Abstract
The purpose of this study was to investigate the relationship between various polysomnographic variables and the success of modified tongue base suspension combined with uvulopharyngopalatoplasty in patients with severe obstructive sleep apnea (OSA). A total of 90 patients who had apnea hypopnea index (AHI) >30 and had both oropharyngeal and hypopharyngeal obstruction were included in this prospective case series with planned data collection. All patients were assessed preoperatively and at the sixth postoperative month by polysomnography. The surgery was considered to be successful when a ≥50 % reduction in the mean AHI to a final AHI of <20/h was obtained. Multiple logistic regression analyses were performed to determine the impact of variables on the surgical success. A total of 67 patients (74.4 %) met the surgical success criteria. The univariate analysis revealed a relationship between success and AHI (P = 0.001), obstructive apnea duration (P = 0.001), sleep time with oxygen saturation below 90 % (ST90) (P = 0.004), minimum O2 saturation (P = 0.0001), mean O2 saturation (P = 0.011), mean O2 desaturation (P = 0.0001), and oxygen desaturation index (P = 0.001). However, ST90 [OR (95 % CI) = 1.40 (1.04–1.89), P = 0.023] was the only independent parameter predicting the surgical success in multivariate analysis. The ROC analysis revealed that the ST90 value of ≤36 min was the best cutoff value with 96.97 % sensitivity (CI 89.5–99.6), 95.83 % specificity (CI 78.9–99.9), 98.5 % PPV (CI 91.6–100.0), and 92.0 % NPV (CI 74.0–99.0). The stratification of patients with severe OSA according to the ST90 may allow better identification of patients in whom surgical success is probable.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) is a global health problem that affects up to 20 % of adults [1]. It is a chronic disease which does not resolve spontaneously, and is rarely completely cured. Continuous positive airway pressure (CPAP) is the gold standard treatment of moderate to severe OSA [2]. Unfortunately, compliance rates are poor with estimates that between 40 and 60 % of patients use CPAP as prescribed, many reject therapy within the first few months [3]. Surgery may be indicated to improve compliance and outcome in cases where CPAP is poorly tolerated [4].
Although anatomic disorders are eliminated by surgery, this disease cannot be eliminated fully in a significant percentage of patients, from which arises the question of whether surgical treatment is overused. If the cases in which surgical success is not probable can be accurately estimated beforehand, then unnecessary surgeries and complications can be avoided. In the current study, we aimed to determine factors predicting the success of multi-level surgery including modified tongue base suspension (mTBS) combined with uvulopharyngopalatoplasty (UPPP) in patients with severe OSA.
Materials and methods
Study design and patients
From November 2011 to February 2014, a total of 90 patients with severe OSA who underwent mTBS combined with UPPP were included in this prospective case series with planned data collection following Institutional Ethics Committee approval. Written informed consent was obtained from all patients. This study was not registered in any trial database.
Prior to study, all of the patients were initially offered CPAP therapy, and were informed about CPAP usage. Patients who cannot tolerate or do not want to use CPAP were offered surgery. Inclusion criteria were (1) severe OSA (apnea hypopnea index (AHI) >30), (2) patients who rejected CPAP, (3) no evidence of nasal obstruction, and (4) existence of both oropharyngeal and hypopharyngeal obstruction. Patients were excluded if they had simple snoring, mild to moderate OSA, central sleep apnea syndrome, history of OSA surgery, body mass index (BMI) >40 kg/m2, age >70 years, serious cardiovascular disease, neuropathy or active neurological disease, medications known to affect peripheral nerves, and diabetes mellitus.
Procedures
Physical head and neck examinations were performed on all patients. The nasal passage opening and the location of the soft palate in relation to the tongue base were assessed. The width and mass of the tongue base, and its distance to the epiglottis was subjectively evaluated with flexible fiberoptic nasopharyngoscopy. Polysomnography (PSG) was applied (Compumedics E Series Profusion) to all patients and was scored manually based on the American Academy of Sleep Medicine 2007 criteria [5]. Apnea was defined as cessation of airflow for at least 10 s with continued effort (obstructive) or lack of effort (central) to breathe. Hypopnea was defined as with a >50 % decrease in a valid measure of airflow without a requirement for associated oxygen desaturation or arousal, and with a lesser airflow reduction in association with oxygen desaturation of >3 % or an arousal for at least 10 s. AHI was defined as the number of apnea and hypopnea occurrences per hour. An AHI score between 5 and 15 was considered as mild OSA; 15–30 as moderate OSA; and >30 as severe OSA.
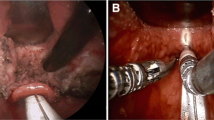
The operating procedures for the mTBS were carried out as we reported in detail in our earlier report [6]. This procedure is a modification of the Repose System which was described by DeRowe et al. [7] without the use of a screw. UPPP was performed using the modified technique described by Shin et al. [8]. Both procedures were performed during the same session by the same surgeon. Patients were informed that they may or may not benefit from this surgery. Even if the surgery may not keep them away from CPAP use completely, it may still be useful in reducing the need for CPAP therapy.
Patients were subjected to a control PSG at the sixth month of postoperative period. Both measurements were carried out in the same laboratory and under the same circumstances. In this study, the surgery was considered to be successful when a ≥50 % reduction in the mean AHI to a final AHI of <20/h was obtained [9].
Statistical analysis
The primary endpoint was the determination of factors predicting the success of mTBS combined with UPPP. We expressed data as median and range for continuous variables. We reported binary variables as counts and percentages. First, simple logistic regression analyses were performed. Variables with a P value <0.05 were included in the multiple logistic regression analysis. The influence of each factor on surgical success was examined using the Wald test. Results were expressed as Odd’s ratio (OR) and 95 % confidential interval (95 % CI). All P values were two-sided with the level of significance set at <0.05. To calculate the cutoff value in predicting surgical success by the independent factor, a receiver operating characteristic (ROC) analysis was calculated using the dichotomous surgical success findings (“Success” and “Failure”). Using the ROC curve, the responsiveness is described in terms of sensitivity and specificity. Values for sensitivity and for false-positive rates (1–specificity) are plotted on the y- and the x-axis of the curve and the area under the curve (AUC) represents the probability that a measure correctly classifies surgery as successful or unsuccessful. In presenting the results, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were all reported. For the ROC curve, the point with the largest sum of sensitivity and specificity was chosen as a threshold. During the comparison of quantitative data, the Wilcoxon Signed Ranks Test was used. All statistical analyses were performed by a professional biostatistician using PASW 18 (SPSS/IBM, Chicago, IL, USA) software.
Results
The median age at surgery was 48 (31–66) years, and most patients were male (91.1 %). The median BMI was 30.7 (24.7–38.6) kg/m2. A total of 67 patients (74.4 %) met the surgical success criteria. Table 1 presents the characteristics of the patients. The median AHI, supine AHI, AHI REM, AHI NREM, arousal index (ARI), and oxygen desaturation index (ODI) were 44.8, 63.9, 46.4, 47, 42.7, and 41 events/h, respectively. The median oxymetric values of patients were as follows: minimum O2 saturation, 77.5 %; mean O2 saturation, 95 %; mean O2 desaturation, 7 %; obstructive apnea duration (OAD), 25.6 s; sleep time with oxygen saturation below 90 % (ST90), 21.5 min; and percentage of cumulative time with oxygen saturation below 90 % (CT90), 5.6 %.
Table 2 compares the preoperative and postoperative PSG results. Postoperatively, mean AHI (51.81 ± 18.84 vs. 20.46 ± 17.73), mean O2 desaturation (8.38 ± 3.95 vs. 6.36 ± 3.80), ODI (47.97 ± 19.49 vs. 18.24 ± 15.50), CT90 (10.86 ± 9.40 vs. 3.86 ± 0.91) and ST90 (44.30 ± 32.30 vs. 21.30 ± 4.10) were decreased, and minimum O2 saturation (75.63 ± 9.30 vs. 82.38 ± 6.57) and mean O2 saturation (94.33 ± 2.60 vs. 95.20 ± 4.41) were increased significantly (p < 0.001 for all parameters). Patients were stratified according to their surgical outcome (success vs. failure), and the main preoperative and postoperative PSG parameters were compared again (Table 3). In patients with surgical success, there were statistically significant differences in all parameters (p < 0.001); whereas in patients with failure, no statistically significant differences were observed.
We performed a logistic regression analysis to determine if those variables have an impact on the success of mTBS combined with UPPP. Table 4 presents unadjusted and adjusted ORs for surgical failure. The univariate analysis revealed a relationship between surgical success and AHI (P = 0.001), OAD (P = 0.001), ST90 (P = 0.004), minimum O2 saturation (P = 0.0001), mean O2 saturation (P = 0.011), mean O2 desaturation (P = 0.0001), and ODI (P = 0.001). However, ST90 [OR (95 % CI) = 1.40 (1.04–1.89), P = 0.023] was the only independent parameter predicting the surgical success in multivariate analysis.
A ROC analysis was performed to determine the ST90 value that would be the most significant in predicting surgical success (Fig. 1). The AUC was determined to be 0.971 ± 0.027 (CI: 0.912–0.995; P = 0.0001). The cutoff value was found to be 36 min, with 96.97 % sensitivity (CI 89.5–99.6), 95.83 % specificity (CI 78.9–99.9), 98.5 % PPV (CI 91.6–100.0), and 92.0 % NPV (CI 74.0–99.0). Patients were stratified according to the cutoff value of ST90 (Table 5). Patients with a ST90 value of ≤36 min had a surgical success rate of 100 %, compared with 8 % in those with a value of >36 min.
Discussion
The current study investigates the relationship between various polysomnographic variables and the surgical success of multi-level surgery including mTBS combined with UPPP in patients with severe OSA. The study provides evidence that the ST90 is a unique independent predictor of surgical success with a high sensitivity and high NPV, and can be used by clinicians to allow better selection of patients to achieve maximal outcomes.
Several studies have assessed the procedural outcomes and predictors of success in OSA surgery [9–16]. However, the surgical approaches evaluated in these studies vary greatly. UPPP is still the most commonly performed procedure for the surgical treatment of OSA [4]. The overall success rate from mild to severe OSA is reported to be approximately 40 % [9]. Several factors including tongue position, tonsil size, BMI, site of pharyngeal narrowing and severity of the disease have been shown related to the surgical success or failure [10–12]. Recently, Zhang et al. [13] reported the results of consecutive 119 patients who underwent velopharyngeal surgery including revised UPPP with transpalatal advancement pharyngoplasty. In this study, the overall success rate was 62.2 %, and three factors including tonsil size, CT90, and the vertical distance between the lower edge of the mandible and the lower edge of the hyoid were found to be predictive in outcomes.
The tongue base obstruction in OSA is generally underestimated. It is well known that hypopharyngeal obstruction especially in the tongue base leads to a more severe respiratory distress than soft palate obstruction, and the chance of tongue base obstruction is higher in severe forms of OSA [17]. Pang et al. [18] demonstrated that while 65 % of the severe OSA patients display more than 50 % tongue base obstruction, the same pathology was observed only in 6.9 % of mild OSA sufferers. In most patients where UPPP has failed to achieve a favorable outcome, it may be due to the fact that identifying the contribution of the tongue base to the upper airway obstruction has been missed [4]. In a recent meta-analysis including 1978 patients with multi-level surgery involving at least two involved anatomic sites, nose, oropharynx and hypopharynx, Lin et al. [14] reported a success rate of 66.4 %. Thomas et al. first presented the preliminary data from a prospective, randomized trial comparing two tongue base surgeries (TBS vs. tongue base advancement) combined with UPPP for patients with moderate to severe OSA. They reported a slight advantage of TBS over tongue base advancement in terms of surgical success (57 vs. 50 %) [15]. In this study, TBS was performed with a minimally invasive technique called Repose system. Later, Vicente et al. [16] aimed to evaluate the usefulness of TBS with the Repose system in addition to UPPP in the treatment of 55 patients with severe OSA, and reported a surgical success of up to 78 %. They also noted that BMI at baseline was the only variable with significant statistical power to predict surgical success (OR 0.85; 0.73–0.95, 95 % CI, P < 0.01). Our success rate is comparable to the result of this report, although there are some differences between the two types of TBS technique used. However, in our study, the logistic regression analysis revealed no evidence of an association between BMI and surgical success.
The pathogenesis of OSA is still fully not known. OSA can be encountered in patients with a normal upper airway anatomy but may not be observed in patients with a narrow upper airway [19]. Reestablishing airway patency in OSA is achieved due to arousal. The mucosal sensory receptor impairment in the upper airway might cause a delayed end-apneic arousal and extension of the apnea duration [20]. The anatomic factors alone were demonstrated to be responsible for 1/3 of all cases, with the remainder being related to neural factors [20, 21]. The longer the apnea duration, the deeper the hypoxia becomes. The ST90 and its percentage to the total sleep time (CT90) are two objective parameters that can be obtained from PSG, and they directly reflect hypoxia. In this study, we demonstrated that the ST90 (≤36 min) rather than other polysomnographic parameters is independently related to the success of surgery with 96.97 % sensitivity and 92.0 % NPV. As the ST90 value exceeds 36 min, the sensitivity is reduced, and the specificity is increased. Consequently, the chances of benefiting from the surgery decrease. We observed a success rate of 100 % in patients with ST90 ≤36 min, whereas this rate was only 8 % in patients with ST90 greater than 36 min.
This is the first study examining the predictors of surgical success in a large series of patients with severe OSA who underwent mTBS combined with UPPP. Potential limitations of our study include the lack of analysis of the anatomical measurements, and subjective evaluation of tongue base and hypopharynx in selection of the patients for this treatment. However, the preoperative precise evaluation of the upper airway anatomy mostly requires imaging studies including magnetic resonance imaging and/or computerized tomography with 3D technology, and it will not be cost-effective to adopt these expensive technologies as a regular part of current practice. So, we suggest that more attention should be paid to the ST90 as an easily available parameter that can be routinely obtained from PSG to predict the treatment outcome.
Conclusion
In conclusion, based on our results, the stratification of patients with severe OSA according to the ST90 may allow better identification of patients in whom surgical success is probable. Future trials are needed to confirm these findings.
References
Ho ML, Brass SD (2011) Obstructive sleep apnea. Neurol Int 3:e15
Holmdahl C, Schöllin IL, Alton M, Nilsson K (2009) CPAP treatment in obstructive sleep apnoea: a randomised, controlled trial of follow–up with a focus on patient satisfaction. Sleep Med 10:869–874
Weaver TE, Grunstein RR (2008) Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc 5:173–178
Kotecha BT, Hall AC (2014) Role of surgery in adult obstructive sleep apnoea. Sleep Med Rev. doi:10.1016/j.smrv.2014.02.003
Iber C, Ancoli-Israel S, Chesson A, Quan S (2007) The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. American Academy of Sleep Medicine, Westchester
Turhan M, Bostanci A, Akdag M (2014) The impact of modified tongue base suspension on CPAP levels in patients with severe OSA. Eur Arch Otorhinolaryngol. doi:10.1007/s00405-014-3034-2
DeRowe A, Gunther E, Fibbi A, Lehtimaki K, Vahatalo K, Maurer J, Ophir D (2000) Tongue-base suspension with soft tissue-to-bone anchor for obstructive sleep apnea: preliminary clinical results of a new minimally invasive technique. Otolaryngol Head Neck Surg 122:100–103
Shin SH, Ye MK, Kim CG (2009) Modified uvulopalatopharyngoplasty for the treatment of obstructive sleep apnea-hypopnea syndrome: resection of the musculus uvulae. Otolaryngol Head Neck Surg 140:924–929
Sher AE, Schechtman KB, Piccirillo JF (1996) The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep 19:156–177
Friedman M, Ibrahim H, Joseph NJ (2004) Staging of obstructive sleep apnea/hypopnea syndrome: a guide to appropriate treatment. Laryngoscope 114:454–459
Launois SH, Feroah TR, Campbell WN, Issa FG, Morrison D, Whitelaw WA, Isono S, Remmers JE (1993) Site of pharyngeal narrowing predicts outcome of surgery for obstructive sleep apnea. Am Rev Respir Dis 147:182–189
Senior BA, Rosenthal L, Lumley A, Gerhardstein R, Day R (2000) Efficacy of uvulopalatopharyngoplasty in unselected patients with mild obstructive sleep apnea. Otolaryngol Head Neck Surg 123:179–182
Zhang J, Li Y, Cao X, Xian J, Tan J, Dong J, Ye J (2013) The combination of anatomy and physiology in predicting the outcomes of velopharyngeal surgery. Laryngoscope. doi:10.1002/lary.24510
Lin HC, Friedman M, Chang HW, Gurpinar B (2008) The efficacy of multilevel surgery of the upper airway in adults with obstructive sleep apnea/hypopnea syndrome. Laryngoscope 118:902–908
Thomas AJ, Chavoya M, Terris DJ (2003) Preliminary findings from a prospective, randomized trial of two tongue-base surgeries for sleep-disordered breathing. Otolaryngol Head Neck Surg 129:539–546
Vicente E, Marín JM, Carrizo S, Naya MJ (2006) Tongue-base suspension in conjunction with uvulopalatopharyngoplasty for treatment of severe obstructive sleep apnea: long-term follow-up results. Laryngoscope 116:1223–1227
Kim JW, Yoon IY, Chung S, Lee CH, Moon SJ, Yun PY (2009) Comparison between tongue base and soft palate obstruction in obstructive sleep apnea. Acta Otolaryngol 129:855–861
Pang KP, Terris DJ, Podolsky R (2006) Severity of obstructive sleep apnea: correlation with clinical examination and patient perception. Otolaryngol Head Neck Surg 135:555–560
Guilleminault C, Ramar K (2009) Neurologic aspects of sleep apnea: is obstructive sleep apnea a neurologic disorder? Semin Neurol 29:368–371
Kimoff RJ, Sforza E, Champagne V, Ofiara L, Gendron D (2001) Upper airway sensation in snoring and obstructive sleep apnea. Am J Respir Crit Care Med 164:250–255
Ryan CM, Bradley TD (2005) Pathogenesis of obstructive sleep apnea. J Appl Physiol 99:2440–2450
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Turhan, M., Bostanci, A. & Bozkurt, S. Predicting the outcome of modified tongue base suspension combined with uvulopalatopharyngoplasty. Eur Arch Otorhinolaryngol 272, 3411–3416 (2015). https://doi.org/10.1007/s00405-014-3311-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-014-3311-0