Abstract
Objective
To develop clinical tools assessing the refluxogenic potential of foods and beverages (F&B) consumed by patients with laryngopharyngeal reflux (LPR).
Methods
European experts of the LPR Study group of the Young-Otolaryngologists of the International Federation of Oto-rhino-laryngological societies were invited to identify the components of Western European F&B that would be associated with the development of LPR. Based on the list generated by experts, four authors conducted a systematic review to identify the F&B involved in the development of esophageal sphincter and motility dysfunctions, both mechanisms involved in the development of gastroesophageal reflux disease and LPR. Regarding the F&B components and the characteristics identified as important in the development of reflux, experts developed three rational scores for the assessment of the refluxogenic potential of F&B, a dish, or the overall diet of the patient.
Results
Twenty-six European experts participated to the study and identified the following components of F&B as important in the development of LPR: pH; lipid, carbohydrate, protein composition; fiber composition of vegetables; alcohol degree; caffeine/theine composition; and high osmolality of beverage. A total of 72 relevant studies have contributed to identifying the Western European F&B that are highly susceptible to be involved in the development of reflux. The F&B characteristics were considered for developing a Refluxogenic Diet Score (REDS), allowing a categorization of F&B into five categories ranging from 1 (low refluxogenic F&B) to 5 (high refluxogenic F&B). From REDS, experts developed the Refluxogenic Score of a Dish (RESDI) and the Global Refluxogenic Diet Score (GRES), which allow the assessment of the refluxogenic potential of dish and the overall diet of the LPR patient, respectively.
Conclusion
REDS, RESDI and GRES are proposed as objective scores for assessing the refluxogenic potential of F&B composing a dish or the overall diet of LPR patients. Future studies are needed to study the correlation between these scores and the development of LPR according to impedance–pH study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laryngopharyngeal reflux (LPR) is an inflammatory condition of the upper aerodigestive tract tissues related to direct and indirect effect of gastric or duodenal content reflux, which induces morphological changes in the upper aerodigestive tract [1]. LPR symptoms concern 10–30% of patients visiting otolaryngological departments [2], and are associated with significant impairment of quality of life [3]. The etiopathological mechanisms underlying the development of LPR are poorly understood and would involve poor diet [4,5,6]; autonomic nerve dysfunction [7, 8]; lower (LES) and upper (UES) esophageal sphincter dysfunctions [9, 10]; and other unknown factors. The involvement of diet in the development of reflux has been mainly studied in patients with gastroesophageal reflux disease (GERD) through clinical and experimental studies. Overall, acid, fat, and low-protein foods, caffeine, alcohol and high-sugar beverages are suspected to be associated with impairments of the tonicity of LES (transient relaxation) or esophageal dysmotility, leading to abnormal acid exposure in the esophagus and GERD-related symptoms [11]. In otolaryngology, studies found that following a low-fat, high-protein and alkaline diet is associated with higher symptom resolution in patients with LPR symptoms or with recalcitrant symptoms to proton pump inhibitors (PPIs) [6, 12].
Currently, there is no tool that precisely assesses the refluxogenic potential of foods, beverages or the overall diet of reflux patients. Moreover, a significant proportion of otolaryngologists are still unaware about the foods and beverages (F&B) that the patient has to avoid [13]. The lack of a diet tool makes subjective and difficult both the physician’s judgment and the post-treatment assessment of the respect of anti-reflux diet. Such tool could undeniably contribute to improve the management of LPR patients through a better identification of the diet factors that would be associated with LPR; providing more objective information to LPR patients.
The LPR Study Group of Young-Otolaryngologists of Otorhinolaryngological Societies (YO-IFOS) is composed of international experts in the management of LPR. The aim of this study is to develop clinical tools assessing the refluxogenic potential of foods, beverages, and overall diet of patients with LPR.
Materials and methods
This study was realized following three steps:
- 1.
The establishment of components of F&B that may be involved in the development of reflux (panel of experts and survey).
- 2.
The realization of a systematic review about the impact of diet on reflux. On one hand, the review considered the studies investigating the impact of diet on clinical findings of LPR. On the other hand, the review considered the studies describing the role of foods, beverages (and their related components) in the development of reflux.
- 3.
The establishment of Refluxogenic Diet Scores.
Panel selection and survey
Panel selection
Experts in LPR came from the LPR Study Group of YO-IFOS, which coordinates many studies on reflux. Initially, the research committee of YO-IFOS identified experts if they were actively working on LPR over the past few years. Since the diet is strongly related to the world area, we only considered European experts to establish scores considering Western European F&B.
Survey
A modified Delphi technique [14] was used, asking experts to review and rate a list of potential components of F&B that may be involved in the dysfunction of esophageal sphincters and motility. This survey was conducted through Survey Monkey (San Mateo, CA, USA), allowing each participant to complete the survey only once each. The survey itself was developed in iterative fashion, with drafts revised by three certified otolaryngologists and one dietician.
Systematic review
Based on the list generated by experts, four authors conducted the systematic review through Google Scholar, PubMed, and Scopus search to identify the potential foods, beverages, and their related components that may be involved in the development of esophageal sphincter and motility dysfunctions. Studies that have evaluated the impact of diet on the clinical evolution of LPR were also identified. The diagnostic of GERD or LPR should be based on symptoms ± findings ± objective examination (pH monitoring). Studies investigating the impact of diet on healthy subjects were also considered. They selected studies that had database abstracts, available full texts, books or other works referring to the condition. In addition, references were obtained from citations within the retrieved articles.
Development of Refluxogenic Diet Scores
Based on the findings of the literature, the authors extracted the composition and the relevant characteristics of F&B from publications or scientific books. Four experts (2 otolaryngologists, 1 gastroenterologist, and 1 dietician) and one statistician developed a ‘refluxogenic coefficient of severity’ of the selected F&B, which served for the development of Refluxogenic Diet Scores.
Three diet scores has been developed for assessing (1) the refluxogenic potential of F&B (Refluxogenic Diet Score, REDS); (2) the Refluxogenic Score of a Dish (RESDI); and (3) the refluxogenic potential of the overall diet of the patient (Global Refluxogenic Score; GRES). Foods, beverages, and greasy substances were distinctly treated due to their different biochemical composition.
Results
Survey
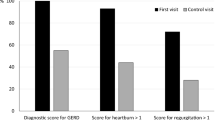
Twenty-six experts agreed to participate, coming from 10 countries (Belgium, France, Spain, Turkish, Italy, Poland, Greece, Luxembourg, Sweden, and Czech Republic) and 22 universities or hospitals. The mean years of practice of the panel was 17.6 ± 11.4 (range 1–36 years). The experts identified the following components of F&B as important in the development of reflux (> 50% converging opinion): alcohol degree; fat composition; pH; caffeine/theine composition; carbohydrate composition; the high osmolality of beverage (high-sugar beverages); protein composition; and water composition (Fig. 1).
Systematic review
According to the survey results, the following keywords were used for the review: “food(s)”, “beverage(s)”; “pH”; “acidity”; “alkaline”; “composition”; “lipid”; “carbohydrate”; “protein”; “caffeine”; “tea”; “sugar”; and “alcohol”.
A total of 708 relevant studies were identified. From them, 9 described the impact of diet on LPR disease (Table 1) [4, 5, 12, 15,16,17,18,19,20] and 63 focused on the relationship between the consumption of specific F&B and the development of esophageal dysmotility or sphincter dysfunctions or GERD-related symptoms or findings (i.e., esophagitis, hiatal hernia, etc.).
Two books of European dietician societies (Belgium: La Table de composition des Aliments and France: Ciqual) [21, 22] were used for the establishment of the composition (+ pH) of F&B. Figure 2 summarized the different steps of the study (chart flow). Figure 3 summarizes the diet characteristics associated with the development of reflux regarding the literature research.
Diet and LPR
A few studies specifically analyzed the impact of diet in LPR patients (Table 1). In the majority of studies, the anti-reflux diet is composed of alkaline diet/water and avoidance of fat, alcohol, and coffee/tea. The respect of anti-reflux diet is associated with better symptom improvement in LPR patients treated with PPIs in comparison with those treated with PPIs alone [5, 20]. Note that the effect of diet was assessed in association with some lifestyle changes, i.e., elevation of the head of the bed; avoidance of meal before sleep; and non-fasting eat in the majority of studies. The evidence level of studies is low and there is an important heterogeneity in the LPR diagnostic, content of diet and the outcomes used to assess the diet treatment efficacy [12]. The LPR diagnostic was based in pH monitoring in one study [12].
Fat foods
The majority of clinical and experimental studies showed that the fat foods, including chocolates, decrease the LES pressure and increase the esophageal acid exposure [21, 23,24,25,26]. In addition, fat foods would increase the sensitivity of the esophagus to acid exposure [11]. Two studies reported a positive association between the consumption of fat foods, GERD and the occurrence of esophagitis [27, 28]. The results of these studies are, however, balanced by other, which failed to find similar association [29, 30]. The refluxogenic potential of fat would be related to the slow gastric emptying time (related to the lipid digestion) leading to a higher number of transient relaxation of LES [31]. There are limited studies investigating the refluxogenic potential of chocolate. Two studies [25, 32] reported that the ingestion of chocolate syrup was associated with a decrease of LES pressure and a greater esophageal acid exposure time. In summary, fat foods may be considered as refluxogenic foods and have to be avoided by reflux patients.
High-osmolality beverages, coffee, and tea
High-osmolality beverages, such as sport beverages or fruit juices, are predictors of GERD symptoms [33,34,35]; while carbonated beverages decrease LES pressure [36]. Some studies supported that coffee (caffeine) ingestion induces heartburn in GERD patients [35, 37, 38], and decreases the LES pressure [39], while other did not find negative impact of coffee on esophageal function [40].
As for coffee, the majority of studies investigated the individual impact of tea in GERD, but not in LPR patients. The chronic consumption of tea increases the risk of erosive esophagitis [41], and GERD [34, 35, 38, 42,43,44,45]. Only Wei et al. did not corroborate these findings [46]. A recent meta-analysis investigating the association between the consumption of tea and the development of GERD reported that there will be several subgroups of tea drinkers; some developing GERD, other not [47]. In the same way, it has been supported that there are inter-individual differences in the caffeine (or theine) metabolisms, which may lead to controversial results. Thus, the gender [48] and the intake of contraceptives [49] are both factors modifying the metabolism of caffeine. In summary, coffee and tea are beverages that are still suspected to be associated with reflux.
Alcohol
The association between alcohol and LES dysfunction is not yet formally demonstrated regarding the studies that find significant association [41, 45, 50,51,52,53] and those that did not find such association [54,55,56,57]. However, regarding the systematic review of Kaltenbach et al., alcohol appears to worse the pH of gastric content, leading to GERD symptoms [11]. White wine would be worse than red wine, whereas beer would similarly lead to GERD symptoms than wine [58, 59]. Moreover, the alcohol intake would be associated with a reduced perception of esophageal acid reflux events [28]. Pathophysiologically, alcohol consumption may precipitate GERD by increasing acid secretion through gastrin stimulation, impairing LES pressure, esophageal motility and gastric emptying time [60]. Even a moderate consumption of alcohol would be associated with a decrease of esophageal pH in asymptomatic individuals with normal pH study measurements [61,62,63,64]. Although there are few controversial data, alcohol may be considered as risk factor of reflux.
Spicy and fried foods
Fried and spicy foods have been suggested as two of the most common precipitating factors of GERD symptoms and LES insufficiency [65,66,67]. Precisely, chilli causes reflux-associated symptoms, including heartburn, chest discomfort, nausea, belching, abdominal discomfort and distension [68, 69]. Regarding some reports, chilli and spicy foods do not affect the overall esophageal motility but only alter the LES tonicity [70,71,72].
Fruits and vegetables
Tomato, citrus fruits, onions and high-fiber vegetables are potential refluxogenic foods, involving many pathophysiological mechanisms such as increase of acidity or slow gastric emptying time (fiber composition) [54]. The consumption of tomato, or its based products [73] was higher in GERD patients than healthy controls [51, 74, 75]. Precisely, the two prominent organic acids present in tomato, i.e., citric and malic acids, are the most potent triggers of acid reflux in prone individuals and higher tomato consumers [76]. Citrus fruits are associated with the increase of heartburn [77, 78] and GERD [79], irrespective to the pH of citrus [37]. The high concentration of sugar in fruit juices consists of another component involved in the development of GERD [31]. Regarding the literature, onions may be a potent and long-lasting refluxogenic agent in heartburn patients [67], and may increase the number of reflux episodes and the esophageal acid exposure [67]. Similarly, mint is commonly thought to relax LES [11] although with controversial results [80].
Other foods and factors
Additional foods or beverages have been identified as risk factors of GERD or esophageal dysfunction, including rice cakes, ramen noodles, topokki, white bread, and extra-salt on regular meals [66, 81]. Sparkling beverages would be associated with GERD [5, 34, 82].
About the recommended foods, the high-protein foods would be associated with an increase of the LES tonicity, and may, therefore, be recommended [5, 12].
Refluxogenic Diet Scores
Refluxogenic Diet Score (REDS)
REDS was based on two subscores: the ‘pH score’ and the ‘composition score’.
The pH score has been created on the basis of a severity scale ranging from 0 (pH 10, very alkaline food/beverage) to 10 (pH 0, very acid food/beverage).
For each food, the experts identified protein, carbohydrate and lipid composition per 100 g. The ratio lipid/protein has been calculated for each food, leading to values ranging from 0 (very low-fat or very high-protein food) to 55 (very high-fat food); the latter being the food of our list with the maximal ratio value. Considering 0 as the minimal value and 55 as the maximal value, the authors transformed the values related to the ratio calculation to a composition score ranging from 0 to 10 (10 being the previous 55 value). At most the food is rich in lipids and poor in proteins, at the most its composition score will be closed from 10. The final REDS per food consisted of the multiplication of the pH score and the composition score. REDS was theoretically ranged from 0 to 100. From the REDS values, five categories of foods have been established ranging from ‘very low refluxogenic food’ to ‘very high refluxogenic food’ (Table 2).
According to the literature, experts proposed to consider additional elements that are not considered in the pH or the composition score for the classification of the foods: the origin of the food [6, 12]; the fiber content and the cooking of vegetables [5]; and the spicy or aromatic herb composition [65,66,67]. The dietician or the physician may upgrade the category of a food if it is composed of many conservative agents (industrial food), most of them being acidifying agents. The consumption of raw high-fiber vegetables would be associated with a slow rate of gastric emptying that leads to an increased number of transient relaxation of LES, justifying the upgrade of the category. Moreover, some fibers may be irritative for the digestive tract. Thus, the addition of spicy or aromatic herbs may also lead to an upgrade of the category. Table 3 describes the classification of foods into the five categories regarding the REDS values. Note that some greasy foods (oils) or spicy (herbs) are not water soluble and their acidity cannot be measured in terms of pH. They also did not contain enough proteins. For these reasons, they were classified on the basis of their refluxogenic potential regarding the literature.
Score for beverages
Since beverages are often not composed of fat (exception of milk), experts proposed to consider the pH as the main factor for the assessment of the refluxogenic potential of beverages (Table 2). Once the category is determined, regarding the literature findings, physician may upgrade the category score with regard to the glycemic index (which partly reflects the sugar concentration of the beverages; > 40 = upgrade); the alcohol degree (> 3% = upgrade), and the composition of caffeine or theine (upgrade). Sparkling beverages may also be upgraded. Coffee and tea without caffeine and theine may be downgraded. Table 3 summarizes the categories of beverages.
Absolute and average Refluxogenic Score of a Dish (RESDI)
Absolute RESDI consists of the addition of the categories of the F&B of a meal respecting the weight (quantity) of the foods/beverages (100 g of a food of category 5 + 200 g of a food of category 3: RESDI = (1 × 5) + (2 × 3) = 11). Absolute RESDI (abRESDI) considers the size of the dish because at most the patient eats a large amount of food, at most the absolute RESDI is high. Average RESDI (avRESDI) is the mean category of the dish (set at 100 g). Thus, avRESDI is the abRESDI divided by the foods/beverages quantity. An example of RESDI calculation is available in Fig. 4.
Global Refluxogenic Score (GRES)
GRES is dedicated to the assessment of the Global Refluxogenic Score of the daily life F&B consumed by the patient. Based on Tables 3 and 4, the patient selects the F&B that she/he have consumed over the previous 3 weeks and the physician may add the categories of the F&B to get a score. In case of daily consumption of a food, the physician has to multiply the category of the food by the number of day on which it was consumed. An example of GRES calculation is available in Fig. 4.
Discussion
Laryngopharyngeal reflux is a multifactorial disease in which anatomical and functional factors play a pathological role. The main pathophysiological mechanism consists of transient relaxations of LES and UES and the deposit of pepsin in the mucosa of the upper aerodigestive tract [83, 84]. The tonicity of LES and UES depends on many factors, including autonomic nerve function, mechanical factors, intrinsic factors and diet [85, 86]. In this study, based on evidences of the literature and expert opinion, we developed a clinical score allowing the rating and the classification of F&B regarding their refluxogenic potentials. From this score (REDS), two additional scores were developed, evaluating the refluxogenic potential of both a dish and the overall diet of LPR patients.
The pH and the ratio lipid/protein are considered as the most important factors associated with reflux. The impact of acid F&B is easily understood. At most the food is acid, at the most the gastric content is acid, as well as the gaseous droplets of proximal reflux episodes that contain pepsin and other gastroduodenal enzymes. The acidic environment is important for the pepsin activity and its related mucosa toxicity [87]. This fact is supported by the studies conducting on LPR patients treated with alkaline diet [4,5,6, 12, 20]. As presumed by our experts and confirmed by the studies, fat food is associated with a higher risk of reflux through the longer slow gastric emptying time and the related number of LES(/UES) transient relaxations. For these reasons, REDS was mainly based on two parameters: pH and lipid/protein ratio; proteins strengthening the sphincter tonicity. However, as reported by Newberry and Lynch [88], there is little doubt over the impact of high-fat, low-protein, and acidic foods on the development of both GERD and LPR; although some investigations of the role of specific foods or beverages (separately considered) have reported controversial results.
The controversial results of these studies are probably related to inter-individual differences in the mucosa sensitivity, food/beverage component metabolism (caffeine, etc.) and other unknown environmental factors. First, the esophageal mucosa sensitivity to acid food may vary from one patient to another and would depend on the composition of food. Thus, Shapiro et al. observed that the alcohol intake was associated with a reduced perception of esophageal acid reflux events in some patients [28]. The reduction of the perception of esophageal acid reflux events could be an important factor, biasing the clinical assessment of some patients in the detection of reflux and leading to unclear conclusions. As found for caffeine, the metabolism of some refluxogenic molecules would be different from one patient to another [48, 49], being an additional factor that could explain the controversial results of many studies. The origin of food is probably an environmental factor associated with a higher risk of reflux. This finding has been reported by the works of Koufman [6, 12] who stated that the industrial foods are often more acidic than the organic (bio) foods regarding the acidic potential of artificial preservative of the industrial foods (named E200 to E297). These findings are strengthened by the authors who reported that the consumption of Mediterranean fresh products may be associated with a decreased risk of GERD [89]. Among the F&B of the same family, some component differences may exist, yielding to different impacts on the gastroesophageal function. This is the case for tea according to our pH analysis, which reported that, among the various types of tea, some has a low pH (blackberry tea) whereas other has neutral pH (green tea). Interestingly, the meta-analysis of Cao et al., who investigated the association between the consumption of tea and the development of GERD, showed that there are several subgroups of tea drinkers, some developing GERD and some other not [47]. Additionally to individual factors, the conclusion of this meta-analysis may highlight these component differences. If the pH or the food composition does not significantly change regarding the cooking, the cooking process may, however, have an impact on the fiber composition of many high-fiber vegetables (onions, shallots, etc.), which are more digestible. This point has been considered in REDS. A meal-related factor that would be involved in both GERD and LPR patients is the size of the meals [90]. Thus, a strength of RESDI and GRES is the consideration of the quantity of the F&B consumed during the meal and over the previous 3 weeks, respectively.
According to the above-mentioned factors, and because reflux results from the concurrence of many F&B, the experts of YO-IFOS want to emphasize about the importance to consider the diet in a holistic way, which may decrease the potential impact of the individual differences.
In this study, many additional factors that may be involved in the development of reflux, i.e., tobacco [39, 54, 72,73,74, 91,92,93] or exercise [94], has not been considered because our objective was to develop specifically diet scores. Other factors are still poorly investigated in LPR such as the heredity, which accounts for 31–43% of the likelihood of GERD [95, 96], whereas some GERD recommendations could be less important for LPR patients without GERD at the MII-pH [or without temporary pro-GERD habits (Ramadan, etc.)], such as avoidance meals before sleep and the elevation of the head of the bed. Indeed, in LPR, there are less evidences about the usefulness of the elevation of the head of the bed because the majority of reflux episodes occur daytime and upright [3]. Future studies are needed to specifically investigate the impact of these recommendations in LPR patients in comparison with GERD patients.
The main theoretical weakness of these scores is the time to calculate each of them. For this reason, our team, which owns the intellectual properties of these scores, is developing a mobile phone application for the calculations of REDS, GRES, and RESDI.
Conclusion and perspectives
The development of clinical tools assessing the refluxogenic potential of the diet of the LPR patients makes sense for improving the reflux management and opens up some opportunities for nonpharmacologic interventions in patients with mild LPR. The three scores developed in the present study are still theoretical and need future studies to be validated or correlated with impedance–pH monitoring or esophageal manometry findings. These studies should consider GERD, LPR patients and healthy individuals. The healthy population is particularly important for the establishment of pathological thresholds or categories for GRES. Since some pathophysiological differences exist between GERD and LPR, the consideration of these populations in a different way is important. The development of similar food and beverage categories is required for the use of REDS, RESDI and GRES in the other world regions which are characterized by local and specific diet.
References
Lechien JR, Akst LM, Hamdan AL et al (2019) Evaluation and management of laryngopharyngeal reflux disease: state of the art review. Otolaryngol Neck Surg Off J Am Acad Otolaryngol Head Neck Surg 160(5):762–782. https://doi.org/10.1177/0194599819827488
Koufman JA (1991) The otolaryngologic manifestations of gastroesophageal reflux disease (GERD): a clinical investigation of 225 patients using ambulatory 24-hour pH monitoring and an experimental investigation of the role of acid and pepsin in the development of laryngeal injury. Laryngoscope 101(4 Pt 2 Suppl 53):1–78
Lechien JR, Bobin F, Muls V et al (2019) Validity and reliability of the reflux symptom score. Laryngoscope. https://doi.org/10.1002/lary.28017
Zalvan CH, Hu S, Greenberg B, Geliebter J (2017) A comparison of alkaline water and Mediterranean diet vs proton pump inhibition for treatment of laryngopharyngeal reflux. JAMA Otolaryngol Neck Surg 143(10):1023. https://doi.org/10.1001/jamaoto.2017.1454
Lechien JR, Huet K, Khalife M et al (2019) Alkaline, protein, low-fat and low-acid diet in laryngopharyngeal reflux disease: our experience on 65 patients. Clin Otolaryngol Off J ENT-UK Off J Neth Soc Oto-Rhino-Laryngol Cervico-Facial Surg 44(3):379–384. https://doi.org/10.1111/coa.13269
Koufman JA, Johnston N (2012) Potential benefits of pH 8.8 alkaline drinking water as an adjunct in the treatment of reflux disease. Ann Otol Rhinol Laryngol 121(7):431–434. https://doi.org/10.1177/000348941212100702
Wang AM, Wang G, Huang N et al (2019) Association between laryngopharyngeal reflux disease and autonomic nerve dysfunction. Eur Arch Oto-Rhino-Laryngol Off J Eur Fed Oto-Rhino-Laryngol Soc EUFOS Affil Ger Soc Oto-Rhino-Laryngol Neck Surg 276(8):2283–2287. https://doi.org/10.1007/s00405-019-05482-w
Lechien JR, Nandhan Sampath Kumar R, Chiesa-Estomba CM (2019) Laryngopharyngeal reflux and autonomic nerve dysfunction: what about stress? Eur Arch Oto-Rhino-Laryngol Off J Eur Fed Oto-Rhino-Laryngol Soc EUFOS Affil Ger Soc Oto-Rhino-Laryngol Neck Surg. https://doi.org/10.1007/s00405-019-05567-6
Ding H, Duan Z, Yang D et al (2017) High-resolution manometry in patients with and without globus pharyngeus and/or symptoms of laryngopharyngeal reflux. BMC Gastroenterol 17(1):109. https://doi.org/10.1186/s12876-017-0666-x
Passaretti S, Mazzoleni G, Vailati C, Testoni PA (2016) Oropharyngeal acid reflux and motility abnormalities of the proximal esophagus. World J Gastroenterol 22(40):8991–8998. https://doi.org/10.3748/wjg.v22.i40.8991
Kaltenbach T, Crockett S, Gerson LB (2006) Are lifestyle measures effective in patients with gastroesophageal reflux disease? An evidence-based approach. Arch Intern Med 166(9):965–971. https://doi.org/10.1001/archinte.166.9.965
Koufman JA (2011) Low-acid diet for recalcitrant laryngopharyngeal reflux: Therapeutic benefits and their implications. Ann Otol Rhinol Laryngol 120(5):281–287. https://doi.org/10.1177/000348941112000501
Lechien JR, Mouawad F, Mortuaire G et al (2019) Awareness of European Otolaryngologists and General Practitioners toward laryngopharyngeal reflux. Ann Otol Rhinol Laryngol. https://doi.org/10.1177/0003489419858090
Fackrell K, Smith H, Colley V et al (2017) Core outcome domains for early phase clinical trials of sound-, psychology-, and pharmacology-based interventions to manage chronic subjective tinnitus in adults: the COMIT’ID study protocol for using a Delphi process and face-to-face meetings to establish consensus. Trials 18(1):388. https://doi.org/10.1186/s13063-017-2123-0
Giacchi RJ, Sullivan D, Rothstein SG (2000) Compliance with anti-reflux therapy in patients with otolaryngologic manifestations of gastroesophageal reflux disease. Laryngoscope 110(1):19–22. https://doi.org/10.1097/00005537-200001000-00004
Siupsinskiene N, Adamonis K (2003) Diagnostic test with omeprazole in patients with posterior laryngitis. Med Kaunas Lith 39(1):47–55
Hamdan A, Nassar J, Dowli A, Al Zaghal Z, Sabri A (2012) Effect of fasting on laryngopharyngeal reflux disease in male subjects. Eur Arch Oto-Rhino-Laryngol Off J Eur Fed Oto-Rhino-Laryngol Soc EUFOS Affil Ger Soc Oto-Rhino-Laryngol Neck Surg 269(11):2361–2366. https://doi.org/10.1007/s00405-012-2038-z
Chappity P, Kumar R, Deka RC, Chokkalingam V, Saraya A, Sikka K (2014) Proton pump inhibitors versus solitary lifestyle modification in management of laryngopharyngeal reflux and evaluating who is at risk: scenario in a developing country. Clin Med Insights Ear Nose Throat 7:1–5. https://doi.org/10.4137/CMENT.S13799
Nanda MS (2016) Role of adjuvant lifestyle modifications in patients with laryngopharyngeal reflux disease in Hilly. Int J Sci Study 3(10):6
Yang J, Dehom S, Sanders S, Murry T, Krishna P, Crawley BK (2018) Treating laryngopharyngeal reflux: evaluation of an anti-reflux program with comparison to medications. Am J Otolaryngol 39(1):50–55. https://doi.org/10.1016/j.amjoto.2017.10.014
Ciqual Table de composition nutritionnelle des aliments. https://ciqual.anses.fr/. Accessed 30 July 2019
Amazon.fr, Table de composition des aliments, Etude Nutrinet Santé, Belgium. https://www.amazon.fr/Table-composition-aliments-Etude-Nutrinet/dp/2717865373/ref=sr_1_1?hvadid=80814136925022&hvbmt=be&hvdev=c&hvqmt=e&keywords=table+de+composition+des+aliments&qid=1564494275&s=gateway&sr=8-1. Accessed 30 July 2019
Becker DJ, Sinclair J, Castell DO, Wu WC (1989) A comparison of high and low fat meals on postprandial esophageal acid exposure. Am J Gastroenterol 84(7):782–786
Hills JM, Aaronson PI (1991) The mechanism of action of peppermint oil on gastrointestinal smooth muscle. An analysis using patch clamp electrophysiology and isolated tissue pharmacology in rabbit and guinea pig. Gastroenterology 101(1):55–65. https://doi.org/10.1016/0016-5085(91)90459-x
Murphy DW, Castell DO (1988) Chocolate and heartburn: Evidence of increased esophageal acid exposure after chocolate ingestion. Am J Gastroenterol 83(6):633–636
Nebel OT, Castell DO (1972) Lower esophageal sphincter pressure changes after food ingestion. Gastroenterology 63(5):778–783
El-Serag HB, Satia JA, Rabeneck L (2005) Dietary intake and the risk of gastro-oesophageal reflux disease: a cross sectional study in volunteers. Gut 54(1):11–17. https://doi.org/10.1136/gut.2004.040337
Shapiro M, Green C, Bautista JM et al (2007) Assessment of dietary nutrients that influence perception of intra-oesophageal acid reflux events in patients with gastro-oesophageal reflux disease. Aliment Pharmacol Ther 25(1):93–101. https://doi.org/10.1111/j.1365-2036.2006.03170.x
Pehl C, Waizenhoefer A, Wendl B, Schmidt T, Schepp W, Pfeiffer A (1999) Effect of low and high fat meals on lower esophageal sphincter motility and gastroesophageal reflux in healthy subjects. Am J Gastroenterol 94(5):1192–1196. https://doi.org/10.1111/j.1572-0241.1999.01064.x
Colombo P, Mangano M, Bianchi PA, Penagini R (2002) Effect of calories and fat on postprandial gastro-oesophageal reflux. Scand J Gastroenterol 37(1):3–5
Sutphen JL, Dillard VL (1989) Dietary caloric density and osmolality influence gastroesophageal reflux in infants. Gastroenterology 97(3):601–604. https://doi.org/10.5555/uri:pii:0016508589906306
Wright LE, Castell DO (1975) The adverse effect of chocolate on lower esophageal sphincter pressure. Am J Dig Dis 20(8):703–707
Fass R, Quan SF, O’Connor GT, Ervin A, Iber C (2005) Predictors of heartburn during sleep in a large prospective cohort study. Chest 127(5):1658–1666. https://doi.org/10.1378/chest.127.5.1658
Alrashed AA, Aljammaz KI, Pathan A et al (2019) Prevalence and risk factors of gastroesophageal reflux disease among Shaqra University students, Saudi Arabia. J Fam Med Prim Care 8(2):462–467. https://doi.org/10.4103/jfmpc.jfmpc_443_18
Arivan R, Deepanjali S (2018) Prevalence and risk factors of gastro-esophageal reflux disease among undergraduate medical students from a southern Indian medical school: a cross-sectional study. BMC Res Notes 11(1):448. https://doi.org/10.1186/s13104-018-3569-1
Hamoui N, Lord RV, Hagen JA, Theisen J, Demeester TR, Crookes PF (2006) Response of the lower esophageal sphincter to gastric distention by carbonated beverages. J Gastrointest Surg Off J Soc Surg Aliment Tract 10(6):870–877. https://doi.org/10.1016/j.gassur.2005.11.010
Price SF, Smithson KW, Castell DO (1978) Food sensitivity in reflux esophagitis. Gastroenterology 75(2):240–243
Vossoughinia H, Salari M, Mokhtari Amirmajdi E et al (2014) An epidemiological study of gastroesophageal reflux disease and related risk factors in urban population of Mashhad, Iran. Iran Red Crescent Med J 16(12):e15832. https://doi.org/10.5812/ircmj.15832
Thomas FB, Steinbaugh JT, Fromkes JJ, Mekhjian HS, Caldwell JH (1980) Inhibitory effect of coffee on lower esophageal sphincter pressure. Gastroenterology 79(6):1262–1266
Boekema PJ, Samsom M, Smout AJ (1999) Effect of coffee on gastro-oesophageal reflux in patients with reflux disease and healthy controls. Eur J Gastroenterol Hepatol 11(11):1271–1276
Chang C-H, Wu C-P, Wang J-D et al (2017) Alcohol and tea consumption are associated with asymptomatic erosive esophagitis in Taiwanese men. PLoS ONE 12(3):e0173230. https://doi.org/10.1371/journal.pone.0173230
Jarosz M, Taraszewska A (2014) Risk factors for gastroesophageal reflux disease: The role of diet. Przeglad Gastroenterol 9(5):297–301. https://doi.org/10.5114/pg.2014.46166
Lee S-W, Lee T-Y, Lien H-C, Yeh H-Z, Chang C-S, Ko C-W (2014) The risk factors and quality of life in patients with overlapping functional dyspepsia or peptic ulcer disease with gastroesophageal reflux disease. Gut Liver 8(2):160–164. https://doi.org/10.5009/gnl.2014.8.2.160
Lee S-W, Lee T-Y, Lien H-C, Yeh H-Z, Chang C-S, Ko C-W (2013) Comparison of risk factors and disease severity between old and young patients with gastroesophageal reflux disease. Gastroenterol Res 6(3):91–94. https://doi.org/10.4021/gr549w
Niu C-Y, Zhou Y-L, Yan R et al (2012) Incidence of gastroesophageal reflux disease in Uygur and Han Chinese adults in Urumqi. World J Gastroenterol 18(48):7333–7340. https://doi.org/10.3748/wjg.v18.i48.7333
Wei T-Y, Hsueh P-H, Wen S-H, Chen C-L, Wang C-C (2019) The role of tea and coffee in the development of gastroesophageal reflux disease. Ci Ji Yi Xue Za Zhi Tzu-Chi Med J 31(3):169–176. https://doi.org/10.4103/tcmj.tcmj_48_18
Cao H, Huang X, Zhi X, Han C, Li L, Li Y (2019) Association between tea consumption and gastroesophageal reflux disease: a meta-analysis. Medicine (Baltimore) 98(4):e14173. https://doi.org/10.1097/MD.0000000000014173
Pollock BG, Wylie M, Stack JA et al (1999) Inhibition of caffeine metabolism by estrogen replacement therapy in postmenopausal women. J Clin Pharmacol 39(9):936–940
Abernethy DR, Todd EL (1985) Impairment of caffeine clearance by chronic use of low-dose oestrogen-containing oral contraceptives. Eur J Clin Pharmacol 28(4):425–428
Mohammed I, Nightingale P, Trudgill NJ (2005) Risk factors for gastro-oesophageal reflux disease symptoms: a community study. Aliment Pharmacol Ther 21(7):821–827. https://doi.org/10.1111/j.1365-2036.2005.02426.x
Wang J-H, Luo J-Y, Dong L, Gong J, Tong M (2004) Epidemiology of gastroesophageal reflux disease: a general population-based study in Xi’an of Northwest China. World J Gastroenterol 10(11):1647–1651. https://doi.org/10.3748/wjg.v10.i11.1647
O’Leary C, McCarthy J, Humphries M, Shanahan F, Quigley E (2003) The prophylactic use of a proton pump inhibitor before food and alcohol. Aliment Pharmacol Ther 17(5):683–686
Rosaida MS, Goh K-L (2004) Gastro-oesophageal reflux disease, reflux oesophagitis and non-erosive reflux disease in a multiracial Asian population: a prospective, endoscopy based study. Eur J Gastroenterol Hepatol 16(5):495–501
Nilsson M, Johnsen R, Ye W, Hveem K, Lagergren J (2004) Lifestyle related risk factors in the aetiology of gastro-oesophageal reflux. Gut 53(12):1730–1735. https://doi.org/10.1136/gut.2004.043265
Nilsson M, Johnsen R, Ye W, Hveem K, Lagergren J (2004) Prevalence of gastro-oesophageal reflux symptoms and the influence of age and sex. Scand J Gastroenterol 39(11):1040–1045. https://doi.org/10.1080/00365520410003498
Stanghellini V (1999) Relationship between upper gastrointestinal symptoms and lifestyle, psychosocial factors and comorbidity in the general population: results from the Domestic/International Gastroenterology Surveillance Study (DIGEST). Scand J Gastroenterol Suppl 231:29–37
Talley NJ, Zinsmeister AR, Schleck CD, Melton LJ (1994) Smoking, alcohol, and analgesics in dyspepsia and among dyspepsia subgroups: lack of an association in a community. Gut 35(5):619–624. https://doi.org/10.1136/gut.35.5.619
Pehl C, Wendl B, Pfeiffer A (2006) White wine and beer induce gastro-oesophageal reflux in patients with reflux disease. Aliment Pharmacol Ther 23(11):1581–1586. https://doi.org/10.1111/j.1365-2036.2006.02922.x
Pehl C, Pfeiffer A, Wendl B, Kaess H (1998) Different effects of white and red wine on lower esophageal sphincter pressure and gastroesophageal reflux. Scand J Gastroenterol 33(2):118–122
Bujanda L (2000) The effects of alcohol consumption upon the gastrointestinal tract. Am J Gastroenterol 95(12):3374–3382. https://doi.org/10.1111/j.1572-0241.2000.03347.x
Kaufman SE, Kaye MD (1978) Induction of gastro-oesophageal reflux by alcohol. Gut 19(4):336–338. https://doi.org/10.1136/gut.19.4.336
Vitale GC, Cheadle WG, Patel B, Sadek SA, Michel ME, Cuschieri A (1987) The effect of alcohol on nocturnal gastroesophageal reflux. JAMA 258(15):2077–2079
Rubinstein E, Hauge C, Sommer P, Mortensen T (1993) Oesophageal and gastric potential difference and pH in healthy volunteers following intake of coca-cola, red wine, and alcohol. Pharmacol Toxicol 72(1):61–65
Grande L, Manterola C, Ros E, Lacima G, Pera C (1997) Effects of red wine on 24-hour esophageal pH and pressures in healthy volunteers. Dig Dis Sci 42(6):1189–1193. https://doi.org/10.1023/a:1018893721735
Nebel OT, Fornes MF, Castell DO (1976) Symptomatic gastroesophageal reflux: Incidence and precipitating factors. Am J Dig Dis 21(11):953–956
Choe JW, Joo MK, Kim HJ et al (2017) Foods inducing typical gastroesophageal reflux disease symptoms in Korea. J Neurogastroenterol Motil 23(3):363–369. https://doi.org/10.5056/jnm16122
Allen ML, Mellow MH, Robinson MG, Orr WC (1990) The effect of raw onions on acid reflux and reflux symptoms. Am J Gastroenterol 85(4):377–380
Kang JY, Tay HH, Guan R (1992) Chronic upper abdominal pain: site and radiation in various structural and functional disorders and the effect of various foods. Gut 33(6):743–748. https://doi.org/10.1136/gut.33.6.743
Lim LG, Tay H, Ho KY (2011) Curry induces acid reflux and symptoms in gastroesophageal reflux disease. Dig Dis Sci 56(12):3546–3550. https://doi.org/10.1007/s10620-011-1799-3
Yeoh KG, Ho KY, Guan R, Kang JY (1995) How does chili cause upper gastrointestinal symptoms? A correlation study with esophageal mucosal sensitivity and esophageal motility. J Clin Gastroenterol 21(2):87–90
Milke P, Diaz A, Valdovinos MA, Moran S (2006) Gastroesophageal reflux in healthy subjects induced by two different species of chilli (Capsicum annum). Dig Dis 24(1–2):184–188. https://doi.org/10.1159/000090323
Alsulobi AM, El-Fetoh NMA, Alenezi SGE et al (2017) Gastroesophageal reflux disease among population of Arar City. North Saudi Arabia Electron Physician 9(10):5499–5505. https://doi.org/10.19082/5499
Kubo A, Block G, Quesenberry CP, Buffler P, Corley DA (2014) Dietary guideline adherence for gastroesophageal reflux disease. BMC Gastroenterol 14:144. https://doi.org/10.1186/1471-230X-14-144
Richter JE (2000) Gastroesophageal reflux disease in the older patient: Presentation, treatment, and complications. Am J Gastroenterol 95(2):368–373. https://doi.org/10.1111/j.1572-0241.2000.t01-1-01791.x
de Bortoli N, Guidi G, Martinucci I et al (2016) Voluntary and controlled weight loss can reduce symptoms and proton pump inhibitor use and dosage in patients with gastroesophageal reflux disease: a comparative study. Dis Esophagus Off J Int Soc Dis Esophagus 29(2):197–204. https://doi.org/10.1111/dote.12319
Saleh K, Eid R, Haddad FG, Khalife-Saleh N, Kourie HR (2018) New developments in the management of head and neck cancer—impact of pembrolizumab. Ther Clin Risk Manag 14:295–303. https://doi.org/10.2147/TCRM.S125059
López-Colombo A, Pacio-Quiterio MS, Jesús-Mejenes LY et al (2017) Risk factors associated with gastroesophageal reflux disease relapse in primary care patients successfully treated with a proton pump inhibitor. Rev Gastroenterol Mex 82(2):106–114. https://doi.org/10.1016/j.rgmx.2016.09.001
Feldman M, Barnett C (1995) Relationships between the acidity and osmolality of popular beverages and reported postprandial heartburn. Gastroenterology 108(1):125–131. https://doi.org/10.1016/0016-5085(95)90016-0
Eslami O, Shahraki M, Bahari A, Shahraki T (2017) Dietary habits and obesity indices in patients with gastro-esophageal reflux disease: a comparative cross-sectional study. BMC Gastroenterol 17(1):132. https://doi.org/10.1186/s12876-017-0699-1
Bulat R, Fachnie E, Chauhan U, Chen Y, Tougas G (1999) Lack of effect of spearmint on lower oesophageal sphincter function and acid reflux in healthy volunteers. Aliment Pharmacol Ther 13(6):805–812
Yadegarfar G, Momenyan S, Khoobi M et al (2018) Iranian lifestyle factors affecting reflux disease among healthy people in Qom. Electron Physician 10(4):6718–6724. https://doi.org/10.19082/6718
Artanti D, Hegar B, Kaswandani N et al (2019) The gastroesophageal reflux disease questionnaire in adolescents: what is the best cutoff score? Pediatr Gastroenterol Hepatol Nutr 22(4):341–349. https://doi.org/10.5223/pghn.2019.22.4.341
Rees LEN, Pazmany L, Gutowska-Owsiak D et al (2008) The mucosal immune response to laryngopharyngeal reflux. Am J Respir Crit Care Med 177(11):1187–1193. https://doi.org/10.1164/rccm.200706-895OC
Johnston N, Dettmar PW, Strugala V, Allen JE, Chan WW (2013) Laryngopharyngeal reflux and GERD. Ann N Y Acad Sci 1300:71–79. https://doi.org/10.1111/nyas.12237
Crookes PF (2006) Physiology of reflux disease: role of the lower esophageal sphincter. Surg Endosc 20(Suppl 2):S462–466. https://doi.org/10.1007/s00464-006-0039-y
Sidhu AS, Triadafilopoulos G (2008) Neuro-regulation of lower esophageal sphincter function as treatment for gastroesophageal reflux disease. World J Gastroenterol 14(7):985–990. https://doi.org/10.3748/wjg.14.985
Johnston N, Dettmar PW, Bishwokarma B, Lively MO, Koufman JA (2007) Activity/stability of human pepsin: implications for reflux attributed laryngeal disease. The Laryngoscope 117(6):1036–1039. https://doi.org/10.1097/MLG.0b013e31804154c3
Newberry C, Lynch K (2017) Can we use diet to effectively treat esophageal disease? A review of the current literature. Curr Gastroenterol Rep 19(8):38. https://doi.org/10.1007/s11894-017-0578-5
Mone I, Kraja B, Bregu A et al (2016) Adherence to a predominantly Mediterranean diet decreases the risk of gastroesophageal reflux disease: a cross-sectional study in a South Eastern European population. Dis Esophagus Off J Int Soc Dis Esophagus 29(7):794–800. https://doi.org/10.1111/dote.12384
Delgado-Aros S, Camilleri M, Cremonini F, Ferber I, Stephens D, Burton DD (2004) Contributions of gastric volumes and gastric emptying to meal size and postmeal symptoms in functional dyspepsia. Gastroenterology 127(6):1685–1694. https://doi.org/10.1053/j.gastro.2004.09.006
Watanabe Y, Fujiwara Y, Shiba M et al (2003) Cigarette smoking and alcohol consumption associated with gastro-oesophageal reflux disease in Japanese men. Scand J Gastroenterol 38(8):807–811
Tibbling L, Gibellino FM, Johansson KE (1995) Is mis-swallowing or smoking a cause of respiratory symptoms in patients with gastroesophageal reflux disease? Dysphagia 10(2):113–116
Chattopadhyay DK, Greaney MG, Irvin TT (1977) Effect of cigarette smoking on the lower oesophageal sphincter. Gut 18(10):833–835. https://doi.org/10.1136/gut.18.10.833
Pandolfino JE, Bianchi LK, Lee TJ, Hirano I, Kahrilas PJ (2004) Esophagogastric junction morphology predicts susceptibility to exercise-induced reflux. Am J Gastroenterol 99(8):1430–1436. https://doi.org/10.1111/j.1572-0241.2004.30515.x
Cameron AJ, Lagergren J, Henriksson C, Nyren O, Locke GR, Pedersen NL (2002) Gastroesophageal reflux disease in monozygotic and dizygotic twins. Gastroenterology 122(1):55–59. https://doi.org/10.1053/gast.2002.30301
Mohammed I, Cherkas LF, Riley SA, Spector TD, Trudgill NJ (2003) Genetic influences in gastro-oesophageal reflux disease: a twin study. Gut 52(8):1085–1089. https://doi.org/10.1136/gut.52.8.1085
Acknowledgements
Vesale Grant and IRIS-Recherche Grant for the studies conducted in Brussels over the last year; these studies allowing Dr. Jerome Lechien to propose this consensus paper (Dr. Jerome R. Lechien owns the intellectual properties of diet scores).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lechien, J.R., Bobin, F., Mouawad, F. et al. Development of scores assessing the refluxogenic potential of diet of patients with laryngopharyngeal reflux. Eur Arch Otorhinolaryngol 276, 3389–3404 (2019). https://doi.org/10.1007/s00405-019-05631-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-019-05631-1