Abstract
Objective
To report a simple and novel method for intra-operative planning of fibula free flap reconstruction by means of a balsa wood (BW) model.
Study design
Retrospective chart review.
Methods
Between 2010 and 2015, 29 patients underwent mandibular reconstruction by a BW osteotomy design in which a single BW beam (US$4) is cut into segments to match the plate. The segments are then assembled together in a three-dimensional (3D) fashion to conform to the contour of the defect and the angles of attachment. Osteotomies are then performed according to the BW segment lengths and angles. Outcomes were retrospectively analyzed for number of procedures, operative times, and complications between the balsa wood method and more standard techniques, e.g., conventional 3D models.
Results
The length of the average mandibular defect was 9.62 cm (4–19), and the mean number of fibula segments was 2.03 ± 0.92 (range 1–4). Only one case (3.4%) necessitated revision surgery. Three patients (10.3%) had minor complications. Comparison of the results of the 13 patients reconstructed solely by BW to the 16 reconstructed by both BW and a 3D-printed model revealed that the use of BW alone did not significantly alter the average number of segments [2.31 (BW) vs 1.69 (combined); P = 0.07] or ischemia time (173 min vs 171 min, respectively, P = 0.938).
Conclusion
The use of balsa wood as a model for intra-operative planning of fibula free flap osteotomies is an effective, inexpensive, and safe technique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fibula free flaps (FFF) are almost universally the first choice for mandibular bony reconstruction in patients with benign as well as malignant disease [1]. One of the most important aspects of composite mandibular defect reconstruction by means of FFF is the flexibility that is made possible by a reliable periosteal blood supply after osteotomy [2]. However, bone vascularization is compromised when there are multiple osteotomies, and, as such, the number of osteotomies should be kept to a minimum to preserve reliable segmental periosteal circulation [3, 4]. Towards this end, accurate planning is crucial for limiting the need for repeat intra-operative osteotomies.
Preoperative virtual surgical planning has refined mandible reconstruction with FFF through the introduction of patient-specific models, pre-bent plates, and osteotomy guides, decreasing both operative time and accuracy [5]. Unfortunately, this technique is still unaffordable and not feasible in many centers worldwide.
As a naturally occurring porous bio-composite, balsa wood (BW) offers salient mechanical and physical properties that have long been used in flying plane models [6]. Its cellular/porous microstructure enables its application in large deformations, and the fine composite nano-architecture of the wood cell material increases its specific strength and stiffness, producing a high specific energy dissipation capacity [7]. This easy-to-cut yet rigid material can imitate bone qualities.
We assessed the feasibility and ease of applying BW to create an intra-operative template for guiding FFF osteotomies. The aim of the current study is to objectively quantify the advantages of intra-operative use of BW as a mockup for a neo-mandible. In this study, BW has been used as a template for mandibular osteotomies prior to actual bone cuts. We hypothesized that this model will aid in planning osteotomies without increasing overall operative times.
Materials and methods
Study design and setting
After acquiring approval from the institutional review board (TLV-0254-16), we performed a retrospective chart review of all patients who underwent BW-assisted FFF mandible reconstruction at our institution. Patient, disease, and procedure-specific variables were recorded and analyzed.
BW beams are highly accessible for purchase and are found in numerous sizes that are usually a function of thickness (measured in millimetres), width and length, with an average price of US$3–4 for a single beam, depending on beam size. The BW beam size usually corresponds to an average fibula cross-sectional area of 75 ± 14 mm2 (mean ± standard deviation) [8], so that an 8 × 8 mm or a 9 × 9 mm (square profile) beam is usually the matching caliber. One beam is more than enough for a single procedure, and it is disposed of at the end of the operation. BW has the advantage of not requiring radio opaque marking and a surgical count, since it is processed on a side table. The BW segments are measured and cut ex-vivo and then attached to the recon plate. After achieving satisfactory alignment with the plate, the beams are finally replaced by the FFF segments. Preoperatively, the BW beam is sterilized by autoclaving at 121 °C for 20 min, as previously demonstrated in other types of wood [9]. After the mandibular resection has been carried out, the FFF is harvested and reconstructed in the following steps [10].
Pre-plating
Our operative technique involves the use of a standard 2.4 mm recon plate applied to the external surface of the mandible after it has been bent or modified as needed in cases for which a pre-bent plate is used to fit the resected segment. We use at least two and preferably three extra screw holes on each side of the resected segment. The mandibular resection is then completed after removal of the plate.
Template modeling
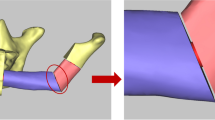
In this step (performed on a side table) a single beam of BW with roughly the same dimensions as the fibula is cut to fit the length of the resected fibular segment. The beam is then cut into separate segments to match the plate, with segments at least 1.5–2 cm in length to maintain the vascularity of each segment (as previously discussed elsewhere) [11]. The segments are then assembled together in a three-dimensional (3D) fashion to conform both to the contour of the defect and to the angles of attachment (Fig. 1). The BW segments are temporarily assembled together and fixed to the plate by means of operative needles to simulate the new mandible at the site of the defect (Fig. 2). After achieving satisfactory alignment, the segments are numbered on the superior part and marked with Xs or dots on the anterior aspect (through the screw holes) to denote the exact position of each segment (Fig. 3). At this point, the BW segments are disassembled and osteotomies are performed on the side table according to the BW segments’ lengths and angles (Fig. 4). The bone segments are assembled to the plate, mimicking the angles between the segments in all three axes and attached to the plate by means of screws. The plate with the FFF is now fixed in place and the microsurgical anastomoses are completed (Fig. 5).
Results
Between 2010 and 2015, 29 patients underwent mandibular reconstruction using the described BW technique. The average age of the patients was 52.5 ± 14.6 (range 5–73), the average length of the mandibular defect was 9.62 cm (4–19), and the mean ± standard deviation number of fibula segments was 2.03 ± 0.92 (range 1–4). Preoperative computer-aided 3D planning and printing using extrapolations from the noninvolved side in addition to the BW were performed in 16 of the patients. Comparison of the results of the 13 patients that were reconstructed solely with the aid of BW to the 16 that were reconstructed with both BW and the 3D model revealed that the use of BW alone did not significantly alter the average number of segments [2.31 (BW) vs 1.69 (combined); P = 0.07] or ischemia time [173 min vs 171 min, respectively, P = 0.938). Twenty-eight of the 29 (96.5%) flaps survived, and all osteotomy sites achieved solid bone union. There were no major complications, and the minor complications were fistula formation (n = 2; 6.9%) and fixation failure (n = 1; 3.4%). All 29 patients regained good function of the mandible without structural deformity or joint pain. Postoperative imaging studies demonstrated excellent precision and accuracy of flap positioning (Fig. 6).
Discussion
Conversion of a straight fibula bone flap into a parabolic mandible shape can be performed by means of various techniques, ranging from the use of the basic paper ruler cut to simulate the various segments through customized acrylic templates made from a 1:1 mandible computed tomography scan and pre-fabricated cutting guides [12]. One of the main disadvantages of using the paper ruler is the inability to create a 3D model that will allow the reconstructing surgeon to understand the complex angles between the various segments and to accurately simulate the rigid segments for precise alignment with the plate.
Previous studies conducted on customized acrylic templates have demonstrated that although osteotomy angles vary minimally (3–5%) during actual surgery, bone segment lengths can vary from 10 to 15%, thus suggesting that intra-operative modifications will be encountered even with the most advanced and accurate technology [12]. One classic scenario that changes the surgical plan is when the ablative surgeon decides to modify the resection margins due to disease advancement, positive margins, and/or intra-operative considerations. Any deviations made from the original surgical plan (more commonly encountered in malignancies) may necessitate modification of the pre-bent plate and, consequently, the intended cutting guide. Another drawback of virtual surgical planning is the increased time required to plan the reconstruction and create the models, possibly resulting in an undesirable delay in performing the surgery. Previous studies have shown that these efforts are worthwhile because of the improvements in reconstructive accuracy and surgical efficiency that result from the elimination of trial and error in bone flap-shaping [13]. In this study, the perioperative and long-term outcomes were equivalent for both of our study groups, notably, recipient-site infection, partial and total flap loss, and rate of soft-tissue and bony tissue revisions. The advantages of the BW model do not embody increased costs nor do they delay surgery.
On the same note, a recent published cost analysis has showed that when calculated as overall operating room and equipment costs, the use of preoperative surgical planning and intra-operative guides (including an acrylic model of the mandible), a preoperative planning session, and osteotomy guides resulted in reduced overall expenses compared to not using them [14]. However, based on data that revealed a very high price tag for this technology (US$8200), it can safely be assumed that the economic drawback will prevent the widespread use of this expensive highly accurate technology, especially if these aids are not covered by patients’ health plans and in countries where this technology is unavailable.
The BW model allows for precise contouring of the FFF. Since the classic maneuver of fitting the FFF to the plate has not yet became obsolete, the use of BW may significantly assist the reconstructing surgeon in adhering to the famous cliché of “measure twice, cut once”. It is especially valuable to the novice micro-surgeon who can plan the osteotomies while the fibula flap is still vascularized. Hence, the BW may assist in preventing redundant osteotomies and extended ischemia time. As mentioned before, this method is also practical in the event of major changes in the surgical plan that may have prevented the use of pre-fabricated cutting guides. Since the BW model is easily used and intuitively incorporated, this tool is a great addition to the reconstructing surgeon’s armamentarium.
Conclusion
The use of balsa wood as a model for intra-operative planning of fibula free flap osteotomies is an effective, inexpensive, and safe technique.
References
Monaco C et al (2016) Evolution of surgical techniques for mandibular reconstruction using free fibula flaps: the next generation. Head Neck 38:E2066–E2073
Wallace CG, Chang Y-M, Tsai C-Y, Wei F-C (2010) Harnessing the potential of the free fibula osteoseptocutaneous flap in mandible reconstruction. Plast Reconstr Surg 125:305–314
Strackee SD, Kroon F, Jaspers J, Bos KE (2001) Modeling a fibula transplant in mandibular reconstructions: evaluation of the effects of a minimal number of osteotomies on the contour of the jaw. Plast Reconstr Surg 108:1915–1921 (discussion 1922–191)
Kokosis G, Schmitz R, Powers DB, Erdmann D (2016) Mandibular reconstruction using the free vascularized fibula graft: an overview of different modifications. Arch Plast Surg 43:3
Chang EI, Jenkins MP, Patel SA, Topham NS (2016) Long-term operative outcomes of preoperative computed tomography-guided virtual surgical planning for osteocutaneous free flap mandible reconstruction. Plast Reconstr Surg 137:619–623. https://doi.org/10.1097/01.prs.0000475796.61855.a7
Zimmerman CH (1937) Preliminary tests in the NACA free-spinning wind tunnel. NACA Report 557
Vural M, Ravichandran G (2003) Dynamic response and energy dissipation characteristics of balsa wood: experiment and analysis. Int J Solids Struct 40:2147–2170
Sievänen H et al (1998) Peripheral quantitative computed tomography in human long bones: evaluation of in vitro and in vivo precision. J Bone Miner Res 13:871–882
Kallioinen A et al (2003) Effects of bacterial treatments on wood extractives. J Biotechnol 103:67–76
Moro A, Cannas R, Boniello R, Gasparini G, Pelo S (2009) Techniques on modeling the vascularized free fibula flap in mandibular reconstruction. J Craniofac Surg 20:1571–1573. https://doi.org/10.1097/SCS.0b013e3181b0db5c
Wang Y et al (2016) Mandibular reconstruction with the vascularized fibula flap: comparison of virtual planning surgery and conventional surgery. Int J Oral Maxillofac Surg 45(11):1400–1405. https://doi.org/10.1016/j.ijom.2016.06.015
Matros E, Santamaria E, Cordeiro PG (2013) Standardized templates for shaping the fibula free flap in mandible reconstruction. J Reconstr Microsurg 29:619–622. https://doi.org/10.1055/s-0033-1356645
Seruya M, Fisher M, Rodriguez ED (2013) Computer-assisted versus conventional free fibula flap technique for craniofacial reconstruction: an outcomes comparison. Plast Reconstr Surg 132:1219–1228. https://doi.org/10.1097/PRS.0b013e3182a3c0b1
Toto JM et al (2015) Improved operative efficiency of free fibula flap mandible reconstruction with patient-specific, computer-guided preoperative planning. Head Neck 37:1660–1664. https://doi.org/10.1002/hed.23815
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Ethical approval
The study was approved by the institutional ethics committee board (TLV-0254-16).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Horowitz, G., Warshavsky, A., Fridman, O. et al. Balsa wood for precise intra-operative bone contouring in fibula free-flap mandible reconstruction. Eur Arch Otorhinolaryngol 276, 2339–2343 (2019). https://doi.org/10.1007/s00405-019-05496-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-019-05496-4