanostomy tube insertion (36.4%) compared to those submitted only to adenotonsillectomy (46.1%) (P = 0.472). There was no retained forgotten packing in the study.
Discussion
Current clinical practice guidelines in the surgical management of the tonsils in children indicates the necessity to determine the cost-effectiveness (direct and indirect) of different tonsillectomy techniques [20], once reducing postoperative complications related to tonsillectomy technique may reduce delayed discharge and the need for readmission and re-intervention. The primary reasons for readmission or prolonged initial stay include pain, vomiting, fever, and tonsillar hemorrhage [21]. Together with strabismus surgery, adenotonsillectomy with or without tympanostomy tube insertion is one of the surgical procedures with higher incidence of PONV [5]. HP is frequently used in the prevention of PONV during ear, nose and throat surgeries for many years, despite the absence of any evidence of efficacy.
Our study analyzed the efficacy of HP during adenotonsillectomy in reducing the incidence of PONV. We could not show any statistical difference in the occurrence of PONV between the two comparison groups, a finding in accordance with previous studies addressing nasal surgery in adults [10,11,12,13, 22,23,24]. In the attempt to evaluate the role of swallowed blood in PONV, Jones et al. performed a randomized clinical trial investigating the effect of gastric aspiration in the prevention of PONV in children submitted for tonsillectomy. Here, also, there was no difference in the incidence of such complications between patients subjected and not subjected to postoperative gastric aspiration [25]. It is noteworthy that, in contrast to our study, adenotonsillectomy was performed using electrocautery and suction electrocautery technique in this study, which is known to reduce transoperatory bleeding, although with an increased in the postoperative pain [26].
Children can present nausea and vomiting after oral medication intake because of its undesirable taste. We chose to analyze the incidence of PONV only in the first 24 h as primary outcome due to the more accurate registration by the medical personal and the possible interference of oral analgesic intake after discharge. Nausea is a subjective symptom without any developed scale adapted to children under 9 years and it has different perceptions along different ages [27]. Emesis is the most common objective outcome used in pediatric nausea studies, but it may not correlate with the symptom of nausea [28]. Also, there is lack of validated scores to measure postoperative vomiting intensity in children in the available literature [29]. For those reasons, nausea was analyzed together and separated from vomiting in our study. Every child with referred nausea or presented vomiting received ondansetron IV for symptomatic relief. We considered hospital discharge after 24 h from surgery as a secondary outcome, because it could be in some way related to PONV, once these events in children are hardly treated with oral medication, frequently demanding prolonged hospital staying or readmission due the necessity of a venous route.
Eberhart et al. [5] identified four independent predictors of postoperative vomiting in children: duration of surgery > 30 min; age > 3 years; history of PONV in patient, parent, or sibling; and strabismus surgery. Based on the presence of 0, 1, 2, 3, and 4 factors, the risk of postoperative vomiting was 9, 10, 30, 55, and 70%, respectively. In our study, mean duration of surgery was prolonged, as most of our surgeons responsible for the procedure were residents. Even so, we could not find a higher incidence of PONV than that described in the literature [29]. The routine use of dexamethasone, ondansetron and propofol, as recommended by anesthesia guidelines [27] may have contributed to our reduction of PONV occurrence.
Literature shows conflicting evidence about postoperative sore throat when using HP [8, 10, 12, 22, 23], and one limitation of our study is the absence of analgesic use registration, including IV morphine. Post-tonsillectomy pain has a complex mechanism and several medications can be needed to obtain symptom relief. In children, its evaluation is dependent in different scales according to age [30]. Pain related to HP use has been suggested by previous studies in adults [12, 23], and possible higher opioid consumption could lead to increased PONV, advocating against the use of HP. In this scenario, there is lack of prospective studies evaluating the effect of IV morphine in the postoperative period of tonsillectomy in children when prophylactic antiemetic medication is used during anesthesia. The retrospective study of Anderson et al. suggest that, in the absence of use of prophylactic antiemetic medication during anesthesia, morphine doses lower than 0.1 mg/kg IV, as used in our study, have no association with increased PONV, but higher doses lead to increased postoperative vomiting [31]. More studies are necessary to investigate this association.
Unintentionally retained packs are considered as “Never Event”—medical errors believed to be preventable with appropriate measures [32]. Recent guidelines recommend that, when using HP, at least one visual aid and at least one documented piece of evidence should be undertaken [33]. Our investigation used a silk suture in the gauze packing to reduce the chance of this complication. None of these adverse events was related in our sample.
To exclude a type II error as a possible explanation of our main result, we calculated the statistical power of our study. We concluded that a much larger sample would be necessary to prove a statistical significant reduction in PONV with HP during adenotonsillectomy. It would be necessary to include a sample of nearly 4000 patients to get a significant result at a 5% level (P < 0.05). In this case, the number necessary to treat (NNT) of 35 could be too large to justify the routine use of HP during adenotonsillectomy in children to prevent PONV, if, as in our study, routine prophylactic antiemetic medication were used during anesthesia in the absence of individual factors for major bleeding.
Conclusion
These results suggest that there is no benefit in using HP during adenotonsillectomy in children in PONV prevention, when prophylactic antiemetic medication during anesthesia was used and in the absence of individual factors for major bleeding.
References
Parker NP, Walner DL (2011) Trends in the indications for pediatric tonsillectomy or adenotonsillectomy. Int J Pediatr Otorhinolaryngol 75(2):282–285
Ved SA, Walden TL, Montana J, Lea DE, Tefft MC, Kataria BK et al (1996) Vomiting and recovery after outpatient tonsillectomy and adenoidectomy in children. Comparison of four anesthetic techniques using nitrous oxide with halothane or propofol. Anesthesiology 85(1):4–10
Litman RS, Wu CL, Catanzaro FA (1994) Ondansetron decreases emesis after tonsillectomy in children. Anesth Analg 78(3):478–481
Ferrari LR, Donlon JV (1992) Metoclopramide reduces the incidence of vomiting after tonsillectomy in children. Anesth Analg 75(3):351–354
Eberhart LHJ, Geldner G, Kranke P, Morin AM, Schäuffelen A, Treiber H et al (2004) The development and validation of a risk score to predict the probability of postoperative vomiting in pediatric patients. Anesth Analg 99(6):1630–1637
Apfel CC, Läärä E, Koivuranta M, Greim CA, Roewer N (1999) A simplified risk score for predicting postoperative nausea and vomiting: conclusions from cross-validations between two centers. Anesthesiology 91(3):693–700
Watcha MF, White PF (1992) Postoperative nausea and vomiting: its etiology, treatment, and prevention. Anesthesiology 77(1):162–184
Marais J, Prescott RJ (1993) Throat pain and pharyngeal packing: a controlled randomized double-blind comparison between gauze and tampons. Clin Otolaryngol Allied Sci 18(5):426–429
Ozer C, Ozer F, Sener M, Yavuz H (2007) A forgotten gauze pack in the nasopharynx: an unfortunate complication of adenotonsillectomy. Am J Otolaryngol 28(3):191–193
Piltcher O, Lavinsky M, Lavinsky J, de Oliveira Basso PR (2007) Effectiveness of hypopharyngeal packing during nasal and sinus surgery in the prevention of PONV. Otolaryngol Head Neck Surg 137(4):552–554
Korkut AY, Erkalp K, Erden V, Teker AM, Demirel A, Gedikli O et al (2010) Effect of pharyngeal packing during nasal surgery on postoperative nausea and vomiting. Otolaryngol Head Neck Surg 143(6):831–836
Basha SI, McCoy E, Ullah R, Kinsella JB (2006) The efficacy of pharyngeal packing during routine nasal surgery—a prospective randomised controlled study. Anaesthesia 61(12):1161–1165
Fennessy BG, Mannion S, Kinsella JB, O’Sullivan P (2011) The benefits of hypopharyngeal packing in nasal surgery: a pilot study. Ir J Med Sci 180(1):181–183
Kearney R, Mack C, Entwistle L (1998) Withholding oral fluids from children undergoing day surgery reduces vomiting. Paediatr Anaesth 8(4):331–336
Kermode J, Walker S, Webb I (1995) Postoperative vomiting in children. Anaesth Intensive Care 23(2):196–199
Schreiner MS, Nicolson SC, Martin T, Whitney L (1992) Should children drink before discharge from day surgery? Anesthesiology 76(4):528–533
Miura MS, Saleh C, de Andrade M, Assmann M, Lima LH, Lubianca Neto JF (2009) Topical clindamycin in post-adenotonsillectomy analgesia in children: a double-blind, randomized clinical trial. Otolaryngol Head Neck Surg 141(4):509–515
Miura MS, Saleh C, de Andrade M, Assmann M, Ayres M, Lubianca Neto JF (2009) Topical sucralfate in post-adenotonsillectomy analgesia in children: a double-blind randomized clinical trial. Otolaryngol Head Neck Surg 141(3):322–328
Brum MR, Miura MS, de Castro SF, Machado GM, Lima LH, Lubianca Neto JF (2012) Tranexamic acid in adenotonsillectomy in children: a double-blind randomized clinical trial. Int J Pediatr Otorhinolaryngol 76(10):1401–1405
Baugh RF, Archer SM, Mitchell RB, Rosenfeld RM, Amin R, Burns JJ et al (2011) Clinical practice guideline: tonsillectomy in children. Otolaryngol Neck Surg 144(1):S1–30
Royal college of surgeons of England (2005) National prospective tonsillectomy audit final report
Meco BC, Ozcelik M, Yildirim Guclu C, Beton S, Islamoglu Y, Turgay A et al (2016) Does type of pharyngeal packing during sinonasal surgery have an effect on PONV and throat pain? Otolaryngol Head Neck Surg 154(4):742–747
Karbasforushan A, Hemmatpoor B, Makhsosi BR, Mahvar T, Golfam P, Khiabani B (2014) The effect of pharyngeal packing during nasal surgery on the incidence of post operative nausea, vomiting, and sore throat. Iran J Otorhinolaryngol 26(77):219–223
Green R, Konuthula N, Sobrero M, Saini A, Parasher A, Pool C et al (2017) Use of pharyngeal packs in functional endoscopic sinus surgery: a randomized controlled trial. Laryngoscope 127(11):2460–2465
Jones JE, Tabaee A, Glasgold R, Gomillion MC (2001) Efficacy of gastric aspiration in reducing posttonsillectomy vomiting. Arch Otolaryngol Head Neck Surg 127(8):980–984
Pinder DK, Wilson H, Hilton MP (2011) Dissection versus diathermy for tonsillectomy. Cochrane Database Syst Rev 16(3):CD02211
Gan TJ, Diemunsch P, Habib AS, Kovac A, Kranke P, Meyer TA et al (2014) Consensus guidelines for the management of postoperative nausea and vomiting. Anesth Analg 118(1):85–113
Stadler M, Bardiau F, Seidel L, Albert A, Boogaerts JG (2003) Difference in risk factors for postoperative nausea and vomiting. Anesthesiology 98(1):46–52
Bolton CM, Myles PS, Nolan T, Sterne JA (2006) Prophylaxis of postoperative vomiting in children undergoing tonsillectomy: a systematic review and meta-analysis. Br J Anaesth 97(5):593–604
Bieri D, Reeve RA, Champion GD, Addicoat L, Ziegler JB (1990) The Faces Pain Scale for the self-assessment of the severity of pain experienced by children: development, initial validation, and preliminary investigation for ratio scale properties. Pain 41(2):139–150
Anderson BJ, Ralph CJ, Stewart AW, Barber C, Holford NH (2000) The dose-effect relationship for morphine and vomiting after day-stay tonsillectomy in children. Anaesth Intensive Care 28(2):155–160
Moppett IK, Moppett SH (2016) Surgical caseload and the risk of surgical never events in England. Anaesthesia 71(1):17–30
Athanassoglou V, Patel A, McGuire B, Higgs A, Dover MS, Brennan PA et al (2018) Systematic review of benefits or harms of routine anaesthetist-inserted throat packs in adults: practice recommendations for inserting and counting throat packs: an evidence-based consensus statement by the Difficult Airway Society (DAS), the British association of oral and maxillofacial surgery (BAOMS) and the British association of otorhinolaryngology, head and neck surgery (ENT-UK). Anaesthesia 73(5):612–618
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No competing interests declared.
Ethical approval
This study was submitted to and approved by the Research and Ethics Committee of Irmandade da Santa Casa de Misericórdia de Porto Alegre, under number 12630013500005335, as recommended by the Brazilian National Health Council.
Informed consent
All caregivers signed an informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Oppermann, L.P., Lubianca Neto, J.F., Drummond, R.L. et al. Hypopharyngeal packing during adenotonsillectomy by cold dissection in children: a randomized controlled trial. Eur Arch Otorhinolaryngol 277, 2603–2609 (2020). https://doi.org/10.1007/s00405-020-06032-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-020-06032-5