Abstract
Background
Serum amyloid A (SAA) was involved in the pathogenesis of glucocorticoid resistance in lung diseases. However, their association with systemic corticosteroid insensitivity in chronic rhinosinusitis with nasal polyps (CRSwNP) patients remains to be assessed.
Methods
This study enrolled 32 CRSwNP patients to evaluate the association between SAA expression in NP and corticosteroid insensitivity, and the value of polyp SAA level for predicting the response to oral corticosteroids in CRSwNP patients. All patients were given a course of oral prednisone (30 mg daily for 2 weeks) and subdivided into glucocorticoid(GC)-sensitive and -insensitive subgroup according to the change in polyp size scores. The polyp specimens were obtained before and after corticosteroid treatment. SAA levels in polyp tissues were evaluated by enzyme-linked immunosorbent assay and quantitative reverse transcription polymerase chain reaction. Regression analysis was performed to analyze the association between SAA protein levels and corticosteroid insensitivity.
Results
13/32 (40.62%) CRSwNP patients were insensitive to the oral corticosteroid therapy. SAA mRNA and protein levels were significantly increased in GC-insensitive NP compared to those in GC-sensitive NP. Tissue SAA protein levels were positively correlated with tissue neutrophil numbers. Regression analysis revealed tissue SAA levels were significantly correlated with corticosteroid insensitivity (P < 0.01). ROC curves indicated that the area under the curve was 0.87. When the polyp SAA protein level was 122.2 ng/ml or higher, the sensitivity and specificity were 76.92 and 73.68%, respectively.
Conclusions
Our findings suggest that increased SAA in NP is associated with reduced response to oral corticosteroids in CRSwNP. SAA levels in NP may have potential value in predicting corticosteroid insensitivity in CRSwNP patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic rhinosinusitis (CRS), affecting 14% of adults in the United States and 8% in China [1, 2], is a common mucosal inflammation in nasal sinus comprising two subtypes: chronic rhinosinusitis without nasal polyps (CRSsNP) and chronic rhinosinusitis with nasal polyps (CRSwNP). Compared with CRSsNP, CRSwNP shows higher degree of disease severity and poorer response to medical and surgical therapy [1]. In the western world, CRSwNP has been characterized by a Th2-biased response and tissue eosinophilia [3,4,5]. However, CRSwNP patients in China present a distinct pathogenic phenotype including neutrophilic accumulations and mixed T helper(Th)1/Th2/Th17 response [6, 7], suggesting a more heterogeneous nature of CRSwNP in China.
Corticosteroids are the most effective therapy for many inflammatory airway diseases, including asthma, chronic obstructive pulmonary disease (COPD) and CRS. However, the therapeutic response varies markedly between individuals. It has been reported that up to one-third of patients with asthma display insensitivity to corticosteroids [8]. Although the prevalence of corticosteroid insensitivity in CRSwNP is unclear, it is reasonable to deduce that there are more CRSwNP patients with corticosteroid insensitivity in China, since the additional neutrophilic infiltrate in nasal polyps could reduce the efficacy of oral corticosteroid treatment [7]. Therefore, corticosteroid insensitivity in CRSwNP represents a huge management problem, and novel biological predictors of treatment response to corticosteroids are needed for precision treatment.
SAA is a major acute-phase protein and has been a clinical biomarker for active inflammation [9]. Many studies have shown that SAA levels are remarkably elevated in patients with a broad spectrum of chronic inflammatory diseases, such as atherosclerosis [10], rheumatoid arthritis [11], severe allergic asthma [12] and CRSwNP [13]. The association of SAA with neutrophilic inflammation and Th17 immune response in CDPD [14], allergic asthma [15] as well as CRSwNP [13] have been demonstrated. More recently, SAA was found to play an important role in the pathogenicity of glucocorticoid-resistant lung disease. For example, Steven et al. showed that SAA could elicit glucocorticoid-resistant inflammation in lung through induction of a potent neutrophilic airway inflammation by counteracting lipoxin A4, an endogenous proresolving mediator [14]. Ather et al. showed that SAA induced a glucocorticoid-resistant Th17 response in an ovalbumin-induced mouse model of allergic airway disease by inhibiting dendritic cell apoptosis [16]. However, the relationship between the local expression of SAA and systemic corticosteroid insensitivity in patients with CRSwNP remains unclear. In this study, we conducted a cohort of patients with CRSwNP to explore the association between SAA expression in nasal polyp and systemic corticosteroid insensitivity, and evaluate the value of polyp SAA level for predicting the response to oral corticosteroid treatment.
Methods
Patients and tissue samples
Thirty-two patients with CRSwNP were recruited from the Shantou Central Hospital and the First Affiliated Hospital of Sun Yat-sen University (Shantou and Guangzhou, China). This study was approved by the Ethics Committee of the first affiliated hospital of Sun Yat-sen University and the Ethics Committee of Shantou Central Hospital, and an informed consent was obtained from each subject. The diagnosis of CRSwNP was carried out according to the European position paper on rhinosinusitis and nasal polyps (EPOS 2012) [1]. All patients showed score 2–4 on both sides of polyps based on nasal polyp scoring system (Table 1). The CRSwNP patients were prescribed with oral corticosteroids (30 mg of prednisone once daily for 14 days). Before and after oral corticosteroid treatment, polyp tissues were sampled from each subject. GC-insensitive CRSwNP subgroup was defined as described by Milara et al. [17, 18], namely patients who are unable to reduce more than 1 polyp score based on nasal polyp scoring system (Table 1) after oral corticosteroid treatment. The diagnosis of asthma was determined by a pneumologist. Diagnosis of aspirin intolerance is based on detailed clinical history. None of the patients included used oral or nasal steroids or other immunomodulatory drugs within 4 weeks before starting oral corticosteroids.
Quantitative reverse transcription polymerase chain reaction (qRT-PCR)
The mRNA expression level of SAA gene in polyp tissue was detected by qRT-PCR analysis as previously described [13]. Briefly, total RNA was extracted from the polyp samples with TRIzol reagent (Invitrogen) following the manufacturer’s instructions. Reverse transcription was performed and the cDNA was synthesized from 2 µg of total RNA using an oligo (dT) 18 primer and M-MLV reverse transcriptase (TAKARA, Syuzou, Shiga, Japan) for quantitative PCR. RNA integrity and the success of the reverse transcription reaction were monitored by PCR amplification of β-actin transcripts. Expression of mRNA was determined using ABI PRISM 7500 Detection System (Applied Biosystems, Foster City, CA, USA) and SYBR Premix Taq™ (TAKARA). The primer sequences were as follows: SAA forward: 5′-CTT GGC GAG CCT TTT GAT G-3′; reverse: 5′-TAG TTC CCC CGA GCA TGG-3′; β-actin forward: 5′-AAG ATG ACC CAG ATC ATG TTT GAG ACC-3′; β-actin reverse 5′-AGC CAG GTC CAG ACG CAG GAT-3′. PRISM samples contained 1 × SYBR Green Master Mix, 1.5 μL 5 μM primers, and 25 ng synthesized cDNA in a 25-μL volume. Reactions were heated to 95 °C for 10 min followed by 40 cycles of denaturation at 95 °C for 10 s, annealing extension at 60 °C for 60 s. Melting curve analysis was used to control for amplification specificity. Expression of target gene was expressed as fold increase relative to the expression of β-actin. The mean value of the replicates for each sample was calculated and expressed as cycle threshold (C t). The amount of gene expression was then calculated as the difference (ΔC t) between the C t value of target gene and the tt value of β-actin. Fold changes in target gene mRNA were determined as 2− ΔCt.
Enzyme-linked immunosorbent assay (ELISA)
Freshly obtained polyp tissue samples were weighed, and placed in PBS-Tween supplemented with a protease inhibitor cocktail (Keygentec, Nanjing, Jiangsu, China), and homogenized for 1 min on ice. The samples were then centrifuged at 4000 rpm for 20 min at 4 °C, and the supernatants were stored at − 20 °C until ELISA analysis. The SAA concentrations in polyp tissues were measured with commercially available ELISA (ab100635, Abcam) according to the manufacturer’s instructions. Detection limits were 0.41 ng/mL of SAA.
Histologic analysis and immunohistochemical (IHC) staining
NP tissues embedded in paraffin were cut into 5-μm sections and placed onto glass slides. HE and IHC staining were performed for histological examination using the standardized procedures as previously described [13]. Briefly, sections were deparaffinized by serial treatment. Sections stained with HE were used to determine the general pathologic features of tissues at 40× and 100× magnification. The number of eosinophils in the lamina propria was counted at high power (HP) magnification (400×), and 10 HP fields were randomly selected and analyzed. Results were expressed as cells per HP field of LP. After blocking the endogenous peroxidase in 3% hydrogen peroxide and with 1% bovine serum albumin, the sections were incubated overnight at 4 °C in the presence of a mouse anti-human SAA monoclonal antibody (Abcam, Cambridge, MA, USA) at a dilution of 1:100, or anti-myeloperoxidase (MPO) antibody (Abcam, Cambridge, MA, USA) at a dilution of 1:50 according to the manufacturer’s instructions. Each of these sections was incubated with a secondary antibody and then with horseradish peroxidase-labeled streptavidin complex (Zhongshanjinqiao, Beijing, China). Distribution of peroxidase was revealed by incubating the sections in a solution containing 3% 3,3′-diaminobenzidine tetrahy-drochloride before being counterstained with hematoxylin and cover slipped. Negative control studies were performed by omitting the incubation step with the primary antibody. Sections were inspected by a single “blinded” observer in a coded random order. Number of MPO-positive cells per HP field was analyzed. Five fields were randomly selected.
Statistical analysis
GraphPad Prism 6 software (San Diego, CA, USA) was used for statistical analyses. Discrete data were expressed as the medians and interquartile ranges (IQRs) and analyzed using the nonparametric Mann–Whitney U test. A univariate logistic regression analysis was performed to assess the association between systemic cocorticosteroid insensitivity and and the tissue SAA protein levels and the tissue eosinophil and neutrophil numbers. The predictive abilities of tissue eosinophil and neutrophil numbers and tissue SAA pretein levels were evaluated by receiver operating characteristic (ROC) curve. A P value less than 0.05 was considered as statistically significant.
Results
Clinical parameters between GC-sensitive and GC-insensitive NP groups
To determine the sensitivity of CRSwNP patients responding to corticosteroid, we compared the endoscopy scores before and after 14 days of treatment with oral prednisone. According to previous studies [17, 18], we defined patients who were unable to reduce more than 1 NP endoscopic score after oral prednisone course as GC-insensitive NP subgroup. As a result, there are 19 NP patients in the GC-sensitive NP subgroup and 13 NP patients in the GC-insensitive NP subgroup. The clinical characteristics of the two subgroups were showed in Table 2. We found that the mean absolute number of blood eosinophils in GC-sensitive subgroup was significantly higher than that in GC-insensitive subgroup. The mean NP endoscopic scores were significantly reduced after treatment in GC-sensitive subgroup (P < 0.05), but not in GC-insensitive subgroup.
SAA expression in NP tissues before and after oral corticosteroid treatment
Next, we sought to determine the effect of oral prednisone treatment on the tissue eosinophils and neutrophils as well as SAA expression. As indicated Fig. 1, the mean number of eosinophils (Fig. 1a) in polyp tissues was significantly reduced after corticosteroid treatment compared with baseline number (P < 0.01). However, there were no significant differences in the mean number of neutrophils (Fig. 1b) and the mRNA (Fig. 1c) and protein (Fig. 1d) levels of SAA expression in polyp tissues between before and after oral corticosteroid treatment (P > 0.05).
Changes from baseline in tissue eosinophil and neutrophil counts and SAA expression in nasal polyps treated with oral corticosteroid treatment. After corticosteroid treatment, the mean number of eosinophils (a), but not neutrophils (b), as well as SAA mRNA (c) and protein (d) levels were significantly reduced in polyp tissues. **P < 0.01; ns no significance, NP nasal polyps, SAA serum amyloid A, EOS eosinophil, NEU neutrophil, HPF high power field
SAA expression in GC-sensitive and GC-insensitive NP tissues
Next, we subdivided the patients with CRSwNP into two groups on the basis of the response to oral corticosteroid treatment. As indicated in Fig. 2, we found that the mean number of eosinophils was significantly lower (Fig. 2a, b), but neutrophils was higher (Fig. 2c, d) in GC-insensitive NP than in GC-sensitive NP (both P < 0.01). By doing IHC staining, we found strong immunoreactivity of SAA was mainly observed in the epithelium of GC-insensitive NP. By contrast, the SAA immunoreactivity was relatively weak in the epithelium of GC-sensitive NP (Fig. 3a). Consistently, the SAA protein levels as evaluated by ELISA and mRNA levels as evaluated by qRT-PCT in NP tissues were significantly elevated in GC-insensitive subgroup as compared to the GC-sensitive subgroup (P < 0.001 and 0.01, respectively) (Fig. 3b, c). By correlation analysis, we found that the SAA protein level was positively associated with the mean number of neutrophils in nasal polyps (R = 0.61, P < 0.001) (Fig. 4).
Numbers of eosinophils and neutrophils in GC-sensitive and GC-insensitive NP. Representative H&E (a) and immunohistochemical staining of MPO (c) in GC-sensitive and GC-insensitive NP. Original magnification: ×400. By histopathologic analysis, the mean number of eosinophils b was significantly lower, but neutrophils (MPO+ cells) d was higher in GC-insensitive NP. GC glucocorticoid, MPO myeloperoxidase, H&E hematoxylin and eosin, NP nasal polyps, EOS eosinophil, NEU neutrophil, HPF high power field
SAA expression in GC-sensitive and GC-insensitive NP. a Representative immunohistochemical staining of SAA in GC-sensitive and GC-insensitive NP. Original magnification: ×400. The protein level (b) and mRNA level (c) of SAA in GC-sensitive and GC-insensitive NP assessed by ELISA. **P < 0.01; ***P < 0.001. GC glucocorticoid, NP nasal polyps, NP nasal polyps, SAA serum amyloid A
Association of local SAA expression and systemic corticosteroid insensitivity in patients with CRSwNP
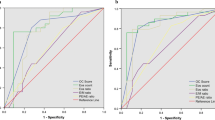
We further performed logistic regression analysis to determine the association between corticosteroid insensitivity and the tissue SAA protein levels and the tissue eosinophil and neutrophil numbers followed by ROC curve analysis. The results revealed that corticosteroid insensitivity was significantly correlated with polyp SAA protein levels, tissue eosinophil numbers and tissue neutrophil numbers (P < 0.01, 0.05 and 0.05, respectively). Odds ratio (OR) were 1.03, 0.887 and 1.163, respectively. 95% confidence interval (CI) were 1.01–1.05, 0.799–0.984 and 1.022–1.322, respectively. As shown in Fig. 5, the receiver operating characteristic (ROC) curves analysis indicated that the polyp SAA protein levels [area under the curve (AUC) = 0.87] had a higher predictive value for corticosteroid insensitivity than tissue eosinophil numbers (AUC = 0.8) and tissue neutrophil numbers (AUC = 0.77). When the polyp SAA protein level was 122.2 ng/ml or higher, the sensitivity and specificity were 76.92 and 73.68%, respectively.
The ROC curve for polyp SAA protein levels, tissue eosinophil and neutrophil numbers. AUC of polyp SAA protein level, tissue eosinophil and neutrophil numbers were 0.8704 (95% CI 0.7503–0.9906), 0.8016 (95% CI 0.6427–0.9606) and 0.7733 (95% CI 0.5991–0.9475), respectively. ROC receiver operating characteristic, SAA serum amyloid A, AUC area under the ROC curve, CI confidence interval, EOS eosinophil, NEU neutrophil
Discussion
Corticosteroids are now first-line therapy for patients with CRSwNP [1]. Different endotypes of CRSwNP could display similar clinical features but significant difference in responding to corticosteroid treatment [19, 20]. To date, there is no effective marker to predict corticosteroid insensitivity or sensitivity in CRSwNP patients. In the present study, we found that oral corticosteroids was unable to affect the SAA expression in nasal polyps, elevated SAA level in nasal polyps was significantly associated with tissue neutrophil number and systemic corticosteroid insensitivity in patients with CRSwNP, and provided the first evidence that polyp tissue SAA level could be considered as a predictor of oral corticosteroid insensitivity in CRSwNP patients. Our findings may also expand current understandings of CRSwNP heterogeneity and contribute to the precision treatment of CRSwNP.
Corticosteroid insensitivity is present in many chronic inflammatory airway diseases, such as allergic asthma [8], COPD [21], allergic rhinitis and CRS [22], and may contribute to continuing disease severity with the potential risks, such as hyperglycemia and infection et al [19], representing a challenging clinical problem despite the availability of modern treatments. Several strategies attempting to address this problem have been proposed, including avoiding patients with factors associated with corticosteroid insensitivity, targeting molecular mechanisms underlying corticosteroid insensitivity to prevent or restore corticosteroid insensitivity, and developing biomarkers to predict patients with corticosteroid insensitivity or sensitivity [8]. From the standpoint of precision treatment, it would be an advantage to be able to predict the response to corticosteroid treatment. Indeed, many biomarkers have been developed for predicting corticosteroid responsiveness in asthma [23, 24] and COPD [25]. However, there is no effective predictors of corticosteroid efficacy for CRSwNP. Here, we extended our previous study [13] and found the SAA protein level is a good indicator of poor response to systemic corticosteroid therapy in CRSwNP patients. Thus, it is logical to postulate that use of this biomarker might allow for better identification of CRSwNP patients who are most unlikely to benefit from corticosteroid therapy.
SAA have been shown to be involved in the pathogenesis of steroid resistance. Bozinovski et al. [14] showed that SAA administered into lung was able to induce a neutrophilic response, which can be relieved by lipoxin A4 but not dexamethasone, suggesting SAA might be a mediator of GC-resistant lung inflammation. Ather et al. [16] demonstrated that SAA could prolong the viability of DC and enhance their pro-inflammatory potential by stimulating CD4+ T cells, contributing to the pathogenesis of GC resistance in lung disease. In the current study, we showed SAA expression was significantly increased in GC-insensitive NP compared to those in GC-sensitive NP and positively correlated with tissue neutrophil number, which have been reported to contribute to corticosteroid insensitivity in CRSwNP [7]. Further regresion analysis confirmed the close association between SAA protein level in NP and systemic corticosteroid insensitivity. However, it is still unclear whether and how SAA involves in mechanism underlying corticosteroid insensitivity in CRSwNP. Further study will be required to address this issue.
In this study, we show that systemic corticosteroid therapy had no significant effect on the expression of SAA in NP. Our findings conflict with results of a recently published report by Bozinovski et al. [14] showing that corticosteroids could significantly increase SAA expression in a THP-1 cell line. It is likely that this discrepancy may simply reflect differences between in vitro and in vivo study, or possibly that one course of oral corticosteroids (30 mg of prednisone once daily for 14 days) is insufficient to upregulate SAA level in NP. Thus, prolonged course of oral corticosteroids might be needed in the future study.
Our current study is limited because of the small sample size and lack of a placebo group. These would restrict the ability to extrapolate our findings to the general population. A placebo-controlled trial with larger sample size is, therefore, necessary to strengthen the conclusion. In additon, to minimize the influence on the nasal polyp score, we only took biopsies of very small pieces of nasal polyp tissue before corticosteroid therapy. This limit our capacity to measure additional cytokines, such as IL-4, IL-5, IL-13 and IL-17A, in the present study. Therefore, molecular endotypes of nasal polyps in this study remain unclear. Future study using cytokine microarray might address this issue.
Conclusions
In summary, our preliminary study provides the first evidence that increased expression of SAA in nasal polyps is associated with reduced response to oral corticosteroid treatment in patients with CRSwNP. SAA levels in nasal polyps might have potential value in predicting corticosteroid insensitivity in CRSwNP patients.
References
Fokkens WJ, Lund VJ, Mullol J, Bachert C, Alobid I, Baroody F, Cohen N, Cervin A, Douglas R, Gevaert P et al (2012) European position paper on rhinosinusitis and nasal polyps 2012. Rhinol Suppl(23):1–298 (3 p preceding table of contents)
Shi JB, Fu QL, Zhang H, Cheng L, Wang YJ, Zhu DD, Lv W, Liu SX, Li PZ, Ou CQ et al (2015) Epidemiology of chronic rhinosinusitis: results from a cross-sectional survey in seven Chinese cities. Allergy 70(5):533–539
Wang X, Zhang N, Bo M, Holtappels G, Zheng M, Lou H, Wang H, Zhang L, Bachert C (2016) Diversity of TH cytokine profiles in patients with chronic rhinosinusitis: a multicenter study in Europe, Asia, and Oceania. J Allergy Clin Immunol 138(5):1344–1353
Newman LJ, Platts-Mills TA, Phillips CD, Hazen KC, Gross CW (1994) Chronic sinusitis: relationship of computed tomographic findings to allergy, asthma, and eosinophilia. JAMA 271(5):363–367
Bachert C, Gevaert P, Holtappels G, Johansson SG, van Cauwenberge P (2001) Total and specific IgE in nasal polyps is related to local eosinophilic inflammation. J Allergy Clin Immunol 107(4):607–614
Cao PP, Li HB, Wang BF, Wang SB, You XJ, Cui YH, Wang DY, Desrosiers M, Liu Z (2009) Distinct immunopathologic characteristics of various types of chronic rhinosinusitis in adult Chinese. J Allergy Clin Immunol 124(3):478–484 (484 e471–472)
Wen W, Liu W, Zhang L, Bai J, Fan Y, Xia W, Luo Q, Zheng J, Wang H, Li Z et al (2012) Increased neutrophilia in nasal polyps reduces the response to oral corticosteroid therapy. J Allergy Clin Immunol 129(6):1522–1528 e1525
Thomson NC (2016) Addressing corticosteroid insensitivity in adults with asthma. Expert Rev Respir Med 10(2):137–156
Ye RD, Sun L (2015) Emerging functions of serum amyloid A in inflammation. J Leukoc Biol 98(6):923–929
Fyfe AI, Rothenberg LS, DeBeer FC, Cantor RM, Rotter JI, Lusis AJ (1997) Association between serum amyloid A proteins and coronary artery disease: evidence from two distinct arteriosclerotic processes. Circulation 96(9):2914–2919
Chambers RE, MacFarlane DG, Whicher JT, Dieppe PA (1983) Serum amyloid-A protein concentration in rheumatoid arthritis and its role in monitoring disease activity. Ann Rheum Dis 42(6):665–667
Buyukozturk S, Gelincik AA, Genc S, Kocak H, Oneriyidogan Y, Erden S, Dal M, Colakoglu B (2004) Acute phase reactants in allergic airway disease. Tohoku J Exp Med 204(3):209–213
Wang H, Bai J, Ding M, Liu W, Xu R, Zhang J, Shi J, Li H (2013) Interleukin-17A contributes to the expression of serum amyloid A in chronic rhinosinusitis with nasal polyps. Eur Arch Otorhinolaryngol 270(6):1867–1872
Bozinovski S, Uddin M, Vlahos R, Thompson M, McQualter JL, Merritt AS, Wark PA, Hutchinson A, Irving LB, Levy BD et al (2012) Serum amyloid A opposes lipoxin A(4) to mediate glucocorticoid refractory lung inflammation in chronic obstructive pulmonary disease. Proc Natl Acad Sci USA 109(3):935–940
Ather JL, Ckless K, Martin R, Foley KL, Suratt BT, Boyson JE, Fitzgerald KA, Flavell RA, Eisenbarth SC, Poynter ME (2011) Serum amyloid A activates the NLRP3 inflammasome and promotes Th17 allergic asthma in mice. J Immunol 187(1):64–73
Ather JL, Fortner KA, Budd RC, Anathy V, Poynter ME (2013) Serum amyloid A inhibits dendritic cell apoptosis to induce glucocorticoid resistance in CD4(+) T cells. Cell Death Dis 4:e786
Milara J, Peiro T, Armengot M, Frias S, Morell A, Serrano A, Cortijo J (2015) Mucin 1 downregulation associates with corticosteroid resistance in chronic rhinosinusitis with nasal polyps. J Allergy Clin Immunol 135(2):470–476
Milara J, Morell A, Ballester B, Armengot M, Morcillo E, Cortijo J (2017) MUC4 impairs the anti-inflammatory effects of corticosteroids in patients with chronic rhinosinusitis with nasal polyps. J Allergy Clin Immunol 139(3):855–862 e813
Poetker DM (2015) Oral corticosteroids in the management of chronic rhinosinusitis with and without nasal polyps: Risks and benefits. Am J Rhinol Allergy 29(5):339–342
Van Zele T, Gevaert P, Holtappels G, Beule A, Wormald PJ, Mayr S, Hens G, Hellings P, Ebbens FA, Fokkens W et al (2010) Oral steroids and doxycycline: two different approaches to treat nasal polyps. J Allergy Clin Immunol 125(5):1069–1076 e1064
Barnes PJ, Adcock IM (2009) Glucocorticoid resistance in inflammatory diseases. Lancet 373(9678):1905–1917
Hellings PW, Fokkens WJ, Akdis C, Bachert C, Cingi C, Dietz de Loos D, Gevaert P, Hox V, Kalogjera L, Lund V et al (2013) Uncontrolled allergic rhinitis and chronic rhinosinusitis: where do we stand today? Allergy 68(1):1–7
Donohue JF, Jain N (2013) Exhaled nitric oxide to predict corticosteroid responsiveness and reduce asthma exacerbation rates. Respir Med 107(7):943–952
Cowan DC, Taylor DR, Peterson LE, Cowan JO, Palmay R, Williamson A, Hammel J, Erzurum SC, Hazen SL, Comhair SA (2015) Biomarker-based asthma phenotypes of corticosteroid response. J Allergy Clin Immunol 135(4):877–883 e871
Bafadhel M, McKenna S, Terry S, Mistry V, Pancholi M, Venge P, Lomas DA, Barer MR, Johnston SL, Pavord ID et al (2012) Blood eosinophils to direct corticosteroid treatment of exacerbations of chronic obstructive pulmonary disease: a randomized placebo-controlled trial. Am J Respir Crit Care Med 186(1):48–55
Acknowledgements
The study was supported by Grants from National Natural Science Foundation of China (no. 81500768), the Natural Science Foundation of Guangdong Province, China (no. 2014A030310392) and the Science and Technology Planning Project of Guangdong Province, China (no. 2016A020215049).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
No conflicts of interest to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the first affiliated hospital of Sun Yat-sen University and the Shantou Central Hospital research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Lu, H., Lin, XS., Yao, DM. et al. Increased serum amyloid A in nasal polyps is associated with systemic corticosteroid insensitivity in patients with chronic rhinosinusitis with nasal polyps: a pilot study. Eur Arch Otorhinolaryngol 275, 401–408 (2018). https://doi.org/10.1007/s00405-017-4809-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-017-4809-z