Abstract
The purpose of the study was to compare the accuracy of computer-assisted surgery (CAS) and the traditional freehand technique for fibular free flap mandibular reconstruction as well as to evaluate the accuracy of the CAS planning. The medical records of 18 patients who underwent mandibular reconstruction with fibular free flap were reviewed. The CAS group (n = 7) benefited from virtual surgical planning and custom patient-specific plates and surgical cutting guides. The Control group (n = 11) was treated by conventional surgery. Morphometric comparison was done by calculating the differences in specific linear and angular parameters on pre- and postoperative CT-scans for both groups by using ProPlan CMF® software. Symmetry was also assessed by calculating the ratio of the affected versus the nonaffected side. In the CAS group, planned and postoperative CT-scans were compared to evaluate accuracy. The morphometric comparison showed no statistically significant differences between the groups except for the axial angle on the nonaffected side (mean difference 1.0° in the CAS group versus 2.9° in the Control group; p = 0.03). Ratios of the affected side over the nonaffected side showed no differences between the two groups. In the CAS group, the accuracy assessment showed a mean distance deviation of 2.3 mm for mandibular osteotomies and 1.9 mm for fibular osteotomies. Our results indicated that CAS and the conventional freehand techniques were comparable in their ability to provide a satisfactory morphological fibular free flap mandibular reconstruction. Moreover, the accuracy of the CAS technique was within the range reported in the literature.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Since the first report by Hidalgo in 1989, the fibula free flap procedure has rapidly become the gold standard in mandibular reconstruction [1]. However, the functional and cosmetic restoration of mandibular defects still remains challenging. The procedure entails the simultaneous management of insidious steps that are crucial for surgical success such as anatomical and symmetrical bone shaping, reestablishment of stable dental occlusion, and condylar repositioning into a centric relation [2–4].
The traditional method of mandibular reconstruction with freehand segmental osteotomies followed by fixation with either a reconstructive plate bent by hand intraoperatively or with multiple miniplates is being challenged by the recent advances in computer-assisted surgery (CAS), especially with regard to computer-aided design/computer-aided manufacturing (CAD/CAM) technology [5–11].
In recent years, this new approach has strongly contributed to a dramatic and global improvement in the strategy for reconstructive surgery of the craniofacial skeleton. It is becoming the landmark technique over conventional non-computer-assisted techniques for achieving the most accurate and symmetric bone restoration [5–11].
With CAD/CAM technology, detailed pre-operative 3D virtual surgical planning as well as its transfer to the operating room by using custom patient-specific plates and surgical cutting guides can be achieved. This technology has been advocated by many surgical teams as the most accurate and reliable method for optimizing mandibular reconstruction, which also has the potential to reduce costs by decreasing length of time for the surgery [12–20].
Although some studies have confirmed the clinical feasibility and the reproducible accuracy of CAD/CAM technology in mandibular reconstruction with fibular free flap and have argued that this technique is superior to traditional techniques, to date only four studies have been published reporting on a comparison of computer-assisted versus a conventional freehand technique [12–20].
The aims of our study were: (a) to compare outcomes from patients undergoing morphological mandibular reconstruction by fibular free flap with CAD/CAM custom patient-specific plates and surgical cutting guides versus the traditional freehand technique; (b) to evaluate the accuracy and reproducibility of the virtual surgical planning.
Materials and methods
Study design
This retrospective study included two groups of patients (CAS and Control group) who underwent mandibular reconstruction with fibular free flap after segmental mandibulectomy at the Hôpitaux Universitaires de Genève, Switzerland between 2012 and 2014. The CAS group benefited from virtual surgical planning and CAD/CAM custom patient-specific plates and surgical cutting guides. The Control group underwent conventional freehand non-computer-assisted surgery. The study was designed and conducted in accordance with the Helsinki Declaration of 1975, as revised in 2000, and was approved by our local ethics board.
Patients were excluded from the study if they had a previous history of mandibular surgery, trauma and/or if pre-and/or postoperative CT scans were not available.
Virtual surgical planning
Head and lower extremity CT-scans with 64-slice resolution were obtained in accordance with the bone acquisition protocol recommended by the manufacturer’s user guide (http://www3.gehealthcare.com).
The CT scanned images in DICOM (Digital Imaging and Communications in Medicine) format were processed using ProPlan CMF® software (Materialise, Technologielaan 15, 3001 Leuven, Belgium http://www.materialise.com). The virtual 3D pre-operative computational planning was made via the web-based Synthes PROPLAN CMF® service (GoToMeeting®, Citrix Online, Santa Barbara, CA, USA) together with a clinical engineer at Materialise in Belgium.
The 3D bone mandibular segment to be removed and the fibular segments for the reconstruction were first segmented. The fibular segments were then adapted to ensure symmetrical reconstruction after mirroring and superimposition of the nonaffected on the affected side. Virtual patient-specific mandibular and fibular surgical cutting guides were created according to the osteotomies lines and angle previously determined and the design of the future 2.5 mm custom patient-specific plate with at least three screws planned on either side of the osteotomies lines. Specific trocar guide cylinders corresponding to screw holes on the plate as well as fixation holes to maintain the cutting guides temporarily in the planned position were also integrated within the final design of the fibular and mandibular guides. Moreover, the optimal length and angulation of each screw was also planned. After the surgeon’s approval of the treatment planning, data were used to create the specific surgical cutting guides and reconstruction plate based upon the images. The final mandibular and fibular cutting guides and the reconstruction plate were then sent by the manufacturer to the surgeon and sterilized by autoclave in the hospital prior to their utilization.
Surgical technique
A double simultaneous team approach was performed in all patients of both groups.
CAS group
Prior to making the mandibular osteotomies, the cutting guides were temporarily fixed with at least two predetermined 2.0 mm screws. The screw holes of the plate were then predrilled via the specific trocar guide cylinders and the planned osteotomies were performed with a reciprocating saw through the cutting slots. After removal of the cutting guides and completion of the tumor’s resection, the reconstruction plate was then fixed with bicortical 2.4 mm locking screws. The same procedure was then performed at the fibular level. The fibular segments obtained were then fixed to the plate with monocortical 2.4 mm locking screws.
Control group (freehand technique)
The site of the mandibular osteotomies was determined pre-operatively by the surgeon on the basis of the CT scan and the MRI. First, the osteotomies lines were marked with a pencil and then a 2.4 mm reconstruction plate was bent based on a template previously contoured to the external mandible at the basilar border. At least three bicortical screw holes were drilled on either side of the osteotomies and then the plate was removed. After the completion of the tumor’s removal, the plate was fixed with bicortical 2.4 mm locking screws. The fibular graft was then osteotomized and contoured to the plate. The fibular segments were then secured with monocortical 2.4 mm locking screws.
Post-operative computational image analysis
A 64-slice high-resolution head CT-scan was obtained for each patient at least 3 months after surgery. Planned pre- and post-operative 3D CT scan images were fused by means of an automated surface matching method by using ProPlan CMF® software (Materialise, Technologielaan 15, 3001 Leuven, Belgium-http://www.materialise.com). Morphometric comparison was done by calculating the differences in linear and angular parameters on pre- and postoperative scans for both groups. The chosen parameters were measurements between well-defined anatomical landmarks on the affected versus nonaffected side (Fig. 1a–c) as follows:
-
1.
Mandibular ramus length: distance between condylion (Co) and gonion (Go).
-
2.
Mandibular body length 1: distance between gonion (Go) and the parasymphysis (ParaSym).
-
3.
Mandibular body length 2: distance between gonion (Co) and gnathion (Gn).
-
4.
Axial mandibular angle: angle formed by the plane passing through the gonion (Go) and the parasymphysis (ParaSym) and a midsagittal plane.
-
5.
Sagittal mandibular angle: angle formed by the plane passing through the gonion (Go) and the parasymhysis (ParaSym) and the plane passing through the gonion (Go) and condylion (Co).
Bony landmarks and angular and linear measurements were independently validated by two different observers. Symmetry was also assessed by calculating the ratio of affected over nonaffected side for the different parameters, with ratio closer to one indicating greater symmetry.
In the CAS group, the accuracy of the virtual surgical planning was evaluated by calculating the difference between planned and actual mandibular and fibular osteotomy sites as well as the length of the different fibular segments as follows:
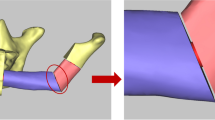
The postoperative segments were aligned with the planned segments. After alignment and per osteotomy plane, the maximum distance between the actual and the planned osteotomy was measured. The osteotomy plane of the planned mandible and fibular segments was taken as a reference. The measurements were performed in the 2D plane perpendicularly to the osteotomy plane, so that the osteotomy plane was visualized as a line. In this case, the measurements were done in two different 2D planes per osteotomy to visualize the maximum distance more clearly (Fig. 2a, b). Moreover, the accuracy of patient-specific reconstruction plate positioning was assessed by superimposing the planned and postoperative 3D mandible (Fig. 2c).
Accuracy of the virtual surgical planning. Postoperative mandibular (a) and fibular (b) segments aligned with the planned segments and measurement of the maximum distance between the actual and the planned osteotomies. Comparison of postoperative plate position on the mandible with planned plate position (c)
Results
The CAS group consisted of seven patients (5 women and 2 men) with a mean age of 65.8 years (range 45–79 years). Six had squamous cell carcinoma and one osteoradionecrosis. Two patients had a simple mandibular reconstruction using one single fibular segment, while the remaining five underwent a mandibular reconstruction by means of two fibular segments. In two patients, the lesion extended contralaterally with the involvement of the entire symphysis (Table 1).
The Control group included 11 patients (2 women and 9 men) with a mean age of 55.9 years (range 42–62 years). Six patients had squamous cell carcinoma and five had osteoradionecrosis. One patient had a simple mandibular reconstruction using one single fibular segment, while among the remaining nine patients, seven underwent a mandibular reconstruction by means of two fibular segments and three patients by means of three segments. In eight patients, the lesion extended contralaterally with involvement of the entire symphysis (Table 1). In both groups, the mandibular bone defects were classified based on their anatomic location and divided into defects involving the symphysis (S) or hemisymphysis (SH), the body (B), the ramus (R) and the condyle (C) according to Urken et al. classification [3].
The morphometric accuracy, assessed by calculating the mean and standard deviation of the absolute difference between pre- and postoperative linear and angular measurements, showed no statistically significant differences in both groups except for the axial angle on the nonaffected side (1.0° in the CAS group versus 2.9° in the control group; p = 0.03) (Table 2).
Ratios of the affected side over the nonaffected side were calculated for the different parameters obtained, and all of them were close to 1 in both groups, indicating no differences between the two groups in terms of overall accuracy (Table 3).
In the CAS group, the accuracy assessment showed a mean distance deviation of 2.3 ± 1.0 mm for mandibular osteotomies and 1.9 ± 1.1 mm for fibular osteotomies. To note, data of only five patients were included for the fibular osteotomy sites because of deviations from the standard surgery. In two patients, the fibular cutting guides could not be used due to intra-operative change in surgical strategy because of tumoral evolution after the virtual planning. Data from six patients were included for the mandibular osteotomy sites. One patient was excluded from the final analysis because of a consistently long bony spine left of the proximal ramus portion after mandibular osteotomy, which prevented a proper 3D mandibular superimposition (Tables 4, 5).
Discussion
This study aimed to compare the morphology of mandibular reconstruction by fibular free flap with and without the assistance of 3D virtual surgical planning with the use of intra-operative patient-specific surgical guides and reconstruction plates. Additionally, the accuracy of the virtual surgical planning was assessed. Our findings showed comparable precision between the two groups and an acceptable accuracy with respect to the capacity of reproducing the virtually planned fibular segment repositioning and mandibular osteotomies in the CAS group. Thus far, few studies have reported specifically on the evaluation of the accuracy of fibular mandibular reconstruction using virtual surgical planning. The main limitation in analyzing the different studies is the disparity and lack of uniformity of the methodology used. This unfortunately prevents a coherent analysis and comparison of our results with analogous data in the literature. Nevertheless, the general advantages of virtual surgical planning in cranio-facial surgery, which are in part obvious, have been well documented in the literature. Such advantages include reproducible and accurate results, decrease in surgical time, improved bone-to-bone contact, improved facial symmetry and functional outcome, and decrease of overall costs [12–20]. A detailed analysis of each of these advantages is beyond the scope of this article. Conversely, only four studies have focused on the comparison of the results from use of conventional and virtual-planned techniques. Hanasono et al. were the first to assess the morphological differences by analyzing the pre- and postoperative position of specific bony landmarks (i.e., gonion, gnathion and condyle) in patients undergoing mandibular reconstruction with and without virtual surgical planning [12]. They found a statistically significant difference between the two groups for deviations of position in favor of the virtual planned group over the non-virtual planned group (4.11 ± 3.09 versus 6.92 ± 5.64 mm, respectively), thus confirming the superiority of the virtual surgical planning. Moreover, they showed accuracy in linear fibular length and angular measurements of osteotomy lines between planned and actual reconstruction in the virtual planned group of 2.40 ± 2.06 mm versus 3.51° ± 2.69°, respectively. Interestingly, the trend was significantly higher for differences in gnathion position [12]. This is probably due to the fact that reconstructions involving the symphysis are by far the most difficult to reestablish, especially when several fibular segments are needed. Zhang et al. evaluated the mean difference in intercondylar distances, intergonial angle distances, anteroposterior distances and gonial angle [13]. They also found better results when using computer-assisted surgery over the conventional freehand technique. Mean differences were 1.14 mm in intercondylar distance, 1.49 mm in anteroposterior distance, 0.80 mm in intergonial angle distance and 1.60° in gonial angle between the computer-assisted surgery and conventional group. Moreover, the accuracy assessment of the virtual reconstruction showed a mean difference of 1.34 mm in length deviation and 2.29° in angular deviation of the fibular segments [13].
Stirling Craig et al. evaluated interfragmentary gap size and symmetry [14]. They found significantly lessened space between the fibular segments in the CAS group, whereas no difference was found in the reproducibility of symmetry [14].
Weitz et al. evaluated the accuracy of mandibular reconstruction between virtual planned and conventional groups by calculating the mandibular angle between the ramus and the body as well as the distance between the mandibular angle and the midline on a panoramic radiograph [15]. They found a higher statistically significant difference between the angle of the mandible pre- and postoperatively in the conventional group over the virtual group 11.5° versus 4.5° (range 0°–18°) [15]. Contrary to the three other studies, the authors did not assess the intrinsic accuracy of the virtual planning.
Similar to the results found by Stirling Craig et al. and contrary to the findings of the other three aforementioned studies, our results showed that both techniques were equivalent in their ability to provide morphological and symmetrical reconstruction. These results are even more surprising when considering that reconstructions in the control group were more complex than in the CAS group. There could be two main reasons for this finding. First, the freehand technique has been the standard for mandibular free flap reconstruction since its introduction in our department in the late 90s. Therefore, a high level of expertise in managing such a demanding surgery has been developed. Moreover, the same experienced surgeon performed all the procedures in the Control group; whereas three surgeons, performed the virtual planning and the surgery in the CAS group. Second, the cases in the CAS group were the first seven performed by using this new technology, which as pointed out by others has its own learning curve and its own limitations in terms of accuracy [16]. In fact, besides the issue of the intrinsic accuracy of the CAD/CAM systems, there can be difficulties in evaluating clinical accuracy due to incalculable and unavoidable technical, imaging, applicative and human errors. These errors can occur during the planning phase as well as during the process of the accuracy evaluation itself. Furthermore, no consensus has been reached on establishing the range of tolerable accuracy error for the different CAS procedures. When evaluating data extrapolated from studies on the use of 3D virtual planning in orthognathic surgery, some authors have suggested that the accuracy cutoff could reasonably be set at 2 mm, given that differences within this range a priori would not likely be noticeable to the naked eye [17, 18]. Conversely, other authors have considered accuracy between the actual and planned measurements allowed for clinical use to be within 0.5 mm [19]. Thus far, only few studies on the accuracy evaluation of mandibular reconstruction by fibula free flap using the CAD/CAM technique have been reported. Roser et al. were the first to report on the accuracy of virtual surgical planning and its application by using surgical cutting guides and templates in free fibular flap mandibular reconstruction [20]. They found an accuracy within 2 mm for the distance of mandibular resection and within 1.3 mm for the fibular segment osteotomies [20].
Zheng et al. analyzed data of four patients who underwent mandibular reconstruction by using virtual planned surgical templates [21]. They stated that the method was accurate but without performing any scientific analysis. Foley et al. analyzed data from eight patients among which five underwent free fibular flap and three anterior iliac crest mandibular reconstruction, and they evaluated the antero-posterior and transversal dimensions [22]. In the fibular group, they found an average surgical error of 0.2 mm in the antero-posterior dimension, 2.7 mm from condyle to condyle and 2.5 mm from gonial angle to gonial angle [22]. Succo et al. reported the best results in terms of accuracy by comparison with all of the other studies. They found in five patients a mean difference of fibular segment length of 1 mm [23]. Metzler et al. analyzed data of ten patients and performed a 3D morphometric assessment of the mandibular reconstruction [24]. They found a 1.3 mm difference in fibular segment length, 12.4° and—12.5° difference in the anterior and posterior mandibular angles, respectively, and a 1.7 mm difference in the condylar distance and 4.6° difference in the condylar angle [24].
Even with limited studies available and considering the non-negligible heterogeneity in the methodologies, our results seem to be in line with the precision and reproducibility data reported in the literature.
Conclusion
Our results indicate that CAS and the conventional freehand techniques are comparable in their ability to provide a satisfactory morphological fibular free flap mandibular reconstruction. Moreover, the accuracy of the CAS technique is within the range reported by similar studies with data from a similar number of patients. However, given the limited number of patients and the retrospective nature of this study, these results should be interpreted with caution knowing that only a prospective study comparing the two techniques would allow definitive conclusions to be drawn.
References
Hidalgo DA (1989) Fibula free flap: a new method of mandible reconstruction. Plast Reconstr Surg 84:71–79
Hidalgo DA, Pusic AL (2002) Free-flap mandibular reconstruction: a 10-year follow-up study. Plast Reconstr Surg 110:438–449
Urken ML, Weinberg H, Vickery C, Buchbinder D, Lawson W, Biller HF (1991) Oromandibular reconstruction using microvascular composite free flaps. Report of 71 cases and a new classification scheme for bony, soft-tissue, and neurologic defects. Arch Otolaryngol Head Neck Surg 117:733–744
Bak M, Jacobson AS, Buchbinder D, Urken ML (2009) Contemporary reconstruction of the mandible. Oral Oncol 46:71–76
Eckardt A, Swennen GR (2005) Virtual planning of composite mandibular reconstruction with free fibula bone graft. J Craniofac Surg 16:1137–1140
Hallermann W, Olsen S, Bardyn T, Taghizadeh F, Banic A, Iizuka T (2006) A new method for computer-aided operation planning for extensive mandibular reconstruction. Plast Reconstr Surg 117:2431–2437
Adolphs N, Haberl EJ, Liu W, Keeve E, Menneking H, Hoffmeister B (2013) Virtual planning for craniomaxillofacial surgery—7 years of experience. J Craniomaxillofac Surg 42:e289–e295
Wilde F, Cornelius CP, Schramm A (2014) Computer-assisted mandibular reconstruction using a patient-specific reconstruction plate fabricated with computer-aided design and manufacturing techniques. Craniomaxillofac Trauma Reconstr 7:158–166
Rodby KA, Turin S, Jacobs RJ, Cruz JF, Hassid VJ, Kolokythas A, Antony AK (2014) Advances in oncologic head and neck reconstruction: systematic review and future considerations of virtual surgical planning and computer aided design/computer aided modeling. J Plast Reconstr Aesthet Surg 67:1171–1185
Sieira Gil R, Roig AM, Obispo CA, Morla A, Pages CM, Perez JL (2015) Surgical planning and microvascular reconstruction of the mandible with a fibular flap using computer-aided design, rapid prototype modelling, and precontoured titanium reconstruction plates: a prospective study. Br J Oral Maxillofac Surg 53:49–53
Antony AK, Chen WF, Kolokythas A, Weimer KA, Cohen MN (2011) Use of virtual surgery and stereolithography-guided osteotomy for mandibular reconstruction with the free fibula. Plast Reconstr Surg 128:1080–1084
Hanasono MM, Skoracki RJ (2012) Computer-assisted design and rapid prototype modeling in microvascular mandible reconstruction. Laryngoscope 123:597–604
Zhang L, Liu Z, Li B, Yu H, Shen SG, Wang X (2016) Evaluation of computer-assisted mandibular reconstruction with vascularized fibular flap compared to conventional surgery. Oral Surg Oral Med Oral Pathol Oral Radiol 121:139–148
Stirling Craig E, Yuhasz M, Shah A, Blumberg J, Salomon J, Lowlicht R, Fusi S, Steinbacher DM (2015) Simulated surgery and cutting guides enhance spatial positioning in free fibular mandibular reconstruction. Microsurgery 35:29–33
Weitz J, Bauer FJ, Hapfelmeier A, Rohleder NH, Wolff KD, Kesting MR (2016) Accuracy of mandibular reconstruction by three-dimensional guided vascularised fibular free flap after segmental mandibulectomy. Br J Oral Maxillofac Surg. doi:10.1016/j.bjoms.2016.01.029
Farfalli GL, Albergo JI, Ritacco LE, Ayerza MA, Milano FE, Aponte-Tinao LA (2016) What is the expected learning curve in computer-assisted navigation for bone tumor resection? Clin Orthop Relat Res. doi:10.1007/s11999-016-4761-z
Kaipatur N, Al-Thomali Y, Flores-Mir C (2009) Accuracy of computer programs in predicting orthognathic surgery hard tissue response. J Oral Maxillofac Surg 67:1628–1639
Hsu SS, Gateno J, Bell RB, Hirsch DL, Markiewicz MR, Teichgraeber JF, Zhou X, Xia JJ (2013) Accuracy of a computer-aided surgical simulation protocol for orthognathic surgery: a prospective multicenter study. J Oral Maxillofac Surg 71:128–142
Schendel SA, Jacobson R, Khalessi S (2013) 3-dimensional facial simulation in orthognathic surgery: is it accurate? J Oral Maxillofac Surg 71:1406–1414
Roser SM, Ramachandra S, Blair H, Grist W, Carlson GW, Christensen AM, Weimer KA, Steed MB (2010) The accuracy of virtual surgical planning in free fibula mandibular reconstruction: comparison of planned and final results. J Oral Maxillofac Surg 68:2824–2832
Zheng GS, Su YX, Liao GQ, Liu HC, Zhang SE, Liang LZ (2013) Mandibular reconstruction assisted by preoperative simulation and accurate transferring templates: preliminary report of clinical application. J Oral Maxillofac Surg 71:1613–1618
Foley BD, Thayer WP, Honeybrook A, McKenna S, Press S (2013) Mandibular reconstruction using computer-aided design and computer-aided manufacturing: an analysis of surgical results. J Oral Maxillofac Surg 71:e111–e119
Succo G, Berrone M, Battiston B, Tos P, Goia F, Appendino P, Crosetti E (2013) Step-by-step surgical technique for mandibular reconstruction with fibular free flap: application of digital technology in virtual surgical planning. Eur Arch Otorhinolaryngol 272:1491–1501
Metzler P, Geiger EJ, Alcon A, Ma X, Steinbacher DM (2014) Three-dimensional virtual surgery accuracy for free fibula mandibular reconstruction: planned versus actual results. J Oral Maxillofac Surg 72:2601–2612
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
De Maesschalck, T., Courvoisier, D.S. & Scolozzi, P. Computer-assisted versus traditional freehand technique in fibular free flap mandibular reconstruction: a morphological comparative study. Eur Arch Otorhinolaryngol 274, 517–526 (2017). https://doi.org/10.1007/s00405-016-4246-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-016-4246-4